Abstract
Obtaining an aesthetic and functional primary surgical repair in patients with complete cleft lip and palate (CLP) can be challenging due to tissue deficiencies and alveolar ridge displacement. This study aimed to describe surgeons’ assessments of presurgical deformity and predicted surgical outcomes in patients with complete unilateral and bilateral CLP (UCLP and BCLP, respectively) treated with and without nasoalveolar molding (NAM). Cleft surgeon members of the American Cleft Palate-Craniofacial Association completed online surveys to evaluate 20 presurgical photograph sets (frontal and basal views) of patients with UCLP (n=10) and BCLP (n=10) for severity of cleft deformity, quality of predicted surgical outcome, and likelihood of early surgical revision. Five patients in each group (UCLP and BCLP) received NAM and five did not receive NAM. Surgeons were masked to patient group. Twenty-four percent (176/731) of surgeons with valid email addresses responded to the survey. For patients with UCLP, surgeons reported that for NAM-prepared patients 53.3% had minimum severity clefts, 58.9% were anticipated to be among their best surgical outcomes, and 82.9% were unlikely to need revision surgery. For patients with BCLP, these percentages were 29.8%, 38.6%, and 59.9%, respectively. Comparing NAM to non-NAM prepared patients showed statistically significant differences (p < 0.001), favoring NAM-prepared patients. This study suggests that cleft surgeons assess NAM-prepared patients as more likely to have less severe clefts, to be among the best of their surgical outcomes, and to be less likely to need revision surgery when compared to patients not prepared with NAM.
Keywords: nasoalveolar molding, cleft lip and palate
Introduction
The tissue deficiencies and alveolar displacement characteristic of complete cleft lip and palate can make achieving an aesthetic and functional primary repair challenging for the surgeon.1 Patients with wider and more severe clefts generally have more pronounced nasolabial stigmata that tend to worsen with growth.2 If the residual deformity is severe, early secondary cheilorhinoplasty may be indicated to improve nasolabial aesthetics, function, and psychosocial development. Salyer and Henkel et al. report the need for early revisions in as many as 35% of their cases.3,4 However, the incidence of secondary deformities varies by cleft type and is most likely in patients with complete bilateral cleft lip and palate.
Nasoalveolar molding (NAM) is a technique developed by Grayson et al. intended to improve long-term outcomes in patients with cleft lip and palate.5–7 The goal of NAM is to reduce the cleft defect and mold it into a more mild form to improve primary surgical outcomes. This therapy utilizes a removable appliance carefully adjusted to gradually restore normal form and symmetry to the nasolabial region, precisely approximate the alveolar segments, increase patency of the cleft sided nostril(s), and non-surgically elongate the columella.6 Benefits of NAM include improved long-term nasal symmetry, reduction in the number of nasal surgical revisions, and reduced need for secondary alveolar bone grafting when gingivoperiosteoplasty is performed.8–13 Today, 37% of cleft centers in the US report offering NAM.14
The aim of this rater-masked quasi-experimental study was to compare cleft surgeons’ assessments of NAM- and non-NAM-prepared patients with complete cleft lip and palate in terms of the presurgical severity of cleft deformities and anticipated surgical outcomes, including need for secondary cheilorhinoplasty. If NAM therapy influences aesthetic and surgical outcomes, then the following hypotheses should be upheld: compared to patients without NAM preparation, surgeons will, on average, rate patients who received NAM preparation as 1) having less severe clefts prior to primary repair, 2) having better anticipated surgical outcomes, and 3) being less likely to require early revision surgery.
Material and Methods
After obtaining Institutional Review Board approval (IRB#13-676), an initial invitation and up to two follow-up invitations to non-respondents were sent to all of the plastic surgeons and oral surgeons (hereafter “cleft surgeons”) on the American Cleft Palate-Craniofacial Association’s (ACPA) member email list asking them to review and answer questions based on preoperative photographs of twenty patients (hereafter “patients”). Between April 11 and May 5, 2013, we received responses from 176 of 731 surgeons with valid email addresses (24% response rate).
The surgeons were asked to 1) rate the severity of the cleft deformity in this patient compared to other patients they had seen prior to primary surgical repair as minimum, moderate, or maximum severity; 2) take into consideration the width of the cleft, displacement of premaxilla, position of lip segments, asymmetry of alar bases, nasal cartilage form, amount of columella and the shape of the nose, and indicate whether they expected the patient would be among the best, average, or least good of their usual surgical outcomes; and 3) indicate, based upon the expected outcome of the primary surgical repair and degree of severity that presents presurgically, whether the patient would be likely or not likely to need revision surgery prior to entering school (age 5–6 years).
All surgeons received the patients’ preoperative photographs with standardized pictures of two views: frontal and basal (Figures 1 and 2). Presentation was consistent for all surgeons. Of the twenty patients presented in the survey, ten had received presurgical preparation with NAM (all performed by the senior author, BHG) and ten had not; respondents were masked to the NAM treatment status. Within each treatment group, ten of the patients had complete unilateral cleft lip and palates (UCLP), and ten had complete bilateral cleft lip and palates (BCLP).
Figure 1.

Representative sample of unilateral cleft lip and palate patient photographs. Nasoalveolar molding-prepared patient (Above). Non-nasoalveolar molding-prepared patient (Below). Of note, respondents were masked to the nasoalveolar molding treatment status.
Figure 2.

Representative sample of bilateral cleft lip and palate patient photographs. Nasoalveolar molding-prepared patient (Above). Non-nasoalveolar molding-prepared patient (Below). Of note, respondents were masked to the nasoalveolar molding treatment status.
Responses on the first two questions were dichotomized (minimum (1) versus moderate to maximum severity clefts (0); and best surgical outcome (1) versus average to least-good surgical outcome (0)). The responses to the survey resulted in 2,774 observations including 1,496 observations on patients with BCLP and 1,278 on those with UCLP.
To provide summary statistics and compare treatment groups, the likelihood that a particular surgeon would positively rate a NAM-prepared patient (e.g., as having a minimum severity cleft) was calculated and compared to the likelihood that a non-NAM-prepared patient was described in the same way. Cross-tabulations of these data are presented, which provide bivariate results. As a starting estimate, crude differences between surgeons’ ratings of patients with and without NAM are also provided. However, these crude estimates may be biased by repetition in the data: each surgeon rated more than one patient, and more than one surgeon rated each patient. Such repetition can lead to substantial biases and poor model fit, likely increasing the chance of type I error.15 Thus, a cross-classified multi-level logistic modeling (CCMLM) approach was used to ensure robust estimates.16,17 CCMLM approaches are particularly useful because they provide estimates that are robust to data that are missing at random, for instance, due to surgeons’ attrition because of time constraints. The importance of using multi-level logistic over logistic regression was tested to ensure that the CCMLM models provided the best fitting models. To compare types of statistical models, Akaike Information Criteria (AIC) and the relative likelihood (RL) were used.18 The RL estimates the probability that a new model improves on the older model; an RL < 0.05 is interpreted as suggesting that the new model is the better fitting model. Beta coefficients and 95% confidence intervals (95% CI) are provided. For expository purposes, these models are further used to estimate the average percent of surgeons that describe NAM- and non-NAM-prepared patients as having a minimum severity cleft, having the best anticipated surgical outcome, and being unlikely to need revision; these percentages and their corresponding 95% CIs are presented in the figures.
Results
Descriptive analyses
The survey provided information on surgeons’ ratings of patients’ cleft severity, best anticipated surgical outcome, and whether early revision surgery was likely to be necessary (Table 1). Of the 20 patient photograph sets, by design 10 (50%) were patients with BCLP. Masked to the surgeons, 50% of photographs were of NAM-treated patients. Considering the entire sample, surgeons rated 21.3% of patients as having minimal severity clefts, 26.6% as having the best anticipated surgical outcome, and 53.0% as unlikely to require early revision surgery. Within both the UCLP and BCLP groups, crude differences suggest that NAM-prepared patients were more positively rated compared to non-NAM-prepared patients on each of the three outcomes of interest. For example, among patients with UCLP, while over half of those NAM-prepared were considered to have a minimal severity cleft, the best anticipated surgical outcome, and unlikely to need revision, fewer than a third of those without NAM-preparation were rated as such. Among patients with BCLP, results were similar as patients with NAM-preparation were more favorably rated than patients without NAM preparation.
Table 1.
Sample characteristics and bivariate analyses examining the relationship between NAM preparation status and ratings of cleft severity and expected outcomes
| Outcome | Minimum Severity Clefts | Best Anticipated Surgical Outcome | Unlikely to Need Revision | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall % | 21.3 | 26.6 | 53.0 | |||||||||
| Cleft Type | Unilateral | Bilateral | Unilateral | Bilateral | Unilateral | Bilateral | ||||||
|
| ||||||||||||
| % By Cleft Type | 27.8 | 15.7 | 33.7 | 20.6 | 64.6 | 43 | ||||||
| NAM Status | No NAM | NAM | No NAM | NAM | No NAM | NAM | No NAM | NAM | No NAM | NAM | No NAM | NAM |
|
| ||||||||||||
| % By Cleft Type and NAM status | 2.5 | 53.1 | 1.7 | 29.8 | 8.8 | 58.6 | 2.7 | 38.6 | 26.4 | 59.9 | 46.8 | 82.6 |
| Difference between patients with and without NAM | 50.6 | *** | 28.1 | *** | 49.8 | *** | 36 | *** | 33.5 | *** | 35.9 | *** |
Note:
p<0.001,
Support for model selection
In order to address potential repetition bias by the respondents or by repeated analysis of the same patients’ photographs, we assessed different model assumptions using tests of model fit (Table 2). These results show that logistic regression provides a good model fit – the AIC is significant, and the coefficients (not shown: B = 3.2 and 3.8 for UCLP and BCLP respectively) are also highly significant. Incorporating the first level of model clustering, around the surgeons’ responses, provides a better fitting model: the AIC is smaller, the relative likelihood < 0.05. Further, using cross-classified models provide an even better model fit, the AIC is smaller again and the relative likelihood, comparing cross-classified models to multilevel models, shows improved fit as well (relative likelihood < 0.001). This analysis suggests that using the cross-classified models provide the best-fitting results; however, in this case, the conclusions derived from each of these models would be similar.
Table 2.
Assessing model fit using the Akaike information criteria and the relative likelihood that progressive models are similar to or worse than the previous model using estimates linking nasoalveolar molding status to surgical outcomes
| Logistic Regression
|
Multilevel regression adjusting for doctor-level grouping
|
Cross-classified multi-level logistic models shown
|
|||||
|---|---|---|---|---|---|---|---|
| Est. | p-value | Est. | p-value | Est. | p-value | ||
| UCLP Minimum severity cleft | AIC RL |
1034 | <0.001 | 891 <0.001 |
<0.001 | 873 <0.001 |
<0.001 |
|
| |||||||
| Best anticipated surgical outcome | AIC RL |
1246 | <0.001 | 1101 <0.001 |
<0.001 | 1088 0.002 |
<0.001 |
|
| |||||||
| No revision necessary | AIC RL |
1459 | <0.001 | 886 <0.001 |
<0.001 | 878 0.011 |
<0.001 |
|
| |||||||
| BCLP Minimum severity cleft | AIC RL |
1040 | <0.001 | 990 <0.001 |
<0.001 | 806 <0.001 |
<0.001 |
|
| |||||||
| Best anticipated surgical outcome | AIC RL |
1178 | <0.001 | 1112 <0.001 |
<0.001 | 971 <0.001 |
<0.001 |
|
| |||||||
| No revision necessary | AIC RL |
1861 | <0.001 | 1348 <0.001 |
<0.001 | 1255 <0.001 |
<0.001 |
Note: Est. is the estimated value; UCLP is unilateral cleft lip and palate. BCLP is bilateral cleft lip and palate. AIC is the Akaike’s information criterion
Unilateral cleft lip and palate
Associations between NAM treatment among patients with UCLP and the likelihood of surgeons positively rating patients on the variables of interest are provided (Table 3). Significantly different responses from surgeons regarding NAM- and non-NAM-prepared patients were observed; NAM-prepared patients were more likely to be rated as having minimal severity clefts (B = 5.45, p < 0.001), being among the best anticipated surgical outcomes (B = 3.84, p < 0.001), and not needing early revision surgery (B = 4.68, p < 0.001) compared to the non-NAM prepared patients.
Table 3.
Cross-classified multi-level logistic model examining the relationship between nasoalveolar molding preparation status and ratings of cleft severity and expected outcomes among patients with unilateral cleft lip and palate
| Minimum severity cleft
|
Best anticipated surgical outcome
|
Unlikely to need revision
|
|||||
|---|---|---|---|---|---|---|---|
| B | 95% C.I. | B | 95% C.I. | B | 95% C.I. | ||
| NAM | 5.45 | (4.46, 6.44) | 3.84 | (3.14, 4.54) | 4.68 | (3.65, 5.71) | |
|
| |||||||
| Random Intercepts | SD(Surgeons) | 0.50 | (0.28, 0.92) | 0.41 | (0.22, 0.76) | 0.59 | (0.33, 1.07) |
| SD(Patients) | 2.01 | (1.61, 2.5) | 1.69 | (1.37, 2.08) | 4.34 | (3.52, 5.34) | |
|
| |||||||
| AIC | 875.5 | 1089.6 | 879.5 | ||||
Note: NAM is nasoalveolar molding; SD is standard deviation; C.I. is confidence interval; AIC is the Akaike’s information criterion
As depicted in Figure 3, which illustrates estimated population averages, over half of the respondents reported that NAM-prepared patients had minimum severity clefts compared to 2.0% who rated non-NAM prepared patients in the same (53.3% ≠ 2.0%, p < 0.001). Similarly, after considering the degree and type of cleft dysmorphology, 58.9% of surgeons anticipated the NAM-prepared patients to be among the best of their usual surgical outcomes, while 8.1% anticipated non-NAM-prepared patients to be among their best (58.9% ≠ 8.1%, p < 0.001). Finally, 82.9% of surgeons suggested that NAM-prepared patients were unlikely to need revision surgery, compared to 46.7% for non-NAM-prepared patients (82.9% ≠ 46.7%, p < 0.001).
Figure 3.
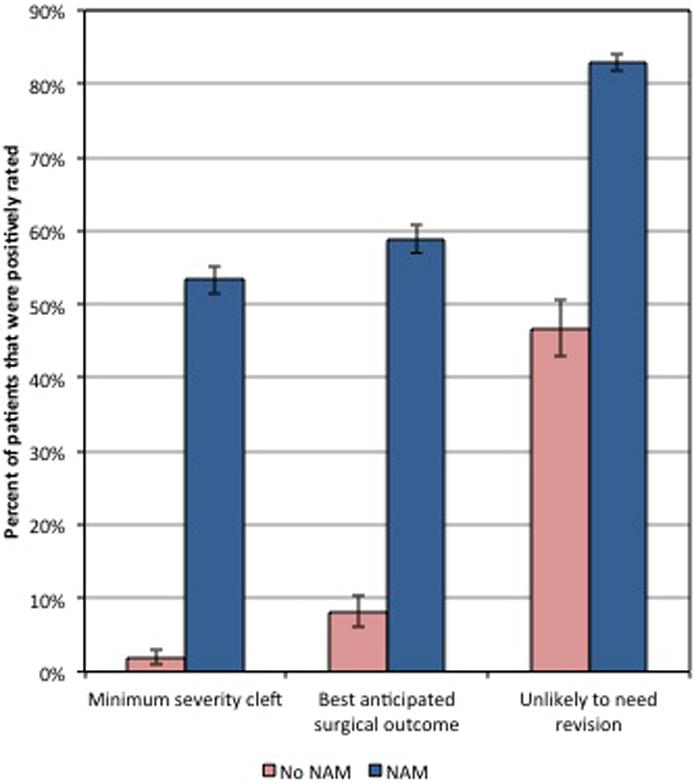
Surgeons’ ratings of cleft severity and anticipated surgical outcomes among unilateral cleft lip and palate patients by nasoalveolar molding preparation group. Estimates and 95% confidence intervals generated from cross-classified multilevel models. Note: All differences between nasoalveolar molding-prepared patient and non-nasoalveolar molding-prepared patient groups are significant (p < 0.001); NAM = nasoalveolar molding.
Bilateral cleft lip and palate
Results among patients with BCLP (Table 4) similarly reveal that surgeons more favorably rated those with NAM preparation compared to those without NAM preparation on all three variables of interest. NAM-prepared patients were more likely to be rated as having minimal severity clefts (B = 5.00, p < 0.001), being among the best anticipated surgical outcomes (B = 4.62, p < 0.001), and not needing early revision surgery (B = 3.47, p < 0.001). The estimated averages (Figure 4) indicate substantial differences depending on NAM status: approximately 30% of surgeons rated NAM-prepared patients as having ‘minimum severity’ clefts whereas 1.6% of surgeons rated non-NAM-prepared patients in same way, a significant difference (29.8% ≠ 1.6%, p < 0.001). Similarly, though 38.6% of surgeons anticipated that NAM-prepared patients would be among the best of their usual surgical outcomes, 2.5% suggested as such for non-NAM-prepared patients (38.6% ≠ 2.5%, p < 0.001). Finally, while 59.9% of surgeons rated NAM-prepared patients as unlikely to need revision surgery, 26.2% anticipated the same for non-NAM-prepared patients (59.9 ≠ 26.2, p < 0.001).
Table 4.
Cross-classified multi-level logistic model examining the relationship between nasoalveolar molding preparation status and ratings of cleft severity and expected outcomes among patients with bilateral cleft lip and palate
| Minimum severity cleft
|
Best anticipated surgical outcome
|
Unlikely to need revision
|
|||||
|---|---|---|---|---|---|---|---|
| B | 95% C.I. | B | 95% C.I. | B | 95% C.I. | ||
| NAM | 5.00 | (2.81, 7.19) | 4.62 | (2.94, 6.30) | 3.47 | (2.11, 4.83) | |
|
| |||||||
| Random Intercepts | SD(Surgeons) | 1.50 | (0.88, 2.58) | 1.19 | (0.71, 2.00) | 1.03 | (0.63, 1.66) |
| SD(Patients) | 1.85 | (1.45, 2.36) | 1.66 | (1.32, 2.09) | 3.31 | (2.76, 3.96) | |
|
| |||||||
| AIC | 807.8 | 972.5 | 1257.2 | ||||
Note: NAM is nasoalveolar molding; SD is standard deviation; AIC is Akaike’s information criterion; C.I. is confidence interval
Figure 4.
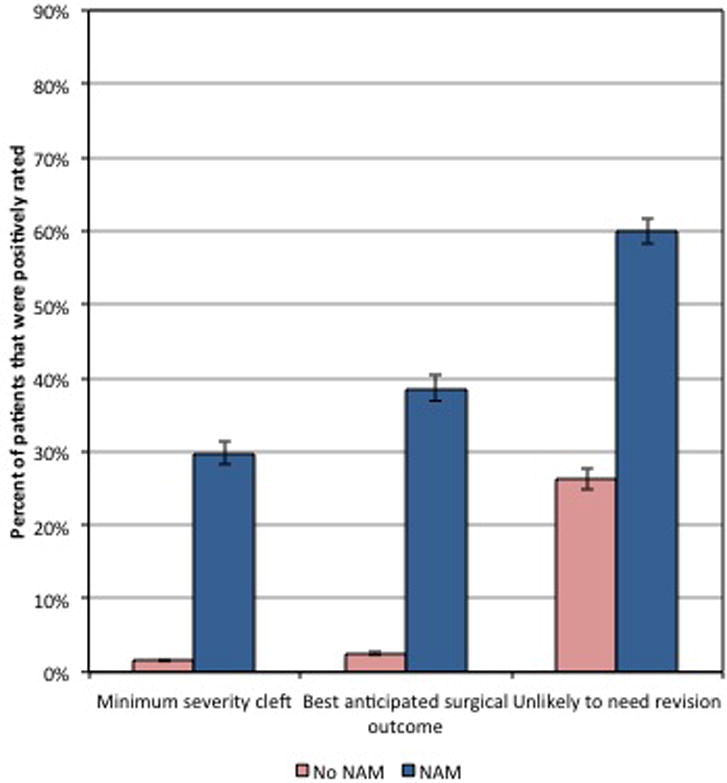
Surgeons’ ratings of cleft severity and anticipated surgical outcomes among bilateral cleft lip and palate patients by nasoalveolar molding preparation group. Estimates and 95% confidence intervals generated from cross-classified multilevel models. Note: All differences between nasoalveolar molding-prepared patient and non-nasoalveolar molding-prepared patient groups are significant (p < 0.001); NAM = nasoalveolar molding.
Discussion
The objective of this study was to test the impact of NAM preparation using a rater-masked quasi-experimental design. Surgeons were asked to rate patients’ presurgical cleft severity and anticipated surgical outcomes. Using cross-classified multilevel logistic regression to account for repeat-testing bias, the results from the surgeons’ ratings reveal a consistent pattern: NAM-prepared patients as having minimal severity clefts, having better anticipated surgical outcomes, and being less likely to need early revision surgery compared to those without NAM preparation. This study lends support to the notion that practicing cleft surgeons view NAM-prepared patients as having less severe clefts preoperatively and better anticipated surgical outcomes than non-NAM-prepared patients.
Estimating the correct results can be difficult with repeating measurement: individuals often respond to questions based on their own degree of optimism and experience. While a number of potential models were examined, CCMLM were chosen because they provided the best-fitting and most robust results. In this study, while we are most confident in the cross-classified results because the model accounts for sample characteristics, we are particularly confident in our findings because all models showed that NAM treatment significantly improves the surgeons’ ratings of patients for the outcomes measured. Surgeons rated NAM-prepared UCLP as minimal severity 53.3% of the time, while only rating non-NAM-prepared UCLP as minimal severity 2.0% of the time, making them approximately (relative risk (RR) = 53.3/2.0 =) 27 times as likely (p-value < 0.001) to rate NAM-prepared ULCP as minimal severity. Results were similarly positive and significant regardless of the measure used; surgeons were 7 times as likely to rate NAM-prepared UCLP patients as among their best surgical outcomes and 1.8 times as likely to say UCLP patients were unlikely to need revision compared to non-NAM-prepared UCLP patients. Analogous trends were evident for patients with BCLP.
This study has several limitations. For example, the response rate to the emailed, web-based survey was low (24%). Historically, clinicians, especially physicians, have been known to be a challenging group to survey19 and recent evidence suggests a decline in physician response rates to surveys.20 To increase sample size, we surveyed the entire population of plastic and oral surgeons belonging to the ACPA, which yielded a substantial sample size (N=176), representing approximately one-quarter of the population.
Also, baseline assessments of NAM- and non-NAM-prepared patients were not available. Such assessments might bias study results if patients who received NAM preparation had less severe pre-treatment clefts than those without NAM preparation. Prior research suggests that patients who receive NAM therapy, on average, tend to have wider pre-treatment clefts than those who do not.14 The lack of data on pre-treatment cleft severity nevertheless represents a major limitation. Future research should include such data.
It is important to note that our analysis is also limited because the outcomes analyzed here represent surgeons’ subjective ratings of anticipated outcomes and not actual outcomes. Surgical outcomes, including the likelihood of revision, are influenced by multiple factors, some of which are not visually evident (e.g., myofibroblast contraction or wound healing characteristics). In general, it makes teleological sense that the degree of preoperative cleft severity would be associated with the long-term surgical outcome as well as the revision rate. Investigating this supposition, Henkel and colleagues found that the incidence of secondary cleft surgery was related to the initial cleft severity.4 Whether one agrees with Henkel and colleagues’ findings, our study suggests that surgeons prefer to operate on NAM-prepared patients.
Irrespective of the impact of NAM on predicted surgical outcomes, NAM therapy has potential limitations including a greater investment of time and resources preoperatively than surgery alone and the potential for caregiver burden. Our analyses suggest that even though NAM increases the preoperative investment, the dividends may pay off in terms of a reduction in the need for secondary surgery. Future analyses should examine the extent to which NAM therapy impacts the overall cost of cleft care in relation both to the higher preoperative investment and the potential savings due to decreased potential need for secondary surgeries. Future research should also investigate caregiver responses to NAM and effect of NAM on family functioning.
Regarding facial appearance and surgical outcomes, the study findings are consistent with previous reports indicating a beneficial role for NAM. Other studies note that NAM may improve long-term nasal symmetry and less need for secondary alveolar bone grafting when gingivoperiosteoplasty is performed.8–13 Our study supports this research by showing that NAM treatment was associated with an improvement in surgeons’ ratings of patients. We found that compared to non-NAM-prepared patients, surgeons were more likely to rate NAM-prepared patients as having minimal severity clefts, and to anticipate that the patients would be among their best surgical outcomes and less likely to need early surgical revision. While further research is needed, insofar as results represent a causal relationship, presurgical NAM preparation may benefit patients, patient families, and surgeons.
Acknowledgments
Part of the project was supported by NIDCR-R21 DE021853, Broder, PI.
Footnotes
A portion of an earlier version of this paper was presented at the 12th International Congress on Cleft Lip/Palate and Related Craniofacial Anomalies. Lake Buena Vista, FL. May 9, 2013.
Conflicts of Interest and Sources of Funding: No authors declared any conflicts of interest. HLB is currently receiving funding from NIDCR-R21 DE021853, Broder, PI. For the remaining authors no sources of funding were declared.
References
- 1.Dec W, Olivera O, Shetye P, et al. Cleft palate midface is both hypoplastic and displaced. J Craniofac Surg. 2013;24:89–93. doi: 10.1097/SCS.0b013e3182646273. [DOI] [PubMed] [Google Scholar]
- 2.Latham RA. Development and structure of the premaxillary deformity in bilateral cleft lip and palate. Br J Plast Surg. 1973;26:1–11. doi: 10.1016/s0007-1226(73)80028-1. [DOI] [PubMed] [Google Scholar]
- 3.Salyer KE, Genecov ER, Genecov DG. Unilateral cleft lip-nose repair: a 33-year experience. J Craniofac Surg. 2003;14:549–558. doi: 10.1097/00001665-200307000-00030. [DOI] [PubMed] [Google Scholar]
- 4.Henkel KO, Gundlach K, Saka B. Incidence of secondary lip surgeries as a function of cleft type and severity: one center’s experience. Cleft Palate Craniofac J. 1998;35:310–312. doi: 10.1597/1545-1569_1998_035_0310_ioslsa_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 5.Grayson BH, Santiago PE, Brecht LE, et al. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. 1999;36:486–498. doi: 10.1597/1545-1569_1999_036_0486_pnmiiw_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 6.Grayson BH, Cutting CB. Presurgical nasoalveolar orthopedic molding in primary correction of the nose, lip, and alveolus of infants born with unilateral and bilateral clefts. Cleft Palate Craniofac J. 2001;38:193–198. doi: 10.1597/1545-1569_2001_038_0193_pnomip_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 7.Grayson BH, Maull D. Nasoalveolar molding for infants born with clefts of the lip, alveolus, and palate. Clin Plast Surg. 2004;31:149–158. vii. doi: 10.1016/S0094-1298(03)00140-8. [DOI] [PubMed] [Google Scholar]
- 8.Santiago PE, Grayson BH, Cutting CB, et al. Reduced need for alveolar bone grafting by presurgical orthopedics and primary gingivoperiosteoplasty. Cleft Palate Craniofac J. 1998;35:77–80. doi: 10.1597/1545-1569_1998_035_0077_rnfabg_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 9.Maull DJ, Grayson BH, Cutting CB, et al. Long-term effects of nasoalveolar molding on three-dimensional nasal shape in unilateral clefts. Cleft Palate Craniofac J. 1999;36:391–397. doi: 10.1597/1545-1569_1999_036_0391_lteonm_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 10.Barillas I, Dec W, Warren SM, et al. Nasoalveolar molding improves long-term nasal symmetry in complete unilateral cleft lip-cleft palate patients. Plast Reconstr Surg. 2009;123:1002–1006. doi: 10.1097/PRS.0b013e318199f46e. [DOI] [PubMed] [Google Scholar]
- 11.Clark SL, Teichgraeber JF, Fleshman RG, et al. Long-term treatment outcome of presurgical nasoalveolar molding in patients with unilateral cleft lip and palate. J Craniofac Surg. 2011;22:333–336. doi: 10.1097/SCS.0b013e318200d874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee CT, Grayson BH, Cutting CB, et al. Prepubertal midface growth in unilateral cleft lip and palate following alveolar molding and gingivoperiosteoplasty. Cleft Palate Craniofac J. 2004;41:375–380. doi: 10.1597/03-037.1. [DOI] [PubMed] [Google Scholar]
- 13.Pfeifer TM, Grayson BH, Cutting CB. Nasoalveolar molding and gingivoperiosteoplasty versus alveolar bone graft: an outcome analysis of costs in the treatment of unilateral cleft alveolus. Cleft Palate Craniofac J. 2002;39:26–29. doi: 10.1597/1545-1569_2002_039_0026_nmagva_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 14.Sischo L, Chan JW, Stein M, et al. Nasoalveolar molding: prevalence of cleft centers offering nam and who seeks it. Cleft Palate Craniofac J. 2012;49:270–275. doi: 10.1597/11-053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luo W, Kwok O-m. The impacts of ignoring a crossed factor in analyzing cross-classified data. Multivariate Behavioral Research. 2009;44:182–212. doi: 10.1080/00273170902794214. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein H. Multilevel Cross-Classified Models. Sociological Methods & Research. 1994;22:364–375. [Google Scholar]
- 17.Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multilevel models in health research. Soc Sci Med. 1998;46:97–117. doi: 10.1016/s0277-9536(97)00148-2. [DOI] [PubMed] [Google Scholar]
- 18.Wagenmakers EJ, Farrell S. AIC model selection using Akaike weights. Pscyhonom Bull Rev. 2004;11:192–196. doi: 10.3758/bf03206482. [DOI] [PubMed] [Google Scholar]
- 19.Klabunde CN, Willis GB, McLeod CC, et al. Improving the Quality of Surveys of Physicians and Medical Groups A Research Agenda. Eval Health Prof. 2012;35:477–506. doi: 10.1177/0163278712458283. [DOI] [PubMed] [Google Scholar]
- 20.McLeod CC, Klabunde CN, Willis GB, et al. Health Care Provider Surveys in the United States, 2000–2010 A Review. Eval Health Prof. 2013;36:106–126. doi: 10.1177/0163278712474001. [DOI] [PubMed] [Google Scholar]


