Abstract
Background
Major depressive disorder (MDD) that onsets by adolescence is associated with various deficits in psychosocial functioning. However, adolescent-onset MDD often follows a recurrent course, which may drive its associated impairment.
Methods
To tease apart these two clinical features, we examined the relative associations of age of onset (adolescent versus adult) and course (recurrent versus single episodes) of MDD with a broad range of psychosocial functioning outcomes assessed in early adulthood. Participants comprised a large, population-based sample of male and female twins from the Minnesota Twin Family Study (N = 1,252) assessed prospectively from ages 17 to 29.
Results
A recurrent course of MDD predicted impairment in a number of psychosocial domains in adulthood, regardless of whether it onset in adolescence or adulthood. In contrast, adolescent-onset MDD showed less evidence of impairment in adulthood after accounting for recurrence. Individuals with both an adolescent onset and recurrent episodes of MDD represented a particularly severe group with pervasive psychosocial impairment in adulthood.
Conclusions
The negative implications of adolescent-onset MDD for psychosocial functioning in adulthood appear to be due primarily to its frequently recurrent course, rather than its early onset, per se. Results highlight the importance of considering both age of onset and course for understanding MDD and its implications for functioning, as well as in guiding targeted intervention efforts.
Keywords: Major depressive disorder, psychosocial functioning, age of onset, adolescence, recurrence
Many cases of major depressive disorder (MDD) onset prior to and during adolescence (Costello et al., 2003, Kessler et al., 2005). Point prevalence estimates of MDD are low in childhood (1% to 3%; Costello et al., 2006), but by adolescence rates are comparable to those found in adulthood (5% to 7%; Costello et al., 2006, Kessler et al., 2005). Individuals with adolescent-onset MDD experience more negative outcomes relative to nondepressed adolescents or those with adult-onset MDD. The Oregon Adolescent Depression Project (OADP; Lewinsohn et al., 1993)—a prospective, epidemiological study of adolescents assessed through age 30—found that the natural course of adolescent-onset MDD is marked by impairment in a range of important psychosocial domains (relationship quality, school and work functioning, finances, physical health; Lewinsohn et al., 2003). Compared to adult-onset MDD, adolescent-onset MDD has been found to be associated with greater psychosocial impairment, physical health problems, psychiatric comorbidity, and suicidality (Hammen et al., 2008, Jaffee et al., 2002, Lewinsohn et al., 1999, Lewinsohn et al., 2003, Marmorstein et al., in press, Rohde et al., 2013, Zisook et al., 2007).
Although the negative implications of adolescent-onset MDD for functioning are well documented, a small body of literature suggests that it is MDD recurrence, rather than early onset, that accounts for this impairment. Hammen et al. (2008) compared adolescents with MDD onset prior to age 15 who did and did not experience recurrence on a number of psychosocial outcomes at age 20, and found that the recurrent group evidenced more severe and pervasive impairment in relationship, school and work, financial, and physical health domains. Lewinsohn et al. (2003) also found impairment in similar domains at age 24 for adolescent-onset MDD, but reported that much of this impairment was accounted for by ongoing MDD symptoms.
Adolescent-onset MDD often follows a chronic, recurrent course (Hammen et al., 2008, Lewinsohn et al., 1999, Rohde et al., 2013, Weissman et al., 1999, Zisook et al., 2007) and its associated psychosocial impairment may be driven by this recurrence. We sought to tease apart these clinical features by comparing the relative associations of MDD (a) age of onset and (b) course on psychosocial functioning outcomes in a large, community sample assessed prospectively from ages 17 to 29. Specifically, we compared adolescent-onset versus adult-onset MDD, and single-episode versus recurrent-episode MDD on a broad range of psychosocial outcomes assessed in early adulthood, including personality, substance use, antisocial behavior, the quality of peer and romantic relationships, work functioning, body mass index, mental health treatment, suicide attempts, and physical and sexual abuse or assault. We selected these variables on the basis of cross-sectional evidence of the negative implications of MDD for functioning in these domains. Our prospective, longitudinal study design allowed us to examine psychosocial functioning outcomes in adulthood as a function of MDD onset and course, thereby determining the extent to which the long-term psychosocial impairment associated with adolescent-onset MDD is specific to MDD that follows a recurrent course.
We extended the existing literature by addressing the following questions: Is adolescent-onset MDD associated with psychosocial functioning outcomes in adulthood after accounting for recurrence? And, is MDD recurrence associated with psychosocial functioning outcomes in adulthood after accounting for age of onset? Evidence that adolescent-onset MDD, regardless of whether it follows a single-episode or recurrent course, is associated with impairment in adulthood would suggest that early onset is the defining clinical feature. In contrast, evidence that recurrent MDD, regardless of whether it onsets in adolescence or adulthood, is associated with impairment would speak to the key role of recurrence for psychosocial functioning outcomes. In addition, because adolescent-onset MDD often follows a chronic and recurrent course, we examined the extent to which impairment in adulthood was driven primarily by individuals with both an adolescent onset and recurrent episodes of MDD.
Method
Participants and Procedures
Participants were 1,252 twins from the Minnesota Twin Family Study (MTFS) (54% female). The MTFS is an ongoing population-based, longitudinal study of reared-together twins and their parents; the study design and sample are described extensively elsewhere (see Iacono and McGue, 2002). The present study included a cohort of twins recruited at age 17. Same-sex twin pairs born between 1972 and 1978 were located using Minnesota birth records, and twins residing within 1 day’s drive of Minneapolis, living with at least one biological parent, and without physical or intellectual deficiencies that could interfere with assessment were recruited. Over 90% of eligible twins were located, and over 80% of located twins were enrolled; participating families did not differ from nonparticipating families in parental occupational status, educational attainment, or history of mental health treatment. Consistent with the demographics of Minnesota during the targeted birth years, participating families were predominately Caucasian (98%). The MTFS design includes assessments at target ages of 17 (M = 17.48, SD = 0.46), 20 (M = 20.67, SD = 0.57), 24 (M = 24.70, SD = 0.97), and 29 years (M = 29.62, SD = 0.61). Rates of retention across follow-up waves were high: age 20 (n = 1111; 89%), age 24 (n = 1167; 93%), and age 29 (n = 1168; 93%). χ2 tests indicated participants with MDD at age 17 were no less likely to provide data at ages 20 or 24 (ps > .05); they were less likely to participate at age 29, χ2(1) = 8.72, p = .003 (88% versus 94% participation rate for those with and without MDD at age 17, respectively, suggesting any attrition effects were likely to be minimal).
Diagnostic Assessment
MDD diagnoses and the onset and course of symptoms were assessed at age 17 in semi-structured interviews with participants using the Structured Clinical Interview for DSM-III-R (SCID; Spitzer et al., 1987) and with participants’ mothers using the Diagnostic Interview for Children and Adolescents—Revised (DICA-R; Reich and Welner, 1988)1. A best-estimate procedure was used to assign age-17 diagnoses if symptoms were endorsed by either mother or participant. MDD diagnoses were assessed at ages 20, 24, and 29 with participants only using the SCID. MDD diagnoses were based on DSM-III-R criteria to maintain continuity with the diagnostic system used at intake. MDD diagnoses were assigned if criteria were met at a “definite” (i.e., full DSM-III-R criteria) or “probable” (i.e., 1 criterion less than full DSM-III-R criteria) level, following guidelines introduced in the Research Diagnostic Criteria (Spitzer et al., 1978), which allow for the fact that participants were rarely acutely symptomatic at assessment and relied on memory when reporting past symptoms. Diagnostic interviews were conducted by extensively trained interviewers with bachelor’s or master’s degrees in psychology or a related discipline. All interviews were reviewed in case conferences and consensus was required prior to assigning each symptom. Computer algorithms were used to assign diagnoses. Interrater reliability was assessed on a randomly selected subsample of 600 participants (kappa = .81).
MDD was defined as adolescent onset (n = 166) if onset was prior to the age-17 assessment and as adult onset (n = 247) if afterward. MDD was defined as single episode (n = 179) if only one episode was reported through age 29, and recurrent (n = 205) if multiple episodes were reported. This resulted in four mutually exclusive MDD groups based on onset and course: the adolescent onset-single group (n = 43) met criteria for MDD by age 17 but reported only a single episode through age 29; the adolescent onset-recurrent group (n = 94) met criteria for MDD by age 17 and reported multiple episodes through age 292; the adult onset-single group (n = 136) first met criteria for MDD after age 17 but reported only a single episode through age 29; and the adult onset-recurrent group (n = 111) first met criteria for MDD after age 17 and reported multiple episodes through age 29. A never depressed group (n = 714) did not meet criteria for MDD (definite or probable) at any assessment point3.
Psychosocial Functioning
Psychosocial functioning variables were assessed at age 29 using multiple methods (questionnaires, interviews). (A subset of psychosocial variables was also assessed at age 17 and used in secondary analyses, as described below.) The frequency distributions of all variables were examined and transformations were applied as appropriate. All continuous variables were transformed to T scores (mean = 50, standard deviation = 0); all binary variables were coded so that 0 = absence, 1 = presence.
Personality
Participants reported on their positive emotionality (tendency to experience positive mood states), negative emotionality (tendency to experience negative mood states), and disconstraint (reversed constraint, tendency to inhibit impulsive, risky behavior) using the 198-item version of the Multidimensional Personality Questionnaire (MPQ; Tellegen and Waller, 2008). Cronbach’s alphas for the MPQ scales were ≥ .85, and 30-day test-retest reliabilities were ≥ .89.
Substance use and abuse
Alcohol, nicotine, and drug use and abuse were assessed using the Substance Abuse Module (SAM; Robins et al., 1987) of the Composite International Diagnostic Interview (CIDI; Robins et al., 1988). All substance use variables were log(x + 1) transformed to reduce positive skew. Participants reported on alcohol use/abuse (quantity of use in the past year, maximum number of drinks consumed in 24 hours, abuse/dependence symptoms). The mean correlation between alcohol use variables was r = .61; variables were transformed to z scores and averaged to create an age-29 alcohol use composite variable. Participants reported on nicotine use/abuse (nicotine dependence symptoms). Participants reported on drug use/abuse (frequency of marijuana use in the past year, number of drug classes tried, abuse/dependence symptoms for the drug class with the most symptoms). The mean correlation between drug use variables was r = .63; variables were transformed to z scores and averaged to create an age-29 drug use composite variable.
Antisocial behavior
Participants reported on antisocial behavior (antisocial personality disorder symptoms) using an MTFS-designed semi-structured interview comparable to the Structured Clinical Interview for DSM-III-R Axis II (SCID-II; Spitzer et al., 1987), updated for the DSM-IV. Interrater reliability was assessed on a randomly selected subsample of 600 participants (kappa = .95).
Peer group quality
Participants reported on their peer group using a 27-item scale of prosocial peers (regular jobs, work hard, volunteer) and antisocial peers (can’t seem to hold a job, substance using, trouble with the police). Cronbach’s alphas for the prosocial (9 items) and antisocial (15 items) scales were .60 and .82, respectively.
Romantic relationship quality
Participants currently involved with (married, living with, or dating for at least 3 months) a romantic partner reported on the quality of their romantic relationship (affection, disagreements, satisfaction) using a brief 12-item version of the Dyadic Adjustment Scale (DAS; Spanier, 1976). Cronbach’s alpha for the brief DAS was .83.
Partner substance use and attitudes
Participants currently involved with (married, living with, or dating for at least 3 months) a romantic partner reported on their partner’s substance use (quantity of alcohol and drug use in the past year, frequency of alcohol and drug use in the past year, proportion of time drank to intoxication, attitudes toward participant substance use). Cronbach’s alpha for the 11-item attitudes scale was .84. The correlation between partner substance use and attitudes variables was r = .69; variables were transformed to z scores and averaged to create a partner substance use composite variable.
Work functioning
Participants reported on work satisfaction (enjoyment, long-term career goals) using the Social Adjustment Interview (Johnson et al., 2007); Cronbach’s alpha for the 4-item work satisfaction scale was .63.
Body mass index
Participants’ body mass index (BMI), a height-corrected weight-height index (weight in kilograms/height in meters2), was calculated by measuring height and weight in person in the laboratory.
Mental health
Participants reported on mental health treatment (number of times treated for an emotional or mental problem since age 17, ever hospitalized for a mental health problem) using the Life Events Interview (LEI; Bemmels et al., 2008, Billig et al., 1996). The correlation between mental health treatment and psychiatric hospitalization variables was r = .40; variables were transformed to z scores and averaged to create a mental health treatment composite variable. Participants reported on suicide attempts (any suicide attempt since age 174) using the LEI.
Abuse and assault
Participants reported on physical abuse/assault and sexual abuse/assault (any physical or sexual abuse or assault since age 175) using the LEI.
Statistical Analysis
We took two complementary approaches to analyses. The first focused on the relative implications of MDD onset and course for psychosocial functioning outcomes in adulthood. We conducted a series of linear mixed models (LMMs) and logistic regression analyses that examined effects of adolescent-onset versus adult-onset, and recurrent versus single-episode MDD, while accounting for the effects of course on age of onset, and age of onset on course. LMMs were conducted for continuous psychosocial variables in SPSS 20; LMMs are similar to ANOVAs, but accommodate missing data (Peugh and Enders, 2005) and adjust standard errors for the correlated data (individual participants nested within twin pairs). Logistic regression analyses were conducted for binary psychosocial variables (suicide attempts, physical abuse/assault, sexual abuse/assault) in Mplus 4.0 using the CLUSTER command to account for correlated data. In each model, we included dummy coded variables representing age of onset (adolescent versus adult) and course (recurrent versus single episode); participant sex was included as a covariate in all analyses6. Because onset and course variables were entered simultaneously in all models, effects for onset accounted for course and vice versa—these analyses provided a direct test of the relative effects of adolescent-onset versus adult-onset MDD and recurrent versus single-episode MDD on psychosocial functioning outcomes in adulthood, as well as the incremental importance of these clinical features. We calculated Cohen’s d statistics for continuous variables and odds ratios (ORs) with 95% confidence intervals (CIs) for binary variables to provide indices of the effects of adolescent-onset versus adult-onset MDD and recurrent versus single-episode MDD. Following conventional guidelines, Cohen’s d values of 0.20 were considered small effects, 0.50 medium effects, and 0.80 large effects (Cohen, 1988).
The second approach to analyses focused on psychosocial functioning outcomes in adulthood for MDD groups defined by age of onset and course (adolescent onset-single, adolescent onset-recurrent, adult onset-single, adult onset-recurrent). We conducted a series of LMMs and logistic regression analyses that examined effects for each MDD group relative to the never depressed group. In each model, we included dummy coded variables representing each MDD group, with the never depressed group coded as the reference group; participant sex was included as a covariate. We calculated Cohen’s ds and ORs (with 95% CIs) separately for each MDD group to provide indices of the effects on psychosocial functioning outcomes for each MDD group relative to the never depressed group. The significance level was set at p < .05 for all analyses.
Results
Psychosocial Functioning Outcomes in Adulthood by MDD Onset and Course
Results of LMM analyses (continuous psychosocial variables) are presented in Table 1 and results of logistic regression analyses (binary psychosocial variables) are presented in Table 2. The first set of analyses examined the relative associations of MDD onset and course on psychosocial functioning outcomes in adulthood (Tables 1 and 2, Columns 2 to 4). Relative to single-episode MDD, recurrent MDD was generally associated with psychosocial impairment in adulthood, even accounting for age of onset (i.e., whether recurrent MDD episodes first onset by adolescence or in adulthood). Relative to single-episode MDD, recurrent MDD predicted lower positive emotionality (d = −0.26) and higher negative emotionality (d = 0.33), greater nicotine use (d = 0.26), more antisocial behavior (d = 0.24), fewer prosocial peers (d = −0.29), lower work satisfaction (d = −0.21), more mental health treatment (d = 0.56), and increased rates of attempted suicide, OR = 6.66 (1.89, 23.55); increased rates of sexual abuse/assault were also evident, but this effect was not significant, OR = 2.30 (0.96, 5.49), p = .061. These results indicate that a recurrent course of MDD predicts pervasive impairment and negative outcomes in multiple important psychosocial domains, regardless of whether it onsets by adolescence or in adulthood. In contrast, there was less evidence that adolescent-onset MDD was associated with psychosocial impairment in adulthood after accounting for recurrence. Notable exceptions were that, relative to adult-onset MDD, adolescent-onset MDD predicted greater drug use (d = 0.23) and increased rates of attempted suicide, though this effect was not significant, OR = 2.17 (0.95, 4.94), p = .065. Finally, a significant onset x course interaction for negative emotionality indicated that the adolescent onset-recurrent group evidenced higher negative emotionality at age 29 relative to the other MDD groups.
Table 1.
Continuous Psychosocial Functioning Outcomes in Adulthood by MDD Onset and Course and Effects for MDD Groups Relative to the Never Depressed Group
| Psychosocial Functioning | Adolescent-Onset vs. Adult-Onset MDD | Recurrent vs. Single-Episode MDD | Onset x Course | Never (n = 714) | Adol-Single (n = 43) | Adol-Recur (n = 94) | Adult-Single (n = 136) | Adult-Recur (n = 111) |
|---|---|---|---|---|---|---|---|---|
| Positive emotionality | F (1, 346.6) = 0.00 | F (1, 346.8) = 6.54*a | - | 50.60 (0.42) | 49.85 (1.54) d = −0.07 |
47.25 (1.08)** d = −0.31 |
50.86 (0.86) d = 0.02 |
48.16 (0.97)* d = −0.23 |
| Negative emotionality | F (1, 346.9) = 0.34 | F (1, 346.1) = 10.46***b | F (1, 338.2) = 5.65*a | 48.25 (0.40) | 50.20 (1.48) d = 0.19 |
57.34 (1.04)*** d = 0.89 |
52.67 (0.83)*** d = 0.44 |
53.83 (0.93)*** d = 0.55 |
| Disconstraint | F (1, 347.8) = 0.28 | F (1, 347.9) = 3.20 | - | 50.24 (0.40) | 50.38 (1.49) d = 0.01 |
51.63 (1.05) d = 0.13 |
49.53 (0.83) d = −0.07 |
51.38 (0.94) d = 0.11 |
| Alcohol use/abuse | F (1, 369.8) = 0.00 | F (1, 367.5) = 1.55 | - | 49.73 (0.39) | 50.04 (1.35) d = 0.03 |
51.47 (0.97) d = 0.17 |
50.84 (0.77) d = 0.11 |
51.84 (0.87)* d = 0.21 |
| Nicotine use/abuse | F (1, 355.7) = 0.93 | F (1, 353.7) = 7.61**b | - | 48.72 (0.41) | 51.13 (1.42) d = 0.22 |
54.97 (1.03)*** d = 0.58 |
50.64 (0.82)* d = 0.18 |
53.46 (0.92)*** d = 0.44 |
| Drug use/abuse | F (1, 339.8) = 5.47*a | F (1, 334.1) = 2.46 | - | 48.85 (0.40) | 50.69 (1.40) d = 0.17 |
55.50 (1.01)*** d = 0.63 |
51.80 (0.81)*** d = 0.28 |
51.53 (0.90)** d = 0.25 |
| Antisocial behavior | F (1, 364.6) = 0.03 | F (1, 362.5) = 6.35*b | - | 49.21 (0.38) | 50.40 (1.42) d = 0.12 |
53.68 (1.00)*** d = 0.44 |
51.63 (0.80)** d = 0.24 |
53.68 (0.89)*** d = 0.44 |
| Prosocial peers | F (1, 349.0) = 3.70 | F (1, 349.4) = 8.28**b | - | 50.40 (0.41) | 50.40 (1.54) d = 0.00 |
44.92 (1.08)*** d = −0.52 |
50.13 (0.86) d = −0.03 |
48.35 (0.96)* d = −0.19 |
| Antisocial peers | F (1, 342.6) = 1.40 | F (1, 343.9) = 0.15 | - | 49.72 (0.39) | 52.52 (1.45) d = 0.28 |
53.18 (1.02)*** d = 0.34 |
51.67 (0.81)* d = 0.19 |
51.87 (0.91)* d = 0.21 |
| Romantic relationship | F (1, 216.0) = 1.31 | F (1, 216.0) = 3.52 | - | 50.74 (0.48) | 50.03 (1.93) d = −0.07 |
45.97 (1.39)*** d = −0.46 |
50.59 (1.11) d = −0.01 |
48.50 (1.25) d = −0.22 |
| Partner substance use | F (1, 276.9) = 1.80 | F (1, 279.0) = 0.29 | - | 49.43 (0.45) | 51.82 (1.58) d = 0.22 |
50.53 (1.18) d = 0.10 |
49.21 (0.94) d = −0.02 |
51.01 (1.11) d = 0.15 |
| Work satisfaction | F (1, 357.0) = 0.07 | F (1, 356.9) = 4.50* | - | 50.97 (0.40) | 49.19 (1.58) d = −0.17 |
47.16 (1.10)*** d = −0.37 |
49.46 (0.88) d = −0.15 |
46.50 (0.96)*** d = −0.43 |
| Body mass index | F (1, 282.9) = 0.55 | F (1, 294.5) = 1.51 | - | 49.81 (0.45) | 51.01 (1.46) d = 0.11 |
52.33 (1.08)* d = 0.23 |
49.66 (0.88) d = −0.01 |
50.24 (0.95) d = 0.04 |
| Mental health treatment | F (1, 378.5) = 0.13 | F (1, 378.8) = 33.54*** | - | 47.55 (0.36) | 50.12 (1.41) d = 0.27 |
60.39 (0.97)*** d = 1.33 |
51.22 (0.79)*** d = 0.38 |
58.52 (0.88)*** d = 1.14 |
Note. Results of LMM analyses that include dummy variables representing MDD onset (adolescent-onset versus adult-onset) and course (recurrent versus single episodes), a term representing their interaction (nonsignificant interaction terms, p > .05, were removed from final models), and participant sex (as a covariate) are presented in Columns 2 to 4. Means (standard errors) adjusted for participant sex for each MDD group and Cohen’s ds indicating effect sizes for each MDD group relative to the never depressed group are presented in Columns 5 to 9; significant effects are noted in bold. MDD = Major Depressive Disorder. Never = never depressed. Adol-Single = adolescent-onset, single episode. Adol-Recur = adolescent-onset, recurrent episodes. Adult-Single = adult-onset, single episode. Adult-Recur = adult-onset, recurrent episodes.
Results were no longer significant after accounting for baseline (adolescent) psychosocial functioning by including the age-17 psychosocial variable as a covariate: positive emotionality, p = .060; negative emotionality, p = .056; drug use/abuse, p = .925.
Results remained significant after accounting for baseline (adolescent) psychosocial functioning by including the age-17 psychosocial variable as a covariate, all ps < .05.
p < .05.
p < .01.
p < .001.
Table 2.
Binary Psychosocial Functioning Outcomes in Adulthood by MDD Onset and Course and Effects for MDD Groups Relative to the Never Depressed Group
| Psychosocial Functioning | Adolescent-Onset vs. Adult-Onset MDD | Recurrent vs. Single-Episode MDD | Onset x Course | Never (n = 714) | Adol-Single (n = 43) | Adol-Recur (n = 94) | Adult-Single (n = 136) | Adult-Recur (n = 111) |
|---|---|---|---|---|---|---|---|---|
| Suicide attempts | χ2(1) = 3.40 | χ2(1) = 8.67** | - | 0 (0%) | 1 (2%) OR = 1.30 (0.17, 10.20) |
12 (16%)*** OR = 9.67 (4.90, 19.09) |
2 (2%) OR = 0.70 (0.16, 3.13) |
9 (8%)*** OR = 4.36 (1.92, 9.89) |
| Physical abuse/assault | χ2(1) = 1.32 | χ2(1) = 0.52 | - | 23 (3%) | 8 (20%)*** OR = 6.31 (2.78, 14.36) |
13 (16%)*** OR = 5.08 (2.37, 10.90) |
12 (9%)** OR = 2.79 (1.44, 5.42) |
15 (14%)*** OR = 4.70 (2.36, 9.35) |
| Sexual abuse/assault | χ2(1) = 0.42 | χ2(1) = 3.51 | - | 10 (1%) | 1 (3%) OR = 1.13 (0.14, 9.19) |
9 (12%)*** OR = 5.90 (2.29, 5.20) |
7 (6%)* OR = 3.55 (1.31, 9.62) |
10 (10%)*** OR = 6.28 (2.46, 16.06) |
Note. Results of logistic regression analyses that include dummy variables representing MDD onset (adolescent-onset versus adult-onset) and course (recurrent versus single episodes), a term representing their interaction (nonsignificant interaction terms, p > .05, were removed from final models), and participant sex (as a covariate) are presented in Columns 2 to 4. n (%) for each MDD group and odds ratios (ORs) with 95% confidence intervals indicating effect sizes for each MDD group relative to the never depressed group are presented in Columns 5 to 9; significant effects are noted in bold. MDD = Major Depressive Disorder. Never = never depressed. Adol-Single = adolescent-onset, single episode. Adol-Recur = adolescent-onset, recurrent episodes. Adult-Single = adult-onset, single episode. Adult-Recur = adult-onset, recurrent episodes.
p < .05.
p < .01.
p < .001.
Of the 17 psychosocial functioning variables assessed at age 29, a subset of 9 variables was also assessed at age 17. For these 9 psychosocial variables that were also assessed at age 17 (positive emotionality, negative emotionality, disconstraint, alcohol use, nicotine use, drug use, antisocial behavior, prosocial peers, antisocial peers), it was possible to account for baseline (adolescent) psychosocial functioning by including the age-17 psychosocial variable as a covariate in models. As the footnotes in Table 1 indicate, the results of these analyses accounting for adolescent psychosocial functioning were largely consistent with results of the original analyses, indicating that a recurrent course of MDD predicts decrements in psychosocial functioning from adolescence to adulthood over and above impairment already apparent in adolescence. The one notable exception for these analyses was for drug use: the effect of adolescent-onset MDD on drug use in adulthood was no longer significant after accounting for adolescent drug use.
Psychosocial Functioning Outcomes in Adulthood for MDD Groups
The second set of analyses examined psychosocial functioning outcomes in adulthood for each MDD group relative to the never depressed group (Tables 1 and 2, Columns 5 to 9). The adolescent onset-recurrent group showed impairment across most measured domains in adulthood, including lower positive emotionality and higher negative emotionality, greater nicotine and drug use, more antisocial behavior, fewer prosocial and more antisocial peers, poorer romantic relationship quality, lower work satisfaction, higher BMI, more mental health treatment, increased rates of attempted suicide, and increased rates of physical and sexual abuse/assault. Both adult-onset groups (single and recurrent episodes) evidenced greater externalizing problems, including nicotine and drug use, antisocial behavior, and fewer prosocial and more antisocial peers, relative to the never depressed group, indicating that MDD in adulthood is associated with proximal impairment (though effects were generally larger for the adult onset-recurrent group than for the adult onset-single group). With the exception of the adolescent onset-single group, all MDD groups evidenced higher negative emotionality, more mental health treatment, and increased rates of physical and sexual abuse/assault relative to the never depressed group. In contrast, only the recurrent groups evidenced lower positive emotionality, speaking to the specificity of low positive emotionality for MDD recurrence. Moreover, only the recurrent groups evidenced increased rates of attempted suicide. Notably, the adolescent onset-single group showed little psychosocial impairment in adulthood relative to the never depressed group, suggesting that long-term impairment for adolescent-onset MDD is restricted to that which follows a recurrent course.
Effect sizes for each MDD group relative to the never depressed group, averaged across all psychosocial functioning variables, are illustrated in Figure 1. Effects were consistently larger in magnitude for the adolescent onset-recurrent (mean d = 0.46) and adult onset-recurrent (mean d = 0.33) groups than for the adolescent onset-single (mean d = 0.14) and adult onset-single (mean d = 0.15) groups. Taken together, these results indicate that, regardless of age of onset, recurrent MDD shows pervasive psychosocial impairment in adulthood, though adolescent onset-recurrent MDD appears to represent a particularly severe group.
Figure 1.
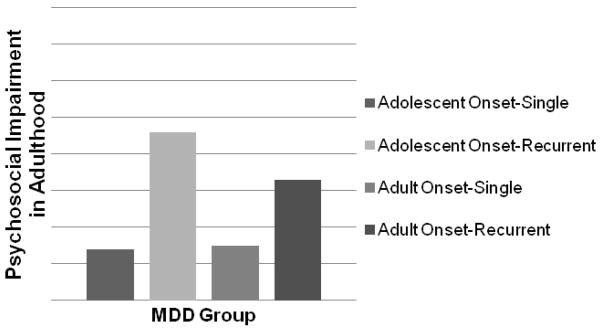
Mean effect sizes (Cohen’s ds) across psychosocial functioning variables assessed in adulthood (age 29) for each MDD group relative to the never depressed group.
Discussion
Early onset of MDD has been found to have deleterious implications for psychosocial and psychiatric functioning (Hammen et al., 2008, Jaffee et al., 2002, Lewinsohn et al., 1999, Lewinsohn et al., 2003, Rohde et al., 2013, Weissman et al., 1999, Zisook et al., 2007). We examined the incremental effects of MDD age of onset and course on psychosocial functioning outcomes in early adulthood. The results of our prospective, longitudinal study indicate that MDD course is the key clinical feature for psychosocial functioning outcomes in adulthood—recurrent MDD predicted impairment in multiple important psychosocial domains, regardless of whether it onset by adolescence or in adulthood, while adolescent-onset MDD showed less impairment in adulthood after accounting for course. Notably, associations for recurrent MDD on psychosocial functioning in adulthood largely held even accounting for adolescent functioning for the subset of variables that had been assessed at both time points, suggesting that MDD recurrence predicts decrements in psychosocial functioning over and above preexisting impairment.
Both adolescent-onset and adult-onset MDD often follow a recurrent course (Hammen et al., 2008, Lewinsohn et al., 1999, Rohde et al., 2013, Solomon et al., 2000, Weissman et al., 1999, Zisook et al., 2007). Although only 12% of participants in our population-based sample experienced adolescent-onset MDD, of those who did, 67% reported recurrent episodes through the age-29 assessment; 22% of participants experienced adult-onset MDD, and of these, 45% reported recurrent episodes. Taken together, the results of the present study indicate that the well-documented negative outcomes for adolescent-onset MDD arise from its frequently recurrent course, rather than its early onset, per se. It is possible that the experience of recurrent MDD episodes leads to psychosocial impairment by interfering with successful navigation of the key developmental tasks and role attainments that mark the adaptive transition into adulthood. It is also possible that the psychosocial impairment evident for recurrent MDD reflects a higher liability for psychopathology and related problems (Bland et al., 1986, McGuffin et al., 1996, Pettit et al., 2013)—that is, other factors may confer risk both for the development of recurrent MDD, as well as impaired psychosocial functioning.
The results of the present study are sobering in speaking to the negative implications of MDD recurrence for psychosocial functioning in adulthood. Adolescent-onset MDD that follows a recurrent course emerged as a particularly severe group that showed pervasive impairment across multiple psychosocial domains in adulthood (see also Hammen et al., 2008). However, the results also suggest room for optimism in that adolescent-onset MDD showed little evidence of impairment in adulthood if it was limited to a single episode. This finding has direct clinical implications—to the extent that experiencing recurrent MDD episodes interferes with psychosocial functioning in important domains, targeted intervention efforts that identify and successfully treat individuals with adolescent-onset MDD, thereby preventing the recurrence of additional episodes, may help to stave off impairment in adulthood.
The present study has a number of strengths, including a large, population-based sample, prospective design, and high participation rates over the 12-year follow-up with minimal attrition. Our assessment of the natural course of adolescent-onset MDD through age 29 is, along with that of the OADP, among the longest community-based longitudinal investigation of adolescent-onset MDD of which we are aware. However, there are also limitations that prompt caution in interpreting the present results. Primary among these is that we are limited in the causal inferences that can be drawn. We cannot definitively determine that psychosocial impairment in adulthood reflects a “scar” effect of MDD by examining pre- and postmorbid psychosocial functioning. Although our results suggest that MDD recurrence does lead to dysfunction (see also Ormel et al., 2004a), we cannot rule out the possibility that impairment preceded MDD onset (i.e., a “vulnerability” effect) and that recurrent episodes simply exacerbated existing dysfunction (see Beevers et al., 2007; Ormel et al., 2004b). The psychosocial functioning variables considered in the present study reflect varied domains and may have different causal relationships with MDD (see Klein et al., 2011; Ormel et al., 2004a; Ormel et al., 2004b). For example, premorbid personality may confer risk for the development of MDD or for its course (e.g., Wilson et al., 2014), the experience of MDD may negatively affect physical health (e.g., Rohde et al., 1994), and associations between MDD and interpersonal dysfunction may be bidirectional (e.g., Bulloch et al., 2009). Moreover, because the majority of participants were not currently symptomatic at the diagnostic assessment, we cannot determine the extent to which MDD has mood-dependent “state” effects on functioning. In addition, we defined adolescent-onset MDD as onset by age 17, but it is possible results might differ had we considered a different age of onset—associations with psychosocial functioning in adulthood may be stronger for childhood- or prepubertal-onset MDD than for adolescent-onset MDD, though childhood-onset MDD does not appear to differ markedly from adolescent-onset MDD (Rohde et al., 2013; Zisook et al., 2007). It is also possible that some participants classified in the present study as having had only a single episode of MDD will experience a recurrence at some point in the future. Finally, although representative of the demographics of Minnesota during the target birth years, the lack of racial and ethnic diversity limits generalizability.
In conclusion, the present study clarifies the relative importance of MDD age of onset and course for psychosocial functioning outcomes in early adulthood. Most notably, results speak to heterogeneity in adolescent-onset MDD and underscore the key role of recurrence for predicting psychosocial impairment in adulthood. Continued research that examines the relative roles of MDD onset and course for functioning in important psychosocial domains will further understanding of the etiology and consequences of this debilitating disorder.
Acknowledgments
Research reported in this article was supported by the National Institute of Drug Abuse of the National Institutes of Health under award number R01DA05147, the National Institute of Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R01AA09367, and the National Institute of Drug Abuse of the National Institutes of Health under award number K01DA025868 (B. M. H.).
Footnotes
Bipolar I and II diagnoses (lifetime history through age 24) were also assessed. Given that the present study focused on MDD, participants who met lifetime criteria for bipolar I or II disorder (n = 9) were excluded from further analyses.
Thirty-two percent of the adolescent onset-recurrent group reported recurrent episodes by age 17.
Due to missing diagnostic assessments, sample sizes for some MDD groups do not sum to the total sample size.
Because we were interested in adult outcomes, we excluded participants who reported a suicide attempt only prior to age 17 in models examining suicide attempts in adulthood.
Because we were interested in adult outcomes, we excluded participants who reported physical or sexual abuse/assault only prior to age 17 in models examining abuse/assault in adulthood.
We also tested for interactions between participant sex and MDD onset and recurrence, but found no significant effects, indicating that associations between MDD and functioning are comparable for males and females.
The authors have no financial involvement or affiliation with any organizations whose financial interests may be affected by material in this work, or that might potentially bias it.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Sylia Wilson, University of Minnesota.
Brian M. Hicks, University of Michigan
Katherine T. Foster, University of Michigan
Matt McGue, University of Minnesota.
William G. Iacono, University of Minnesota
References
- Bemmels HR, Burt SA, Legrand LN, Iacono WG, McGue M. The heritability of life events: An adolescent twin and adoption study. Twin Research and Human Genetics. 2008;11:257–265. doi: 10.1375/twin.11.3.257. [DOI] [PubMed] [Google Scholar]
- Billig JP, Hershberger SL, Iacono WG, McGue M. Life events and personality in late adolescence: Genetic and environmental relations. Behavior Genetics. 1996;26:543–554. doi: 10.1007/BF02361227. [DOI] [PubMed] [Google Scholar]
- Bland RC, Newman SC, Orn H. Recurrent and nonrecurrent depression. A family study. Archives of General Psychiatry. 1986;43:1085–1089. doi: 10.1001/archpsyc.1986.01800110071009. [DOI] [PubMed] [Google Scholar]
- Bulloch AG, Williams JV, Lavorato DH, Patten SB. The relationship between major depression and marital disruption is bidirectional. Depression and Anxiety. 2009;26:1172–1177. doi: 10.1002/da.20618. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Costello EJ, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? Journal of Child Psychology and Psychiatry. 2006;47:1263–1271. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–877. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Keenan-Miller D, Herr NR. Early onset recurrent subtype of adolescent depression: Clinical and psychosocial correlates. Journal of Child Psychology and Psychiatry. 2008;49:433–440. doi: 10.1111/j.1469-7610.2007.01850.x. [DOI] [PubMed] [Google Scholar]
- Iacono WG, McGue M. Minnesota Twin Family Study. Twin Research. 2002;5:482–487. doi: 10.1375/136905202320906327. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry. 2002;58:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Johnson W, Hicks BM, McGue M, Iacono WG. Most of the girls are alright, but some aren’t: Personality trajectory groups from ages 14 to 24 and some associations with outcomes. Journal of Personality and Social Psychology. 2007;93:266–284. doi: 10.1037/0022-3514.93.2.266. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Klein DN, Kotov R, Bufferd SJ. Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:56–63. doi: 10.1097/00004583-199901000-00020. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. Journal of Abnormal Psychology. 2003;112:353–363. doi: 10.1037/0021-843x.112.3.353. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG, Legrand L. Obesity and depression in adolescence and beyond: Reciprocal risks. International Journal of Obesity. doi: 10.1038/ijo.2014.19. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuffin P, Katz R, Watkins S, Rutherford J. A hospital-based twin register of the heritability of DSM-IV unipolar depression. Archives of General Psychiatry. 1996;53:129–136. doi: 10.1001/archpsyc.1996.01830020047006. [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, Nolen WA, Vollebergh W. Psychosocial disability before, during, and after a major depressive episode: A 3-wave population-based study of state, scar, and trait effects. Archives of General Psychiatry. 2004a;61:387–392. doi: 10.1001/archpsyc.61.4.387. [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, Vollebergh W. Vulnerability before, during, and after a major depressive episode: A 3-wave population-based study. Archives of General Psychiatry. 2004b;61:990–996. doi: 10.1001/archpsyc.61.10.990. [DOI] [PubMed] [Google Scholar]
- Pettit JW, Hartley C, Lewinsohn PM, Seeley JR, Klein DN. Is liability to recurrent major depressive disorder present before first episode onset in adolescence or acquired after the initial episode? Journal of Abnormal Psychology. 2013;122:353–358. doi: 10.1037/a0032655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peugh JL, Enders CK. Using the SPSS mixed procedure to fit cross-sectional and longitudinal multilevel models. Educational and Psychological Measurement. 2005;65:717–741. [Google Scholar]
- Reich W, Welner Z. Revised version of the Diagnostic Interview for Children and Adolescents (DICA-R) Washington University School of Medicine, Department of Psychiatry; St. Louis, MO: 1988. [Google Scholar]
- Robins LM, Baber T, Cottler LB. Composite International Diagnostic Interview: Expanded Subtance Abuse Module. Authors; St. Louis, MO: 1987. [Google Scholar]
- Robins LM, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, Sartorius N, Towle LH. The Composite International Diagnostic Interview: An epidemiologic instrument suitable for use in conjunction with different diagnostic systems in different cultures. Archives of General Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR, Gau JM. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clinical Psychological Science. 2013;1:41–53. doi: 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Are adolescents changed by an episode of major depression? Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1289–1298. doi: 10.1097/00004583-199411000-00010. [DOI] [PubMed] [Google Scholar]
- Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea T, Coryell W, Warshaw M, Turvey C, Maser JD, Endicott J. Multiple recurrences of major depressive disorder. American Journal of Psychiatry. 2000;157:229–233. doi: 10.1176/appi.ajp.157.2.229. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: Rationale and reliability. Archives of General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Biometrics Research Division. New York State Psychiatric Institute; New York, NY: 1987. Structured Clinical Interview for DSM-III-R (SCID) [Google Scholar]
- Tellegen A, Waller NG. Exploring personality through test construction: Development of the Multidimensional Personality Questionnaire. In: Boyle GJ, Matthews G, Saklofske DH, editors. Handbook of personality theory and testing: Vol. II. Personality measurement and assessment. Sage; Thousand Oaks, CA: 2008. [Google Scholar]
- Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Greenwald S, Klier CM, Ryan ND, Dahl RE, Wickramaratne P. Depressed adolescents grown up. Journal of the American Medical Association. 1999;281:1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- Wilson S, DiRago AC, Iacono WG. Prospective inter-relationships between late adolescent personality and major depressive disorder in early adulthood. Psychological Medicine. 2014;44:567–577. doi: 10.1017/S0033291713001104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook S, Lesser I, Stewart JW, Wisniewski SR, Balasubramani GK, Fava M, Gilmber WS. Effect of age at onset on the course of major depressive disorder. American Journal of Psychiatry. 2007;164:1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]


