Abstract
Objective
The present study examined anxiety and depressive symptoms in relation to the social functioning of young adolescents with attention-deficit/hyperactivity disorder (ADHD) and builds upon prior work by incorporating youths’ self-reports of internalizing symptoms and examining distinct anxiety and depression dimensions in order to increase specificity.
Method
Participants were 310 young adolescents (ages 10–14; 71% male;78% Caucasian) diagnosed with ADHD. Youth provided ratings of anxiety/depression, and parents provided ratings of their own depression. Parents and youth both reported on youths’ social skills and perceived social acceptance.
Results
Path analyses indicated that above and beyond child demographics, ADHD and oppositional defiant disorder (ODD) symptom severity, and parents’ own depression, self-reported social anxiety and anhedonia were both associated with lower youth-reported social skills and both parent- and youth-reported social acceptance. Negative self-evaluation was associated with poorer parent-reported social skills. Finally, harm avoidance was positively associated with both youth- and parent-reported social skills. A path analysis using comorbid diagnoses (rather than symptom dimensions) indicated that that having a comorbid disruptive behavior disorder or depression diagnosis (but not a comorbid anxiety diagnosis) was associated with poorer parent-reported social functioning.
Conclusions
Results demonstrate that the relation between internalizing symptoms and social functioning among young adolescents with ADHD is nuanced, with social anxiety and anhedonia symptoms associated with lower social skills and social acceptance in contrast to harm avoidance being associated with higher ratings of social skills (and unrelated to social acceptance). In terms of comorbid diagnoses, depression is more clearly related than anxiety to poorer social functioning among young adolescents with ADHD. These results point to the importance of attending to specific facets of anxiety and depression in clinical care and future research.
Keywords: Adolescence, Attention-Deficit/Hyperactivity Disorder, Comorbidity, Peer Functioning, Social Competence
Youth with attention-deficit/hyperactivity disorder (ADHD) experience significant impairments in their social relationships, including higher rates of peer rejection, less social competence, and fewer dyadic friendships than their typically developing peers (see Hoza, 2007). Extant research indicates that the social impairments experienced by children with ADHD are neither transient nor innocuous, but instead tend to be long-lasting and associated with increased impairment as children with ADHD transition to adolescence (Bagwell et al., 2001; Lee et al., 2008; Mrug et al., 2012). However, the vast majority of studies in this area have focused on elementary age children, with surprisingly few studies examining the social functioning of older youth with ADHD. As such, very little is known about factors that are associated with social impairment in adolescents with ADHD.
Youth with ADHD also experience high rates of psychiatric comorbidity, with rates of comorbid externalizing and internalizing disorders occurring in children with ADHD at much higher rates than would be expected by chance (Angold, Costello, & Erkanli, 1999; Jensen et al., 2001). For example, Kadesjö and Gillberg (2001) found that 87% of children with ADHD drawn from a population-based sample had a comorbid disorder, and 67% had at least two comorbid diagnoses. Interestingly, youth with ADHD who have a comorbid disorder are more likely than youth with noncomorbid ADHD to have ADHD that persists into adolescence (Biederman et al., 2011). However, little is known about how co-occurring mental health symptoms, and internalizing symptoms in particular, related to the social functioning of adolescents with ADHD.
The Interrelations of Internalizing Symptoms and Social Functioning among Youth with ADHD
Although comorbid oppositional defiant disorder (ODD) has consistently been shown to exacerbate the social functioning of youth with ADHD, findings examining comorbid anxiety or depression are more mixed (see Becker, Luebbe, & Langberg, 2012, for a review). It is therefore important to consider theoretically, how and why we might expect internalizing symptoms to affect the social functioning of youth with ADHD. One possibility is that internalizing symptoms do not add an incremental contribution to social impairment of youth with ADHD beyond that contributed by the presence of ADHD itself (i.e., no effect hypothesis). That is, social impairment is commonly experienced among youth with ADHD and is likely to persist into adolescence regardless of the presence of internalizing symptoms. Alternatively, since ADHD and internalizing symptoms are each independently associated with social impairment and youth with ADHD are at risk for experiencing higher rates of co-occurring mental health symptoms than their peers, the combined presence of ADHD with internalizing may confer greater risk for social difficulties (i.e., exacerbation effect hypothesis). Support for the exacerbation hypothesis can be found from non-ADHD-specific samples where broadband externalizing and internalizing symptoms have been examined. For example, Keiley and colleagues (2003) found peer rejection as assessed by classroom sociometric nominations to be associated with the covariation of externalizing and internalizing symptoms according to both mother and teacher ratings. Similarly, Fanti and Henrich (2010) recently found that children with co-occurring internalizing and externalizing problems had higher rates of peer exclusion than children with “pure” internalizing or externalizing problems.
When considering co-occurring internalizing symptoms in ADHD-specific samples, studies to date have provided support for both the no effect and exacerbation hypotheses (see Becker et al., 2012). Of note, most studies in this area have examined anxiety as opposed to depression, likely due to higher rates of anxiety in comparison to depression among children with ADHD (MTA Cooperative Group, 1999a). However, depressive symptoms become more prominent as children enter into young adolescence (Costello et al., 2011; Lewinsohn, Clarke, Seeley, & Rohde, 1994), and rates of anxiety and depression are similar in samples of adolescents with ADHD (Smalley et al., 2007). Among studies conducted in this area to date, several studies have concluded that anxiety symptoms have no effect on the social functioning of children with ADHD (Hoza et al., 2005; Lee, Falk, & Aguirre, 2012), but it is more common for studies to report mixed findings, offering some support for anxiety exacerbating the social functioning of children with ADHD as well as some support for anxiety having no effect (Bowen et al., 2008; Jensen et al., 2001; Karustis et al., 2000; Mikami, Ransone, & Calhoun, 2011; Normand et al., 2011). The very few studies focused on depression have also been inconclusive in determining whether depressive symptoms exacerbate (Blackman et al., 2005) or have no effect (Biederman et al., 1996) on the social functioning of youth with ADHD.
There are several possible explanations for the discrepant findings reported to date. First, as mentioned above, ODD symptoms are strongly associated with social impairment and studies examining internalizing symptoms have often failed to control for of the contribution of ODD (see Mikami et al., 2011, for an exception). Second, several of these studies (e.g., Bowen et al., 2008; Newcorn et al., 2004) employed a grouping strategy which resulted in a small number of participants in some of the diagnostic groups and reduced statistical power to detect effects. Third most studies have used parent- and/or teacher-reports of youth internalizing symptoms (see Karustis et al., 2000, for an exception), despite evidence-based recommendations to include self-report methods in the assessment of youth internalizing problems, particularly when assessing depression in adolescence (Klein, Dougherty, & Olino, 2005; Silverman & Ollendick, 2005). Finally, studies conducted to date have almost exclusively relied on unidimensional measures of anxiety and depression (see March et al., 2000, for an exception), even though these constructs are complex and multidimensional in nature (March, Parker, Sullivan, Stallings, & Conners, 1997). Moreover, studies have typically focused on either anxious or depressive symptoms (or collapsed across anxiety and depression to create an internalizing composite), making it difficult to determine if effects (or lack thereof) are due to the overlap of anxiety and depression that is unaccounted for in the analyses or whether results are unique to anxiety or depression.
Differentiating Anxious and Depressive Symptoms in Relation to Social Functioning
Studies conducted with community/school-based and anxiety disordered samples suggest that depressive symptoms may be particularly detrimental for the social functioning of youth with ADHD. Depressive symptoms in late childhood and adolescence are associated with social problems (Fauber, Forehand, Long, Burke, & Faust, 1987; Fröjd et al., 2008), including lower peer acceptance (Kingery, Erdley, & Marshall, 2011) and less friendship support and stability (Klima & Repetti, 2008; Prinstein, Borelli, Cheah, Simon, & Aikins, 2005). Further, when both anxiety and depressive symptoms have been incorporated in the same study, it appears that depression is more detrimental than anxiety for youths’ social adjustment (Chen, Cohen, Johnson, & Kasen, 2009; de Matos, Barrett, Dadds, & Shortt, 2003; Rose et al., 2011; Rudolph, Hammen, Burge, 1994). Likewise, Strauss et al. (1988) found that the lack of popularity among anxiety disordered children was generally limited to only those children who also had coexisting depression.
Despite these findings in nonclinical and anxiety disorder-specific samples, we are aware of only one study (Karustis et al., 2000) that has simultaneously examined both anxiety and depressive symptoms in relation to the social functioning of children diagnosed with ADHD and mixed findings were reported. Specifically, Karustis and colleagues (2000) found that self-reported anxiety symptoms were associated with parent-reported social problems above and beyond self-reported depression, whereas parent-reported depressive symptoms were associated with social problems above and beyond parent-reported anxiety. It is possible that the overall sample age (Mage = 9) contributed to self-reported anxiety having a stronger effect than self-reported depression on children’s social functioning since depressive symptoms are expected to have an increasingly detrimental impact on social functioning as youth enter adolescence. In line with this possibility, Becker and colleagues (2014) recently found self-reported depressive symptoms, but not anxiety symptoms, to exacerbate the relation between teacher-reported ADHD symptoms and social problems in an at-risk sample of Hispanic adolescents (Mage = 16). However, this was a school-based study and no study has examined both anxiety and depressive symptoms in adolescents with clinically-diagnosed ADHD.
Multidimensionality of anxiety and depression
As noted above, extant studies have typically treated anxiety and depression as a singular, unitary constructs, although both are heterogeneous and multidimensional in nature. For example, anxiety is a broad category with some symptoms related to external threats (e.g., social phobia, separation anxiety) and other symptoms that occur in response to threat (e.g., physical symptoms, harm avoidance) (see March et al., 1997, 2000). Both social and separation anxiety include avoidance behaviors, which suggests that these symptoms will be particularly detrimental for youths’ social adjustment (Albano, Chorpita, & Barlow, 2003; Beidel, Turner, & Morris, 1999). That is, since social anxiety by definition includes a fear of social/performance situations, it is not surprising that social anxiety symptoms are consistently linked to poorer social functioning (Ginsburg, La Greca, & Silverman, 1998; La Greca & Lopez, 1998), although this specificity remains to be tested in a clinical sample of adolescents with ADHD.
Similarly, depression is heterogeneous, with a range of symptoms that include negative affect, dysphoric mood (e.g., feeling sad), anhedonia (i.e., loss of the capacity to experience pleasure), negative self-evaluation (e.g., feelings of worthlessness), and fatigue and sleep disturbance. Of these, negative self-evaluation, dysphoric mood, and anhedonia may each be harmful for youths’ social functioning since they are linked to salient social behaviors such as decreased social engagement, withdrawal, and loneliness (Hammen & Rudolph, 2002). For example, anhedonia is a defining characteristic that distinguishes depression from anxiety (Clark & Watson, 1991) and is characterized by a lack of interest in pleasurable activities that may contribute to reduced engagement and fun-seeking behaviors with the peer group. Still, studies have not examined how the various dimensions of depression relate to young adolescents’ social functioning, even though identifying specific depressive symptom dimensions in relation to social functioning difficulties may offer useful targets for maximizing intervention effectiveness.
Differentiating between Social Skills and Social Acceptance
Just as it is important to differentiate between anxiety and depression, it is likewise important to differentiate between distinct domains of social adjustment (Parker, Rubin, Erath, Wojslawowicz, & Buskirk, 2006). In this study we focus on two domains of social functioning, namely, social skills and perceived social acceptance in peer relationships. Social skills encompass a “range of verbal and non-verbal responses that influence the perception and response of other people during social interactions” (Spence, 2003, p. 84). Thus, social skills includes both micro-level behaviors (e.g., eye-contact, social distance, rate/tone of speech) as well as macro-level behaviors (e.g., initiating conversation, selecting appropriate topics for conversation, offering to help) that are important for relationships broadly (including peer relations as well as relationships with parents, teachers, etc.) (Spence, 2003). In contrast, perceived social acceptance in the peer domain is not only specific to peer relationships but also focuses on how successful the child is perceived to be across peer-salient social dimensions (e.g., having friends, being popular). Critically, although social skills set the stage for the possibility of success in social relationships, they are themselves insufficient for the obtainment of social acceptance. As noted by Cavell (1990), “The distinction is one of competence versus performance…Social skills are a necessary but insufficient determinant of effective social behavior” (pp. 114, 118). Indeed, the gap between social skills and social acceptance has posed a significant challenge for intervention research aiming to not simply improve the social skills of peer-rejected children but also ultimately increase children’s social acceptance (Bierman & Powers, 2009). With these considerations in mind, the current study included measures of both social skills and perceived social (peer) acceptance.
The Present Study
To summarize, the purpose of the present study was to separately examine the contributions of anxiety and depressive dimensions in relation to the social functioning of young adolescents diagnosed with ADHD. We sought to address several limitations of previous studies in this area. First, we examined both anxiety and depression, as well as specific symptom domains within these psychopathologies, in order to increase specificity. Given the importance of incorporating youths’ own ratings in the assessment of internalizing symptoms (Klein et al., 2005; Silverman & Ollendick, 2005), we used well-validated measures of youth-reported anxiety and depression. In addition, because ADHD and ODD symptom severity may be associated with increased social problems (Becker et al., 2012), we controlled for inattentive, hyperactive-impulsive, and ODD symptoms in the analyses in order to ensure that any effect of internalizing symptoms in relation to social functioning could not be attributed to ADHD or ODD symptom severity. Since parents’ own depressive symptoms may bias their ratings of child functioning (Fergusson, Lynskey, & Horwood, 1993), we also controlled for parents’ own depressive symptoms. Lastly, we included both youth- and parent-reports of social skills and perceived social acceptance.
Using a large sample of young adolescents with ADHD, we hypothesized that social anxiety symptoms specifically would be strongly and consistently negatively associated with youth- and parent-reported social functioning. We further hypothesized that youth ratings of depressive symptoms would be negatively associated with youth- and parent-reported social functioning above and beyond the contribution of social anxiety symptoms. Previous research has not examined specific depression dimensions in relation to social skills and social acceptance, and so we did not make specific hypotheses in terms of what facets of depression would most strongly associated with social skills and social acceptance. However, we did expect the cognitive and behavioral components of depression (e.g., negative self-evaluation, anhedonia) to be more consistently associated with poorer functioning than somatic symptoms (e.g., feeling sick, sleep disturbance).
Methods
Participants
Participants were 310 young adolescents (219 males, 91 females) with ADHD between the ages of 10 and 14 (M = 12.09, SD = 0.93). Per criteria described below, 157 participants were diagnosed with ADHD Predominantly Inattentive Type (ADHD-I) and 153 participants were diagnosed with ADHD Combined Type (ADHD-C). Approximately two-thirds of the participants were Caucasian (n = 242), with the remaining participants Black (n = 39), multiracial (n = 24), or other (n = 5). Forty-two percent of the youth lived in homes where both parents lived together. When there were multiple caregivers in the home, the caregiver who “spends the most time with the child and most frequently observes their behavior” (i.e. the primary caregiver) was administered the diagnostic interview and completed the ratings. A majority of respondents were mothers (81%); the remaining were fathers (12%), grandparents (5%), or others (e.g., aunt; 2%). For ease of presentation, “parent” will be used hereafter to indicate the primary caregiver. Participants’ annual family income ranged from less than $10,000 to over $225,000 (M = $54,248; Median = $37,500). Highest level of education completed by the participants’ parents is as follows: did not earn a high school degree (5% of mothers, 10% of fathers), high school degree (33% of mothers, 44.5% of fathers), Associate’s degree (32% of mothers, 15% of fathers), Bachelor’s degree (19% of mothers, 20.5% of fathers), and advanced degree (11% of mothers, 10% of fathers).
Procedures
The study was reviewed and approved by the Institutional Review Board (IRB) and parents signed informed consent and youth provided assent. Parents/guardians who called research staff to express interest in the study were administered a phone screen. On the phone screen, parents had to indicate that their child had a diagnosis of ADHD or had to endorse their child as currently exhibiting at least 4 of 9 Diagnosis and Statistical Manual of Mental Disorder, Fourth Edition (DSM-IV; American Psychiatric Association [APA], 1994) symptoms of inattention on a rating scale in order to be scheduled for an inclusion/exclusion evaluation. The inclusionary criteria were: (a) meeting full diagnostic criteria for ADHD-I or ADHD-C; (b) an IQ ≥80 as estimated using the Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV; Wechsler, 2003); and (c) not meeting criteria for a primary diagnosis of a pervasive developmental disorder or meeting diagnostic criteria for any of the following: bipolar disorder, psychosis, substance dependence other than tobacco, or obsessive-compulsive disorder. In total, 574 families called, expressed interest in the study, and completed the phone screen. Of these, 389 families were eligible based upon the phone screen and completed the inclusion/exclusion evaluation and 326 met full study criteria and were enrolled. Of the 326 enrolled, 310 had complete data for the current study variables and were used in analyses.
ADHD diagnoses were determined using procedures similar to those used in the Multimodal Treatment of ADHD (MTA) Study (MTA Cooperative Group, 1999a). Primarily, the presence of ADHD symptoms was established using the Children’s Interview for Psychiatric Syndromes – Parent Version (P-ChIPS; Fristad et al., 1998; Weller, Weller, Rooney, & Fristad, 1999), a well-validated structured diagnostic interview that was administered to parents by advanced doctoral students and doctoral-level psychologists. The parent report of ADHD symptoms on the P-ChIPS could be supplemented with the teacher report of ADHD symptoms as reported on the Disruptive Behavior Disorder Rating Scale (DBD; Pelham Gnagy, Greenslade, & Milich, 1992). The DBD (Pelham et al., 1992) is a well-validated teacher-report measure of DSM-IV ADHD, ODD, and CD symptoms, with items rated on a four-point scale (0 = not at all present, 3 = very much present). If a parent reported at least four symptoms in either ADHD symptom domain on the P-ChIPS, these symptoms could be supplemented with nonoverlapping symptoms (items rated as occurring “pretty much” or “very much”) on the teacher-reported DBD. However, supplementation could only occur if the teacher endorsed at least four symptoms in a domain as occurring “pretty much” or “very much” on the DBD. The same supplementation rules were used to make ADHD subtype determinations. Finally, other criteria for DSM-IV ADHD (i.e., age of onset, pervasiveness, impairment, and ruling out the possibility of other causal disorders) also had to be met.
The P-ChIPS was also used to assess for the presence of comorbid psychiatric disorders. Using DSM-IV criteria, 55% of the participants (n = 171) met criteria for ODD or CD, 27% (n = 84) met criteria for an anxiety disorder (i.e., social phobia, separation anxiety, specific phobia, or generalized anxiety disorder), and 13% (n = 40) met criteria for a depressive disorder (i.e., dysthymia or major depressive disorder). Eighteen participants (6%) met criteria for both an anxiety and depressive disorder.
Measures
ADHD and ODD symptoms
Parents also completed the DBD (Pelham et al., 1992), and sum scale scores were used in the present study as a continuous measure of ADHD inattentive (α = .86), ADHD hyperactive-impulsive (α = .88), and ODD (α = .90) symptoms.
Depressive symptoms
Youth completed the Reynolds Adolescent Depression Scale, Second Edition (RADS-2; Reynolds, 2002) as a measure of their own depressive symptoms. The RADS-2 includes 30 items that measure youths’ depressive symptoms across four domains: dysphoric mood (8 items; e.g., “I feel sad”, “I feel lonely”, “I feel like crying”), anhedonia/negative affect (7 items; e.g., “I feel like eating meals”, “I feel like having fun”, “I feel like having fun with other students”), negative self-evaluation (8 items; e.g., “I feel that no one cares about me”, “I feel that other students don’t like me”, “I feel I am no good”), and somatic complaints (7 items; e.g., “I feel sick”, “I feel tired”, “I have trouble sleeping”). A point of clarification is helpful in distinguishing between the dysphoric mood and anhedonia/negative affect subscales particularly. As noted by Reynolds (2003), the dysphoric mood subscale captures the “feelings of subjective misery typically associated with depression” (p. 225), including sadness, loneliness, and irritability. In contrast, the anhedonia/negative affect subscale assesses a “behavioral component of…reduced engagement in pleasant activities” (p. 226) and thus, focuses more on anhedonia than negative affect; as such and for simplicity, we hereafter refer to this scale simply as anhedonia. Each RADS-2 item is rated on a four-point scale (1 = almost never, 4 = most of the time), with some items reverse-coded before summing the items to create subscale and total scores with higher scores indicating greater levels of depressive symptoms. Internal consistency and test-retest reliability across both school-based and clinical samples demonstrated alphas ranging from .80 to .93 for the subscale and total scores (Reynolds, 2002). Content, convergent, and discriminant validity of the RADS-2 has also been established (Reynolds, 2002). In the present study, total score α = .87, dysphoric mood α = .85, anhedonia/negative affect α = .62, negative self-evaluation α = .82, and somatic complaints α = .77. Subscale T-scores were used in analyses.
Anxiety symptoms
Youth also completed the Multidimensional Anxiety Scale for Children (MASC; March, 1997; March et al., 1997) as a measure of their anxiety. The MASC is a 39-item self-report measure of anxiety symptoms in youth across four domains: physical symptoms (12 items; e.g., “I feel tense or uptight”, “I get shaky or jittery”, “I have pains in my chest”), harm avoidance (9 items; e.g., “I try hard to obey my parents and teachers”, “I try to do everything exactly right”, “I check to make sure things are safe”), social anxiety (9 items; e.g., “I worry about other people laughing at me”, “I worry about getting called on in class”, “I feel shy”), and separation/panic (9 items; e.g., “I get scared when my parents go away”, “The idea of going away to camp scares me”, “I get scared riding in the car or on the bus”). Item responses range from 0 (never true about me) to 3 (often true about me). Internal consistency for the subscales is adequate (>.70), and concurrent, convergent, and divergent validity has been established (Baldwin & Dadds, 2007; March, 1997; March et al., 1997). In the present study, total score α = .91, physical symptoms α = .84, harm avoidance α = .75, social anxiety α = .88, and separation/panic α = .74. Subscale T-scores were used in analyses.
Parent depressive symptoms
The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) is an adult self-report measure that assesses the presence and severity of depressive symptoms. Participants responded to 21 items using a four-point scale that was summed to create a total score, with higher scores indicating greater depressive symptoms. The BDI-II total score has demonstrated strong internal consistency and acceptable convergent and divergent validity (Beck et al., 1996). In the present study, the BDI-II total sum score was used in analyses (α = .92).
Social skills
Youth and parents reported on youths’ general social skills using the Social Skills Improvement System (SSIS; Gresham & Elliott, 2008). On both versions, items are rated on a four-point scale (0 = never/not true, 3 = almost always/very true) and standard scores are calculated with higher scores indicating better social skills. Social skills items on the SSIS include a wide range of child behaviors, including communication, cooperation, assertion, responsibility, empathy, engagement, and self-control. Importantly for the purposes of this study, the majority of items focus on broad social skills that apply to social relationships generally (i.e., relationships with parents, teachers, siblings, and peers). Only four of the 46 items are specific to peer relationships, with three of these items focused on how the individual behaves in the peer group (i.e., “starts conversations with peers,” “interacts well with other children,” “tolerates peers when they are annoying”) and only one item focused on how well the individual is regarded in the peer group (i.e., “makes friends easily”). Internal and test-retest reliability of the SSIS are good and adequate criterion, convergent, and discriminant validity have been established (Gresham & Elliot, 2008). Standard scores were used in the present study (αs = .94 and .95 for the parent- and youth-report versions, respectively).
Social acceptance
Both parents and youth completed the social acceptance subscale of the Self-Perception Profile for Children (SPPC; Harter, 1985) as a measure of youths’ social acceptance. The self-report social acceptance scale is comprised of six items, and the parent-report version parallels the self-report version but includes three items rather than six. Items are scored on a four-point scale with higher scores indicating higher acceptance. The SPPC social acceptance items focus on success in the peer domain (e.g., being able to make and maintain friendships, popularity) that are rated on a four-point scale. The SPPC has demonstrated acceptable reliability and validity (Harter, 1985; Muris, Cor Meesters, & Fijen, 2003). In the present study, mean scale scores were used (αs = .93 and .77 for the parent- and youth-report versions, respectively).
Analytic Approach
First, preliminary analyses were completed to examine the distribution of the data and the bivariate correlations among the study variables. Next, the associations between psychopathology symptoms (i.e., anxiety, depressive, inattentive, hyperactive-impulsive, ODD) and social functioning domains were evaluated by estimating path models using Mplus Version 5.1 (Muthén & Muthén, 1998–2007), which allows for the simultaneous incorporation of multiple independent and dependent variables. Separate path models were run for the social skills and social acceptance domains. Because the estimated path models were fully saturated (i.e., 0 degrees of freedom), they demonstrated perfect fit to the data and model fit statistics are therefore not used or reported. Path models provide standardized path coefficients that closely correspond to correlation coefficients (Peterson & Brown, 2005) and can be interpreted as a measure of effect size, with values ≤.10 considered a small effect, values of .30 considered a medium effect, and values ≥.50 considered a large effect (Cohen, 1988). Finally, we conducted supplemental analyses to examine whether presence of comorbid internalizing disorder based on the structured diagnostic interview with the parent was associated with poorer parent- and youth-reported social functioning, and whether associations of comorbid internalizing diagnoses with social functioning remained after controlling for demographics, parent depressive symptoms, ADHD subtype, and having an ODD/CD diagnosis.
Results
Correlation Analyses
Absolute values of skew and kurtosis for all study variables were below 1.5. The intercorrelations of the parent- and youth-reported social functioning variables are shown in Table 1. Of note, the magnitude of the associations between the youth and parent ratings of social skills and social acceptance (rs = .10–.44) suggests that these social domains are related but not redundant with each other. Likewise, the MASC physical symptoms and RADS-2 somatic complaints subscales were significantly correlated (r = .61), but in sharing only 37% of the variance with each other were not considered to be overlapping and were thus retained as separate dimensions in the correlation and path analyses. Bivariate correlations of youth characteristics, parent depression, and youth psychopathology symptoms in relation to social skills and social acceptance are shown in Table 2.
Table 1.
Intercorrelations and Descriptive Statistics of Social Functioning Variables
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. PR social skills | – | .31*** | .34*** | .10 |
| 2. SR social skills | – | .15* | .29*** | |
| 3. PR social acceptance | – | .44*** | ||
| 4. SR social acceptance | – | |||
|
| ||||
| Mean | 81.74 | 93.47 | 2.69 | 2.92 |
| SD | 15.14 | 17.43 | 0.85 | 0.73 |
Note. N = 310. PR = parent-report. SR = adolescent self-report.
p< .05.
p< .01.
p< .001.
Table 2.
Correlations of Youth Characteristics, Anxiety Symptoms, and Depressive Symptoms with Social Functioning Domains
| Variable | M ± SD | Correlations |
|||
|---|---|---|---|---|---|
| SR Social Skills | PR Social Skills | SR Social Acceptance | PR Social Acceptance | ||
| Youth Characteristics | |||||
| Age | 12.09 ± 0.93 | −.06 | .02 | .03 | −.001 |
| Sex | – | .05 | .14* | .11 | −.07 |
| Race/Ethnicity | – | .11* | .20*** | −.08 | −.03 |
| ADHD Subtype | – | .01 | −.21*** | .02 | −.15** |
| ODD/CD Status | – | −.19** | −.43*** | −.06 | −.26*** |
| Parent Psychopathology (BDI) | |||||
| Depressive Symptoms | 9.57 ± 8.47 | −.09 | −.20*** | −.07 | −.13* |
| ADHD/ODD Symptoms | |||||
| Inattention | 18.77 ± 5.33 | −.02 | −.18** | −.07 | −.18** |
| Hyperactivity-Impulsivity | 11.83 ± 6.59 | .02 | −.27*** | .01 | −.18** |
| ODD | 9.70 ± 5.81 | −.21*** | −.52*** | −.02 | −.28*** |
| Anxiety Symptoms (MASC) | |||||
| Social Anxiety | 51.09 ± 12.60 | −.15** | −.01 | −.44*** | −.16** |
| Separation/Panic | 52.15 ± 12.12 | −.01 | −.01 | −.23*** | −.11 |
| Harm Avoidance | 46.45 ± 11.36 | .42*** | .18** | −.01 | −.01 |
| Physical Symptoms | 46.96 ± 9.98 | −.13* | −.04 | −.26*** | −.15* |
| MASC Total | 48.53 ± 12.16 | .02 | .04 | −.33*** | −.14* |
| Depressive Symptoms (RADS-2) | |||||
| Dysphoric Mood | 44.97 (9.98) | −.22*** | −.09 | −.36*** | −.14* |
| Anhedonia | 47.72 (6.33) | −.42*** | −.21*** | −.31*** | −.18** |
| Negative Self-Evaluation | 46.60 (8.51) | −.32*** | −.20*** | −.37*** | −.17** |
| Somatic Complaints | 44.88 (10.07) | −.19** | −.08 | −.29*** | −.18** |
| RADS Total | 44.40 (9.29) | −.36*** | −.18** | −.42*** | −.19** |
Note. N = 310. For race/ethnicity, non-Caucasian = 0, Caucasian = 1. For sex, female = 0, male = 1. For ADHD subtype, ADHD-I = 0, ADHD-C = 1. For ODD/CD status, no ODD or CD diagnosis = 0, ODD or CD diagnosis = 1. ADHD = attention-deficit/hyperactivity disorder. BDI = Beck Depression Inventory. CD = conduct disorder. MASC = Multidimensional Anxiety Scale for Children. ODD = oppositional defiant disorder. PR = parent-report. RADS-2 = Reynolds Adolescent Depression Scale, Second Edition. SR = adolescent self-report.
p< .05.
p< .01.
p<.001.
Path Analysis for Social Skills
A path model in which parent- and youth-reported social skills were regressed on youth demographics (i.e., age, sex, race), parent depressive symptoms, and youth psychopathology symptoms (i.e., anxiety, depressive, inattentive, hyperactive-impulsive, oppositional) was estimated. Results are displayed in Figure 1. After controlling for the other independent variables, ODD symptoms were negatively associated with both parent- and youth-reported social skills (βs = −0.51 and −0.24 respectively, both ps< .001). In addition, anhedonia was significantly negatively associated with youth-reported social skills (β = −0.23, p < .001), and negative self-evaluation was significantly negatively associated with parent-reported social skills (β = −0.17, p = .03). Finally, youth-reported harm avoidance was significantly positively associated with both youth-reported social skills (β = 0.46, p < .001) and parent-reported social skills (β = 0.18, p = .001).
Figure 1.
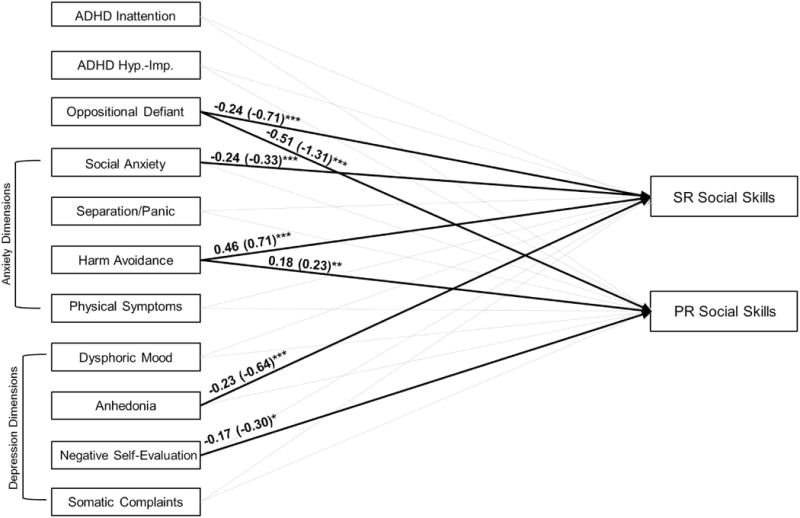
Estimated path model (N = 310). Standardized parameter estimates are reported outside parentheses; unstandardized parameter estimates are reported inside parentheses. All other paths are nonsignificant (ps> .05). Youth demographics (i.e., age, sex, race) and parent depressive symptoms were included as covariates in the model but are not displayed for clarity purposes (none were significantly associated with social skills in the path model with the exception that being a non-Hispanic white youth was significantly positively associated with both parent- and youth-reported social skills). PR = parent-report. SR = adolescent self-report.*p< .05.**p< .01.***p< .001.
Path Analysis for Social Acceptance
A similar path model was estimated in examining psychopathology dimensions in relation to parent- and youth-reported social acceptance. Results are displayed in Figure 2. After controlling for the other independent variables, ODD symptoms were negatively associated with parent-reported social acceptance (β = −0.20, p = .005) whereas inattentive symptoms were negatively associated with youth-reported social acceptance (β = −0.13, p = .03). In addition, social anxiety and anhedonia were both significantly negatively associated with both parent- and youth-reported social acceptance (βs = −0.13 − −0.38; see Figure 2).1
Figure 2.
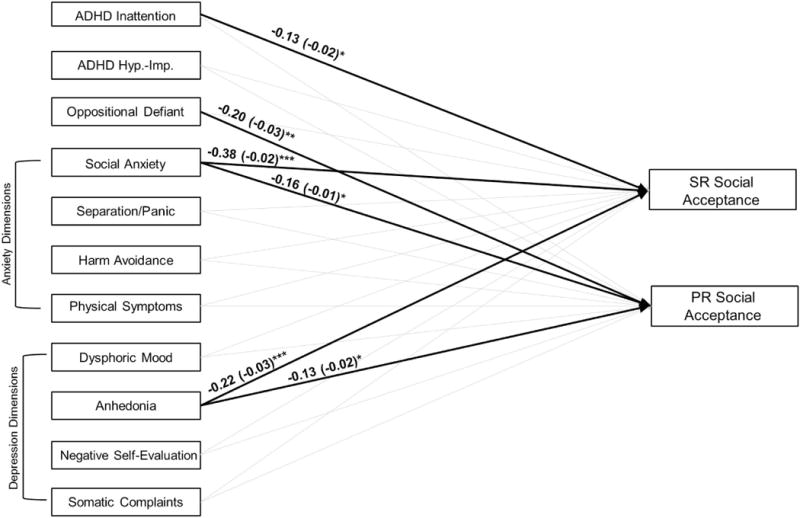
Estimated path model (N = 310). Standardized parameter estimates are reported outside parentheses; unstandardized parameter estimates are reported inside parentheses. All other paths are nonsignificant (ps>.05). Youth demographics (i.e., age, sex, race) and parent depressive symptoms were included as covariates in the model but are not displayed for clarity purposes (none were significantly associated with social acceptance in the path model with the exception that being a male was significantly negatively associated with parent-reported social acceptance). PR = parent-report. SR = adolescent self-report.*p < .05.**p < .01.***p < .001.
Supplemental Analyses Based on Comorbid Internalizing Diagnoses
Youth with a comorbid anxiety disorder (based on the P-ChIPS) had poorer parent-reported social skills (t = 2.71, p = .007) and lower social acceptance (t = 2.52, p = .01) than youth without a comorbid anxiety disorder. Youth with or without an anxiety disorder diagnosis did not differ on youth-reported social skills (t = 1.58, p = .11) or social acceptance (t = 0.56, p = .58). In comparison to participants without a depressive disorder, participants with a comorbid depression diagnosis had poorer parent-reported social skills (t = 5.41, p< .001), poorer self-reported social skills (t = 2.97, p = .003), and lower parent-reported social competence (t = 3.49, p< .001). Youth with a depressive disorder did not differ from youth without a depressive disorder on youth-reported social competence (t = 1.11, p = .27).
Finally, a path model in which parent- and youth-reported social skills and social acceptance were regressed on youth demographics (i.e., age, sex, race), parent depressive symptoms, and youth diagnosis variables (i.e., ADHD subtype, ODD/CD diagnosis, depression diagnosis, anxiety diagnosis) was estimated. After controlling for the other independent variables, having an ODD/CD diagnosis was significantly associated with poorer parent-reported social skills (β = −0.32, p < .001), parent-reported social acceptance (β = −0.19, p = .001), and youth-reported social skills (β = −0.14, p = .02). Youth with ADHD-C also had poorer parent-reported social skills than youth with ADHD-I (β = −0.12, p =.03). In addition, although having an anxiety disorder was not associated with any of the social functioning variables after controlling for the other independent variables, having a depression disorder diagnosis remained significantly associated with poorer parent-reported social skills (β = −0.15, p = .004) and social acceptance (β = −0.13, p = .02).
Discussion
This study examined self-reported depressive and anxiety symptoms in relation to social functioning in a large sample of young adolescents diagnosed with ADHD. This study builds upon prior work by (1) incorporating youths’ self-reports of internalizing symptoms, (2) examining both anxiety and depression in an effort to increase specificity related to distinct internalizing dimensions, (3) controlling for important characteristics in ADHD samples, including ADHD/ODD symptom severity and parents’ own depressive symptoms, and (4) extending previous research primarily conducted with elementary school-aged children to young adolescence when depressive symptoms are increasingly prevalent. Results of the present study suggest that the relation between internalizing symptoms and social functioning in young adolescents with ADHD is nuanced and dependent upon which facets of anxiety and depression – as well as which domains of social adjustment – are considered.
Results of the path analyses underscore the importance of social anxiety and anhedonia symptoms for the social problems of young adolescents with ADHD. First, social anxiety was significantly negatively associated with self-reported social skills and both self- and parent-reported social acceptance. This finding is not surprising given the clear and established link between social anxiety symptoms and social impairment in school/community-based samples and samples of youth with anxiety disorders (Albano et al., 2003; Beidel et al., 1999; Ginsburg et al., 1998; La Greca & Lopez, 1998). Nonetheless, the cross-rater finding in terms of self-reported social anxiety symptoms being associated with poorer parent-reported social acceptance is noteworthy because ODD symptoms and parents’ own depressive symptoms are strongly associated with parents’ perceptions of their child’s social functioning and were controlled for in the analyses.
In addition to these findings related to social anxiety, a more novel contribution of the present study is our finding that depressive symptoms – and anhedonia specifically – were also associated with poorer self-reported social skills and youth-/parent-reported social acceptance. Previous studies examining the contribution of depression to the social functioning of youth with ADHD are few and have focused primarily on elementary school-aged children and have found depression to have no effect (Biederman et al., 1996), to exacerbate (Blackman et al., 2005), or to have a mixed effect (Karustis et al., 2000) on social problems. Our results are most consistent with those of Blackman and colleagues (2005) who found in a school-based sample that children with ADHD and comorbid depression had lower scores on a latent construct measure of social competence (including parent-reported social skills, self-reported popularity, and teacher-reported peer functioning) than non-depressed children with ADHD. Indeed, our supplemental analyses using psychiatric diagnoses (as opposed to symptom dimensions) found that having a comorbid depressive disorder was significantly associated with poorer parent-reported social functioning. Although Karustis et al. (2000) found parent-reported depressive symptoms to be associated with social problems above and beyond anxiety, the reverse was true when child self-report measures of depressive and anxiety symptoms were used. The younger age of most participants in the Karustis et al. (2000) study, as well as the sole reliance on self-reported worry/oversensitivity as a measure of self-reported anxiety, may have played a role in the divergent findings between their results and results found in this study. In contrast, our study found symptoms specific to anhedonia to be most consistently associated with poorer social functioning (across 3 of the 4 social functioning variables). Adolescents experiencing anhedonic symptoms are less likely than their peers to experience positive affect and pleasurable activities, including the enjoyment of spending time with peers and the fun and engaging in activities typical of peer groups in adolescence. Interestingly, anhedonia has recently been identified as potentially critical for identifying adolescents with treatment-resistant depression (McMakin et al., 2012), and our results suggest that attending to anhedonic symptoms may also be important when seeking to intervene among youth with ADHD who experience social impairments.
In addition, the depressive domain of youth negative self-evaluation remained significantly associated with parent-reported social skills in the path model. It is not clear why this negative self-evaluation was uniquely related to parent-reported social skills (and anhedonia was not). One possibility is the difference in the social functioning measures included in this study. As discussed in the Introduction, social skills include micro- and macro-level behaviors that are important for social relationships broadly (including relationships with peers, siblings, and adults) but do not necessarily translate to social success in the peer domain specifically. In contrast, the social acceptance measure used in the present study focuses solely on the peer group (e.g., making friends, popularity). It is possible that the helplessness and worthlessness captured by the negative self-evaluation scale is more salient for general social skills since these skills also include interactions with adults, whereas high negative affect and low positive affect may together be especially harmful for social domains that are salient to the peer group, including peer acceptance and the ability to make friends.
Finally, harm avoidance was significantly positively correlated with both youth- and parent-reported social skills in the path analysis (but unrelated to social acceptance). As summarized above, previous studies have reported mixed findings in terms of whether or not anxiety exacerbates or has no effect on the social functioning of youth with ADHD (see Becker et al., 2012, for a review). These inconsistent findings may be due to the failure of previous studies to tease apart the various symptom dimensions that are encapsulated within the domain of anxiety. For instance, it is interesting to note that the MASC total score was not bivariately correlated with self- or parent-reported social skills (rs = .02 and .04, respectively). If a total anxiety score had been used in this study, as has been done in other studies examining this research question, we would have concluded that anxiety has no effect on the social skills of young adolescents with ADHD. However, this conclusion would have been erroneous and essentially due to a “cancelation effect” of having both positive and negative correlations at the subscale level that wash each other out when the total anxiety score correlations are examined. Rather, when separate anxiety dimensions are used it becomes apparent that social anxiety is related to poorer self-reported social skills as would be expected, but harm avoidance is actually associated with having better social skills. Importantly, this finding was consistent across youth and parents ratings and remained significant when controlling for a host of other variables in the path analyses.
After considering the items included on the MASC harm avoidance and the SSIS social skills scales, the positive association between these variables is not as unexpected as it may initially seem. The harm avoidance scale includes items that assess perfectionism (e.g., “I try to do everything exactly right”) and anxious coping (e.g., “If I get scared or upset, I let someone know right away”), and the SSIS assesses a broad range of social skills including behaviors related to obedience (e.g., “Follows household rules”) and seeking adult assistance (e.g., “Asks for help from adults”). Higher levels of perfectionism and anxious coping are likely related to these types of conscientious social skills, perhaps in ways similar to what has been termed “adaptive perfectionism” (e.g., Gilman & Ashby, 2003).
It is also interesting to consider what role anxious coping and perfectionism might play in the treatment of youth with ADHD. There is some evidence that children with comorbid ADHD and anxiety respond better to behavioral treatment than nonanxious children with ADHD (March et al., 2000; MTA Cooperative Group, 1999b). It may be that youth with ADHD and high levels of harm avoidance are particularly receptive to the skills training components of behavioral treatment. However, March et al. (2000) reported that while youth with an anxiety disorder in the MTA responded better to behavioral treatment, child-reported harm avoidance symptoms were unrelated to parent-reported social skills, with the exception that anxious coping (as a component of harm avoidance) was negatively associated with social skills among children with a comorbid anxiety disorder but without ODD/CD specifically. More research is needed to examine these discrepant findings, as well as to consider developmental differences that may moderate these relations (participants in the MTA were aged 7–9 years at baseline). Certainly, our finding should be considered preliminary and in need of replication, particularly since the MASC harm avoidance subscale tends to have nonsignificant or small correlations with other measures of anxiety and may therefore differ from the other MASC subscales in measuring pathological anxiety in youth (see Rey, Marin, & Silverman, 2013). It is important to note, however, that even if harm avoidance has an adaptive role in terms of social skills as the findings from the present study suggest, this may not translate to higher social acceptance. Specifically, the learning and display of concrete social skills is a necessary but insufficient component for making and maintaining dyadic friendships or experiencing broader acceptance within the peer group (Cavell, 1990; Hoza, 2007).
In addition to the interesting finding of harm avoidance being positively associated with youths’ social skills, it is important to note that there were a number of psychopathology dimensions that were not associated with either social skills or social acceptance in the path models. Specifically, the dysphoric mood, separation/panic, and somatic/physical complaints dimensions were not associated with either social functioning domain. This lack of associations may further explain why previous studies examining the link between internalizing symptoms and social problems in youth with ADHD have yielded mixed results (Becker et al., 2012). Results of our study indicate that specificity matters – both in terms of anxiety/depressive dimensions as well as in the social functioning construct being examined.
Study Limitations and Future Directions
Strengths of this study include use of a large sample of young adolescents diagnosed with ADHD and multiple informants of social functioning. Despite these strengths, several limitations should be noted. First, youth and parent ratings of social functioning were used and other related but distinct dimensions of social functioning such as peer status and friendship were not assessed. Similarly, our measures of social functioning were limited to rating scales, and it would bolster confidence in our results if these findings are replicated using other methods such as sociometric nominations and observational procedures. This may be especially important since youth with ADHD may display a positive bias in terms of their own perceptions of their social functioning (Owens et al, 2007), although it should be noted that internalizing symptoms such as depression may reduce this bias (e.g., Hoza et al., 2002). This is an important consideration for future work, particularly as we know very little about the peer functioning of adolescents with ADHD and the overly biased self-perceptions of social competence among youth with ADHD peaks around age 11.5 and then tends to decrease across adolescence (Hoza et al., 2010).
Also, our results are cross-sectional and so directionality cannot be assumed. In addition to the theoretical possibility that internalizing symptoms contribute to increased social impairment, our analytic strategy is consistent with other research in this area (e.g., Mikami et al., 2011) and allowed us to test the associations between internalizing symptoms and social domains while importantly controlling for demographic variables as well as a range of psychopathologies (e.g., ADHD and ODD symptom severity, distinct anxiety/depression dimensions). Still, just as depressive symptoms are associated with social impairment, it is also clear that social impairment contributes to the development of depression (Fergusson & Woodward, 2002; Segrin, 2000). Transactional processes are likely involved (see Rudolph, Flynn, &Abaied, 2008) and longitudinal research is needed in order to better understand how internalizing symptoms and social impairments unfold across childhood and adolescence for individuals with ADHD. For example, Humphreys and colleagues (2013) recently provided compelling evidence of peer and parent-child problems as mediators of the association between ADHD and depressive symptoms. Other factors, such as friendship quality, may buffer the relation between psychopathology and general social problems (Becker, Fite, Luebbe, Stoppelbein, & Greening, 2013). Hence, studies are needed that not only examine how internalizing symptoms and social problems interact over time among youth with ADHD, but also consider moderators and mediating processes of these transactional relations. In addition, it will be important for future research to examine co-occurring internalizing symptoms and diagnoses in older adolescents and young adults with ADHD when rates of depression continue to rise.
Likewise, we did not include a non-ADHD group in this study or a group of youth with internalizing disorders but without ADHD, and so it remains unclear the degree to which our results are unique to youth with ADHD as opposed to young adolescents more broadly. However, a strength of this study is its use of a large sample of young adolescents diagnosed with ADHD, as youth with ADHD are known to experience high rates of both psychiatric comorbidity and social impairments and we know less about the social difficulties of these youth when rates of internalizing problems (especially depression) are expected to rise. These comorbid mental health symptoms (e.g., ODD vs. depression) may also be important for developing and tailoring interventions for adolescents with ADHD. Still, without a comparison group of youth without ADHD, we were unable to examine whether similar associations apply to typically developing youth or whether ADHD diagnostic status moderates associations. It would certainly be expected that social anxiety symptoms relate to poorer social functioning among non-ADHD youth since social anxiety by definition includes a fear of socially-salient situations. In addition, it is likely that anhedonia has an adverse effect on the social functioning of youth without ADHD, but it would be helpful if future studies included both youth with and without ADHD in order to directly test this possibility. Such studies could also examine the role of ADHD symptom severity. Hyperactive-impulsive symptoms were not associated with any of the social functioning variables in the path models (although having a clinical diagnosis of ADHD-C was associated with poorer parent-reported social skills), and inattentive symptoms were only associated with lower youth-reported social acceptance. This is likely because all participants in this study met criteria for a clinical diagnosis of ADHD, thus limiting the range of ADHD symptom severity that may play an important role in nonclinical samples.
Finally, the RADS anhedonia subscale demonstrated somewhat low internal consistency in the current sample (α = .62). Moreover, two of the seven items on the RADS anhedonia subscale are explicitly social in nature (i.e., “I feel like having fun with other students”, “I feel like talking to other students”), and so while disinterest in social and other pleasurable activities is the defining feature of anhedonia these two items may have inflated associations between the anhedonia dimension of depression and our social functioning variables. Unfortunately, a modified anhedonia scale that removed these two socially-valenced items resulted in a scale with unacceptably low internal consistency (α = .46) to use in analyses. Hence, our findings related to anhedonia should be viewed somewhat cautiously with future research using measures of anhedonia that do not include social-specific items.
Conclusion
Despite the high rates of both social impairment and co-occurring mental health problems in samples of youth with ADHD, remarkably few studies have considered both anxiety and depression when examining the social difficulties of this population, and no studies to date have examined specific anxiety and depressive dimensions. Results of the present study highlight the importance of specificity when examining the role of internalizing symptoms in relation to the adjustment of youth with ADHD. Although social anxiety is negatively associated with these youths’ social adjustment as expected, we found evidence for harm avoidance to be positively associated with social skills specifically. Depressive symptoms related to anhedonia and negative self-evaluation (as well as oppositional-defiant symptoms) were also associated with poorer social functioning across self and parent ratings, and having a comorbid depressive disorder was likewise associated with poorer parent-reported social functioning. In addition to the off-putting and disruptive behaviors associated with ADHD and comorbid ODD/CD, findings from this study indicate that social anxiety and anhedonia may be especially important components to target in interventions designed to improve the social functioning of adolescents with ADHD.
Acknowledgments
Author Note. This research was supported by a grant to the second and third authors from the National Institute of Mental Health (NIMH; R01MH082865). The contents of this manuscript do not necessarily represent the views of the National Institutes of Health and do not imply endorsement by the Federal Government.
Footnotes
One of the tensions encountered when designing models to be tested is the number of covariates and predictor variables to include. On the one hand, including important covariates and other predictor variables bolsters confidence in the findings presented and often sheds light on mixed findings reported by previous studies. On the other hand, increasing the number of variables in the model by definition increases the number of paths to be tested, which may also increase the probability of a Type 1 error. We viewed the inclusion of demographic characteristics and parent depressive symptoms in addition to all anxiety/depressive symptom dimensions in the path models as important in order to improve upon previous studies in this area and inform future research. Still, we acknowledge that this decision may have increased the probability of having a Type 1 error. There is no simple solution to this dilemma, particularly as a Bonferroni or related correction “creates more problems than it solves” (Perneger, 1998, p. 1236; see also Nagagawa, 2004 and Moran, 2003). We therefore did not apply such a correction but note that if such a correction were used the cross-rater effects of youth-rated internalizing symptoms in relation to parent-rated social functioning would be lost with the exception of harm avoidance remaining significantly positively associated with parent-reported social skills.
Contributor Information
Stephen P. Becker, Email: beckersp@miamioh.edu.
Joshua M. Langberg, Email: jlangberg@vcu.edu.
Steven W. Evans, Email: evanss3@ohio.edu.
Erin Girio-Herrera, Email: girioherrera@psy.miami.edu.
Aaron J. Vaughn, Email: aaron.vaughn@cchmc.org.
References
- Albano AM, Chorpita BF, Barlow DH. Childhood anxiety disorders. In: Mash EJ, Barkley RA, editors. Child psychopathology. 2. New York: Guilford; 2003. pp. 279–329. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Bagwell C, Molina BSG, Pelham WE, Hoza B. Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1285–1292. doi: 10.1097/00004583-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Baldwin JS, Dadds MR. Reliability and validity of parent and child versions of the Multidimensional Anxiety Scale for Children in community samples. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:252–260. doi: 10.1097/01.chi.0000246065.93200.a1. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory, 2nd edition (BDI-II) San Antonio, TX: Psychological Corp; 1996. [Google Scholar]
- Becker SP, Fite PJ, Luebbe AM, Stoppelbein L, Greening L. Friendship intimacy exchange buffers the relation between ADHD symptoms and later social problems among children attending an after-school care program. Journal of Psychopathology and Behavioral Assessment. 2013;35:142–152. doi: 10.1007/s10862-012-9334-1. [DOI] [Google Scholar]
- Becker SP, Fite PJ, Vitulano ML, Rubens SL, Evans SC, Cooley JL. Examining anxiety and depression as moderators of the associations between ADHD symptoms and academic and social problems in Hispanic adolescents. Journal of Psychopathology and Behavioral Assessment. 2014;36:265–275. doi: 10.1007/s10862-013-9394-x. [DOI] [Google Scholar]
- Becker SP, Luebbe AM, Langberg JM. Co-occurring mental health problems and peer functioning among youth with attention-deficit/hyperactivity disorder: A review and recommendations for future research. Clinical Child and Family Psychology Review. 2012;15:279–302. doi: 10.1007/s10567-012-0122-y. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Morris TL. Psychopathology of childhood social phobia. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:643–650. doi: 10.1097/00004583-199906000-00010. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Mick E, Moore P, Lelon E. Child Behavior Checklist findings further support comorbidity between ADHD and major depression in a referred sample. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:734–742. doi: 10.1097/00004583-199606000-00013. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Clarke A, Lomedico A, Faraone SV. Predictors of persistent ADHD: An 11-year follow-up study. Journal of Psychiatric Research. 2011;45:150–155. doi: 10.1016/j.jpsychires.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierman KL, Powers CJ. Social skills training to improve peer relations. In: Rubin KH, Bukowski WM, Laursen B, editors. Handbook of peer interactions, relationships, and groups. New York: Guilford; 2009. pp. 603–621. [Google Scholar]
- Blackman GL, Ostrander R, Herman KC. Children with ADHD and depression: A multisource, multimethod assessment of clinical, social, and academic functioning. Journal of Attention Disorders. 2005;8:195–207. doi: 10.1177/1087054705278777. [DOI] [PubMed] [Google Scholar]
- Bowen R, Chavira DA, Bailey K, Stein MT, Stein MB. Nature of anxiety comorbid with attention deficit hyperactivity disorder in children from a pediatric primary care setting. Psychiatry Research. 2008;157:201–209. doi: 10.1016/j.psychres.2004.12.015. [DOI] [PubMed] [Google Scholar]
- Cavell TA. Social adjustment, social performance, and social skills: A tri-component model of social competence. Journal of Clinical Child Psychology. 1990;19:111–122. [Google Scholar]
- Chen H, Cohen P, Johnson JG, Kasen S. Psychiatric disorders during adolescence and relationships with peers from age 17 to age 27. Social Psychiatry and Psychiatric Epidemiology. 2009;44:223–230. doi: 10.1007/s00127-008-0421-2. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry. 2011;52:1015–1025. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Matos MG, Barrett P, Dadds M, Shortt A. Anxiety, depression, and peer relationships during adolescence: Results from the Portugese national health behaviour in school-aged children survey. European Journal of Psychology of Education. 2003;18:3–14. [Google Scholar]
- Fanti KA, Henrich CC. Trajectories of pure and co-occurring internalizing and externalizing problems from age 2 to age 12: Findings from the National Institute of Child Health and Human Development Study of Early Child Care. Developmental Psychology. 2010;46:1159–1175. doi: 10.1037/a0020659. [DOI] [PubMed] [Google Scholar]
- Fauber R, Forehand R, Long N, Burke M, Faust J. The relationship of young adolescent Children’s Depression Inventory (CDI) scores to their social and cognitive functioning. Journal of Psychopathology and Behavioral Assessment. 1987;9:161–172. [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. The effect of maternal depression on maternal ratings of child behavior. Journal of Abnormal Child Psychology. 1993;21:245–269. doi: 10.1007/BF00917534. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- Fristad MA, Cummings J, Verducci JS, Teare M, Weller EB, Weller RA. Study III: Development and concurrent validity of the Children’s Interview for Psychiatric Syndromes – Parent Version (P-ChIPS) Journal of Child and Adolescent Psychopharmacology. 1998;8:221–226. doi: 10.1089/cap.1998.8.221. [DOI] [PubMed] [Google Scholar]
- Fröjd SA, Nissinen ES, Pelkonen MUI, Marttunen MJ, Koivisto AM, Kaltiala-Heino R. Depression and school performance in middle adolescent boys and girls. Journal of Adolescence. 2008;31:485–498. doi: 10.1016/j.adolescence.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Gilman R, Ashby JS. Multidimensional perfectionism in a sample of middle school students: An exploratory investigation. Psychology in the Schools. 2003;40:677–689. [Google Scholar]
- Ginsburg GS, La Greca AM, Silverman WK. Social anxiety in children with anxiety disorders: Relation with social and emotional functioning. Journal of Abnormal Child Psychology. 1998;26:175–185. doi: 10.1023/a:1022668101048. [DOI] [PubMed] [Google Scholar]
- Gresham FM, Elliott SN. Social Skills Improvement System – Rating Scales. Minneapolis, MN: Pearson Assessments; [Google Scholar]
- Hammen C, Rudolph KD. Childhood mood disorders. In: Mash EJ, Barkley RA, editors. Child Psychopathology. 2. New York: Guilford; 2002. pp. 233–278. [Google Scholar]
- Harter S. Manual for the Self-Perception Profile for Children. Denver: University of Denver; 1985. [Google Scholar]
- Hoza B. Peer functioning in children with ADHD. Journal of Pediatric Psychology. 2007;32:655–663. doi: 10.1093/jpepsy/jsm024. [DOI] [PubMed] [Google Scholar]
- Hoza B, Pelham WE, Dobbs J, Owens JS, Pillow DR. Do boys with attention-deficit/hyperactivity disorder have positive illusory self-concepts? Journal of Abnormal Psychology. 2002;111:268–278. doi: 10.1037//0021-843x.111.2.268. [DOI] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, Arnold LE. What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder? Journal of Consulting and Clinical Psychology. 2005;73:411–423. doi: 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- Hoza B, Murray-Close D, Arnold LE, Hinshaw SP, Hechtman L, MTA Cooperative Group Time-dependent changes in positively biased self-perceptions of children with attention-deficit/hyperactivity disorder: A developmental psychopathology perspective. Development and Psychopathology. 2010;22:375–390. doi: 10.1017/S095457941000012X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Katz SJ, Lee SS, Hammen C, Brennan PA, Najman JM. The association of ADHD and depression: Mediation by peer problems and parent-child difficulties in two complementary samples. Journal of Abnormal Psychology. 2013;122:854–867. doi: 10.1037/a0033895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, Vitiello B. ADHD comorbidity findings from the MTA study: Comparing comorbid subgroups. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:147–158. doi: 10.1097/00004583-200102000-00009. [DOI] [PubMed] [Google Scholar]
- Kadesjö B, Gillberg C. The comorbidity of ADHD in the general population of Swedish school-age children. Journal of Child Psychology and Psychiatry. 2001;42:487–492. [PubMed] [Google Scholar]
- Karustis JL, Power TJ, Rescorla LA, Eiraldi RB, Gallagher PR. Anxiety and depression in children with ADHD: Unique associations with academic and social functioning. Journal of Attention Disorders. 2000;4:133–149. [Google Scholar]
- Keiley MK, Lofthouse N, Bates JE, Dodge KA, Pettit GS. Differential risks of covarying and pure components in mother and teacher reports of externalizing and internalizing behavior across ages 5 to 14. Journal of Abnormal Child Psychology. 2003;31:267–283. doi: 10.1023/a:1023277413027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingery JN, Erdley CA, Marshall KC. Peer acceptance and friendship as predictors of early adolescents’ adjustment across the middle school transition. Merrill-Palmer Quarterly. 2011;57:215–243. [Google Scholar]
- Klein DN, Dougherty LR, Olino TM. Towards guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:412–432. doi: 10.1207/s15374424jccp3403_3. [DOI] [PubMed] [Google Scholar]
- Klima T, Repetti T. Children’s peer relations and their psychological adjustment: Differences between close friendships and the larger peer group. Merrill-Palmer Quarterly. 2008;54:151–178. [Google Scholar]
- La Greca A, Lopez N. Social anxiety among adolescents: Linkages to peer relations and friendships. Journal of Abnormal Child Psychology. 1998;26:83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]
- Lee SS, Falk AE, Aguirre VP. Association of comorbid anxiety with social functioning in school-age children with and without attention-deficit/hyperactivity disorder (ADHD) Psychiatry Research. 2012;197:90–96. doi: 10.1016/j.psychres.2012.01.018. [DOI] [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Owens EB, Hinshaw SP. Few preschool boys and girls with ADHD are well-adjusted during adolescence. Journal of Abnormal Child Psychology. 2008;36:373–383. doi: 10.1007/s10802-007-9184-6. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- March JS. Multidimensional Anxiety Scale for Children. North Tonawanda, NY: Multi-Health Systems; 1997. [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners K. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- March JS, Swanson JM, Arnold LE, Hoza B, Conners CK, Hinshaw SP, Pelham WE. Anxiety as a predictor and outcome variable in the Multimodal Treatment Study of Children with ADHD (MTA) Journal of Abnormal Child Psychology. 2000;28:527–541. doi: 10.1023/a:1005179014321. [DOI] [PubMed] [Google Scholar]
- McMakin DL, Olino TM, Porta G, Dietz LJ, Emslie G, Clarke G, Brent DA. Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor treatment-resistant depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:404–411. doi: 10.1016/j.jaac.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikami AY, Ransone ML, Calhoun CD. Influence of anxiety on the social functioning of children with and without ADHD. Journal of Attention Disorders. 2011;15:473–484. doi: 10.1177/1087054710369066. [DOI] [PubMed] [Google Scholar]
- Moran MD. Arguments for rejecting the sequential Bonferroni in ecological studies. Oikos. 2003;100:403–405. [Google Scholar]
- Mrug S, Molina BSG, Hoza B, Gerdes AC, Hinshaw SP, Hechtman L, Arnold LE. Peer rejection and friendships in children with attention-deficit/hyperactivity disorder: Contributions to long-term outcomes. Journal of Abnormal Child Psychology. 2012;40:1013–1026. doi: 10.1007/s10802-012-9610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999a;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999b;56:1088–1096. doi: 10.1001/archpsyc.56.12.1088. [DOI] [PubMed] [Google Scholar]
- Muris P, Meesters C, Fijen P. The Self-Perception Profile for Children: Further evidence for its factor structure, reliability, and validity. Personality and Individual Differences. 2003;35:1791–1802. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 5. Los Angeles, CA: Muthén & Muthén; 1998–2007. [Google Scholar]
- Nakagawa S. A farewell to Bonferroni: The problems of low statistical power and publication bias. Behavioral Ecology. 2004;15:1044–1045. [Google Scholar]
- Newcorn JH, Miller SR, Ivanova I, Schulz KP, Kalmar J, Marks DJ, Halperin JM. Adolescent outcome of ADHD: Impact of childhood conduct and anxiety disorders. CNS Spectrums. 2004;9:668–678. doi: 10.1017/s1092852900001942. [DOI] [PubMed] [Google Scholar]
- Normand S, Schneider BH, Lee MD, Maisonneuve MF, Kuehn SM, Robaey P. How do children with ADHD (mis)manage their real-life dyadic friendships? A multi-method investigation. Journal of Abnormal Child Psychology. 2011;39:293–305. doi: 10.1007/s10802-010-9450-x. [DOI] [PubMed] [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review. 2007;10:335–351. doi: 10.1007/s10567-007-0027-3. [DOI] [PubMed] [Google Scholar]
- Parker JG, Rubin KH, Erath SA, Wojslawowicz JC, Buskirk AA. Peer relationships, child development, and adjustment: A developmental psychopathology perspective. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology, Vol. 1: Theory and method. 2. Hoboken, NJ: Wiley; 2006. pp. 419–493. [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Perneger TV. What’s wrong with Bonferroni adjustments. British Medical Journal. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson RA, Brown SP. On the use of beta coefficients in meta-analysis. Journal of Applied Psychology. 2005;90:175–181. doi: 10.1037/0021-9010.90.1.175. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Borelli JL, Cheah CSL, Simon VA, Aikins JW. Adolescent girls’ interpersonal vulnerability to depressive symptoms: A longitudinal examination of reassurance-seeking and peer relationships. Journal of Abnormal Psychology. 2005;114:676–688. doi: 10.1037/0021-843X.114.4.676. [DOI] [PubMed] [Google Scholar]
- Rey Y, Marin CE, Silverman WK. Assessment of anxiety disorders: Categorical and dimensional perspectives. In: Vasa RA, Roy AK, editors. Pediatric anxiety disorders: A clinical guide. New York: Springer; 2013. pp. 231–267. [Google Scholar]
- Reynolds WM. Reynolds Adolescent Depression Scale: RADS-2: Professional Manual. Odessa, FL: Psychological Assessment Resources; 2002. [Google Scholar]
- Reynolds WM. The Reynolds Adolescent Depression Scale – Second Edition (RADS-2) In: Hilsenroth MJ, Segal DL, editors. Comprehensive Handbook of Psychological Assessment, Volume 2, Personality Assessment. Hoboken, NJ: Wiley; 2003. pp. 224–236. [Google Scholar]
- Rose AJ, Carlson W, Luebbe AM, Schwartz-Mette RA, Smith RR, Swenson LP. Predicting difficulties in youth’s friendships: Are anxiety symptoms as damaging as depressive symptoms? Merrill-Palmer Quarterly. 2011;57:244–262. [Google Scholar]
- Rudolph KD, Flynn M, Abaied JL. A developmental perspective on interpersonal theories of youth depression. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York: Guilford; 2008. pp. 79–102. [Google Scholar]
- Rudolph KD, Hammen C, Burge D. Interpersonal functioning and depressive symptoms in childhood: Addressing the issues of specificity and comorbidity. Journal of Abnormal Child Psychology. 1994;22:355–371. doi: 10.1007/BF02168079. [DOI] [PubMed] [Google Scholar]
- Segrin C. Social skills deficits associated with depression. Clinical Psychology Review. 2000;20:379–403. doi: 10.1016/s0272-7358(98)00104-4. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Smalley SL, McGough JJ, Moilanen IK, Loo SK, Taanila A, Ebeling H, Järvelin MR. Prevalence and psychiatric comorbidity of attention-deficit/hyperactivity disorder in an adolescent Finnish population. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1575–1583. doi: 10.1097/chi.0b013e3181573137. [DOI] [PubMed] [Google Scholar]
- Spence SH. Social skills training with children and young people: Theory, evidence and practice. Child and Adolescent Mental Health. 2003;8:84–96. doi: 10.1111/1475-3588.00051. [DOI] [PubMed] [Google Scholar]
- Strauss CC, Lahey BB, Frick P, Frame CL, Hynd GW. Peer social status of children with anxiety disorders. Journal of Consulting and Clinical Psychology. 1988;56:137–141. doi: 10.1037//0022-006x.56.1.137. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children—Fourth Edition. San Antonio, TX: Psychological Corporation; 2003. [Google Scholar]
- Weller EB, Weller R, Rooney MT, Fristad MA. Children’s Interview for Psychiatric Syndromes (ChIPS) Washington, DC: American Psychiatric Association; 1999. [DOI] [PubMed] [Google Scholar]


