Abstract
Background:
Malaria is an endemic infectious disease in southeastern parts of Iran. Despite years of efforts and intervention programs against malaria, transmission still occurs in Jask County.
Methods:
The epidemiological perspective of malaria in Jask County was conducted by gathering data from Jask County health center, during 2006–2010. A knowledge, attitude and practice study was also carried out. Data analysis was conducted using SPSS ver. 11.5.
Results:
A total of 2875 malaria cases were recorded, with highest and lowest numbers in 2007 and 2010, respectively. The number of cases had a decreasing trend from 1022 cases in 2006 to 114 cases in 2010. The main causative parasitic agent was Plasmodium vivax. Blood examination rate and slide positive rate were also decreased from 39.5% and 4.3% in 2006 to 15.6% and 1.4% in 2010, respectively. Most of people interviewed in the KAP study had a good knowledge about malaria transmission and symptoms but their use of the bed net for prevention was low (35%).
Conclusion:
Malaria incidence had significant reduction during the study years. The main reason for this may be due to changing environmental condition for Anopheline breeding and survival because of drought. Another reason may be integration of vector management by using long lasting insecticide treated bed nets, active case detection and treatment by implementation of mobile teams and increasing in financial sources of malaria control program. Knowledge, attitude and practice of people were good in malaria control and prevention, but needs to do more activities for health education and awareness.
Keywords: Malaria situation, Jask County, Iran
Introduction
More than half of the world's population in approximately 100 countries is exposed to malaria. According to figures provided by the World Health Organization (WHO 2011a), 36% of the global population live in areas where there is risk of malaria transmission, 7% reside in areas where malaria has never been under meaningful control, and 29% live in areas where malaria was once transmitted at low levels or not at all, but where significant transmission has been re-established.
In Iran, the total population at risk of malaria is 2,714,648 (4% of the total population) mainly living in southeastern provinces, namely Sistan and Baluchistan, Kerman and Hormozgan (WHO 2011a). There are some studies in last decade focused on malaria situation analysis (Hanafi-Bojd et al. 2010, Vatandoost et al. 2010, 2011), as well as epidemiological features and community based studies in malarious areas of southern parts of Iran (Rakhshani et al. 2003, Salehi et al. 2010, Hanafi-Bojd et al. 2011a, Youssefi and Rahimi 2011, McKelvie et al. 2012, Zoghi et al. 2012).
According to the national strategy plan for malaria control, in respect to malaria status the total country has been classified in four strata:
Areas where local transmission of malaria occurs such as areas in Sistan and Baluchistan, Hormozgan and south parts of Kerman, and occasionally some-areas in Ardebil, Bushehr, Fars and Khorassan-e-Razavi Provinces.
Areas where the imported cases are found and the potential risk of malaria transmission exists such as areas in Guilan, Mazandaran, and Golestan Provinces.
Areas where the imported cases are found, but there is no risk of malaria transmission such as Yazd, Kurdestan, and Hamedan Provinces.
Areas where no malaria case was reported during the last three years. It seems there was no such area in Iran.
Malaria remains an important public health concern in Jask County, where transmission occurs regularly, and infected immigrants can play an important role as mobile reservoirs (Personal communication with health center authorities). Therefore it is important to do a situation analysis of the disease for planning the control activities in future. The aim of conducting a situational analysis is to systematically understand the malaria epidemiology of an area in a very short space of time and the health status, system and resource available for controlling the disease (WHO 2011b). A successful planning for the County, needs to use of the information that is already available and analyzing in such a way as to understand the problems. On the other hand, the main point of the beginning of the situational analysis is to collect the data from respective references such as, health network office, hospital, health centers, communities, meteorology department and others. These items are covered by international diploma courses on malaria planning and management, as a joint training course by WHO and Tehran University of Medical Sciences (Mesdaghinia et al. 2013).
The general objective of this study was to facilitate the development of friendly-user implementation plan for Jask County to identify malaria-relevant gaps with its possible solutions.
Materials and Methods
Study area
Jask County (25° 64’ N, 57° 77’ E) is a sea port located in South-Eastern corner of Iran adjacent to the Oman Sea, with a surface area of 16063 km2 (Fig. 1). Total population of the County is 50070 (74% are living in rural areas). There are scattered inhabitants and their occupation is mainly fishing and trade.
Fig. 1.
Location of Jask County in Iran
Data collection
In this retrospective study, the needed data for 2006–2010 were obtained from health center of Jask, published papers and reports, weather forecasting organization of the city and annual reports of Hormozgan official authorities. An excel databank was created and analysis was conducted using this software. A knowledge, attitude and practice (KAP) study was conducted to evaluate the knowledge, attitude and practice of people who referred to the urban health center of Touhid, about malaria using structured questionnaire and interviewing.
Data analysis
For this purpose SPSS ver. 11.5 was used and graphs were prepared by excel 2007.
Results
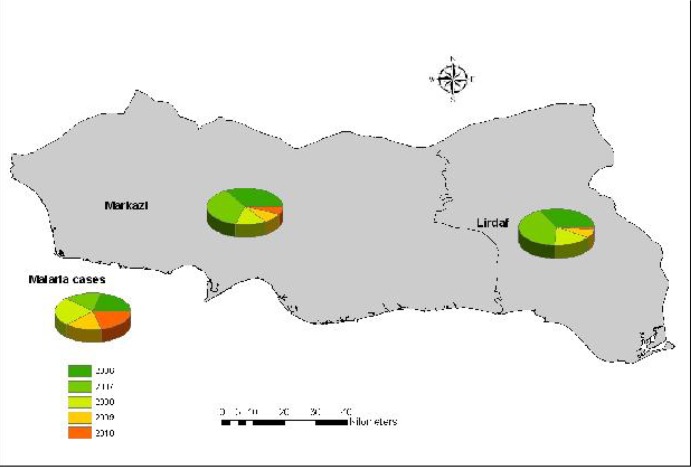
A total of 2875 malaria cases were recorded and treated during the study period (Fig. 2). Plasmodium vivax is the main malaria parasite (94.92%) in the County followed by P. falciparum (5.08%). Average of malaria morbidity in months of the years during the study period showed two peaks in May and November, respectively. The maximum and minimum of Annual Parasitic Index (API) were observed in 2006 (22.1) and 2010 (2.1), respectively (Table 1). Most of cases were reported to be autochthonous during 2006–2009, while in 2010 the imported cases were higher. Blood Examination Rate (BER) has increased to 2007 and then collapsed, but Slide Positive Rate has a decreasing trend during the study period, although it shows a peak in 2008 (Table 1). Autochthonous cases of malaria have decreased during the study period, while the imported cases had an increasing trend (Table 1). Figure 2 shows the distribution of malaria cases based on rural districts of the Jask County during the study period.
Fig. 2.
Malaria distribution map, Jask County, 2006–2010
Table 1.
Malaria indices in Jask County, Southeastern Iran, 2006–2010
| Year | Malaria indices | No. Cases | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| SPR | API | BER | Autochthonous | Imported | P. vivax | P. falciparum | Total | |
| 2006 | 4.3 | 22.1 | 39.5 | 1000 | 22 | 1000 | 22 | 1022 |
| 2007 | 2.5 | 21.6 | 50.6 | 1013 | 12 | 954 | 70 | 1024 |
| 2008 | 3.5 | 10.6 | 28.1 | 485 | 27 | 495 | 11 | 506 |
| 2009 | 2 | 4.2 | 20.6 | 162 | 47 | 183 | 26 | 209 |
| 2010 | 1.4 | 2.2 | 15.6 | 34 | 80 | 97 | 17 | 114 |
SPR: Slide positive rate, API: Annual parasitic index, BER: Blood examination rate
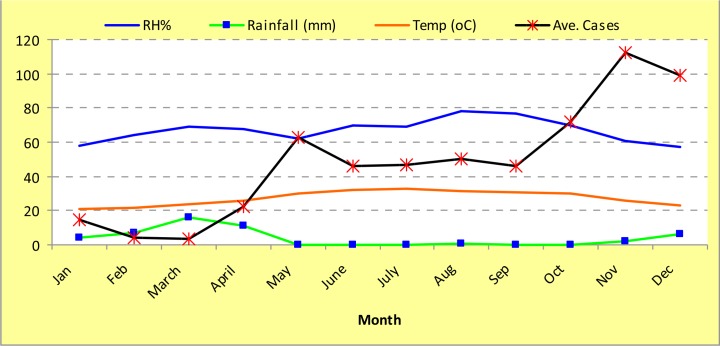
During April–May and October–November the temperature is between 25–30 °C with a relative humidity of more than 60% (Fig. 3), the suitable climatic factors for mosquito breeding and increasing longevity. Based on the unpublished reports of Jask health center, Anopheles stephensi and An. culicifacies seems to be the main vectors in the area. These species are active during the year due to favorite climatic conditions. There was no published entomological investigation in the Jask area for fauna, density, insecticide susceptibility and parasitic infection of Anopheline mosquitoes.
Fig. 3.
Average of malaria cases in relation to climatology parameters in Jask County, southeastern Iran, 2006–2010
The health facilities and personnel of the County were included: one urban heath center, 6 rural health centers, one sub health center, 27 health houses, one hospital, 11 physicians, 6 public health officers and 49 health care workers (Behvarz). Furthermore, malaria control program has had a total of 25 mobile teams.
Based on the national protocol, malaria control interventions in the area are including case detection and treatment, indoor residual spraying by Deltamethrin WP 10% in rural area with 90% coverage, distributing Long Lasting Insecticide impregnated Nets (LLINs) in rural areas with 80% coverage, as well as larviciding. Data obtained from the Jask County health center shows high IRS coverage during the study period and distribution of LLINs during 2009 and 2010. These vector control activities along with other measures such as good active case detection (Table 2) and increasing the financial resources of malaria control program for the study area are the main reasons for the decline of the disease.
Table 2.
Activities of malaria control program in Jask County, Southeastern Iran, 2006–2010
| Index |
Year
|
||||
|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | |
| Total No. of distributed LLINs | 0 | 0 | 0 | 3560 | 2660 |
| IRS coverage | No data | 95% | 93.2% | 93.8% | 95% |
| Active case detection | 687 | 879 | 335 | 118 | 87 |
| Mobil teams | 25 | 25 | 25 | 25 | 25 |
A total of 41 people (64.3% males, 35.7% females) participated in the KAP study, 96.4 % under 45 years old. The education level was categorized in four levels: illiterate (10.7%), primary school (32.1%), high school (25%), and university degree (32.1%). Among the respondents just 17.9% had a history of malaria infection. Most of the study population (82.1%) believed that mosquito bite is the transmission route of malaria and fever is the main symptom. When they asked about the role of insecticide treated bed net (ITNs) for prevention malaria, 67.9% answered yes, meanwhile 60.7% was agree that water storage utensils can increase the risk of malaria transmission. The attitude of respondent showed 28.6% and 39.3% were respectively agree and strongly agree with this fact that ITNs can prevent malaria transmission. These rates about using insecticide were 50% and 17.9%, respectively. In practice, 78.6% stated that they allow the spray men to spray their house, 96.4% will refer to the nearest health center as soon as their child feels feverish, but just 35.7% used ITNs during last year (Table 3).
Table 3.
KAP study on malaria, Jask Country, 2011
| Question | Answer | Frequency | Percent |
|---|---|---|---|
| Gender | Female | 10 | 35.7 |
| Male | 18 | 64.3 | |
|
| |||
| Age | 15–30 | 17 | 60.7 |
| 30–45 | 10 | 35.7 | |
| 45< | 1 | 3.6 | |
|
| |||
| Martial status | Single | 9 | 32.1 |
| Married | 18 | 64.3 | |
| Widow | 1 | 3.6 | |
|
| |||
| Education level | Illiterate | 3 | 10.7 |
| Primary/secondary | 9 | 32.1 | |
| High school | 7 | 25 | |
| University | 9 | 32.1 | |
|
| |||
| Job | Employed | 12 | 42.9 |
| Unemployed | 15 | 53.6 | |
| Retired | 1 | 3.6 | |
|
| |||
| History of malaria infection | Yes | 5 | 17.9 |
| No | 23 | 82.1 | |
|
| |||
| Transmission route | Air | 1 | 3.6 |
| Mosquito bite | 23 | 82.1 | |
| Food | 2 | 7.1 | |
| I don’t know | 2 | 7.1 | |
|
| |||
| Malaria symptoms | Fever | 23 | 82.1 |
| Cough | 4 | 14.3 | |
| Other | 1 | 3.6 | |
|
| |||
| Using insecticide treated bed nets can prevent us from getting Malaria | True | 19 | 67.9 |
| False | 6 | 21.4 | |
| I don’t know | 3 | 10.7 | |
|
| |||
| Storing water in utensils can increase the risk of malaria transmission | True | 17 | 60.7 |
| False | 6 | 21.4 | |
| I don’t know | 5 | 17.9 | |
|
| |||
| Using insecticide treated nets can prevent malaria transmission | Strongly disagree | 3 | 10.7 |
| Disagree | 2 | 7.1 | |
| Uncertain | 4 | 14.3 | |
| Agree | 8 | 28.6 | |
| Strongly agree | 11 | 39.3 | |
|
| |||
| Applying Insecticide Residual Spray can prevent malaria transmission | Disagree | 4 | 14.3 |
| Uncertain | 5 | 17.9 | |
| Agree | 14 | 50 | |
| Strongly agree | 5 | 17.9 | |
|
| |||
| The price of insecticide treated nets is low | Strongly disagree | 1 | 3.6 |
| Disagree | 3 | 10.7 | |
| Uncertain | 12 | 42.9 | |
| Agree | 11 | 39.3 | |
| Strongly agree | 1 | 3.6 | |
|
| |||
| Applying Insecticide Residual Spraying control malaria transmission, cannot contaminate our house | Strongly disagree | 2 | 7.1 |
| Disagree | 1 | 3.6 | |
| Uncertain | 7 | 25 | |
| Agree | 16 | 57.1 | |
| Strongly agree | 2 | 7.1 | |
|
| |||
| I allow the spray man to spray my home to prevent malaria transmission | Yes | 22 | 78.6 |
| No | 3 | 10.7 | |
| Don’t answer | 3 | 10.7 | |
|
| |||
| If my child feels feverish, I bring him/her to the nearest health center | Yes | 27 | 96.4 |
| No | 1 | 3.6 | |
|
| |||
| If I see a place with stagnant water around my house, I will prefer to | Add oil | 5 | 17.9 |
| Land filling or drainage | 19 | 67.9 | |
| leaving | 4 | 14.3 | |
|
| |||
| I used ITN for prevention of malaria in the last 1year | Yes | 10 | 35.7 |
| No | 18 | 64.3 | |
Discussion
Both P. vivax and P. falciparum are reported from the Jask County, although vivax malaria is dominant species. There is also report of malaria due to imported species P. malariae in Bandar Abbas, west of the study area, but this species in not common in Iran (Nateghpour et al. 2010b). Since drug resistance is reported from malaria parasites in Iran (Raeisi et al. 2006, Nateghpour et al. 2010a), it is suggested to do such a survey in Jask County for better understanding the situation of malaria and planning control programs in the area.
Although there is no published report on Anopheline mosquitoes of the study area, five malaria vectors including An. stephensi, An. culicifacies, An. dthali, An. superpictus and An. fluviatilis are reported to be active in Bashagard, adjacent to the north of Jask County (Hanafi-Bojd et al. 2012a,b). Among these species, An. stephensi and An. culicifacies were collected during the entomological activities of Jask health center. These two species are reported as main malaria vectors of south and southeastern parts of Iran (Vatandoost et al. 2006, Hanafi-Bojd et al. 2011a,b).
As it can be understood from the climatology chart (Fig. 3), the mosquito breeding can be done around the year, because of favorable condition. Therefore, a comprehensive entomological study on the fauna of Anopheline and their density during the year, their parasitic infection and susceptibility status to WHO recommended insecticides/ larvicides is suggested and should be included in malaria vector control activities in the area.
Regarding to our results, the knowledge, attitude and practice of the respondents was relatively good in malaria control and prevention, but needs to do more health education to improve their awareness. The relative good level of knowledge may be due to living people in an endemic area for malaria. The same results were obtained by Hanafi-Bojd et al. (2011a) in Bashagard County, north of the study area. Some other studies reported an increasing trend in literacy can be a protective factor for malaria morbidity (Koram 1989, Masoumi et al. 2003). One-third of the respondents in a KAP study in Baluchistan area, east of the Jask County, considered malaria as an important disease in the area, and more than 58% of them considered mosquitoes to be the cause of the malaria disease. So it can be concluded more contact with malaria rural areas resulted to more knowledge about the disease (Rakhshani et al. 2001).
Constraints and challenges seems to be: massive population movement between Iran, Pakistan and Afghanistan, vector control challenges at the County, inadequate skilled medical staff in malaria case management, weak inter-sectoral coordination for malaria control especially in urban areas, low socio-economical status of those who live in the area.
The most important immigrants in southeastern part of the country are illegal and so they pass the unofficial borders, their exact number and infection to infectious diseases including malaria is unknown. But it is necessary to plan for detection of asymptomatic cases that may act as the reservoir of the disease (Nateghpour et al. 2011, Turki et al. 2012).
Priority areas for malaria control in the study area are: strengthening malaria surveillance system in the County, developing integrated vector management strategy, strengthening vector control activities by larviciding at the County level, capacity buildings on prompt case detection and treatment in the immigrant population, supporting cross border coordination with Afghanistan and Pakistan, strengthening malaria early warning and early detection system and developing malaria epidemics preparedness plan based on a powerful database that should be established for the area. Therefore it is recommended to reinforce human capacity on malaria control activities at different levels of health personnel, strengthen the existing vector management program at the County level, establishing a spatial malaria database for the County and training ArcGIS to the malaria experts of the County to handle the database, developing and implementation a plan for malaria epidemics preparedness and response, build up malaria surveillance system with appropriate epidemic thresholds in epidemic-prone settings, support operational research in the field of malaria entomology and parasitology as well as insecticide resistance.
Conclusion
Malaria incidence had significant reduction during the study years. The main reason for this may be due to changing environmental condition for Anopheline breeding and survival because of drought. Another reason may be integration of vector management by using long lasting insecticide treated bed nets, active case detection and treatment by implementation of mobile teams and increasing in financial sources of malaria control program. Knowledge, attitude and practice of people were good in malaria control and prevention, but needs to do more activities for health education and awareness.
Acknowledgments
The authors are grateful to the kind personnel of the Jask County health center as well as Hormozgan Province Health Center authorities, for their collaboration during this study. This work is a part of field exercise in 13th International Diploma Course on Malaria Planning and Management that was held out by collaboration of World Health Organization, Tehran University of Medical Sciences, Ministry of Health and National Institute of Health Research (Bandar Abbas Station as WHO Regional Malaria Training Centre) in 2011. The authors declare that there is no conflict of interest.
References
- Hanafi-Bojd AA, Vatandoost H, Philip E, Stepanova E, Abdi AI, Safari R, Mohseni Gh, Bruhi MI, Peter A, Abdulrazag Sh, Mangal G. Malaria situation analysis and stratification in Bandar Abbas County, Southern Iran, 2004–2008. Iran J Arthropod-Borne Dis. 2010;4(1):31–41. [PMC free article] [PubMed] [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Oshaghi MA, Eshraghian MR, Haghdoost AA, Abedi F, Zamani G, Sedaghat MM, Rashidian A, Madani AH, Raeisi A. Knowledge, attitudes and practices regarding malaria control in an endemic area of Southeastern Iran. Southeast Asian J Trop Med Publ Health. 2011a;42(3):491–501. [PubMed] [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Oshaghi MA, Haghdoost AA, Shahi M, Sedaghat MM, Abedi F, Yeryan M, Pakari A. Entomological and epidemiological attributes for malaria transmission and implementation of vector control in southern Iran. Acta Trop. 2012a;121:85–92. doi: 10.1016/j.actatropica.2011.04.017. [DOI] [PubMed] [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Oshaghi MA, Charrahy Z, Haghdoost AA, Sedaghat MM, Abedi F, Soltani M, Raeisi A. Larval habitats and biodiversity of anopheline mosquitoes (Diptera: Culicidae) in a malarious area of southern Iran. J Vector Borne Dis. 2012b;49:91–100. [PubMed] [Google Scholar]
- Koram KA. Socioeconomic determinants are not major risk factors for severe malaria in Gambian children. Trans R Soc Trop Med Hyg. 1989;89:151–154. doi: 10.1016/0035-9203(95)90472-7. [DOI] [PubMed] [Google Scholar]
- Masoumi AH, Motabar M, Zamani Gh, Naserinejad D, Vatandoost H. A case-control study of determinative factors on malaria morbidity in Minab, Jask and Roodan counties, in Hormozgan Province, southern Iran, 2001. Iran J Public Health. 2003;32:14–18. [Google Scholar]
- McKelvie WR, Haghdoost AA, Raeisi A. Defining and detecting malaria epidemics in south-east. Iran Malaria J. 2012;11:81. doi: 10.1186/1475-2875-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesdaghinia AR, Vatandoost H, Hanafi-Bojd AA, Majdzadeh R, Raeisi A. Conducting international diploma course on malaria program planning and management 1996–2012. J Arthropod-Borne Dis. 2013;7(2):100–112. [PMC free article] [PubMed] [Google Scholar]
- Nateghpour M, Ayazian Mavi S, Keshavarz H, Rezaei S, Abedi F, Edrissian GH, Raeisi A. Molecular monitoring of Plasmodium vivax infection after radical treatment in Southeastern Iran. Iran J Arthropod-Borne Dis. 2010a;4(1):24–30. [PMC free article] [PubMed] [Google Scholar]
- Nateghpour M, Makiani MJ, Mohseni G, Safari R, Hajjaran H, Ataei S. First case of imported Plasmodium ovale from Iran. Iran J Med Sci. 2010b;35(3):264–266. [Google Scholar]
- Nateghpour M, Akbarzadeh K, Farivar L, Amiri A. Detection of asymptomatic malaria infection among the Afghani immigrant population in Iranshahr district of southeastern Iran. Bull Soc Path Exot. 2011;104(4):321–323. doi: 10.1007/s13149-011-0134-8. [DOI] [PubMed] [Google Scholar]
- Raeisi A, Ringwald P, Safa O, Shahbazi A, Ranjbar M, Keshavarz H, Nateghpour M, Faraji L. Monitoring of the therapeutic efficacy of chloroquine for the treatment of uncomplicated, Plasmodium falciparum malaria in Iran. Annals Trop Med Parasitol. 2006;100(1):11–16. doi: 10.1179/136485906X86220. [DOI] [PubMed] [Google Scholar]
- Rakhshani F, Moghadam AR, Alami R. Knowledge, attitude and practice of Baluchestan women about Malaria. Tabib-e-Shargh. J Zahedan Univ Med Sci. 2001;1:15–29. [Google Scholar]
- Rakhshani F, Ansari Moghadam AR, Alemi R, Moradi A. Knowledge, perceptions and prevention of malaria among women in Sistan va Baluchestan, Islamic Republic of Iran. East Mediterr Health J. 2003;9(3):248–256. [PubMed] [Google Scholar]
- Salehi M, Amirmajdi MM, Mashhadi IE, Hakemi Y, Mashhadi AE, Mirinezhad A. Analysis of malaria epidemic features in Sistan and Baluchistan Province, Southeast of Iran, 2005–2008. Iran Red Crescent Med J. 2010;12(3):247–253. [Google Scholar]
- Turki H, Zoghi S, Mehrizi AA, Zakeri S, Raeisi A, Khazan H, Haghdoost AA. Absence of asymptomatic malaria infection in endemic area of Bashagard district, Hormozgan Province, Iran. Iran J Parasitol. 2012;7(1):36–44. [PMC free article] [PubMed] [Google Scholar]
- Vatandoost H, Oshaghi MA, Abaie MR, Shahi M, Yaghoobi F, Baghaii M, Hanafi-Bojd AA, Zamani G, Townson H. Bionomics of Anopheles stephensi Liston in the malarious area of Hormozgan Province, southern Iran, 2002. Acta Trop. 2006;97:196–203. doi: 10.1016/j.actatropica.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Vatandoost H, Akbarzadeh K, Hanafi-Bojd AA, Mashayekhi M, Saffari M, Malik F, Kenyi L, Abakar JB, Busaq A, Esmailpour M, Hassen A, Oshaghi MA. Malaria stratification in a malarious area, a field exercise. Asian Pac J Trop Med. 2010;3(10):807–811. [Google Scholar]
- Vatandoost H, Rashidian A, Jafari M, Raeisi A, Hanafi-Bojd AA, Yousofzai AW, Daryanavard A, Mojahedi AR, Pakari A. Demonstration of malaria situation analysis, stratification and planning in Minab District, southern Iran. Asian Pac J Trop Med. 2011;4:67–71. doi: 10.1016/S1995-7645(11)60036-9. [DOI] [PubMed] [Google Scholar]
- WHO . The World Malaria Report. Geneva: 2011a. [Google Scholar]
- WHO . Global Malaria Programme. Geneva: 2011b. Planning and managing malaria control programmes, guide for participants. [Google Scholar]
- Zoghi S, Mehrizi AA, Raeisi A, Haghdoost AA, Turki H, Safari R, Ahmadi Kahanali A, Zakeri S. Survey for asymptomatic malaria cases in low transmission settings of Iran under elimination programme. Malaria J. 2012;126 doi: 10.1186/1475-2875-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youssefi MR, Rahimi MT. Prevalence of malaria infection in Sarbaz, Sistan and Bluchistan Province. Asian Pac J Trop Biomed. 2011;1(6):491–492. doi: 10.1016/S2221-1691(11)60107-X. [DOI] [PMC free article] [PubMed] [Google Scholar]