Abstract
Objective
To describe feasibility, safety, and outcome results from a treatment development trial of the SAFETY Program, a brief intervention designed for integration with emergency services for suicide-attempting youths.
Method
Suicide-attempting youths, ages 11–18, were enrolled in a 12-week trial of the SAFETY Program, a cognitive-behavioral family intervention designed to increase safety and reduce suicide-attempt (SA) risk (N=35). Rooted in a social-ecological cognitive-behavioral model, treatment sessions included individual youth and parent session-components, with different therapists assigned to youths and parents, and family session-components to practice skills identified as critical in the pathway for preventing repeat SAs in individual youths. Outcomes were evaluated at baseline, 3- and 6-month follow-ups.
Results
At the 3-month post-treatment assessment, there were statistically significant improvements on measures of suicidal behavior, hopelessness, youth and parent depression, and youth social adjustment. There was one reported suicide attempt by 3-months and another by 6-months, yielding cumulative attempt rates of 3% and 6% at 3 and 6-months respectively. Treatment satisfaction was high.
Conclusions
Suicide-attempting youths are at high-risk for repeat attempts and continuing mental health problems. Results support the value of a randomized controlled trial to further evaluate the SAFETY intervention. Extension of treatment effects to parent depression and youth social adjustment are consistent with our strong family focus and social-ecological model of behavior-change.
Adolescence is a key period for suicide prevention; rates of suicide deaths and SAs increase during adolescence and suicide is a leading cause of death for adolescents (National Action Alliance, 2014). Despite efforts to develop effective treatments and accumulating treatment research, empirically supported treatments for reducing SA risk in suicidal adolescents remain elusive. While there is increasing literature on broad suicidality outcomes (for review see, Brent et al., 2013; Corcoran et al, 2011; Goldston, et al., 2010; Ougrin et al., 2012), currently there are only four randomized controlled trials (RCTs) with adolescents documenting statistically significant reductions in repeat SAs or self-harm (a broader category including self-harm with and without suicidal intent). Two of these four RCTs included strong emphases on the family/social environment: (1) a small trial (N=40) demonstrating significant reductions in SAs after integrated cognitive-behavior therapy with separate therapists for youths and parents targeting both suicidal behavior and substance use, compared to treatment as usual (TAU) (Esposito-Smythers et al., 2011); and 2) an RCT demonstrating that multisystemic therapy (MST) led to reduced rates of SAs by youth (but not parent-report) among youths presenting to the ED and authorized for psychiatric hospitalization, however, intervention effects were non-significant within the smaller group of youths with suicidality at baseline (Huey, et al., 2005). Third, initial positive results for developmental group therapy, relative to TAU (Wood et al., 2001), failed to replicate in later trials (Green, et al., 2011; Hazell, et al., 2009). A fourth trial indicates reduced self-harm (with and without suicidal intent) following mentalization-based-therapy vs. TAU; however, results for suicide attempts are not reported separately (Rossouw & Fonagy, 2012). As noted above, there are other trials documenting reductions in broader suicidality and self-harm outcomes, but these trials have not reported statistically significant effects on suicide attempts or the broader self-harm category (for reviews, see Brent et al., 2013; Corcoran et al, 2011; Goldston, et al., 2010; Ougrin et al., 2012).
Because of the low rate of SAs, even among high-risk-youths with prior SAs, large samples are required for adequate statistical power to evaluate intervention effects on SA outcomes. This underscores the importance of treatment development research to pre-test promising treatment strategies before launching the large expensive trials required to adequately power analyses of SA outcomes.
The SAFETY Program is a novel 12-week ecological cognitive-behavioral treatment designed to be integrated within emergency services and grounded in social-ecological theory (Henggeler et al., 2002). Consistent with the social-ecological model, the treatment emphasizes enhancing protective supports within social systems (family, peers, community) and includes one therapist for the youth and another focusing on the family/community. Sessions include a first component where youths work with the youth-therapist, while parents work with the parent-therapist, and a second family-component where all come together to practice skills identified as critical in the pathway for preventing repeat SAs.
The SAFETY model addresses previously-identified challenges in novel ways. First, many youths receiving ED-treatment for SAs never attend or receive inadequate doses of follow-up mental health treatment (USDHHS, 2012). Research has shown that enhanced ED-mental health interventions improve rates of outpatient follow-up treatment, relative to ED TAU, but benefits on clinical outcomes have not emerged (Ougrin, et al., 2012), perhaps due to limited effectiveness of community TAU (Asarnow, et al., 2011), underscoring the critical need for effective outpatient treatments. Because treatment adherence is improved with in-home treatment (Harrington, et al., 1998), in-home treatment is used for the first SAFETY-session and as-needed. Our family emphasis also aimed to increase parent motivation and decrease family treatment barriers.
Second, to address heterogeneity/complexity among the diverse group of suicide-attempting youths, SAFETY focuses specifically on decreasing suicidal behavior, a key treatment target regardless of diagnostic presentation. To balance the need for adequate specification of the treatment model with the need to address heterogeneity in pathways to SAs, we adopt the MST-approach of using core principles to guide treatment and design treatment around a cognitive-behavioral fit analysis (CBFA) that specifies key risk and protective processes hypothesized to impact the likelihood of repeat SAs for each youth.
This report describes a phase-1 treatment development trial of the SAFETY Program, emphasizing feasibility, safety, and outcomes. We hypothesized that the SAFETY Program would be associated with reductions in suicidal behavior (primary outcome). Improvements were also predicted on secondary outcomes: youth and parent depression, hopelessness, and social adjustment.
METHODS
All youths gave written informed assent (or consent if ≥ age 18) and parents gave written informed consent in accordance with local IRB regulations. Progress was monitored by the Data and Safety Monitoring Board (DSMB).
Participants
Building on our prior case finding system (Asarnow et al., 2011), study staff informed ED/hospital staff about the study, were on-call to one medical ED, and available to enroll participants in the ED, hospital, or clinic as soon after the SA as possible. To enhance recruitment, we accepted community referrals. Inclusion criteria were: SA within past-3-months (defined as self-injury with some non-zero intent to die); age 11–18 years; stable living situation/no immediate plans for out-of-home placement. Exclusion criteria were: no contact information available for follow-up; psychosis; substance abuse/dependence; or other factors that would impede participation in assessments and/or intervention (not English-speaking; no family to participate). Towards the end of the trial, we included two Spanish-speaking families and bilingual therapists.
SAFETY Program
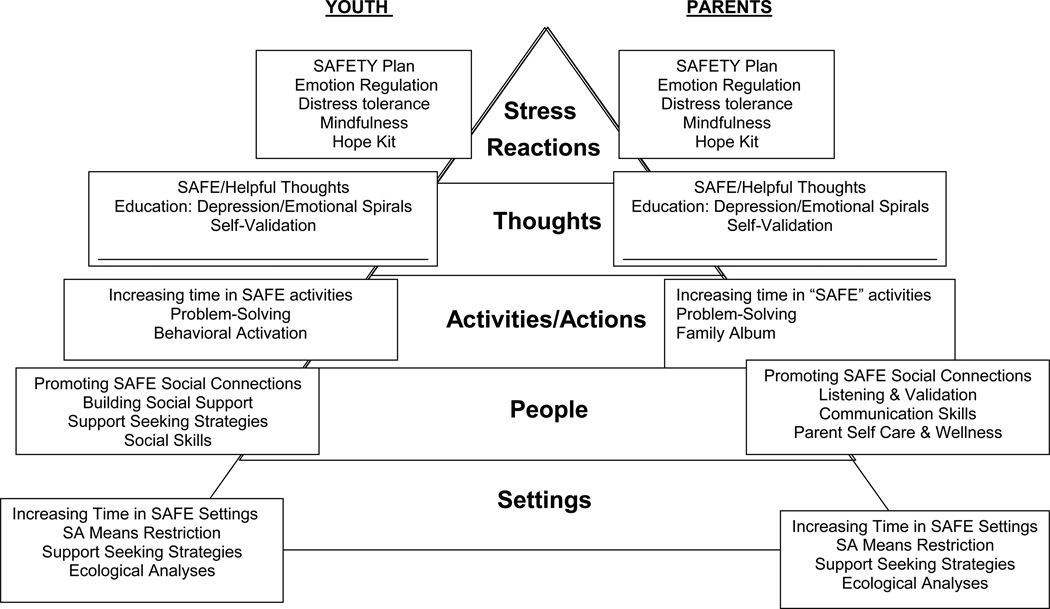
The “SAFETY Program” stands for Safe Alternatives for Teens & Youths, with the name intended as a reminder that the program focused on enhancing SAFETY. Treatment was structured using the SAFETY Pyramid (Figure 1), which describes treatment targets and modules addressing each pyramid-level for youths and parents. This pyramid emphasized: 1) grounding in the principle of SAFE SETTINGS-achieved through restricting access to dangerous SA methods and increasing time in safe settings; 2) promoting interactions with SAFE PEOPLE- strengthening listening, validation, and self-care in parents to increase the likelihood that their children would turn to them instead of suicidal behavior, and enhancing SAFE social connections; 3) encouraging SAFE ACTIVITIES AND ACTIONS; 4) SAFE THOUGHT patterns, that reversed escalating downward SA-triggering spirals; 5) SAFE STRESS REACTIONS, strengthening safe emotion regulation and distress tolerance vs. suicidal behavior.
Figure 1.
SAFETY Pyramid: Conceptual Model and youth and parent intervention modules and foci.
©Joan R. Asarnow
Core principles guide the assessment and treatment process; the intervention uses a standard structure with three phases addressing distinct goals (TABLE 1). Sessions include both required and individually-selected components.
Table 1.
Overview of SAFETY Program: Principles & Sessions
| A. SAFETY Program Principles* | |
| 1. The primary aim of treatment is to enhance SAFETY and reduce suicide attempt risk | |
| 2. Interventions are designed to promote SAFE vs. UNSAFE: settings/environments, social connections, actions/activities, thoughts, and stress reactions. (See SAFETY Pyramid). | |
| 3. The primary aim of assessment is to understand the “cognitive-behavioral fit” between suicide attempts, their broader environmental context, and cognitive-behavioral processes; assessment aims to identify a) cognitive-behavioral and social-environmental processes that increase risk for suicide attempts, and b) protective processes that can reduce risk of repeat SAs for individual youths and families. | |
| 4. Assessment is continuous, linked with treatment, and used to refine the cognitive-behavioral fit analysis and treatment plan. | |
| 5. Treatment interventions build on strengths in the youth, family, and environment as levers of change. | |
| 6. Interventions are patient and family-centered and collaborative. | |
| 7. Interventions focus on the present, requiring consistent effort by the youth and parents/caregivers. | |
| 8. Generalization and persistence of treatment effects are considered from the start; the role of parents/caregivers in nurturing, protecting, and addressing youths’ needs across multiple social contexts is emphasized. | |
| 9. Interventions are developmentally appropriate, culturally sensitive, and fit the developmental needs and cultural context of the youth and family. | |
| 10. Outcomes are evaluated continuously from multiple perspectives (e.g. youth, family, clinician) and used to inform treatment; therapists are accountable for overcoming barriers to successful outcomes. | |
| B. Structure, Objectives, Focus of Treatment Sessions** | |
| Session/Week | Major Objectives and Focus |
| Phase 1 | Establishing safety, development of cognitive-behavioral fit analysis, and treatment plan |
| Session 1 | In home. Initial cognitive-behavioral fit analysis (CBFA) of suicidal behavior, build protective support and monitoring in the home, restrict access to potentially lethal methods, develop and practice initial SAFETY plan, gain commitment to treatment. |
| Session 2 | Expand CBFA to explain how suicidal behavior “fits” within multiple systems (families, peers, school, community) through an ecological analysis identifying risk and protective factors to be targeted through treatment plan, Review and update SAFETY plan |
| Session 3 | Collaborate with youth and family to develop the initial treatment plan and targets, considering all levels of the SAFETY Pyramid. The treatment plan specifies treatment targets which are linked to treatment modules. |
| Phase 2. | Implement treatment plan |
| Session 4 - Wk 9 | Implement treatment plan, refine as new information is acquired and the CBFA clarified. Monitor youth and family response and revise treatment plan as appropriate. As in DBT, session priorities based on an hierarchy of treatment targets: safety issues take priority when self-harm behavior or urges reported; followed by issues that threaten treatment adherence; and other CBFA targets. |
| Phase 3 | Consolidate gains, relapse prevention, link to follow-up care, termination |
| Wk 10–12 | Consolidate gains, relapse prevention, termination, link to follow-up care as indicated. Final session is standard across participants, emphasizes relapse prevention and linkage to follow-up care and other needed services. |
Adapted from Multisystemic Therapy (MST). Henggeler et al.2002.
Frequency and timing of sessions adjusted to meet youth and family needs.
©Joan R. Asarnow
Phase-1: establishing safety and treatment planning
Session-1 had a standard structure and was conducted in the home unless families refused. Modeled after our ED crisis-therapy session (Asarnow, et al., 2009; Rotheram-Borus, et al., 2000) this session included: 1) psychoeducation emphasizing the importance of restricting access to dangerous SA methods, protective monitoring, and commitment to treatment; 2) working with youths and parents to identify youth and family strengths; 3) an “emotional thermometer” task to develop an hierarchy of potential SA-triggering situations and associated youth emotional, physiological, cognitive, and behavioral reactions; 4) developing and practice using a “safety plan” for reducing “emotional temperature” and SA-risk; 5) generating a “Safety Plan Card”, given to youths. Therapists worked with youths to obtain a commitment to use the SAFETY Plan instead of suicidal behavior.
To reduce access to dangerous SA means, a risk factor for suicide deaths (National Action Alliance, 2014), therapists brought a lock box to the session, supported youths and parents in removing potentially dangerous SA-methods (e.g., medications), and looking at youth’s room/living situation (e.g. meeting family pet). Youths were introduced to a mood monitoring form with sections for monitoring suicidal/self-harm thoughts and behavior, to be used in safety checks, and assigned as homework (referred to as “practice”). Sessions included a “thanks note” exercise designed to enhance protective family support, in which family members gave each other short notes sharing something they appreciated about the other person’s actions (e.g. “thanks for sitting with me). Thanks notes were assigned as family “practice.”
The next two sessions emphasized development of a CBFA, which identified the chain of triggering-events, cognitive-behavioral, emotional, and environmental processes leading to SAs, protective processes that could prevent repeat SAs, and considered youth suicidal behavior within broad social systems (Table 1). The CBFA was developed, from the youth and parent perspectives with their therapists during individual sessions. Based on the CBFA and structured using the SAFETY Pyramid (FIGURE 1), treatment plans were reviewed with youths and parents in collaborative patient-centered treatment planning, provided a working treatment conceptualization, and refined throughout treatment. Before sessions therapists met to share information, review clinical dashboards illustrating youth response by treatment modules across sessions (Chorpita, et al., 2008), and reach consensus on the CBFA and treatment targets.
After Session-1, sessions began with simultaneous individual youth and parent session-components. The structure for individual session-components included: agenda-setting; bridging to prior session, review of practices, safety check; work on session-specific skill or topic; address issues identified by youths/parents; updating of SAFETY Plan incorporating session content; and assigning practices. To promote generalization and provide practice using “safe” behaviors in a “family context”, sessions concluded with a family session-component, including: 1) “thanks notes;” 2) practice review; 3) capsule summaries where youths and parents shared what they worked on during individual sessions; 4) work on skill/problem-area; and 5) assigning family-practice. Practices were standard and included: the mood/self-harm monitoring exercise for youths; family “thanks notes;” and optional other practices.
Phase-2: skill-building based on CBFA (FIGURE 1)
Frequently used skills for youths included: developing a “Hope Box” with reminders of reasons for living and cues for “safe” coping, behavioral activation, thoughts, problem-solving, emotion regulation, distress tolerance, understanding depression/emotional spirals. For parents common topics were: parent safety plan; active listening and validation; parent self-care/wellness; communication; problem-solving; understanding depression/emotional spirals; and creating a family album, which was shared with youths to promote feelings of belonging and healthy connections. The sequencing of skills and topics was determined by the CBFA and an hierarchy of session priorities. Like Dialectical Behavior Therapy (Miller, Rathus, Linehan, 2007), safety issues took priority if self-harm behavior or urges were present, followed by issues threatening treatment adherence, and other CBFA targets.
Phase-3: skill consolidation, relapse prevention, termination
Phase-3 emphasized identifying skills that were most helpful for promoting safety, development and guided practice of a relapse-prevention plan, and processing of emotions/reactions to treatment and termination. A care linkage plan connected youths to services if desired and indicated, always including linkage to primary care because of relatively universal access to primary care for children in California.
Therapist Training & Treatment Adherence
Therapists were trained through manual review, guided practice, with treatment adherence checks and feedback from the principal investigator. Therapists had mental health training with a masters or PhD in psychology or social work. Because this was a treatment development trial rooted in CBT and social-ecological multi-systemic theory, we rated a large proportion (65%) of randomly selected sessions for treatment adherence using: The Cognitive Therapy Rating Scale (CTRS), which indicated strong adherence to CBT principles- 99% of sessions exceeded the CTRS adherence score of 40 (Brent, et al., 2009); mean 50.83, SD 8.59); and the MST Therapist Adherence Measure-Revised (Henggeler et al., 2002), which indicated strong use of MST principles, Mean= 4.35, SD = .28, range 0–5.
Assessment
Assessments included brief screening-assessments(Asarnow, et al., 2011), more extensive baseline-assessments after ED-discharge, 3-month post-treatment assessments, and brief parent phone-interviews at 6-months. Assessment-staff were blinded to study design and treatment condition.
Measures: Baseline, 3-Months
Current mood disorders and suicidal behaviors were assessed using the depression module from the Diagnostic Interview Schedule for Children & Adolescents (NIMH DISC IV), a structured computer-assisted diagnostic interview designed for lay-interviewer administration (Shaffer et al., 2000). Timing, method, and lethality of suicidal/self-harm behavior was coded using the Columbia Suicide History Form (Brent, et al., 2009) adapted to include NSSI items. Using previously developed quality assurance (QA) procedures (Asarnow et al., 2011), 20% of randomly selected interviews were rated for accuracy in presenting questions, probing, and coding. Ratings indicated strong quality (Mean =1.2, SD=0.54, 3-point scale 1=good to 3=poor). Self-report on the 17-item Harkavy Asnis Suicide Survey (HASS) (Harkavy-Friedman, 1989) yielded scales for: Active Suicidal Behavior and Ideation (ASBI), Passive Suicidal Ideation (PSI), a SA Behavior subscale (from the ASBI Scale) including 2-items assessing SA behavior (tried to kill yourself; started to do it, then stopped at the last minute) (Asarnow et al., 2012). Youth and parent depressive symptoms were assessed using the Center for Epidemiological Studies- Depression Scale (CES-D, Radloff, 1977). The 20-item Beck Hopelessness Scale (BHS) assessed hopelessness (Beck et al., 1974). The Social Adjustment Scale-Self Report for Youth (SAS-SR, Weissman, Orvaschel, Padian, 1980) assessed 4 areas/subscales: school-adjustment, peer-adjustment, family-adjustment, spare-time. Due to summertime-assessments and expected missing data for the school-scale, the Total SAS-SR excluded the school subscale. We used a Treatment Satisfaction Scale, sensitive to intervention effects in prior research (Asarnow, et al., 2005). The Service Assessment for Children and Adolescents (SACA), adapted for the ED-population (Asarnow, et al., 2011), assessed service use. Demographic variables (age, gender, race, ethnicity) were assessed by parent and youth report. Youth self-report on the Drug Use Screening Inventory (DUSI) measured substance use/abuse (Kirisci, Mezzich, & Tarter, 1995). Parent report on the Child Behavior Checklist (CBCL) assessed broader youth externalizing and internalizing symptoms (Achenbach, 1991).
6-Month Follow-Up
These parent telephone-interviews included the DISC suicidal ideation and attempt items, and SACA questions assessing ER visits, hospitalizations, and residential placements.
Statistical Analysis
This trial evaluated treatment feasibility, safety, and explored initial treatment effects, recognizing the need for caution in considering effect sizes from small treatment development studies (Kraemer, et al., 2006). We report standard descriptive statistics and estimate intervention parameters (e.g. attrition, effect sizes) (Cohen, 1988; Kraemer, et al., 2006). Treatment effects are reported based on repeated measures t-tests. Effect sizes are reported using Cohen’s d, calculated as the standardized difference of the means at each time point, with standardization based on the pooled estimate of variance; thresholds for small, medium, and large effects are 0.30, 0.50, and 0.80 respectively (Cohen, 1988). Primary analyses reported here use all available information. As a sensitivity analysis, we used last observation carried forward, a conservative approach for intent to treat analyses when there are missing follow-up data. These analyses yielded very similar results to the primary analyses, with no substantive change in conclusions; although expected attenuation in effect sizes were observed and noted when interpretation differed from primary analyses. Analyses were conducted using SPSS, version 22.
RESULTS
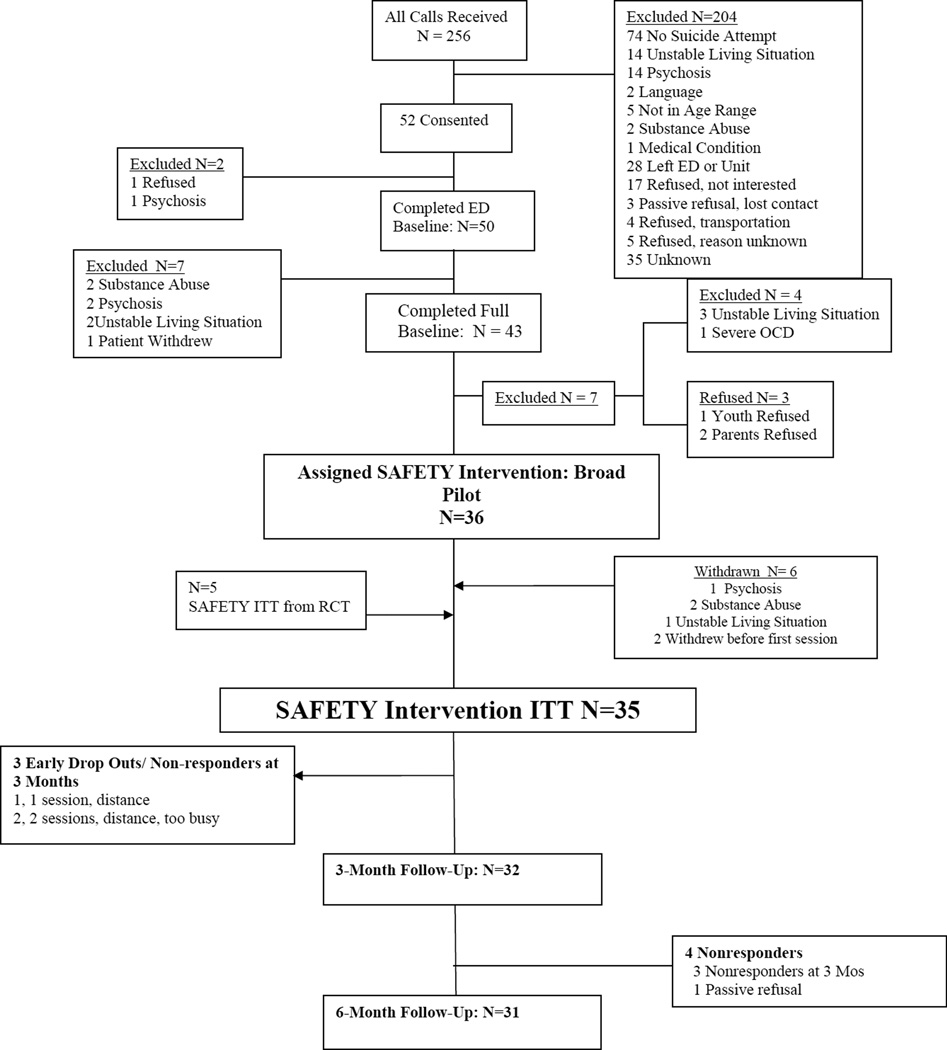
Figure 2 presents participant flow for the SAFETY trial. The final sample included 35 youths: 30 from the open trial recruited during 33 months between March 2006 and November 2010; and 5 drawn from the SAFETY condition of a small Phase-2 pre-test of procedures for an RCT, recruited between Dec 2010 and September 2012. Outcome data were available for 32 (91%) and 31 (89%) youths at 3- and 6-months respectively. Baseline assessments occurred at a mean of 6.86 days (SD = 9.59 days) post-emergency treatment; 3 and 6-month assessments occurred at a mean of 108.66 days/3.6 months (SD=18.75 days) and 208.59 days/6.9 months (SD=28.43 days) from baseline respectively.
Figure 2.
Participant flow through the SAFETY Trial.
The sample was predominantly female, had a mean age of 14.89 years (SD =1.60), was about 60% minority, 97% received ED-treatment (the other received treatment in a non-ED setting), and 86% were hospitalized (TABLE 2). At baseline, 46% of youths reported multiple lifetime suicide attempts, 57% reported NSSI, 40% had past-year major depressive disorder (MDD), 62.5% met DISC criteria for either MDD or intermediate MDD (subsyndromal but significant symptoms); 50% reported current severe depressive symptoms (CES-D ≥ 24); and substance misuse, externalizing, and internalizing symptoms were common.
Table 2.
Description of sample enrolled in SAFETY treatment development trial (N=35).
| Mean or Frequency | SD or % | |
|---|---|---|
| Age, in years | 14.89 | 1.60 |
| Gender) | ||
| Male | 5 | 14% |
| Female | 30 | 86% |
| Race, % (N)* | ||
| White | 14 | 40% |
| Hispanic | 12 | 34% |
| African American | 4 | 11% |
| Asian-Other | 5 | 14% |
| Emergency Department Visit for Suicidal Behavior | 34 | 97% |
| Inpatient Hospitalization | 30 | 86% |
| Number of Lifetime Suicide
Attempts 1 2 3 4 5 |
19 6 6 1 3 |
54% 17% 17% 3% 9% |
| Nonsuicidal Self-Injurious Behavior (NSSI) | 20 | 57% |
| Youth, Major Depressive Disorder (MDD, DISC) Total MDD + Intermediate MDD |
16 25 |
40 % 63 % |
| Severe Depressive Symptoms, CES-D ≥ 24 | 20 | 50 % |
| DUSI, Problematic Substance Use | 20 | 57% |
| CBCL Externalizing, Clinical Range | 12 | 34% |
| CBCL Internalizing, Clinical Range | 16 | 46% |
| CBCL Total Problem Behavior, Clinical Range | 18 | 51% |
Note: NSSI= Nonsuicidal Self-Injury, MDD=Major Depressive Disorder, DISC=Diagnostic Interview Schedule for Children, CES-D=Center for Epidemiological Studies-Depression Scale, DUSI=Drug Use Screening Inventory, problematic use defined as endorsed some substance use related impairment, CBCL=Child Behavior Checklist
Treatment Received
Youths received a mean of 10.14 sessions, SD= 4.63, median 11, range 1–20. Most youths (57%) received 9–13 sessions, rates for youth, parent, and family session-components were similar (TABLE 3).
Table 3.
Distribution of total number of sessions and youth, parent, and family session- components.
| Total Sessions | Youth | Parent | Family | |
|---|---|---|---|---|
| Number of Sessions, Mean (SD) | 10.14 (4.63) | 9.46 (4.57) | 8.74 (4.34) | 9.23 (4.21) |
| Range | 1–20 | 0–16 | 0–15 | 1–16 |
| 0–5 Sessions, f (%) | 6 (17%) | 7 (20%) | 8 (23%) | 6 (17%) |
| 6–8 Sessions, f (%) | 2 (6%) | 2 (6%) | 5 (14%) | 5 (14%) |
| 9–11 Sessions, f (%) | 11 (31%) | 11 (31%) | 12 (34%) | 12 (34%) |
| 12–14 Sessions, f (%) | 12 (35%) | 12 (34%) | 8 (23%) | 10 (29%) |
| 15–20 Sessions, f (%) | 45 (12%) | 3 (9%) | 2 (6%) | 2 (6%) |
Note: f=Frequency
SA/Self-Harm Outcomes
Based on youth-report, there was one SA at the 3-month follow-up point (3.1% of sample), confirmed by parent report. This attempt occurred at week-14 from hospital discharge by asphyxiation. There was no injury/lethality. After a 4-day hospitalization, the youth continued in the trial with no additional SAs. An interrupted attempt occurred in another youth at week-15, where the youth grabbed a knife in front of her parents stating that she wanted to kill herself; parents took the knife preventing any self-harm. This family had discontinued treatment at week-11, after only 7 sessions. By 6-months, another youth made an SA by overdose. This occurred during week-20 of the trial, and resulted in an ED visit, psychiatric hospitalization, and placement in residential treatment.
Parents described SAs in two other youths; these youths described the same events as NSSI (cutting) with the intention of relieving distress and no intent to die.
At 3-month follow-up, statistically significant declines were seen on all of the HASS suicidality indicators: SA Scale, SA-item, ASBI Scale, PSI Scale, and Total HASS Scale (Table 4). Effect sizes for the SA and ASBI scales were medium, and smaller for scales with more passive suicidal ideation items (PSI and Total scales).
Table 4.
Outcome results for the SAFETY Treatment Development Trial
| Baseline Mean(SD) |
Follow-Up Mean (SD) |
Paired Difference Mean (SD) |
95%
Confidence Interval |
t-value | p-value | Cohen’s d | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| HASS –SA Scale | 0.89 (1.86) | 0.13 (0.34) | .87 (1.96) | .15 | 1.59 | 2.42 | .019 | .64 |
| HASS-ASBI | 3.71 (4.42) | 1.81 (2.69) | 2.16 (4.58) | .48 | 3.84 | 2.63 | .013 | .59 |
| HASS-PSI | 12.69 (9.79) | 9.19 (10.14) | 3.87 (8.41) | .79 | 6.96 | 2.56 | .016 | .39 |
| HASS-TOTAL | 16.40 (13.52) | 11.04 (12.05) | 5.99 (12.34) | 1.46 | 10.52 | 2.70 | .011 | .46 |
| CES-D, Mean ± SD | 24.54 (12.33) | 13.69 (9.83) | 9.86 (12.13) | 5.41 | 14.31 | 4.53 | .001 | .91 |
| Hopelessness (BHS) | 8.86 (5.70) | 3.94 (3.79) | 4.85 (4.84) | 3.08 | 6.63 | 5.58 | .001 | 1.01 |
| SAS Total | 41.96 (7.07) | 32.53 (7.26) | 9.02 (8.06) | 6.01 | 12.03 | 6.13 | .001 | 1.27 |
| SAS School | 13.90 (4.94) | 10.37 (3.57) | 3.39 (4.50) | 1.40 | 5.39 | 3.53 | .002 | .90 |
| SAS Peer | 17.26 (4.60) | 12.78 (3.54) | 4.48 (4.65) | 2.77 | 6.18 | 5.36 | .001 | 1.11 |
| SAS Family | 14.02 (3.61) | 11.45 (3.83) | 2.33 (4.57) | .63 | 4.04 | 2.79 | .009 | .66 |
| SAS Spare Time | 5.15 (1.76) | 4.58 (1.57) | .84 (1.70) | .22 | 1.46 | 2.76 | .01 | .52 |
| Parent CES-D | 20.26 (13.34) | 10.86 (8.55) | 7.64 (12.07) | 3.13 | 12.15 | 3.47 | .002 | .71 |
Note. HASS=Harkavy Asnis Suicide Survey, SA=Suicide Attempt; ASBI=Active Suicidal Behavior & Ideation, PSI=Passive Suicidal Ideation, CES-D=Center for Epidemiological Studies-Depression Scale, BHS=Beck Hopelessness Scale, SAS=Social Adjustment Scale (Higher scores reflect > impairment).
Preliminary analyses indicated nonsignificant effects for age and gender, with the exception of a significant age-effect on SAS-Sparetime. Sensitivity analyses controlling for age, yielded similar results: Spare Time t= 2.20, p<. 03, Cohen’s d=.52.
Other Outcomes
Statistically significant improvements were observed on youth hopelessness, youth and parent depressive symptoms (CES-D), and all of the SAS scales (TABLE 4). Effect sizes were large for depression, hopelessness, and SAS scales, with the exception of medium effect sizes for parent-depression, family-adjustment, and spare-time scales. In sensitivity analyses using last observation carried forward, the effect size shifted from large to small for two variables- youth CES-D, School Adjustment; and from medium to small for Spare-time.
NSSI outcomes were explored using youth self-report (substituting parent-report for one non-participating youth). At follow-up, NSSI was reported for 10/32 youths (31.3% of sample) vs. 20/35 youths at baseline (57.1 % of sample). Effect size for this dichotomous variable was estimated using Cohen’s w (Cohen, 1988), Cohen’s w=.38, and is considered a medium effect size using the standard interpretations (Cohen, 1988).
Services Use and Patient Satisfaction
Four youths (12.5% of the sample) were seen in the ED and/or hospitalized during the 3-month follow-up period due to suicidality/self-harm: the youth reporting an SA was seen in the ED and hospitalized; 2 youths were seen in the ED for suicidal ideation and hospitalized; another youth was hospitalized for suicidal ideation. Satisfaction with the SAFETY intervention was high. Mean satisfaction ratings were 4.07 (SD=1.11) and 4.1 (SD=0.79) for parents and youths respectively, on a scale of 1 to 5 (5= very satisfied).
Discussion
Results from this Phase-1 trial support feasibility, safety, and suggest treatment benefits. Youths receiving the SAFETY treatment showed statistically significant improvements in SA behavior, depression, hopelessness, suicidal ideation, and social adjustment. Their parents showed statistically significant declines in depressive symptoms. Treatment satisfaction was high in youths and parents. The observed SA rate (3% at 3-months, increasing to 6% by 6-months) is somewhat lower than those in the literature, ranging from 10–43% over 6-months (Ougrin, et al., 2012). Collectively, these data support the value of an RCT to further evaluate efficacy and effectiveness.
The SAFETY intervention emphasizes safety planning, restricting access to dangerous SA methods, and allows for matching treatment dose to individual needs. In contrast to the TASA study where 40% of suicidal events occurred within 4 weeks of intake (Brent, et al., 2009), the SA occurring during the SAFETY treatment occurred towards the end of treatment. This pattern is consistent with the suggestion that an emphasis on safety and increased therapeutic contact early in treatment may prevent early repeat SAs (Brent, et al., 2009).
Consistent with our social-ecological model and family emphasis, results indicating statistically significant improvements in parent depression and youth social adjustment after SAFETY treatment, indicate extension of treatment effects into youths’ social environments. The SAFETY treatment provided parents with their own therapists to address their individual needs and included family session-components to practice “safe coping/support.” This may have increased parents’ feelings of validation and enhanced their skills for coping with stress in themselves and their children, which in turn may have affected parent depression levels. Our results in conjunction with findings from RCTs indicating that interventions including family components (I-CBT, MST) had the strongest effects on SA outcomes, results from other trials testing family-focused interventions on suicidality and self-harm outcomes (Brent et al., 2013), and data pointing to improvements in family functioning as a mediator of decreasing adolescent suicidality (Pineda & Dadds, 2013), suggest that family and environmental intervention may be particularly critical for preventing SAs in youths.
This treatment development trial offered many lessons. First, expanding the target population to a broader population will be important for more feasible service-delivery programs. In this Phase-1 trial, we restricted sample heterogeneity and targeted youths with SAs, yet many youths seen in EDs present with severe suicidal ideation and/or NSSI, both of which predict later SAs (Brent et al., 2013). Second, although participation rates were similar to that for our prior ED study (Asarnow et al., 2011), restricting the target population to SAs in this study yielded slower recruitment, limiting feasibility from a service delivery perspective. Finally, a substantial number of youths were excluded for psychosis and substance abuse (n=24). Targeting the program for a broader population could be achieved using algorithms to match youths to intervention strategies/modules most appropriate for their clinical presentations and likely treatment adherence patterns (Asarnow, et al., 2005; Chorpita, et al., 2008). Using two therapists created challenges, increased initial costs, but may have reduced treatment duration and later costs by intensifying treatment after the SA.
Study limitations include the nonrandomized design and small sample size. The study design and sample size precluded analysis of moderators of treatment effects. The follow-up period was brief and 6-month assessment limited to parent-report; expanded follow-up would have added information. Consistent with the finding of higher SA rates in females, the sample was 86% female. Special outreach may be needed to reach males, who have the highest risk of death. Results may not generalize to excluded subgroups (e.g., youths with substance abuse, psychosis). Evaluation of intervention costs, exportability, and moderators and mediators of treatment effects are issues for future research. Adherence ratings were designed to capture CBT and MST components of the treatment; future work is needed to develop training and quality assurance protocols to optimize therapist competence, treatment fidelity and adherence, and patient outcomes.
In conclusion, the present results provide Phase I support for the safety, feasibility, and benefits of the SAFETY intervention. Results support the need for a larger RCT to further evaluate efficacy and effectiveness.
Acknowledgments
Research reported in this publication was supported by grants from the American Foundation for Suicide Prevention and the National Institute of Mental Health, R34 MH078082. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank the youths, families, staff, and colleagues who made this project possible, including Stanley Huey PhD who consulted on the treatment development and Donald Guthrie PhD, Gabrielle Carlson MD, and Mark Rappaport MD who served on our Data Safety & Management Board.
Contributor Information
Joan Rosenbaum Asarnow, Email: jasarnow@mednet.ucla.edu, University of California, Los Angeles, Department of Psychiatry, Los Angeles, CA.
Michele Berk, Email: micheleberk@gmail.com, Harbor-UCLA Medical Center/Los Angeles Biomedical Research Institute, Los Angeles, CA.
Jennifer L. Hughes, Email: jlhughes@mednet.ucla.edu, University of California, Los Angeles, Department of Psychiatry, Los Angeles, CA.
Nicholas L. Anderson, Email: nlanderson@mednet.ucla.edu, University of California, Los Angeles, Department of Psychiatry, Los Angeles, CA.
REFERENCES
- Achenbach TM. Manual for the Child Behavior Checklist. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- Asarnow J, Baraff LJ, Berk M, Grob CS, Devich-Navarro M, Suddath R, et al. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatr Serv. 2011;62(11):1303–1309. doi: 10.1176/appi.ps.62.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow J, Berk M, Baraff LJ. Family intervention for suicide prevention: A specialized emergency department intervention for suicidal youth. Professional Psychology: Research and Practice. 2009;40(2):118–125. [Google Scholar]
- Asarnow J, Jaycox LH, Duan N, LaBorde AP, Rea MM, Murray P, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. JAMA. 2005;293(3):311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]
- Asarnow J, McArthur D, Hughes J, Barbery V, Berk M. Suicide attempt risk in youths: utility of the Harkavy-Asnis suicide scale for monitoring risk levels. Suicide Life Threat Behav. 2012;42(6):684–698. doi: 10.1111/j.1943-278X.2012.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42(6):861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Brent D, Greenhill LL, Compton S, Emslie G, Wells K, Walkup JT, et al. The Treatment of Adolescent Suicide Attempters study (TASA): predictors of suicidal events in an open treatment trial. J Am Acad Child Adolesc Psychiatry. 2009;48(10):987–996. doi: 10.1097/CHI.0b013e3181b5dbe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, Douaihy AB. Protecting adolescents from self-harm: a critical review of intervention studies. J Am Acad Child Adolesc Psychiatry. 2013;52(12):1260–1271. doi: 10.1016/j.jaac.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Bernstein A, Daleiden EL. Driving with roadmaps and dashboards: using information resources to structure the decision models in service organizations. Adm Policy Ment Health. 2008;35(1–2):114–123. doi: 10.1007/s10488-007-0151-x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Corcoran J, Dattalo P, Crowley M, Brown E, Grindle L. A systematic review of psychosocial interventions for suicidal adolescents. Children and Youth Services Review. 2011;33(11):2112–2118. [Google Scholar]
- Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: a randomized trial. J Consult Clin Psychol. 2011;79(6):728–739. doi: 10.1037/a0026074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB, Walrath CM, McKeon R, Puddy RW, Lubell KM, Potter LB, et al. The Garrett Lee Smith memorial suicide prevention program. Suicide Life Threat Behav. 2010;40(3):245–256. doi: 10.1521/suli.2010.40.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J, Wood AJ, Kerfoot MJ, Trainor G, Roberts C, Rothwell J, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ. 2011;342:d682. doi: 10.1136/bmj.d682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkavy Friedman JMA, G M. Assessment of suicidal behavior: A new instrument. Psychiatric Annals. 1989;19(7):382–387. [Google Scholar]
- Harrington R, Kerfoot M, Dyer E, McNiven F, Gill J, Harrington V, et al. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry. 1998;37(5):512–518. [PubMed] [Google Scholar]
- Hazell P, Martin G, McGill K, Kay T, Wood A, Trainor G, et al. Group therapy for repeated deliberate self-harm in adolescents: failure of replication of a randomized trial. J Am Acad Child Adolesc Psychiatry. 2009;48(6):662–670. doi: 10.1097/CHI.0b013e3181aOacec. [DOI] [PubMed] [Google Scholar]
- Henggeler S, Schoenwald SK, Rowland MD, Cunningham PB. Serious Emotional Disturbance in Children and Adolescents: Multisystemic Therapy. New York: Guilford Press; 2002. [Google Scholar]
- Huey SJ, Henggeler SW, Rowland MD, Halliday-Boykins CA, Cunningham PB, Pickrel SG. Predictors of treatment response for suicidal youth referred for emergency psychiatric hospitalization. J Clin Child Adolesc Psychol. 2005;34(3):582–589. doi: 10.1207/s15374424jccp3403_13. [DOI] [PubMed] [Google Scholar]
- Kirisci L, Mezzich A, Tarter R. Norms and sensitivity of the adolescent version of the drug use screening inventory. Addict Behav. 1995;20(2):149–157. doi: 10.1016/0306-4603(94)00058-1. [DOI] [PubMed] [Google Scholar]
- Kraemer H, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- Miller A, Rathus J, Linehan M. Dialectical Behavior Therapy with Suicidal Adolescents. New York: Guilford Press; 2007. [Google Scholar]
- National Action Alliance for Suicide Prevention: Research Prioritization Task Force. A prioritized research agenda for suicide prevention: An action plan to save lives. 2014 [Google Scholar]
- Ougrin D, Tranah T, Leigh E, Taylor L, Asarnow JR. Practitioner review: Self-harm in adolescents. J Child Psychol Psychiatry. 2012;53(4):337–350. doi: 10.1111/j.1469-7610.2012.02525.x. [DOI] [PubMed] [Google Scholar]
- Pineda J, Dadds MR. Family intervention for adolescents with suicidal behavior: A randomized controlled trial and mediation analysis. J Am Acad Child Adolesc Psychiatry. 2013;52(8):851–862. doi: 10.1016/j.jaac.2013.05.015. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurment. 1977;1(3):385–401. [Google Scholar]
- Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlledtrial. J Am Acad Child Adolesc Psychiatry. 2012;51(12):1304–1313. doi: 10.1016/j.jaac.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Piacentini J, Cantwell C, Belin TR, Song J. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. J Consult Clin Psychol. 2000;68(6):1081–1093. doi: 10.1037//0022-006x.68.6.1081. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) National Strategy for Suicide Prevention: Goals and Objectives for Action. 2012 [PubMed] [Google Scholar]
- Weissman M, Orvaschel H, Padian N. Children's symptom and social functioning self-report scales. J Nerv Ment Dis. 1980;168(12):736–740. doi: 10.1097/00005053-198012000-00005. [DOI] [PubMed] [Google Scholar]
- Wood A, Trainor G, Rothwell J, Moore A, Harrington R. Randomized trial of group therapy for repeated deliberate self-harm in adolescents. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1246–1253. doi: 10.1097/00004583-200111000-00003. [DOI] [PubMed] [Google Scholar]