Abstract
Despite several calls to support evidence-informed policy-making, variations in uptake of evidence into policy persist. This editorial brings together and builds on previous Knowledge Translation (KT) frameworks and theories to present a simple, yet, holistic approach for promoting evidence-informed policies. The proposed conceptual framework is characterized by its impact-oriented approach and its view of KT as a continuum from the evidence synthesis stage to uptake and evaluation, while highlighting capacity and resource requirement at every step. A practical example is given to guide readers through the different steps of the framework. With a growing interest in strengthening evidence-informed policy-making, there is a need to continuously develop theories to understand and improve the science of KT and its implementation within the field of policy-making.
Keywords: Evidence-Informed Policy, Knowledge Translation (KT), Research Utilization, Lebanon
Evidence-informed policy-making refers to the use of the best available data and research evidence in the time available to inform policy decisions (1). The past few years have witnessed an increase in global calls for evidence-informed policies and actions to strengthen health systems and population health (2–4).
Knowledge Translation (KT) has emerged as an important concept in bridging the gap between research and policy. For the purpose of this editorial, we define KT as a “dynamic and iterative process that includes the synthesis, dissemination, exchange and ethically sound application of knowledge to improve health, provide more effective health services and products, and strengthen the healthcare system” (5). A review of the literature revealed a positive movement towards KT in policy-making, with numerous KT frameworks being developed and proposed over the last decade to promote evidence-informed policies (6,7).
Despite international initiatives to support the use of research evidence, variations in uptake of evidence persist (8). In this editorial, we bring together and build on existing KT frameworks, theories and gaps to present a simple, yet, holistic approach for promoting evidence-informed health policies (6,7,9). Some of the existing frameworks do not provide emphasis on context and politics. Others did not address research production, capacity requirements, stakeholder involvement, and monitoring and evaluation as key aspects of KT. In addition, some frameworks proposed a range of activities without a systematic approach, or focused only on the implementation or dissemination process. Thus, our framework was constructed with the aforementioned points in mind to present a comprehensive approach for promoting evidence-informed policies.
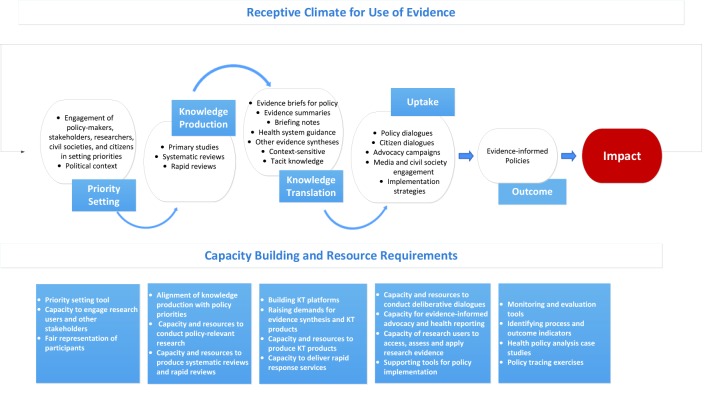
Three key features are integral to the conceptual framework. First, it is impact-oriented, which means that the entire KT process should be driven by the desired end results. Second, the framework presents KT as a continuum that commences from the point of setting the research agenda to implementation into policy and evaluation. Third, capacity building and resource requirement are incorporated into every step of the framework as critical components to successful evidence-informed policy-making. The proposed framework is presented in Figure 1.
Figure 1 .
A conceptual framework for a backward design in Knowledge Translation (KT)
Capacity building components
Central to the framework is capacity building for researchers, users of research, and relevant stakeholders. Specifically, capacity-building efforts should target the individual, team, institutional, and systems levels (10). At the individual level, these include researchers’ skills to: i) conduct policy-relevant research and systematic reviews, ii) prepare evidence briefs for policy and other evidence synthesis products, iii) engage research users and other stakeholders in priority setting meetings and deliberative dialogues, and iv) conduct ongoing monitoring and evaluations (11,12). For research users and other stakeholders in particular, capacity should be built to access, assess and apply research evidence into policy-making as well as to promote evidence-informed advocacy and health reporting (the latter especially for media). At the team level, efforts should be directed towards the formation of groups with the right mix of skills and expertise to undertake systematic reviews and other evidence synthesis products. The institutional level components include institutional strengthening for KT (technical support and protected time for faculty members and researchers) and integration of KT courses within curricula. Efforts should also be directed towards the establishment of demand-driven rapid response units and online clearinghouses for timely response to research users’ and other stakeholders’ needs (11,12). At the systems level, strong leadership support is required to promote a receptive climate for evidence-informed policies. This should be coupled with institutionalized mechanisms for researcher-policy-maker interactions (e.g. KT platforms), and supportive policy structures for implementation of research evidence (plans, guidelines, monitoring frameworks) (6). These are crucial as they can potentially offset the consequences of the high turnover in government related to leakage of capacity, discontinued relationships and shuffled priorities.
An overview of the different steps in the framework: a practical example
We will use the food safety issue in Lebanon as a practical example to guide readers through the different steps of the framework. Recently, there have been serious public concerns about food safety in Lebanon. In November 2014, the Lebanese public was overwhelmed with the latest food contamination scandal when the Minister of Public Health publicized a list of restaurants, supermarkets and other food service providers that did not meet the ministry’s food regulation standards with some products testing positive for salmonella, E. coli, and obligate aerobes. This adds to already existing concerns about food safety in Lebanon as illustrated by several cases of spoiled and expired food that were discovered in the last few years.
The proposed framework can be used to guide efforts to promote evidence-informed policies and action on food safety.
The first step would be to specify the desired outcomes and impact of the given priority topic. The choice of priority topic requires careful considerations of the political environment and judgment about whether a window of opportunity for action could open, or has opened, which can help push the problem or option higher on the political agenda (13).
The case study under investigation received significant media coverage coupled with the political-will of the Minister of Health to address the issue, which opened a window of opportunity for action. Indeed, the convergence of Kingdon’s politics, problem, and policy streams rendered this a priority topic. In this case, the outcome of the KT process would be the establishment of an effective food safety system informed by the best available evidence, which in turn would ensure the provision of safe food to consumers (desired impact). To achieve these, we would need to move through the different steps of the framework, starting with the priority setting exercise. The priority setting exercise should engage researchers, policy-makers and other stakeholders including implementing actors, civil societies and consumer groups to deliberate on the causes of the problem (i.e. inadequate food safety laws and weak governance) and prioritize research areas and review questions. Establishing a sustained partnership with all relevant stakeholders that spans the entire process from setting the research agenda to implementation, increases the acceptability of the evidence among stakeholders, which in turn, promotes its uptake and use in policy-making (6,11,14). Although the role of civil societies and community representatives remains largely unexplored (15), involving the latter two groups is important in light of the increasing push for people-centred care and people-centred health systems. In fact, the involvement of civil societies in priority setting has been successful in several African countries (16).
Following the priority setting exercise, a team of researchers working at KT platforms would proceed with searching for global research evidence and systematic reviews that align with the prioritized research areas on effective governance and food safety law (they may also consider conducting a systematic review or rapid review depending on what they find). The researchers would then need to package the information using audience-tailored formats and disseminate it to different user groups through multiple channels. Several KT tools are available, including evidence briefs for policy, evidence summaries, and briefing notes (12,17). The choice of KT product will eventually depend on the target audience, the type and quality of research evidence and availability of local data. For the case study at hand, preparing an evidence brief for policy or briefing note can effectively advise policy-makers and stakeholders about the food safety problem (by bringing together global research evidence and local evidence) and offer options and/or recommendations for action. This can be supplemented by the development of media releases and the use of mass media to disseminate the findings on effective food safety systems.
However, as research evidence is only one input into the policy-making process, researchers would need to consider holding a deliberative dialogue with a diverse range of audiences (12,18). Such dialogues have recently captured attention given their potential to address several key factors that influence the uptake of evidence in policy-making, namely: 1) interactions between researchers and policy-makers; 2) timeliness of evidence; and 3) helping identify accordance between research evidence and the values, beliefs, interests or political goals, and strategies of politicians, stakeholders, and civil servants (19). A good example on the importance of the latter point can be drawn from the voluntary health insurance policy in Lebanon where failure to establish accordance between research evidence and tacit knowledge led to its eventual collapse (20).
For critical issues in particular, researchers may also consider holding a citizen panel which provides an opportunity for citizens to share their views and experiences about the issue, which in turn can inform the deliberative dialogue. In Ontario, for example, citizen panel dialogues directly informed the Medical Association’s end-of-life care strategy (18).
While advocacy may not be needed for all issues, it is important to develop an advocacy strategy for topics with ethical and equality implications (21) or politically-charged topics with conflicting stakeholders’ interests. One good example to draw upon is the tobacco law in Lebanon which involved banning of smoking in public places and closed spaces. A significant amount of resources was expended on advocacy and lobbying to promote the uptake of the law. The advocacy strategy was successful since the law was eventually adopted and implemented, albeit for a short time; law 174 proved not to be sustainable and failed to achieve its intended objectives. Why was that? This brings us to the importance of the next, often overlooked, step which entails coming up with and incorporating strategies to support policy implementation and enforcement, with particular attention to system capacity in terms of infrastructure, technical support, inputs (including existing policies) and personnel (type and skills). In the absence of a well-designed implementation strategy to ensure the success and sustainability of the tobacco law, it eventually collapsed. Thus, to avoid the occurrence of a similar scenario for the food safety law, it would be critical to develop an implementation strategy that takes into consideration the barriers, facilitators, and ways to overcome barriers along every step of implementation.
At this point, we would like to re-iterate on the importance of taking the context into consideration when deciding on the different KT strategies and tools throughout the entire continuum. Indeed, evidence has shown that contextual factors, particularly the institutions, interests, and values of a given context, can influence the uptake of the evidence and its usefulness in supporting evidence-informed health policies (11,22). The existing political system is another contextual issue that needs to be considered when implementing the framework. A recent systematic review identified the level of state centralization and democratization as one of the “relevant political and institutional aspects affecting the use of health evidence” (23). The included studies suggested that centralized political systems were likely to be less open to the uptake of research evidence than decentralized systems and democratic governments (23). Regardless of the type of government, the presence of a receptive environment for the use of evidence is essential for the operation of the framework.
Following the implementation of a policy, it is important to assess success in achieving the desired outcomes and impacts (identified at the very beginning). Two questions immediately come to mind: what should we evaluate? And are we interested in the KT process or its outcomes and impact? Indeed, there is no consensus among researchers as to the best way to evaluate knowledge use (24). The proposed framework incorporates two types of evaluations: KT process evaluation at every step of the continuum, and outcome and impact evaluations towards the end. KT process evaluation examines whether the policy, program or service was formulated and implemented as intended (e.g. establishment of an effective food safety policy informed by the best available evidence). For outcome evaluations, these include short-term outcomes related to KT activities (e.g. improved relationship between researchers and research users) and intermediate outcomes related to whether the policy achieved the anticipated results or if there were unanticipated outcomes (e.g. delivery of safe food to consumers). Impact evaluation reflects the ultimate goal of the policy, program or service in improving health systems and population health status.
The framework also highlights the importance of planning for and integrating monitoring and evaluation as key components of KT right from the very start. Such evaluations allow us to measure whether, how, and why research evidence was used or not used in policy, and whether the policy achieved its intended outcomes and impact. While some efforts have been put to evaluate outcomes such as strengthened relationships among policy-makers, stakeholders and researchers, and enhanced capacity for undertaking and using research (11,17), very little has been done to evaluate the impact of implementing evidence-informed policy-making (e.g. improved population health status) (25–27). Indeed, there is a general assumption that evidence-informed policy-making will eventually improve outcomes; however, the evidence base to support/disprove this assumption is not robust. As such, assessing the impact of policies informed by evidence is needed to complete the monitoring and evaluation cycle and to strengthen the case for promoting evidence-informed health policies. More so, by assessing impact and linking it to the process of knowledge uptake, one can examine how instrumental, conceptual, or symbolic use of knowledge (24) differentially affect policy development and implementation, which in turn can contribute to a better understanding of the various elements that drive the KT process.
Going back to the food safety example, researchers and research users as well as other key stakeholders including funders and civil society groups would need to monitor the role of evidence in informing the implementation of an effective food safety system and evaluate the impact of evidence-informed policy-making on the safety of food in Lebanon. In the absence of clear mechanisms for evaluating impact, they may consider conducting policy tracing whereby data is collected using multiple sources including comprehensive and chronological media review, key informant interviews, and document reviews. Policy tracing was successfully employed to explore the development, implementation and impact of the voluntary health insurance policy in Lebanon (20).
The way forward
KT is a relatively new and evolving concept that is gaining increasing interest within the field of policy-making. This editorial piece is a call for institutions in countries (i.e. universities, civil society groups, think tanks, ministries, etc.) to start investing in evidence syntheses and creating centers/systems that specialize in KT. The framework can serve as guidance, characterized by its impact-based approach and its push for KT as a continuum from the pre-research generation/evidence synthesis stage to uptake and evaluation, while highlighting capacity and resource requirement at every step. This can be particularly useful for low- and middle-income countries where few studies exist on KT (16).
The key messages in the framework are as follows: policy-makers and other relevant research users need to work on creating a receptive climate for evidence-informed policy-making and institute a “user-pull” for evidence. Researchers need to align the production of research and systematic reviews with policy-makers’ and stakeholders’ priorities as well as prepare various KT products and engage research users in dialogues and priority settings. Communities, civil societies and media need to be empowered and assume stronger roles in priority setting, advocacy, and dialogues to promote evidence informed policies. Finally, funders need to earmark funding to projects that link research to policy and to capacity building activities that target the different steps, levels, and participants along the framework.
With a growing interest in strengthening evidence-informed policy-making, there is a need to continuously develop theories to understand and improve the science of KT (28) and its implementation within the field of policy-making. Specifically, there is a need for further research on the effectiveness of different KT strategies and KT tools and on ways in which they are designed and the context in which they are developed. Indeed, the role of context in the uptake of evidence into policy and the influence of political systems on the use of KT frameworks are critical areas that warrant further exploration. Equally important is the need to develop rigorous methods and instruments for evaluating the outcome and impact of KT and evidence-informed policies. Our proposed framework can be operationalized and tested through research studies using sound methodologies and key indicators. The issues highlighted in this editorial should remain the subject of ongoing deliberations if we are to improve our understanding of KT and its role in promoting evidence-informed policies and practice.
Ethical issues
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
FE contributed to the conception of this editorial and both authors contributed to the design, drafting, and revision of the final manuscript.
Authors’ affiliations
1Department of Health Management and Policy, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon. 2Knowledge to Policy (K2P) Center, American University of Beirut, Beirut, Lebanon. 3Center for Systematic Reviews in Health Policy and Systems Research (SPARK), American University of Beirut, Beirut, Lebanon. 4Department of Clinical Epidemiology and Biostatistics, Faculty of Health Sciences, McMaster University, Hamilton, Ontario, Canada.
Citation: El-Jardali F, Fadlallah R. A call for a backward design to knowledge translation. Int J Health Policy Manag 2015; 4: 1–5. doi: 10.15171/ijhpm.2015.10
References
- 1.Lavis JN, Oxman AD, Lewin S, Fretheim A. SUPPORT Tools for evidence-informed health Policymaking (STP) 3: Setting priorities for supporting evidence-informed policymaking. Health Res Policy Syst. 2009;7 Suppl 1:S3. doi: 10.1186/1478-4505-7-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Assembly: Resolution on Health Research. 2005. Available from: http://www.who.int/rpc/meetings/58th_WHA_resolution.pdf.
- 3. World Health Organization (WHO). The Bamako Call to Action on Research for Health. 2008. Available from: http://www.who.int/gb/ebwha/pdf_files/EB124/B124_12Add2-en.pdf.
- 4. Beijing Statement from the Second Global Symposium on Health Systems Research. 2012. Available from: http://healthsystemsresearch.org/hsr2012/images/stories/downloads/beijing%20_statement.pdf.
- 5.Straus S. Defining knowledge translation. CMAJ. 2009;181:165–8. doi: 10.1503/cmaj.081229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orem JN, Mafigiri DK, Marchal B, Ssengooba F, Macq J, Criel B. Research, evidence and policymaking: the perspectives of policy actors on improving uptake of evidence in health policy development and implementation in Uganda. BMC Public Health. 2012;12:109. doi: 10.1186/1471-2458-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization (WHO). Knowledge translation framework for ageing and health [internet]. 2012. Available from: http://www.who.int/ageing/publications/knowledge_translation/en/.
- 8.Murthy L, Shepperd S, Clarke MJ, Garner SE, Lavis JN, Perrier L. et al. Interventions to improve the use of systematic reviews in decision-making by health system managers, policy makers and clinicians. Cochrane Database Syst Rev. 2012;9:CD009401. doi: 10.1002/14651858.CD009401.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43:337–50. doi: 10.1016/j.amepre.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bangpan M, Stansfield C, Vigurs C, Oliver S. Systematic reviewing in low and middle income countries: a rapid appraisal of capacity. 2013. EPPI-Centre, SSRU, Institute of Education, University of London. Available from: http://www.cochrane.org/sites/default/files/uploads/CCSG%20agenda%20and%20open%20access%20background%20papers%20-%20Quebec%202013.pdf.
- 11.El-Jardali F, Lavis J, Moat K, Pantoja T, Ataya N. Capturing lessons learned from evidence-to-policy initiatives through structured reflection. Health Res Policy Syst. 2014;12:2. doi: 10.1186/1478-4505-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavis JN, Lomas J, Hamid M, Sewankambo NK. Assessing country-level efforts to link research to action. Bull World Health Organ. 2006;84:620–8. doi: 10.2471/blt.06.030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lavis JN. How can we support the use of systematic reviews in policymaking? PLoS Med. 2009;6:e1000141. doi: 10.1371/journal.pmed.1000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lavis JN, Catallo C. Bridging the worlds of research and policy in European health systems. Copenhagen, Denmark: WHO Regional Office for Europe; 2013. [PubMed]
- 15.Armstrong R, Waters E, Roberts H, Oliver S, Popay J. The role and theoretical evolution of knowledge translation and exchange in public health. J Public Health. 2006;28:384–9. doi: 10.1093/pubmed/fdl072. [DOI] [PubMed] [Google Scholar]
- 16.Young J. Research, policy and practice: why developing countries are different. J Int Dev. 2005;17:727–34. doi: 10.1002/jid.1235. [DOI] [Google Scholar]
- 17.Moat KA, Lavis JN, Clancy SJ, El-Jardali F, Pantoja T. Evidence briefs and deliberative dialogues: perceptions and intentions to act on what was learnt. Bull World Health Organ. 2014;92:20–8. doi: 10.2471/blt.12.116806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson M, Lavis J, Moat K, Paprica A, Panisset U. The State-of-the-Art in Policy-Focused Knowledge Translatio. CAHSPR Annual Conference. 2014 [Google Scholar]
- 19.Lavis J, Boyko J, Gauvin F. Evaluating deliberative dialogues focused on healthy public policy. BMC Public Health. 2014;14:1287. doi: 10.1186/1471-2458-14-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-Jardali F, Bou-Karroum L, Ataya N, El-Ghali HA, Hammoud R. A retrospective health policy analysis of the development and implementation of the voluntary health insurance system in Lebanon: Learning from failure. Soc Sci Med. 2014;123:45–54. doi: 10.1016/j.socscimed.2014.10.044. [DOI] [PubMed] [Google Scholar]
- 21.Carlisle S. Health promotion, advocacy and health inequalities: a conceptual framework. Health Promot Int. 2000;15:369–76. doi: 10.1093/heapro/15.4.369. [DOI] [Google Scholar]
- 22.Moat KA, Lavis JN, Abelson J. How contexts and issues influence the use of policy-relevant research syntheses: a critical interpretive synthesis. Milbank Q. 2013;91:604–48. doi: 10.1111/1468-0009.12026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liverani M, Hawkins B, Parkhurst JO. Political and Institutional Influences on the Use of Evidence in Public Health Policy A Systematic Review. PLoS One. 2013;8:e77404. doi: 10.1371/journal.pone.0077404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lemire N, Souffez K, Laurendeau M. Facilitating a knowledge translation process: Knowledge review and facilitation tool. Institut National de Sante Publique du Quebec; 2013. p. 1-71.
- 25.LaRocca R, Yost J, Dobbins M, Ciliska D, Butt M. The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health. 2012;12:751. doi: 10.1186/1471-2458-12-751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bunn F, Sworn K. Strategies to promote the impact of systematic reviews on healthcare policy: A systematic review of the literature. Evid Policy. 2011;7:403–28. doi: 10.1332/174426411x603434. [DOI] [Google Scholar]
- 27.Mitton C, Adair CE, McKenzie E, Patten SB, Wayne Perry B. Knowledge transfer and exchange: Review and synthesis of the literature. Milbank Q. 2007;85:729–68. doi: 10.1111/j.1468-0009.2007.00506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brehaut JC, Eva KW. Building theories of knowledge translation interventions: use the entire menu of constructs. Implement Sci. 2012;7:114. doi: 10.1111/j.1468-0009.2007.00506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]