Abstract
Background: Dose assessment using proper dosimeters is especially important in radiation protection optimization and imaging justification in diagnostic radiology.
Objective: The aim of this study is to obtain the Entrance Skin Dose (ESD) of patients undergoing lumbar spine imaging using two thermoluminescence dosimeters TLD-100 (LiF: Mg, Ti) and GR-200 (LiF: Mg, Cu, P) and also to obtain the absorbed dose to different organs in lumbar spine imaging with several views.
Methods: To measure the ESD values of the patients undergoing lumbar spine imaging, the two TLD types were put on their skin surface. The ESD values for different views of lumbar spine imaging were also measured by putting the TLDs at the surface of the Rando phantom. Several TLD chips were inserted inside different organs of Rando phantom to measure the absorbed dose to different organs in lumbar spine imaging.
Results: The results indicate that there is a close agreement between the results of the two dosimeters. Based on the results of this experiment, the ESD dose of the 16 patients included in this study varied between 2.71 mGy and 26.29 mGy with the average of 11.89 mGy for TLD-100, and between 2.55 mGy and 27.41 mGy with the average of 12.32 mGy for GR-200 measurements. The ESDs obtained by putting the two types of TLDs at the surface of Rando phantom are in close agreement.
Conclusion: According to the results, the GR200 has greater sensitivity than the TLD-100.
Keywords: Entrance Skin Dose, TLD-100, Rando phantom
Introduction
Accurate knowledge of the entrance surface dose (ESD) of the patients undergoing diagnostic radiology, as a part of quality control and quality assurance programs in medical programs, would be helpful in optimization of the patient protection and setting standards of good practice worldwide. Different investigations have been performed on the measurement of the ESD or organ dose in radiology [1-6].
Risk assessment is not possible without the mean absorbed doses to organs. The International Commission of Radiation Protection has recommended the dose measurement in sensitive organs, for stochastic radiation effects [7].
Lumbar spine imaging is a common radiology procedure which is usually requested in several views. Therefore the optimization of patient protection and justification of radiography techniques are necessary to lessen the need to repeat the imaging process, and decreasing the dose to patients. The ESD or organ dose measurements in lumbar spine x-ray imaging in AP and lateral views have been the subject of numerous studies[8, 9].
Thermoluminescence dosimetry has been the method of choice of different investigators for dose measurement in clinical practices with low energy X-ray imaging[2, 10-12].
Thermoluminescence dosimetry using standard TLD-100 is known as an effective means for dose measurement in medical exposures. In addition, the tissue equivalent GR-200 has been found to be an ideal dosimeter in environmental and medical dosimetry.
The aim of this study is to investigate the entrance surface dose (ESD) for the patients undergoing lumbar spine imaging using two kinds of thermoluminescence dosimeters (LiF: Mg, Ti, and LiF: Mg, Cu, P). Finally, the ESD and the absorbed doses to different organs were measured by TLD-100 chips inside the Alderson RANDO phantom.
Materials and Methods
Thermoluminescence dosimetry
The Entrance Skin Dose (ESD) of the patients undergoing lumbar spine imaging were measured using Li-F Thermoluminescence dosimeters (LiF: Mg, Ti, and LiF: Mg, Cu, P chips).
Each TLD100 cubical chip used in this study has a dimension of about 3*3*1 mm3, while each cylindrical GR-200 chip has a diameter of 4 mm with 1mm thickness.
The chips were annealed using standard procedures (see table 1) [6, 13]. The irradiated TLDs were read using a Harshaw Model 4500 TLD reader (Harshaw, Bicron USA). Each kind of TLD chip was read out by a special time temperature profile (TTP). The TTPs used in this study for reading out the TLD-100, and GR-200 dosimeters are found in table 2. The following equation was used to correct the TLD responses.
Table 1.
Annealing procedure used for TLD-100, and GR-200 dosimeters
| Dosimeter | Annealing procedure |
|---|---|
| TLD-100 |
1hour at 400°c 20 hours at 80°c |
| GR-200 | 10 minutes at 240°c |
Table 2.
Time temperature profile used for reading out TLD-100, and GR-200 chips
| Dosimeter | TTP | |
|---|---|---|
| TLD-100 | Preheat | |
| Temp (◦C) | 50 | |
| Time (sec) | 0 | |
| Acquisition | ||
| Max Temp(◦C) | 300 | |
| Time (sec) | 13.33 | |
| Rate (◦C/sec) | 25 | |
| Anneal | ||
| Temp (◦C) | 0 | |
| Time (sec) | 0 | |
| GR-200 | Preheat | |
| Temp (◦C) | 135 | |
| Time (sec) | 5 | |
| Acquisition | ||
| Max Temp (◦C) | 240 | |
| Time (sec) | 13 | |
| Rate (◦C/sec) | 20 | |
| Anneal | ||
| Temp (◦C) | 0 | |
| Time (sec) | 0 | |
Where Rcorrected is the corrected response of the TLD chips, Rchip is the TLD reading (in nc), Rbg is the average of the readings of the chips used for background measurement, and the ECC is the Element Correction Coefficient of each chip or the pre-determined chip factors.
To determine the ECC factor of each chip, all TLD chips were exposed to a specific amount of dose, and then the ECCs were obtained by dividing the average value of the readings by the reading of each TLD. The Rcorrected values were then converted to the dose (mGy) using the calibration curves. To obtain the calibration curves, thin, dark plastic covers were prepared to accommodate three chips, these pockets were then exposed to different amounts of doses and the calibration curve was drawn. Two calibration curves were drawn for TLD-100, and GR-200 dosimeters separately. The two curves were then used for derive the dose values (mGy) from the corrected readings Rcorrected (in nc).
Patient dosimetry
To obtain the ESD of the patients undergoing lumbar spine imaging, the tissue equivalent pockets including annealed TLD chips were put at the surface of their body. The ESD values were obtained for 16 patients in two of the biggest radiology sections of Shiraz city in Iran. The results of dosimetry obtained by TLD-100 chips were compared with those obtained by GR-200.
Dose measurements using Alderson Rando Phantom
The Alderson Rando phantom
The Alderson Rando Phantom was used in this study for Entrance Skin Dose (ESD) and organ dose measurements using thermoluminescence dosimetry. This phantom contains lung, natural human skeleton embedded in a tissue equivalent urethane rubber. It contains horizontal slabs; each contains a matrix of holes, 5mm in diameter, filled with removable wax plug.
Dose measurements
To measure the ESD and organ doses in lumbar spine imaging, the Rando phantom was exposed to the x-ray produced by different radiography techniques. The wax plugs in some slabs, containing uterus, kidney, and spine, were removed to accommodate the plugs containing TLD-100 chips for measurement of organ doses. The TLD-100 chips were inserted in different slabs of the phantom inside the kidney, uterus, and tissue around the spine and then the phantom was exposed to X-ray radiation for lumbar spine imaging.
For the purpose of ESD measurements, each three annealed TLD-100 chips, with approximately similar ECC values, were put in a dark, thin plastic pocket. Each time the phantom was exposed to radiation for lumbar spine imaging, one of the pockets was put on the phantom surface, and finally the average of the doses of the three chips was used as the ESD. To compare the response of GR-200 TLD chips with TLD-100 chips, the measurements of ESD were repeated using the GR-200. This time the RTI SoliDose model 400 instrument was used for active measurement of the entrance surface dose, the probe of this instrument was placed in the same position as the thermoluminescence dosimeters to measure the dose in each imaging process.
Results and Discussions
TLD calibration curves
The calibration curves of TLD-100 and GR-200 dosimeters show that responses of both of the TLD types are linear. The sensitivity (nc per unit dose) of each TLD type can be obtained according to the following relationship.
The results indicate that the sensitivity of the GR-200 chips (1/0.002=500) is much more than that of TLD-100 (1/0.142=7.04).
The results of patient dosimetry
Table 3 compares the sum of the patient’s doses in imaging with several views obtained by TLD-100 and GR-200 dosimeters. The number of views and the imaging technique used for each dosimeter are also shown in the table.
Table 3.
Comparison of the dose measured by LiF
| Patient | # of views | kVP | mAs |
Dose (mGy)
LiF: Mg, Cu, P (GR-200) |
Dose (mGy)
LiF: Mg, Ti (TLD-100) |
%difference
(GR200 Dose-TLD100 Dose)*100/ GR200 Dose |
|---|---|---|---|---|---|---|
| 1 | 2 | 70 | 40 | 15.00 | 15.89 | -5.93% |
| 70 | 64 | |||||
| 2 | 3 | 80 | 50 | 17.87 | 17.22 | 3.64% |
| 80 | 63 | |||||
| 80 | 63 | |||||
| 3 | 5 | 66 | 40 | 25.99 | 23.41 | 9.93% |
| 86 | 50 | |||||
| 86 | 50 | |||||
| 72 | 64 | |||||
| 72 | 64 | |||||
| 4 | 2 | 70 | 56 | 11.80 | 11.29 | 4.32% |
| 85 | 71 | |||||
| 5 | 2 | 63 | 40 | 8.78 | 8.49 | 3.30% |
| 66 | 64 | |||||
| 6 | 2 | 66 | 28 | 8.80 | 8.72 | 0.91% |
| 69 | 71 | |||||
| 7 | 2 | 67 | 50 | 5.27 | 4.81 | 8.73% |
| 75 | 64 | |||||
| 8 | 2 | 64 | 20 | 5.01 | 5.49 | -9.58% |
| 68 | 32 | |||||
| 9 | 2 | 63 | 40 | 9.62 | 9.48 | 1.46% |
| 66 | 64 | |||||
| 10 | 2 | 73 | 50 | 11.60 | 11.05 | 4.74% |
| 71 | 80 | |||||
| 11 | 4 | 86 | 50 | 14.55 | 12.88 | 11.48% |
| 86 | 50 | |||||
| 69 | 64 | |||||
| 69 | 64 | |||||
| 12 | 5 | 79 | 64 | 19.23 | 18.22 | 5.25% |
| 79 | 50 | |||||
| 65 | 32 | |||||
| 73 | 40 | |||||
| 73 | 40 | |||||
| 13 | 5 | 73 | 64 | 27.41 | 26.29 | 4.09% |
| 90 | 64 | |||||
| 90 | 64 | |||||
| 72 | 80 | |||||
| 72 | 80 | |||||
| 14 | 1 | 64 | 32 | 2.55 | 2.71 | -6.27% |
| 15 | 2 | 54 | 25 | 4.50 | 4.65 | -3.33% |
| 59 | 32 | |||||
| 16 | 2 | 60 | 40 | 9.16 | 9.65 | -5.35% |
| 66 | 63 |
Dosimetry using RANDO phantom
ESD measurements
ESD was measured by putting the TLD-100 and GR-200 chips on the surface of the RANDO phantom. Table 4 demonstrates the dose measured by three methods (using TLD-100, GR-200, and SoliDose) for single view images (AP or Lateral) obtained by different imaging techniques (kV & mAs).
Table 4.
The entrance surface dose on the surface of Rando phantom, for single view images.
| Measurement | View | kVp | mAs | (TLD-100) (mGy) | (GR-200) (mGy) |
Dose
(SOLIDOSE) |
|---|---|---|---|---|---|---|
| 1 | AP | 68 | 64 | 3.55 | 3.43 | 3.36 |
| 2 | AP | 72 | 64 | 3.84 | 3.74 | 3.76 |
| 3 | AP | 70 | 80 | 4.37 | 4.79 | 4.46 |
| 4 | Lateral | 80 | 80 | 6.63 | 5.96 | 6.34 |
| 5 | Lateral | 85 | 80 | 6.67 | 6.61 | 7.14 |
| 6 | Lateral | 80 | 80 | 7.24 | 7.38 | 8.02 |
Comparison of the ESD values for 2, 4, and 5 view images, obtained by TLD-100, GR-200, and SoliDose, are shown in table 5. The percentage differences between the three above-mentioned methods are shown in figure 1.
Table 5.
The entrance surface dose on the surface of Rando phantom, for multiple view images.
| Measurement | # of views | View | kVp | mAs |
Dose
(TLD-100) (mGy) |
Dose
(GR-200) (mGy) |
Dose (SOLIDOSE) (mGy) |
|---|---|---|---|---|---|---|---|
| 1 | 5 | AP | 68 | 64 | ------ | ------ | 3.68 |
| Lateral | 80 | 80 | ------ | ------ | 6.76 | ||
| Lateral | 80 | 80 | ------ | ------ | 6.76 | ||
| Oblique | 75 | 80 | ------ | ------ | 5.68 | ||
| Oblique | 75 | 80 | ------ | ------ | 5.68 | ||
| Total Dose in 5 views | ---- | ---- | 30.73 | 29.02 | 28.56 | ||
| 2 | 4 | AP | 68 | 64 | ------ | ------ | 3.74 |
| Lateral | 80 | 80 | ------ | ------ | 6.82 | ||
| Oblique | 75 | 80 | ------ | ------ | 5.56 | ||
| Oblique | 75 | 80 | ------ | ------ | 5.56 | ||
| Total Dose in 4 views | ---- | ---- | 23.40 | 21.46 | 21.66 | ||
| 3 | 2 | AP | 68 | 64 | ------ | ------ | 3.70 |
| Lateral | 80 | 80 | ------ | ------ | 6.38 | ||
| Total Dose in 2 views | ---- | ---- | 9.87 | 10.46 | 10.08 |
Figure 1.
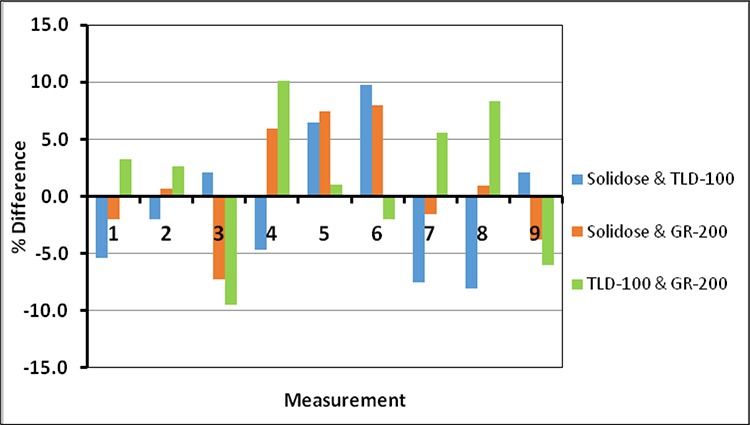
Percentage difference between the dose measured by TLD-100, GR-200, and SoliDose
Absorbed doses to different organs
The minimum, maximum, and average absorbed doses to each organ, measured by TLD-100 dosimeter, in 2, 4, and 5 view imaging are shown in table 6.
Table 6.
The minimum, maximum, and average absorbed doses to each organ
| Number of views | Organ |
(Min, max)
absorbed dose (mGy) |
Mean absorbed dose
(mGy) |
|
|---|---|---|---|---|
| 5 |
AP Lateral Lateral Oblique Oblique |
Kidney | (0.48-4.86) | 2.3 |
| Uterus | (0.94-7.62) | 3.2 | ||
| Soft tissue around spine | (1.7-2.50) | 2 |
Uncertainty analysis of TL dosimetry
The uncertainty analysis for TLD-100 and GR-200 dosimetries is shown in tables 7 and 8 respectively. As can be seen from the tables, the quadrature combination of statistical uncertainties (type A) due to repetitive TLD measurements is found to be 5%, and 4% for TLD-100 and GR-200 respectively. Thus the total uncertainties for these dosimeters are calculated as 7.14%, and 6.48% respectively.
Table 7.
Uncertainty analysis of TLD-100 results.
| Component of uncertainty |
Type A
(%) |
Type B
(%) |
|---|---|---|
| Repetitive TLD measurements | 5.0 | ___ |
| TLD dose calibration | ___ | 5.0 |
| Correction for energy dependence of TLD | ___ | 0 |
| TLD positioning | ___ | 1.0 |
| Quadrature combination | 5.0 | 5.1 |
| Total uncertainty | 7.14 | |
Table 8.
Uncertainty analysis of GR-200 results.
| Component of uncertainty |
Type A
(%) |
Type B
(%) |
|---|---|---|
| Repetitive TLD measurements | 4.0 | ___ |
| TLD dose calibration | ___ | 5.0 |
| Correction for energy dependence of TLD | ___ | 0 |
| TLD positioning | ___ | 1.0 |
| Quadrature combination | 4.0 | 5.1 |
| Total uncertainty | 6.48 | |
Comparison with the previous investigations
The results shown in table 5 were used to obtain the dose per view in the images with several views. The results of table 4 were also used to obtain the dose per view in different projections (AP or Lateral). Table 9 compares the results obtained in this study with the results of other investigations.
Table 9.
Comparison of the results with other investigations.
| Measurement method |
ESD per view
(mGy) |
Projection | Examination |
DRL
(mGy) Per view |
Country | Reference | |
|---|---|---|---|---|---|---|---|
| 1 | TLD-100 | 5.64 | All projections | Lumbar spine | ------- | Iran | This work |
| GR-200 | 5.46 | ||||||
| Solidose 400 | 5.4 | ||||||
| 2 | TLD-100 | 3.92 | AP | Lumbar spine | ------- | Iran | This work |
| GR-200 | 3.98 | ||||||
| Solidose 400 | 3.86 | ||||||
| 3 | TLD-100 | 6.84 | Lateral | Lumbar spine | Iran | This work | |
| GR-200 | 6.64 | ||||||
| Solidose 400 | 7.16 | ||||||
| 4 | ------- | ------- | AP | Lumbar spine | 5 | UK | [14] |
| 5 | ------- | ------- | Lateral | Lumbar spine | 11 | UK | [14] |
| 5 | ------- | ------- | AP | Lumbar spine | 8 | Ireland | [15] |
| 6 | -------- | ------- | Lateral | Lumbar spine | 24 | Ireland | [15] |
Conclusion
The measurements of entrance surface dose (ESD) and the organ dose in lumbar spine imaging were performed using thermoluminescence dosimetry. The LiF: Mg, Ti, and LiF: Mg, Cu, P TLD chips were used for dose measurement in this study. The results indicate that both TLD types are applicable in dose measurement in low dose fields. The comparison between the results of the two TLDs show that the LiF: Mg, Cu, P TLDs have higher sensitivity (i.e. nc per unit dose) than the LiF: Mg, Ti chips.
Conflict of Interest: None
References
- 1.Mooney R, Thomas PS. Dose reduction in a paediatric X-ray department following optimization of radiographic technique. Br J Radiol. 1998;71(848):852–60. doi: 10.1259/bjr.71.848.9828798. doi: 10.1259/bjr.71.848.9828798. PubMed PMID: 9828798. [DOI] [PubMed] [Google Scholar]
- 2.Duggan L, Warren-Forward H, Smith T, Kron T. Investigation of dose reduction in neonatal radiography using specially designed phantoms and LiF: Mg, Cu, P TLDs. Br J Radiol. 2003;76(904): 232–7. doi: 10.1259/bjr/79291075. doi: 10.1259/bjr/79291075. PubMed PMID: 12711642. [DOI] [PubMed] [Google Scholar]
- 3.Omrane LB, Verhaegen F, Chahed N, Mtimet S. An investigation of entrance surface dose calculations for diagnostic radiology using Monte Carlo simulations and radiotherapy dosimetry formalisms. Phys Med Biol. 2003;48(12):1809–24. doi: 10.1088/0031-9155/48/12/310. doi:10.1088/0031-9155/48/12/310. PubMed PMID: 12870585. [DOI] [PubMed] [Google Scholar]
- 4.Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M. Effective Doses in Radiology and Diagnostic Nuclear Medicine: A Catalog. Radiology. 2008;248(1):254–63. doi: 10.1148/radiol.2481071451. doi: 10.1148/radiol.2481071451. PubMed PMID: 18566177. [DOI] [PubMed] [Google Scholar]
- 5.Theocharopoulos N, Perisinakis K, Damilakis J, Varveris H, Gourtsoyiannis N. Comparison of four methods for assessing patient effective dose from radiological examinations. Med Phys. 2002;29(9):2070–9. doi: 10.1118/1.1500769. doi: 10.1118/1.1500769. PubMed PMID: 12349928. [DOI] [PubMed] [Google Scholar]
- 6.Faghihi R, Mehdizadeh S, Sina S, Alizadeh FN, Zeinali B, Kamyab GR, et al. Radiation dose to neonates undergoing X-ray imaging in special care baby units in Iran. Radiat Prot Dosimetry. 2012;150(1):55–9. doi: 10.1093/rpd/ncr373. doi: 10.1093/rpd/ncr373. PubMed PMID: 22128357. [DOI] [PubMed] [Google Scholar]
- 7.1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991;21(1-3):1–201. PubMed PMID: 2053748. [PubMed] [Google Scholar]
- 8.Niittymaki H, Hakanen A, Rautio S, Jarvinen H. Portable TL dosemeter--ESD phantom combination for chest and lumbar spine radiography. Radiat Prot Dosimetry. 2008;130(2):224–7. doi: 10.1093/rpd/ncm492. doi: 10.1093/rpd/ncm492. PubMed PMID: 18204082. [DOI] [PubMed] [Google Scholar]
- 9.Simpson AK, Whang PG, Jonisch A, Haims A, Grauer JN. The radiation exposure associated with cervical and lumbar spine radiographs. J Spinal Disord Tech. 2008;21(6):409–12. doi: 10.1097/BSD.0b013e3181568656. doi: 10.1097/BSD.0b013e3181568656. PubMed PMID: 18679095. [DOI] [PubMed] [Google Scholar]
- 10.Fung KK, Gilboy WB. The effect of beam tube potential variation on gonad dose to patients during chest radiography investigated using high sensitivity LiF: Mg, Cu, P thermoluminescent dosemeters. Br J Radiol. 2001;74(880):358–67. doi: 10.1259/bjr.74.880.740358. doi: 10.1259/bjr.74.880.740358. PubMed PMID: 11387155. [DOI] [PubMed] [Google Scholar]
- 11.Edwards CR, Mountford PJ, Green S, Palethorpe JE, Moloney AJ. The low energy X-ray response of the LiF: Mg: Cu: P thermoluminescent dosemeter: a comparison with LiF: Mg: Ti. Br J Radiol. 2005;78(930):543–7. doi: 10.1259/bjr/73133162. doi: 10.1259/bjr/73133162. PubMed PMID: 15900061. [DOI] [PubMed] [Google Scholar]
- 12.Duggan L, Hood C, Warren-Forward H, Haque M, Kron T. Variations in dose response with x-ray energy of LiF: Mg, Cu, P thermoluminescence dosimeters: implications for clinical dosimetry. Phys Med Biol. 2004;49(17):3831–45. doi: 10.1088/0031-9155/49/17/001. doi:10.1088/0031-9155/49/17/001. PubMed PMID: 15470908. [DOI] [PubMed] [Google Scholar]
- 13.Hood C, Duggan L, Bazley S, Denham J, Budzanowski M, Kron T. LiF: Mg, Cu, P'pin worms': miniature detectors for brachytherapy dosimetry. Radiat Prot Dosimetry. 2002;101(1-4):407–10. doi: 10.1093/oxfordjournals.rpd.a006012. PubMed PMID: 12382778. [DOI] [PubMed] [Google Scholar]
- 14.Hart D, Hillier MC, Wall BF. National reference doses for common radiographic, fluoroscopic and dental X-ray examinations in the UK. Br J Radiol. 2009;82(973):1–12. doi: 10.1259/bjr/12568539. doi: 10.1259/bjr/12568539. PubMed PMID: 18852213. [DOI] [PubMed] [Google Scholar]
- 15.Johnston DA, Brennan PC. Reference dose levels for patients undergoing common diagnostic X-ray examinations in Irish hospitals. Br J Radiol. 2000;73(868):396–402. doi: 10.1259/bjr.73.868.10844865. doi: 10.1259/bjr.73.868.10844865. PubMed PMID: 10844865. [DOI] [PubMed] [Google Scholar]


