Abstract
Animal models of antibody-mediated rejection (ABMR) may provide important evidence supporting proof of concept. We elicited donor-specific antibodies (DSA) by transfusion of donor blood (Brown Norway RT1n) into a complete mismatch recipient (Lewis RT1l) 3 weeks prior to kidney transplantation. Sensitized recipients had increased anti-donor splenocyte IgG1, IgG2b and IgG2c DSA 1 week after transplantation. Histopathology was consistent with ABMR characterized by diffuse peritubular capillary C4d and moderate microvascular inflammation with peritubular capillaritis + glomerulitis > 2. Immunofluorescence studies of kidney allograft tissue demonstrated a greater CD68/CD3 ratio in sensitized animals, primarily of the M1 (pro-inflammatory) phenotype, consistent with cytokine gene analyses that demonstrated a predominant T helper (TH)1 (interferon-γ, IL-2) profile. Immunoblot analyses confirmed the activation of the M1 macrophage phenotype as interferon regulatory factor 5, inducible nitric oxide synthase and phagocytic NADPH oxidase 2 were significantly up-regulated. Clinical biopsy samples in sensitized patients with acute ABMR confirmed the dominance of M1 macrophage phenotype in humans. Despite the absence of tubulitis, we were unable to exclude the effects of T cell–mediated rejection. These studies suggest that M1 macrophages and TH1 cytokines play an important role in the pathogenesis of acute mixed rejection in sensitized allograft recipients.
Keywords: Animal model, antibody-mediated rejection, C4d, donor-specific antibody, phenotype, transfusion
Introduction
Antibody-mediated injury has reached epidemic proportions in kidney transplantation. Preformed donor-specific antibodies (DSA) are associated with a delay in transplant rates and poor outcomes, and de novo DSA are associated with reduced graft and patient survival after transplantation (1,2). Recent studies suggest that antibody-mediated rejection (ABMR) is the most important cause of allograft loss following kidney transplantation (3,4). The first description of acute ABMR identified two distinct features: neutrophils in peritubular capillaries (PTC) and de novo anti-donor HLA Class I antibodies (5,6). Around the same time, C4d, a degradation product of the complement pathway that binds covalently to the endothelium, was identified as a stable marker of anti-donor humoral activity (7,8). Subsequently, the correlation between DSA, histologic findings of acute or chronic tissue injury, and C4d deposition in the PTC were described as acute or chronic active ABMR by the Banff 2009 consensus (9), and were recently revised by the Banff 2013 work group (10). In this new definition, C4d staining is not an absolute requirement for the diagnosis of ABMR. Instead, emphasis is placed on the evidence of current/recent antibody interaction with vascular endothelium, which includes C4d staining, microvascular inflammation (peritubular capillaritis [ptc] + glomerulitis [g] score ≥ 2), and increased expression of endothelial activation and injury transcripts (ENDATs), or other gene expression markers of endothelial injury in the biopsy tissue if thoroughly validated.
Although the cellular and molecular pathways that regulate ABMR are still under investigation, new knowledge of humoral immunobiology indicate that B cell and plasma cell activation results in the generation of DSA, which bind to HLA or non-HLA molecules on the endothelium (11–14). In the acute setting, antibody binding to endothelium and subsequent cellular activation involving complement-dependent and -independent pathways leads to the recruitment of natural killer (NK) cells, T cells, polymorphonuclear neutrophils and macrophages, which contribute to capillaritis and tissue injury (11–14). Macrophages have been identified in biopsies with glomerulitis, endothelialitis and intimal arteritis (15). These infiltrates may be facilitated during ABMR by macrophage Fc receptors (FcRs) engaging DSA bound to the endothelium, as well as binding to complement split products C3a and C5a, both potent chemoattractants. Accumulation of monocytes and macrophages in the glomeruli or PTC is associated with poor outcomes in ABMR (16,17). Macrophages can be classified into two major functional subsets: classically activated (M1), which after stimulation by lipopolysaccharide or interferon gamma (IFN-γ) are characterized by anti-microbial and cytotoxic properties; and alternatively activated (M2), which after exposure to T helper (TH) 2 cytokines such as IL-4 and IL-10 are involved in fibrosis, tissue repair and resolution of inflammation (18). Most likely, these phenotypes have a range of overlapping activities, with classically activated, wound-healing and regulatory macrophage occupying different points along the spectrum (18). Further studies are needed to understand the mechanisms of macrophage-mediated injury, explore their potential reparative role and determine if they or their functional products are biomarkers of poor graft outcomes (17).
Animal models of ABMR may provide important evidence supporting proof of concept, and a better understanding of the cellular and molecular pathways that regulate this process (19). In this article, we describe a new rat model in which transfusion elicits DSA, resulting in ABMR. The model replicates many aspects of human ABMR including DSA that activate complement, a massive influx of macrophages and an inflammatory environment that promotes M1 macrophage development. We can now uncover mechanisms of DSA development and understand potential areas of intervention to prevent or alleviate this major cause of chronic kidney rejection.
Materials and Methods
Animals
Adult (200–250 g) male Lewis (RT1l) and Brown Norway (BN) (RT1n) rats were purchased from Harlan Laboratories (Madison, WI) and were housed in the animal care facility at the William S. Middleton VA Hospital in Madison, WI. All procedures including kidney transplants were performed in accordance with the Animal Care and Use Policies at the VA Hospital and University of Wisconsin as described previously (20–22). Rats were randomized into six treatment groups: no treatment (C), donor-specific transfusion alone (Tn) in which Lewis rats were transfused intravenously with 0.5 mL of heparinized whole blood from BN rats; BN to Lewis transplant with cyclosporine A (TxCsA, CsA 10 mg/kg/day); transfusion followed 3 weeks later by transplant and CsA (TnTxCsA); transplant without CsA treatment (Tx) and transfusion followed 3 weeks later by transplant without CsA treatment (TnTx) (Table 1).
Table 1.
Experimental design and kidney function 1 week after transplant1
| Group | Transfusion | Transplant | Immunosuppression | BUN (mg/dL) | Scr (mg/dL) |
|---|---|---|---|---|---|
| Control (C) | − | − | − | 21.90 ± 2.37 | 0.32 ± 0.08 |
| Transfusion alone (Tn) | + | − | − | 21.46 ± 1.38 | 0.24 ± 0.14 |
| Transplant + CsA (TxCsA) | − | + | CsA (10 mg/kg/day × 7 days) | 39.42 ± 9.322 | 0.57 ± 0.222 |
| TnTxCsA | + | + | CsA (10 mg/kg/day × 7 days) | 51.80 ± 12.952 | 0.76 ± 0.312 |
| Tx | − | + | − | 253.27 ± 46.052 | 3.97 ± 1.202 |
| TnTx | + | + | − | 54.42 ± 15.032 | 1.03 ± 0.502 |
BUN, blood urea nitrogen; Scr, serum creatinine. Normal range: BUN = 9–21 mg/dL; Scr = 0.1–0.6mg/dL.
Study design; animal model of acute antibody-mediated rejection; 500 μL of donor (Brown Norway (BN), RT1n) blood was drawn into a heparinized syringe, and then injected intravenously into a recipient (Lewis, RT1I) rat. Three weeks later, recipients received a transplant from a BN rat, in conjunction with bilateral kidney nephrectomy. In some groups, animals were given 10 mg/kg cyclosporine A (CsA 10 mg/ kg/day) to mitigate cellular rejection.
Control and transfusion alone (Tn) groups were not transplanted. In these groups, kidney function was measured 4 weeks after study enrollment (control group) or 4 weeks after blood transfusion (Tn group).
p < 0.02 compared with C and Tn.
Patients
This HIPAA compliant study was approved by our institutional human subjects review committee and written informed consent was obtained from all subjects. We evaluated subjects who had undergone postkidney transplant indication biopsies within 1 year of transplant, between 2009 and 2012. Subjects were selected if they were diagnosed with ABMR based on Banff 2009 and had a history of blood transfusion in the 24 months preceding ABMR.
DSA analysis
DSA in humans were analyzed as described previously, using the single antigen bead Luminex (One Lambda) assay (23,24). Rat DSA measurement was performed as described elsewhere (25,26). Briefly, donor (BN, RT1n) splenocytes were freshly isolated from spleen macerated through a 50-μm sieve and washed after red blood cell lysis. Cells were resuspended, counted and aliquoted into cluster tubes for staining. Fifty microliters of 1:4 dilution of serum or plasma from 1 week posttransplant (or similar time points for control or transfusion only rats) were incubated for 30 min at 37°C, then washed and stained. Flow cytometry was performed on a BD LSR II at the Immunology Core of the WNPRC, UW-Madison and data analyzed using FlowJo (TreeStar, Inc., Ashland, OR). Cells were gated to remove nonsinglets, through a lymphocyte gate, then a CD3-positive gate to remove cells that had an FcR, which could skew analyses. Mean fluorescence intensity was determined for the populations of interest. Antibodies used were anti-IgG1 (clone RG11/39.4; BD Biosciences, San Diego, CA), IgG2a (clone RG7/1.30; BD Biosciences), IgG2b (clone RG7/11.1; BD Biosciences), IgG2c (biotinylated, clone A92-1, BD Biosciences), IgM (clone G53-238; BD Biosciences) and CD3 (clone 1F4 [BioLegend, San Diego, CA] or clone G4.18 [BD Biosciences]).
Complement-binding antibody analysis for C4d
C4d staining of Lewis recipient splenocytes was performed as described elsewhere (27,28). Briefly, splenocytes were obtained and incubated with 50 μL of 1:4 dilution of serum or plasma as above. Cells were washed with FACS buffer, then further incubated with Gelatin Veronal Buffer (Sigma–Aldrich, St. Louis MO; No. G6514) containing 10% fetal calf serum at 37°C for 45 min. After washing, cells were stained with C4d (anti-Rat C4d Cat. No. HP8034; Hycult Biotech Inc., Plymouth Meeting, PA), using donkey anti-rabbit IgG F(ab′)2 as the secondary antibody (Jackson ImmunoResearch, West Grove, PA; Cat. No. 711-606-152) or goat anti-rabbit IgG(H + L) (Life Technologies, Eugene, OR). Flow cytometry was performed as above.
Histology
Formalin-fixed, paraffin-embedded kidneys were cut into 5 μm sections. Slides were deparaffinized, rehydrated from xylene through a graded ethanol series to ddH2O and subsequently treated as described below. Slides were viewed on a Nikon EclipseE600 microscope (Melville, NY) and analyzed with an Olympus DP70 camera and software or an Olympus BX51 microscope equipped with an Olympus DP70 camera and software (Olympus America Inc., Center Valley, PA). All H&E and C4d slides were reviewed by Dr. Weixiong Zhong, MD, PhD, transplant pathologist, and scored for ptc, glomerulitis (g), vasculitis (v)/intimal arteritis, interstitial inflammation (i) and C4d staining, according to Banff 2009 (29,30). Morphometric analysis using electron microscopy was performed using standard methodology, as described earlier by the UW Department of Pathology and Laboratory Medicine (31).
Immunostaining and immunoblotting
Immunoperoxidase, immunofluorescence staining and Western blotting was done as previously described (20,32). The following antibodies were used for immunohistochemical studies: Rat anti-C4d (200−1; American Research Products, Waltham, MA; Cat. No. 12-5000), CD3 (300−1; Biocare Medical, Concord, CA; Cat. No. CP215A), CD68 (100−1; AbSerotec, Raleigh, NC; Cat. No. MCA341R), CD163 (100−1; AbSerotec; Cat. No. MCA342R) and Human anti-CD3 (500−1; Epitomics, Burlingame, CA; Cat. No. 3256-1), CD68 (500−1; Dako, Carpinteria, CA; Cat. No. M0814) and CD163 (100−1; Enzo, Farmingdale, NY; Cat. No. ALX-810-213).The following antibodies were used for immunoblotting studies: CD35 (Crry, 100−1; Abcam, Cambridge, MA; Cat. No. ab106109), CD55 (decay accelerating factor [DAF], 100−1; Santa Cruz, Dallas, TX; Cat. No. sc-9156),interferon regulatory factor 5 (IRF5)(500−1; Proteintech, Chicago, IL; Cat. No. 10547-1-AP), inducible nitric oxide synthase (iNOS) (1000−1; Enzo; Cat. No. BML-SA200), NADPH oxidase 2 (Nox2) (100−1; BD Biosciences; Cat. No. 611414) and GAPDH (5000−1; Abcam; Cat. No. ab8245).
RNA extraction, purification and reverse transcriptase PCR analysis
These methods were previously published (20). Briefly, total RNA extraction was done from crushed frozen kidney tissue using Trizol (Life Technologies). RNA was further purified using the RNAeasy kit (Qiagen, Valencia, CA). First strand cDNA synthesis kit (Roche, Indianapolis, IN) was used to generate cDNA. TaqMan Gene Expression Assays (all from Life Technologies) were run on a 7500 Reverse Transcriptase PCR System from Applied Biosystems. Mean Ct, standard deviation and ΔΔCt (compared with control animals) for IL-2 (Rn00587673_m1), IL-4 (Rn99999010_m1), IL-10 (Rn00563409_m1), IFN-γ (Rn00594078_m1) and internal control glyceraldehyde 3-phospate dehydrogenase (GAPDH) (Rn01775763_g1).
Statistical analysis
Student’s t-test and Mann–Whitney rank sum test were utilized to compare parametric and nonparametric continuous data when appropriate. One-way ANOVA was utilized to compare between multiple groups simultaneously. Similarly, Chi-squared or Fisher’s exact tests were utilized when appropriate to compare categorical data between groups. p-Values ≤ 0.05 were considered significant.
Results
Experimental design and kidney function
We selected the 1-week time point after transplant because all animals in our preliminary studies survived 7 days posttransplant regardless of the treatment group. Notably, preliminary studies established that the majority of animals in the Tx and TnTx groups died by Days 10 and 15, respectively. The experimental design included six animals in each group (Table 1). Compared to control (C) and transfusion alone (Tn), allograft recipients in all groups had a significant decline in kidney allograft function at 1 week posttransplant. Animals in the Tx group had the most severe decline compared to all groups (p < 0.0006) (Table 1).
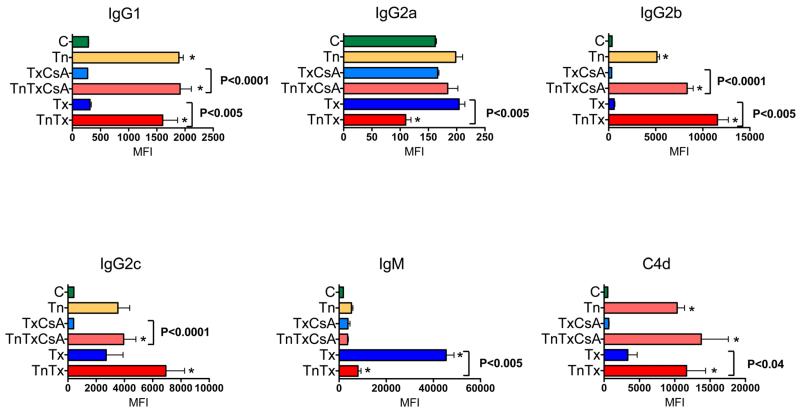
DSA were elicited by transfusion and fixed the complement
Transfusion and transplant were independently associated with DSA generation at 1 week posttransplant. While IgM DSA were the predominant isotype in the Tx group (first exposure to MHC antigens), animals with prior transfusion had elevated IgG1, IgG2b and IgG2c isotypes. IgG2a was not significantly changed compared to controls. We further noted that DSA elicited by transfusion were able to fix complement, as indicated by a significant difference in the amount of C4d deposition present on the surface of CD3 (FcR−) donor splenocytes in animals that received transfusion. Time course analyses demonstrated that total IgG and IgM DSA and complement-fixing alloantibodies increased with time, following both transfusion and transplant (Figure 2). In aggregate, these studies demonstrated that pretransplant conditioning with donor-specific blood transfusion was an effective means to elicit complement-fixing and noncomplement-fixing DSA in rats (Figures 1 and 2).
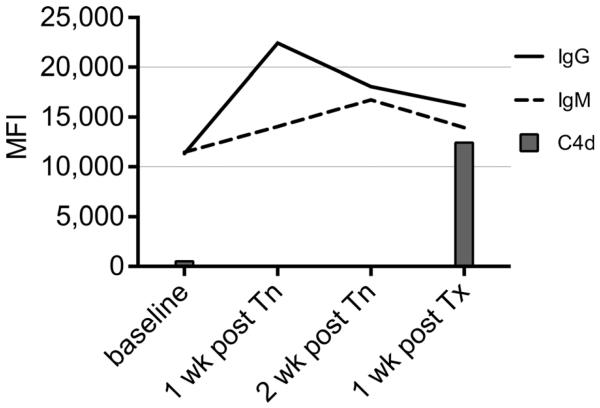
Figure 2. Time course of DSA and complement-fixing alloantibodies in sensitized animals.
Time course studies demonstrated that total IgG and IgM DSA and complement-fixing alloantibodies increased after both transfusion and transplantation. DSA, donor-specific antibody.
Figure 1. DSA and complement-fixing alloantibodies were increased in transfused animals.
Donor-specific IgG1, IgG2b and IgG2c were significantly increased in sensitized (transfused) animals at 1-week posttransplant. IgM was particularly high in the Tx group because this was the first time the immune system experienced foreign MHC antigen (primary response). For animals that received transfusions, 1 week post-Tx is 4 weeks postinitial exposure to foreign antigen and the response is more mature and class switching has occurred. To assess the complement-fixing ability of donor-specific alloantibodies, we incubated Brown Norway (donor) splenocytes with recipient serum and examined the expression of membrane-bound C4d. For all analyses, the MFI was determined after gating on CD3+ T cells, to avoid antibody that bound nonspecifically to cells expressing Fc receptors. Bars marked with a* were significantly (p < 0.05) different from control. DSA, donor-specific antibody; MFI, mean fluorescence intensity; Tx, transplant.
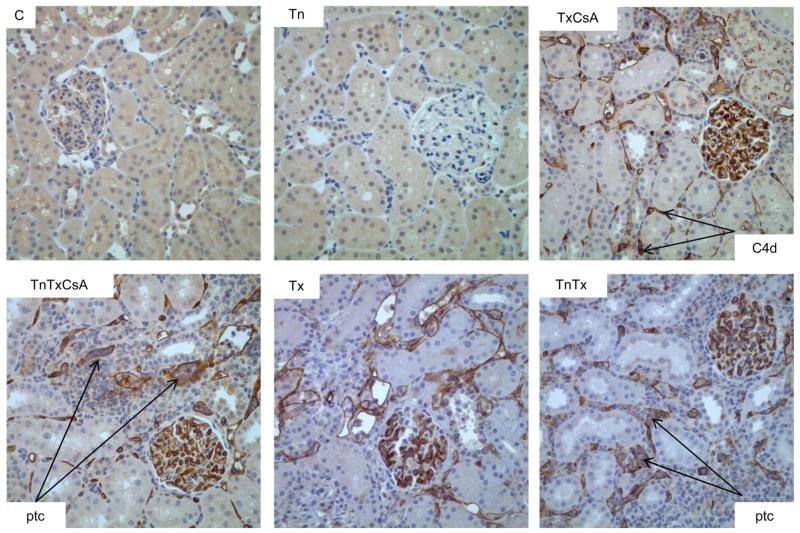
Transfusion was associated with diffuse C4d deposition in PTC
Diffuse C4d deposition was evident in all experimental groups that included transplant. CsA treatment and transfusion were not associated with significant differences in the semiquantitative scoring of C4d, suggesting that neither sensitization nor immunosuppression with high dose CsA affected the in situ binding of complement. However, transfusion alone did not elicit C4d staining in tissue, indicating that the presence of DSA alone was not sufficient to cause complement fixation in the absence of donor antigens (Figure 3; Table 2).
Figure 3. Sensitization and transplant were associated with diffuse C4d staining.
Transplant, with or without transfusion, was associated with diffuse C4d staining, particularly in the peritubular capillaries (brown peroxidase staining). Transfusion alone did not elicit this staining.
Table 2.
Histological assessment of kidney tissue for Banff criteria at 1-week posttransplant
| Group | C4d | t | v | i | g | ptc | MI |
|---|---|---|---|---|---|---|---|
| C | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| Tn | 0.3 ± 0.6 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| TxCsA | 2.0 ± 1.1 | 0.0 ± 0.0 | 0.0 ± 0.01 | 1.8 ± 1.0 | 0.2 ± 0.4 | 0.8 ± 0.4 | 1.0 ± 0.6 |
| TnTxCsA | 3.0 ± 0.0 | 0.0 ± 0.0 | 0.8 ± 0.81 | 2.5 ± 0.8 | 0.7 ± 0.5 | 1.2 ± 0.4 | 1.8 ± 0.8 |
| Tx | 3.0 ± 0.0 | 0.0 ± 0.0 | 1.7 ± 1.0 | 2.3 ± 0.52 | 1.1 ± 0.4 | 1.0 ± 0.03 | 2.1 ± 0.44 |
| TnTx | 3.0 ± 0.0 | 0.0 ± 0.0 | 1.0 ± 0.0 | 3.0 ± 0.02 | 1.5 ± 0.5 | 2.0 ± 0.03 | 3.5 ± 0.54 |
C, control; CsA, cyclosporine A; g, glomerulitis; i, interstitial inflammation; ptc, peritubular capillaritis; t, tubulitis; Tn, transfusion; Tx, transplant; v, vasculitis.
Microcirculation inflammation (MI) score is derived by adding ptc and g scores (MI = ptc + g).
p < 0.03 for v in TnTxCsA compared with TxCsA.
p < 0.02 for i in TnTx compared with Tx.
p < 0.0007 for ptc in TnTx compared with Tx.
p < 0.004 for MI in TnTx compared with Tx.
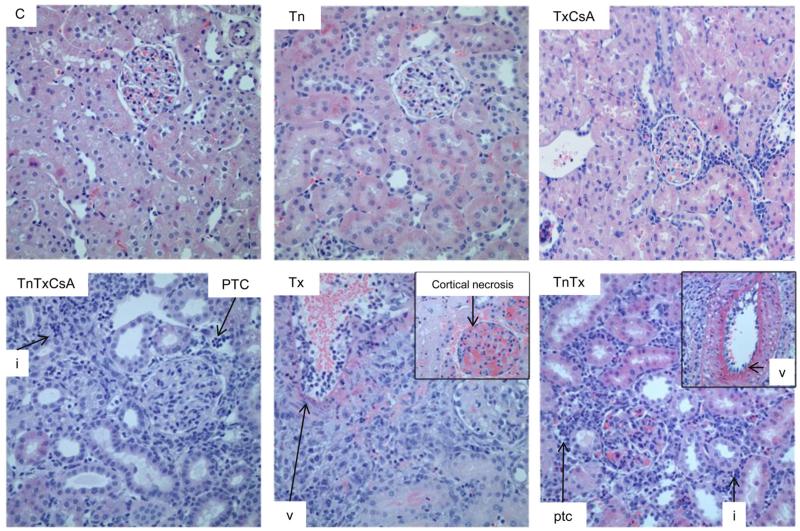
Transfusion was associated with significant microcirculation inflammation
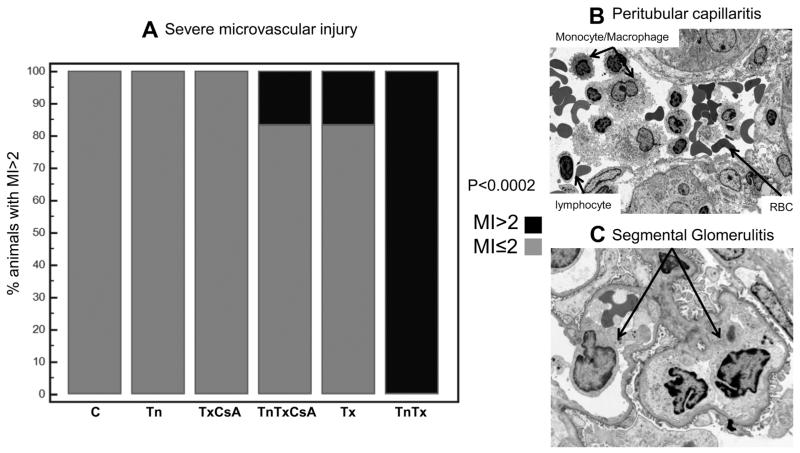
Microcirculation inflammation (MI), characterized by presence of glomerulitis and ptc, was associated with both transfusion and transplant. Table 2 shows the Banff scoring for all groups. Arteritis (v), glomerulitis (g) and interstitial inflammation (i) had higher values in groups that were not immunosuppressed. Intimal arteritis was also present in all groups that received transplant, except the TxCsA group (Figure 4). Transfusion was significantly associated with v in groups that received CsA and with i and ptc in groups that did not. Tx animals also presented with cortical necrosis (Figure 4). As noted in Figure 5, transfusion-associated ABMR correlated with severe MI (>2). Monocyte/macrophages as well as lymphocytes were observed in the PTC and glomeruli of sensitized rats undergoing ABMR (Figure 5B and C). In aggregate, these studies determined that donor-specific transfusion prior to transplant was associated with significant microvascular injury by monocyte/macrophages and lymphocytes, consistent with clinical observations in patients with severe ABMR. It is important to note that despite the absence of tubulitis on Day 7 samples (Table 2), the contribution of T cell–mediated rejection (TCMR) to renal allograft pathology could not be excluded. Banff i scores were indeed increased in sensitized animals. It is also possible that MI is associated with TCMR (Figures 4 and 5; Table 2).
Figure 4. Sensitization and transplant were associated with vascular and interstitial injury.
Microcirculation inflammation was more strongly associated with TnTx rather than Tx alone, especially peritubular capillaritis (ptc). Areas of interstitial inflammation (i) and vasculitis (v) were also observed. Tn, transfer; Tx, transplant.
Figure 5. Transfusion-associated antibody-mediated rejection (ABMR) correlated with severe microvascular inflammation.
Panel A displays a bar graph representing the % of animals with severe microcirculation inflammation (MI) = ptc + g > 2. Panels B and C display electron micrographs of peritubular capillaritis (ptc) and glomerulitis (g) in sensitized rats with acute ABMR.
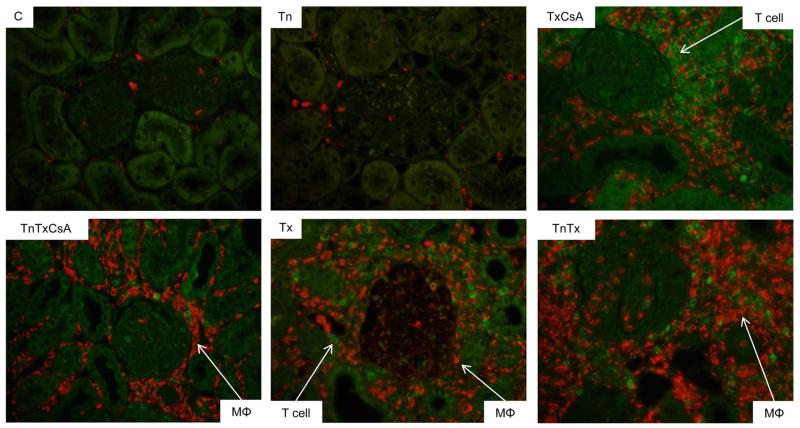
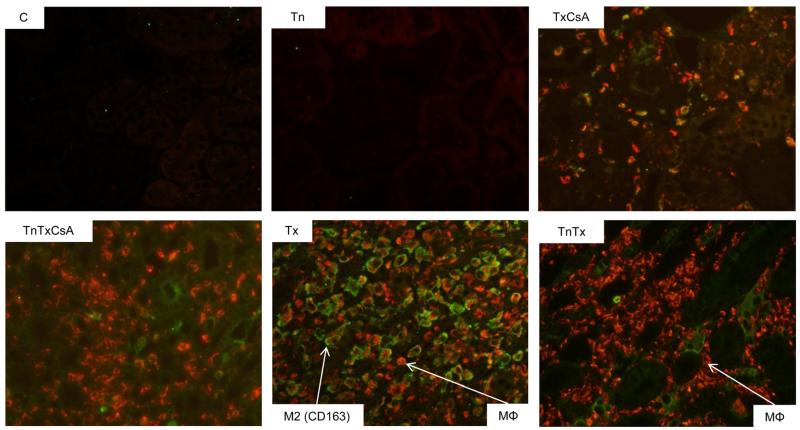
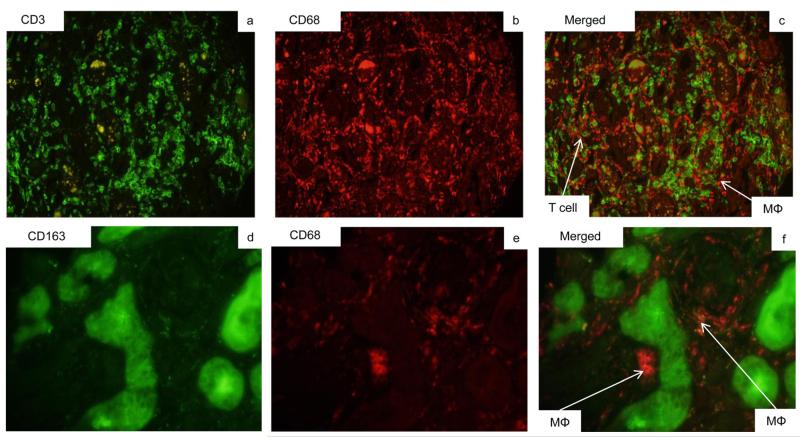
Transfusion-induced ABMR was associated with M1 phenotype macrophages and TH1 type responses in CsA-treated animals
To further characterize this animal model of ABMR, we examined the phenotype of graft infiltrating cells using immunofluorescent studies with anti-CD3 (T cells-green immunofluorescence) and CD68 (monocyte–macrophages, red immunofluorescence) antibodies (Figure 6). We identified widespread monocytic infiltration, predominantly in the TnTx and TnTxCsA groups, suggesting that the presence of DSA and their ability to fix complement was responsible for macrophage recruitment in these animals. To further characterize the phenotype of graft infiltrating monocyte–macrophages, we studied CD163 expression as a surface marker of M2 macrophages (Figure 7). In TxCsA and Tx alone groups, approximately half of the macrophages were CD163+CD68+M2. Conversely, sensitized animals (TnTxCsA and TnTx groups) had very few M2 macrophages, suggesting that transfusion resulted in an influx of macrophages to the donor kidney, but that this recruitment was specific for M1, almost to the exclusion of M2 macrophages. Alternatively, macrophages recruited into the kidney may have converted to M1 upon exposure to the inflammatory milieu created by the interaction of DSA, donor endothelium and complement (Figures 6–10).
Figure 6. Transfusion-associated ABMR correlated with significant macrophage infiltration.
The cellular infiltrate in TnTx kidneys largely consisted of macrophages (CD68 red) rather than T cells (CD3 green). ABMR, antibody-mediated rejection; Tn, transfusion; Tx, transplant.
Figure 7. Transfusion-associated ABMR correlated with downregulation of M2 macrophages.
CD68 (macrophages) were immunostained in red; CD163 (M2 macrophages) were immunostained in green. In both transfusion groups (TnTxCsA and TnTx), while there was a strong influx of macrophages, however, very few of these are of the M2 (CD163+) phenotype. In contrast, in the TxCsA and Tx groups, M2 macrophages (green and red) and non-M2 macrophages (red) are seen. ABMR, antibody-mediated rejection; CsA, cyclosporine A; Tn, transfusion; Tx, transplant.
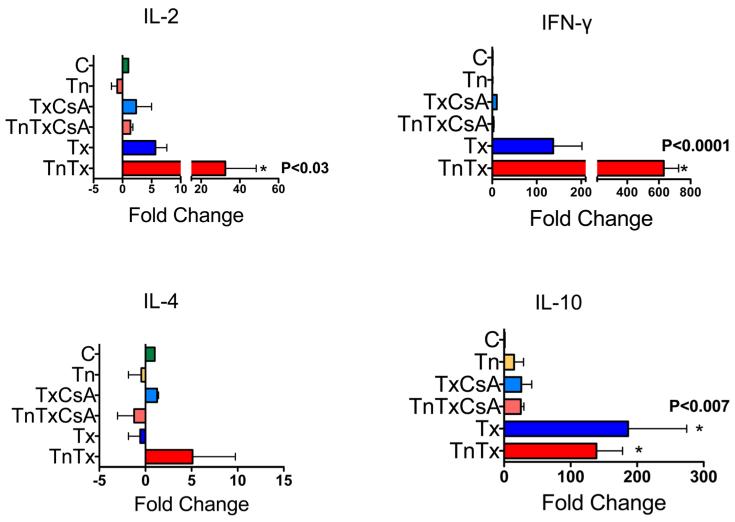
Figure 10. Transfusion-associated ABMR correlated with upregulation of TH1 type cytokines.
Transfusion-induced ABMR correlates with up-regulation of TH1 type cytokines (IL-2, IFN-γ) by reverse transcriptase PCR of whole frozen kidney from TnTx animals; whereas animals in the Tx group are making a mixed TH1/TH2 response, up-regulating IL-10, a TH2 cytokine, as well as IL-2 and IFN-γ, * and p-values indicate comparisons between each group and control using one-way analysis of variance. ABMR, antibody-mediated rejection; IFN-γ, interferon gamma; TH, T helper; Tn, transfusion; Tx, transplant.
To determine the clinical relevance of our studies, we examined the T cell and macrophage phenotypes in graft infiltrating cells of patients with a history of blood transfusion and acute ABMR in the first year posttransplant (n = 5). In these studies, the CD68:CD3 ratio was not as high as in the rat model, but similar to rats, macrophages had predominantly a CD68+, CD163− phenotype (M2 negative; Figure 8).
Figure 8. Transfusion-associated antibody-mediated rejection (ABMR) correlated with CD163 (M2) negative macrophages in humans.
ABMR in patients with a history of blood transfusion was associated with graft infiltrating macrophages (CD68 red) and T cells (CD3 green). The phenotype of graft infiltrating macrophages was predominantly CD163 negative, suggestive of an M1 phenotype.
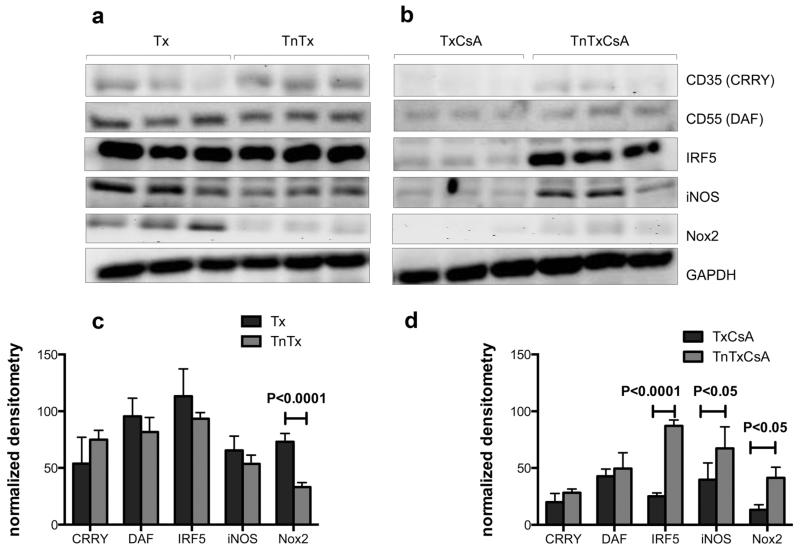
To confirm the role of M1 macrophages in this experimental model, we performed immunoblot and quantitative analyses of IRF5, a transcription factor central for the transition to, and maintenance of the M1 macrophage phenotype (33), as well as iNOS and Nox2, proteins associated with the pro-inflammatory macrophage phenotype (17,18,20,34) (Figure 9). We also assessed complement regulatory proteins CD35 (Crry) and CD55 (DAF). Although the role of these proteins in ABMR remains unknown, in vitro studies suggest that the TH1 cytokine IFN-γ increases DAF expression by endothelial cells (35). We observed that in animals not treated with CsA, transfusion only associated with a significant decline in Nox2. However, in the more clinically relevant group of animals treated with CsA, transfusion-associated ABMR correlated with greater inflammation (iNOS, Nox2) and the M1 macrophage phenotype (iNOS, Nox2) (Figure 9). We also noted what appeared to be a biologically relevant up-regulation of complement regulatory proteins DAF (CD55) and Crry (CD35) in animals that received TnTxCsA, although it did not reach the level of significance.
Figure 9. In CsA-treated animals, transfusion-associated ABMR correlated with greater inflammation and M1 macrophage phenotype.
Transfusion-induced ABMR in rats was associated with inflammation (iNOS, Nox2) and M1 (iNOS, IRF5) macrophage phenotype. Complement regulatory proteins (Crry, DAF) were not significantly affected by transfusion. ABMR, antibody-mediated rejection; CsA, cyclosporine A; iNOS, inducible nitrogen oxide synthase; IRF5, interferon regulatory factor 5; Nox2, NADPH oxidase 2.
To further characterize the phenotype of transfusion-induced ABMR in the kidney allograft, we evaluated the TH1 and TH2 cytokine profiles by assessing IL-2, IFN-γ, IL-4 and IL-10 messenger RNA (mRNA) levels using reverse transcriptase PCR analyses (Figure 10). We observed that in transfused animals, IL-2 increased by 30-fold compared with control and by sixfold compared with Tx alone. Remarkably, this same group had a 600-fold increase for IFN-γ compared with control and a fourfold increase compared with Tx alone. By contrast, the Tx alone group had significantly increased amounts of mRNA for IFN-γ as well as IL-10 compared with control and the increase in IL-10 was greater than that observed for the TnTx group. In aggregate, these studies demonstrate that transfusion-associated ABMR is characterized by TH1 cytokine and M1 macrophage inflammatory profiles.
Discussion
Animal models of transplantation may provide important evidence supporting proof of concept (19). As outlined by the FDA workshop on ABMR, and in the Banff 2009 meeting report, animal models of ABMR after kidney transplantation are needed as they provide opportunities to better understand the science underlying potential therapies directed against ABMR (9,19). In agreement with this concept, we developed a rat model of ABMR in which kidney transplants were performed across a full HLA mismatch, 3 weeks following donor-specific blood transfusion. We demonstrated that blood transfusion-induced sensitization was associated with severe microvascular inflammation and ABMR. Our observations further suggest that TH1 cytokines and M1 macrophages play an important role in the regulation of transfusion-associated ABMR. However, it is important to note that despite the absence of tubulitis, the effects of TCMR could not be excluded and it is likely that akin to clinical rejection, this model is more descriptive of mixed rejection than pure ABMR.
A recent experimental study of ABMR presensitized recipient rats by skin transplantation (36). Anti-donor-specific IgG levels reached a maximum 2 weeks following presensitization after which the rats underwent renal transplantation from the same donor strain. In sensitized rats, neutrophil and mononuclear cell infiltration and C4d staining in PTC was detected beginning 2 h after transplantation. DSA IgG levels decreased rapidly and several cytokines and complement components showed marked changes in the presensitized group (36). Because of the clinical importance of blood transfusion in sensitization, we used donor-specific blood transfusion to immunize allograft recipients in our studies (37). It is important to note that earlier studies from the pre-CsA era demonstrated that approximately a third of patients receiving blood transfusion developed the “transfusion effect” with a significant increase in graft survival rates (38–41). Transfusion may indeed regulate antigen-specific immunosuppression through direct clonal inactivation, anti-idiotypic network generation, and suppressor T cell generation (41,42). Conversely, donor-specific transfusion also induces allosensitization in a third of patients who, as a result, cannot undergo kidney transplantation from the same donor (39–41). The significant risks of alloimmunization and infections, and the arrival of more potent immunosuppressants have ended the therapeutic use of donor-specific transfusion in organ transplantation. However, the cellular and molecular mechanisms that regulate the immune response after transfusion remain of great and contemporary interest, especially as patients on the transplant waitlist are likely to receive transfusions due to multiple co-morbidities (43,44).
Complement has been considered to be a main player in ABMR (45). We observed a significant increase in complement-fixing and noncomplement-fixing alloantibodies, both of which are important and synergize to cause rejection (46–49). In humans, IgG1 (a complement-fixing isotype) is the most commonly observed isotype and is present in 45% of all patients, followed by IgG3 (rat IgG2c equivalent) (46). In rats, IgG2b and IgM fix complement, while IgG1 does not (50). We noted that C4d deposition in PTC, as well as dilation of PTC with infiltration of monocyte/macrophages, was similar to patients with ABMR (51,52). While the up-regulation of complement regulatory proteins CD35 (Crry) and CD55 (DAF) did not reach statistical significance, this change may be biologically relevant as endothelial DAF may increase under the influence of IFN-γ, a key player in TH1 response (35).
We observed a strong TH1 (IFN-γ and IL-2) and M1 macrophage response in this model. These results are consistent with cell types observed in PTC in patients with ABMR, as NK cells and macrophages are significantly increased in ABMR compared to TCMR and are predictive of poor outcome (12,52,53). Transfusion-induced ABMR was associated with a robust infiltration of macrophages (CD68+ cells) at 1 week after transplant. These macrophages were primarily of M1 phenotype as they were negative for CD163, and were associated with significantly increased levels of iNOS and Nox2. It is possible that complement activation by preformed DSA attracts macrophages and up-regulates FcRs and complement receptors on macrophages (54). As activated M1 macrophages differentiate when exposed to IFN-γ produced by T cells or NK cells (17), it is also possible that the pathogenesis of transfusion-induced ABMR and macrophage recruitment is regulated by a TH1 milieu. However, it is important to note that we were unable to exclude the effects of TCMR and it is likely that similar to clinical rejection, this model is descriptive of mixed rejection rather than pure ABMR.
Many patients on the kidney donor waitlist end up receiving transfusions (43), putting them at risk of developing DSA while they are waiting for a kidney. A better understanding of the mechanisms that regulate donor-specific B cell and plasma cell development will identify additional intervention targets. The closeness of our model to the human system allows us to consider potential mechanisms of inflammation, such as complement activation and TH1/M1 macrophage influx as potential targets for intervention. We can further use this animal model to address novel treatment strategies to prevent transfusion-induced sensitization, test desensitization interventions and develop strategies for the treatment of ABMR in humans.
Acknowledgments
We wish to thank the Department of Medicine for financial support. Financial support was also provided by NIDDK R01 DK092454. We wish to acknowledge support of the Wisconsin National Primate Research Center, P51RR000167/P51OD011106, and Eva Rakasz and Kim Weisgrau in the Immunology core at WNPRC in particular for use of the BD LSR II flow cytometer.
Abbreviations
- ABMR
antibody-mediated rejection
- BN
Brown Norway
- BUN
blood urea nitrogen
- CsA
cyclosporine A
- DAF
decay accelerating factor
- DSA
donor-specific antibody
- FcR
Fc receptor
- g
glomerulitis
- GAPDH
glyceraldehyde 3-phospate dehydrogenase
- i
interstitial inflammation
- IFN-γ
interferon gamma
- iNOS
inducible nitrogen oxide synthase
- IRF5
interferon regulatory factor 5
- MI
microcirculation inflammation
- mRNA
messenger RNA
- NK
natural killer
- Nox2
NADPH oxidase 2
- ptc
peritubular capillaritis
- PTC
peritubular capillaries
- Scr
serum creatinine
- t
tubulitis
- TCMR
T cell–mediated rejection
- TH
T helper
- v
vasculitis
Footnotes
Disclosure
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
References
- 1.Wiebe C, Gibson IW, Blydt-Hansen TD, et al. Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am J Transplant. 2012;12:1157–1167. doi: 10.1111/j.1600-6143.2012.04013.x. [DOI] [PubMed] [Google Scholar]
- 2.Djamali A, Kaufman DB, Ellis TM, Zhong W, Matas A, Samaniego M. Diagnosis and management of antibody-mediated rejection: Current status and novel approaches. Am J Transplant. 2014;14:255–271. doi: 10.1111/ajt.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Zoghby ZM, Stegall MD, Lager DJ, et al. Identifying specific causes of kidney allograft loss. Am J Transplant. 2009;9:527–535. doi: 10.1111/j.1600-6143.2008.02519.x. [DOI] [PubMed] [Google Scholar]
- 4.Sellares J, de Freitas DG, Mengel M, et al. Understanding the causes of kidney transplant failure: The dominant role of antibody-mediated rejection and nonadherence. Am J Transplant. 2012;12:388–399. doi: 10.1111/j.1600-6143.2011.03840.x. [DOI] [PubMed] [Google Scholar]
- 5.Halloran PF, Wadgymar A, Ritchie S, Falk J, Solez K, Srinivasa NS. The significance of the anti-class I antibody response. I. Clinical and pathologic features of anti-class I-mediated rejection. Transplantation. 1990;49:85–91. doi: 10.1097/00007890-199001000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Halloran PF, Schlaut J, Solez K, Srinivasa NS. The significance of the anti-class I response. II. Clinical and pathologic features of renal transplants with anti-class I-like antibody. Transplantation. 1992;53:550–555. [PubMed] [Google Scholar]
- 7.Feucht HE, Schneeberger H, Hillebrand G, et al. Capillary deposition of C4d complement fragment and early renal graft loss. Kidney Int. 1993;43:1333–1338. doi: 10.1038/ki.1993.187. [DOI] [PubMed] [Google Scholar]
- 8.Mauiyyedi S, Pelle PD, Saidman S, et al. Chronic humoral rejection: Identification of antibody-mediated chronic renal allograft rejection by C4d deposits in peritubular capillaries. J Am Soc Nephrol. 2001;12:574–582. doi: 10.1681/ASN.V123574. [DOI] [PubMed] [Google Scholar]
- 9.Sis B, Mengel M, Haas M, et al. Banff ’09 meeting report: Antibody mediated graft deterioration and implementation of Banff Working Groups. Am J Transplant. 2010;10:464–471. doi: 10.1111/j.1600-6143.2009.02987.x. [DOI] [PubMed] [Google Scholar]
- 10.Haas M, Sis B, Racusen L, et al. Banff 2013 meeting report: Findings of Banff working groups and inclusion of C4d-negative antibody-mediated rejection. Am J Transplant. 2014;14:272–283. doi: 10.1111/ajt.12590. [DOI] [PubMed] [Google Scholar]
- 11.Farkash EA, Colvin RB. Diagnostic challenges in chronic antibody-mediated rejection. Nat Rev Nephrol. 2012;8:255–257. doi: 10.1038/nrneph.2012.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hidalgo LG, Sis B, Sellares J, et al. NK cell transcripts and NK cells in kidney biopsies from patients with donor-specific antibodies: Evidence for NK cell involvement in antibody-mediated rejection. Am J Transplant. 2010;10:1812–1822. doi: 10.1111/j.1600-6143.2010.03201.x. [DOI] [PubMed] [Google Scholar]
- 13.Sis B, Halloran PF. Endothelial transcripts uncover a previously unknown phenotype: C4d-negative antibody-mediated rejection. Curr Opin Organ Transplant. 2010;15:42–48. doi: 10.1097/MOT.0b013e3283352a50. [DOI] [PubMed] [Google Scholar]
- 14.Jane-Wit D, Manes TD, Yi T, et al. Alloantibody and complement promote T cell-mediated cardiac allograft vasculopathy through non-canonical NF-kappaB signaling in endothelial cells. Circulation. 2013;128:2504–2516. doi: 10.1161/CIRCULATIONAHA.113.002972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mannon R. Macrophages: Contributors to allograft dysfunction, repair, or innocent bystanders? Curr Opin Organ Transplant. 2012;17:20–25. doi: 10.1097/MOT.0b013e32834ee5b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lefaucheur C, Nochy D, Hill G, et al. Determinants of poor graft outcome in patients with antibody-mediated acute rejection. Am J Transplant. 2007;7:832–841. doi: 10.1111/j.1600-6143.2006.01686.x. [DOI] [PubMed] [Google Scholar]
- 17.Mannon RB. Macrophages: Contributors to allograft dysfunction, repair, or innocent bystanders? Curr Opin Organ Transplant. 2012;17:20–25. doi: 10.1097/MOT.0b013e32834ee5b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cao Q, Wang Y, Harris DC. Pathogenic and protective role of macrophages in kidney disease. Am J Physiol Renal Physiol. 2013;305:F3–F11. doi: 10.1152/ajprenal.00122.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Archdeacon P, Chan M, Neuland C, et al. Summary of FDA antibody-mediated rejection workshop. Am J Transplant. 2011;11:896–906. doi: 10.1111/j.1600-6143.2011.03525.x. [DOI] [PubMed] [Google Scholar]
- 20.Djamali A, Vidyasagar A, Adulla M, Hullett D, Reese S. Nox-2 is a modulator of fibrogenesis in kidney allografts. Am J Transplant. 2009;9:74–82. doi: 10.1111/j.1600-6143.2008.02463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Djamali A, Reese S, Yracheta J, Oberley T, Hullett D, Becker B. Epithelial-to-mesenchymal transition and oxidative stress in chronic allograft nephropathy. Am J Transplant. 2005;5:500–509. doi: 10.1111/j.1600-6143.2004.00713.x. [DOI] [PubMed] [Google Scholar]
- 22.Djamali A, Reese S, Oberley T, Hullett D, Becker B. Heat shock protein 27 in chronic allograft nephropathy: A local stress response. Transplantation. 2005;79:1645–1657. doi: 10.1097/01.tp.0000164319.83159.a7. [DOI] [PubMed] [Google Scholar]
- 23.Djamali A, Muth BL, Ellis TM, et al. Increased C4d in post-reperfusion biopsies and increased donor specific antibodies at one-week post transplant are risk factors for acute rejection in mild to moderately sensitized kidney transplant recipients. Kidney Int. 2013;83:1185–1192. doi: 10.1038/ki.2013.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niederhaus SV, Muth B, Lorentzen DF, et al. Luminex-based desensitization protocols: The University of Wisconsin initial experience. Transplantation. 2011;1:12–17. doi: 10.1097/TP.0b013e31821c93bb. [DOI] [PubMed] [Google Scholar]
- 25.Sicard A, Phares TW, Yu H, et al. The spleen is the major source of antidonor antibody-secreting cells in murine heart allograft recipients. Am J Transplant. 2012;12:1708–1719. doi: 10.1111/j.1600-6143.2012.04009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hattori Y, Bucy RP, Kubota Y, Baldwin WM, III, Fairchild RL. Antibody-mediated rejection of single class I MHC-disparate cardiac allografts. Am J Transplant. 2012;12:2017–2028. doi: 10.1111/j.1600-6143.2012.04073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Minami K, Murata K, Lee C, et al. C4d deposition and clearance in cardiac transplants correlates with alloantibody levels and rejection in rats. Am J Transplant. 2006;6:923–932. doi: 10.1111/j.1600-6143.2006.01281.x. [DOI] [PubMed] [Google Scholar]
- 28.Qian Z, Lee C, Murata K, et al. Antibody and complement mediated injury in transplants following sensitization by allogeneic blood transfusion. Transplantation. 2006;82:857–864. doi: 10.1097/01.tp.0000232335.06792.35. [DOI] [PubMed] [Google Scholar]
- 29.Mengel M, Sis B, Haas M, et al. Banff 2011 meeting report: New concepts in antibody-mediated rejection. Am J Transplant. 2012;12:563–570. doi: 10.1111/j.1600-6143.2011.03926.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sis B, Mengel M, Haas M, et al. Banff ’09 meeting report: Antibody mediated graft deterioration and implementation of Banff working groups. Am J Transplant. 2010;10:464–471. doi: 10.1111/j.1600-6143.2009.02987.x. [DOI] [PubMed] [Google Scholar]
- 31.Swanlund JM, Kregel KC, Oberley TD. Investigating autophagy: Quantitative morphometric analysis using electron microscopy. Autophagy. 2010;6:270–277. doi: 10.4161/auto.6.2.10439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vidyasagar A, Reese S, Acun Z, Hullett D, Djamali A. HSP27 is involved in the pathogenesis of kidney tubulointerstitial fibrosis. Am J Physiol Renal Physiol. 2008;295:F707–F716. doi: 10.1152/ajprenal.90240.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krausgruber T, Blazek K, Smallie T, et al. IRF5 promotes inflammatory macrophage polarization and TH1-TH17 responses. Nat Immunol. 2011;12:231–238. doi: 10.1038/ni.1990. [DOI] [PubMed] [Google Scholar]
- 34.Djamali A, Reese S, Hafez O, et al. Nox2 is a mediator of chronic CsA nephrotoxicity. Am J Transplant. 2012;12:1997–2997. doi: 10.1111/j.1600-6143.2012.04081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mason JC, Yarwood H, Sugars K, Morgan BP, Davies KA, Haskard DO. Induction of decay-accelerating factor by cytokines or the membrane-attack complex protects vascular endothelial cells against complement deposition. Blood. 1999;94:1673–1682. [PubMed] [Google Scholar]
- 36.Kohei N, Tanabe T, Horita S, et al. Sequential analysis of donor-specific antibodies and pathological findings in acute antibody-mediated rejection in a rat renal transplantation model. Kidney Int. 2013;84:722–732. doi: 10.1038/ki.2013.117. [DOI] [PubMed] [Google Scholar]
- 37.Toyoda M, Ge S, Pao A, et al. Cellular allo reactivity against paternal HLA antigens in normal multiparous females as detected by intracellular cytokine flow cytometry remains elevated over years despite diminution of anti-HLA antibody levels. Transpl Immunol. 2010;23:133–140. doi: 10.1016/j.trim.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 38.Opelz G, Terasaki PI. Improvement of kidney-graft survival with increased numbers of blood transfusions. N Engl J Med. 1978;299:799–803. doi: 10.1056/NEJM197810122991503. [DOI] [PubMed] [Google Scholar]
- 39.Salvatierra O, Jr, Vincenti F, Amend W, et al. Deliberate donor-specific blood transfusions prior to living related renal transplantation. A new approach. Ann Surg. 1980;192:543–552. doi: 10.1097/00000658-198010000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sollinger HW, Kalayoglu M, Belzer FO. Use of the donor specific transfusion protocol in living-unrelated donor-recipient combinations. Ann Surg. 1986;204:315–321. doi: 10.1097/00000658-198609000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burlingham WJ, Grailer A, Sparks-Mackety EM, Sondel PM, Sollinger HW. Improved renal allograft survival following donor-specific transfusions. II. In vitro correlates of early (DST-type) rejection episodes. Transplantation. 1987;43:41–46. doi: 10.1097/00007890-198701000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Brunson ME, Alexander JW. Mechanisms of transfusion-induced immunosuppression. Transfusion. 1990;30:651–658. doi: 10.1046/j.1537-2995.1990.30790385527.x. [DOI] [PubMed] [Google Scholar]
- 43.Ibrahim H, Skeans M, Li Q, Ishani A, Snyder J. Blood transfusions in kidney transplant candidates are common and associated with adverse outcomes. Clin Transplant. 2011;25:653–659. doi: 10.1111/j.1399-0012.2011.01397.x. [DOI] [PubMed] [Google Scholar]
- 44.Murata K, Baldwin WM., III Mechanisms of complement activation, C4d deposition, and their contribution to the pathogenesis of antibody-mediated rejection. Transplant Rev (Orlando) 2009;23:139–150. doi: 10.1016/j.trre.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Akiyoshi T, Hirohashi T, Alessandrini A, et al. Role of complement and NK cells in antibody mediated rejection. Hum Immunol. 2012;73:1226–1232. doi: 10.1016/j.humimm.2012.07.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaneku H, O’Leary J, Taniguchi M, Susskind B, Terasaki P, Klintmalm G. Donor-specific human leukocyte antigen antibodies of the immunoglobulin G3 subclass are associated with chronic rejection and graft loss after liver transplantation. Liver Transpl. 2012;18:984–992. doi: 10.1002/lt.23451. [DOI] [PubMed] [Google Scholar]
- 47.Lee C, Lotfi-Emran S, Erdinc M, et al. The involvement of FcR mechanisms in antibody-mediated rejection. Transplantation. 2007;84:1324–1334. doi: 10.1097/01.tp.0000287457.54761.53. [DOI] [PubMed] [Google Scholar]
- 48.Murata K, Fox-Talbot K, Qian Z, et al. Synergistic deposition of C4d by complement-activating and non-activating antibodies in cardiac transplants. Am J Transplant. 2007;7:2605–2614. doi: 10.1111/j.1600-6143.2007.01971.x. [DOI] [PubMed] [Google Scholar]
- 49.Rahimi S, Qian Z, Layton J, Fox-Talbot K, Baldwin WM., III Wasowska B. Non-complement- and complement-activating antibodies synergize to cause rejection of cardiac allografts. Am J Transplant. 2004;4:326–334. doi: 10.1111/j.1600-6143.2004.00334.x. [DOI] [PubMed] [Google Scholar]
- 50.Baldwin WM, III, Pruitt S, Brauer R, Daha M, Sanfilippo F. Complement in organ transplantation. Contributions to inflammation, injury, and rejection. Transplantation. 1995;59:797–808. [PubMed] [Google Scholar]
- 51.Hidalgo LG, Campbell PM, Sis B, et al. De novo donor-specific antibody at the time of kidney transplant biopsy associates with microvascular pathology and late graft failure. Am J Transplant. 2009;9:2532–2541. doi: 10.1111/j.1600-6143.2009.02800.x. [DOI] [PubMed] [Google Scholar]
- 52.Sis B, Jhangri GS, Riopel J, et al. A new diagnostic algorithm for antibody-mediated microcirculation inflammation in kidney transplants. Am J Transplant. 2012;12:1168–1179. doi: 10.1111/j.1600-6143.2011.03931.x. [DOI] [PubMed] [Google Scholar]
- 53.Magil A, Tinckam K. Monocytes and peritubular capillary C4d deposition in acute renal allograft rejection. Kidney Int. 2003;63:1888–1893. doi: 10.1046/j.1523-1755.2003.00921.x. [DOI] [PubMed] [Google Scholar]
- 54.Baldwin WM, III, Halushka M, Valujskikh A, Fairchild R. B cells in cardiac transplants: From clinical questions to experimental models. Semin Immunol. 2012;24:122–130. doi: 10.1016/j.smim.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]