Abstract
Inflammatory conditions of the lung such as chronic obstructive pulmonary disease (COPD) are known to increase lung cancer risk, particularly lung squamous cell carcinoma (LSCC). In the present study, we developed a mouse model of inflammation-driven LSCC that was induced by N-nitroso-trischloroethylurea (NTCU) and enhanced by lipopolysaccharide (LPS), a potent proinflammatory agent contained in tobacco and tobacco smoke, and determined the chemopreventive effects of BioResponse diindolylmethane (DIM) in the same model. Compared to mice treated with NTCU alone, mice treated with the combination of NTCU and LPS had a 9-fold increase in the number of bronchioles with LSCC. Also, compared to mice treated with LPS alone, mice treated with NTCU plus LPS showed significantly increased expression of the inflammatory cytokines IL-1α, IL-6, and TNFα (all three increased about 7-fold). Parallel to the increased cytokine gene expression, the NTCU plus LPS-treated group exhibited significantly enhanced activation of NF-κB, STAT3, ERK, p-38, and Akt, expression of p53, COX-2, and Mcl-1, and NF-κB- and STAT3-DNA binding in the lung. Dietary administration of DIM (10 µmol/g diet or 2460 ppm) to mice treated with NTCU plus LPS reduced the incidence of LSCC by 2-fold, suppressed activation/expression of proinflammatory and procarcinogenic proteins and NF-κB- and STAT3-DNA binding, but not the expression of cytokines and p53. This study highlights the potential significance of our mouse model to identify promising drugs or dietary agents for the chemoprevention of human LSCC and that DIM is a very good candidate for clinical lung cancer chemoprevention trials.
Keywords: pulmonary inflammation, lung squamous cell carcinoma, diindolylmethane
Introduction
Lung cancer is the leading cause of cancer-related mortality in the United States and worldwide (1,2). Despite advances in the diagnosis and therapy of lung cancer, the overall five-year survival rate of patients is still not more than 15%. One promising approach to reduce lung cancer mortality is identification of preneoplastic lesions and administration of chemopreventive agents with the objective of reversing, suppressing or arresting lung tumorigenesis. Mucosal changes in the large airways that precede or accompany lung squamous cell carcinoma (LSCC), the second most common type of lung cancer, include hyperplasia, squamous metaplasia, squamous dysplasia, and carcinoma in situ (3). Whereas hyperplasia and squamous metaplasia are considered reactive and reversible changes, dysplasias and carcinoma in situ are the changes most frequently associated with the development of LSCC (4). Thus, chemopreventive agents that inhibit malignant progression of dysplastic or carcinoma in situ lesions could prevent LSCC.
So far, the success of translating preclinical lung cancer chemoprevention studies to the clinic has been poor and there is not a single clinically proven lung cancer chemopreventive agent. One explanation for this could be that the animal models used and the lesions targeted are not representative of the human disease treated in clinical chemoprevention trials. For instance, whereas the majority of the preclinical models develop only lung adenoma/adenocarcinoma which arises peripherally in smaller airways and alveoli, the lesions targeted in almost all clinical lung cancer chemoprevention trials are bronchial preneoplastic lesions that arise centrally and have the potential to develop into LSCC. Moreover, since molecular signatures of lung adenocarcinoma are different from those found in LSCC (5,6), chemopreventive agents that show efficacy against lung adenocarcinoma may not be equally effective towards LSCC. To rectify these problems, Wang et al (7) developed N-nitroso-trischloroethylurea (NTCU)-induced mouse model of LSCC, which exhibited similar histopathologic features and keratin staining to human LSCC, therefore providing a valuable preclinical model for LSCC. In lieu of the strong epidemiological evidence that links chronic obstructive pulmonary disease (COPD), the main form of chronic pulmonary inflammation, to a higher risk of lung cancer, in particular LSCC (8–11), and the many common signaling pathways involved in chronic inflammation and lung tumorigenesis (12,13), a mouse model of inflammation-driven LSCC would better mirror the human disease.
Here, we report on the role of lipopolysaccharide (LPS)-induced pulmonary inflammation in enhancing NTCU-induced mouse LSCC and the efficacy of diindolylmethane (DIM), one of the breakdown products of indole-3-carbinol, a constituent of Brassica vegetables, to suppress inflammation-driven LSCC in mice. LPS, the major component of the cell wall of Gram-negative bacteria and a potent inflammatory agent, exists in substantial amounts in mainstream and sidestream cigarette smoke (14,15) and has been shown to induce inflammatory response mimicking COPD in mice (16). Our studies showed that the incidence of LSCC was significantly higher in mice treated with a combination of NTCU and LPS, as compared to the group treated with NTCU alone, and dietary administration of DIM significantly reduced the incidence of LSCC in NTCU plus LPS-treated mice. Assessment of molecular pathways showed increased activation of inflammatory pathways and higher expression of cell proliferation/survival-related proteins and these effects were modulated by DIM.
Materials and Methods
Chemicals and Reagents
NTCU and LPS were purchased from Toronto Research Chemicals (Toronto, Canada) and Sigma (St. Louis, MO), respectively. BioResponse diindolylmethane (DIM) was kindly provided by Dr. Michael Zeligs (BioResponse, LLC). Anti-phospho-STAT3, anti-total STAT3, anti-phospho-Akt, anti-total Akt, anti-phospho-extracellular signal-regulated kinase (ERK), anti-total ERK, anti-phospho-p38, total p-38, anti-Mcl-1, anti-p53, anti-COX2, anti-phospho IκBα, anti-total IκBα, anti-Bax, anti-p-21, anti-PARP, anti-β-actin and goat anti-rabbit IgG secondary antibody were from Cell Signaling Technology (Beverly, MA). Mouse diets (AIN-93G and AIN-93M) were purchased from Harlan Teklad (Madison, WI). These diets are standard diets for lung tumorigenesis studies in A/J mice. The AIN-93G diet, high in protein and fat, was used to support rapid growth of the mice until eight weeks of age. AIN-93G diet was then replaced by AIN-93M diet, a low-protein and low-fat diet, which is recommended for adult maintenance.
Mouse LSCC bioassay
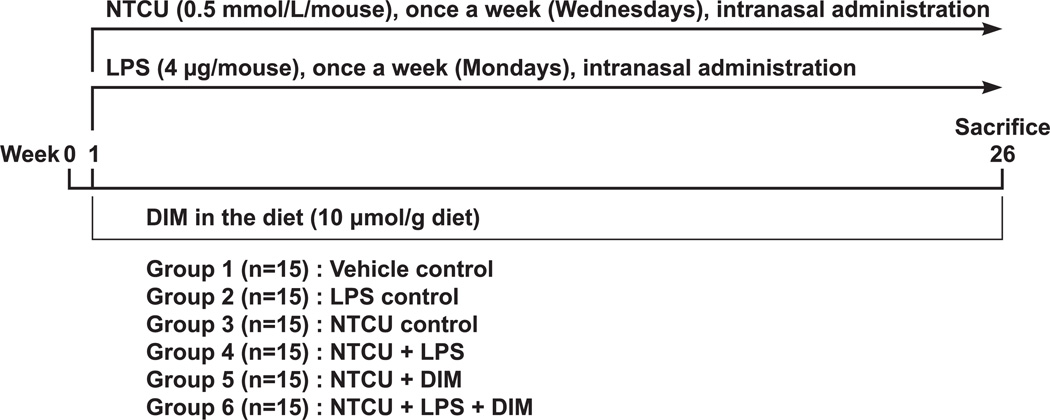
For LSCC bioassay, six weeks-old female A/J mice were obtained from the Jackson Laboratory (Bar Harbor, ME) and housed in the specific-pathogen-free animal quarters of Research Animal Resources, University of Minnesota Academic Health Center. After one week of acclimatization, the mice were randomized into six treatment groups (15 mice/group) as follows: Groups 1, 2, 3 and 4 were vehicle control (5% DMSO and 95% physiological saline), LPS control, NTCU control, and NTCU plus LPS control, respectively. LPS (4 µg/mouse, in 50 µl of physiological saline solution) and NTCU (0.5 mmol/L/mouse in 50 µl of vehicle control, 25 µl in each nostril) were administered intranasally, once a week, on Mondays and Wednesdays, respectively, throughout the study. The vehicle group was given 50 µl physiological saline solution in the same manner. Mice in groups 5 and 6 were treated with NTCU or NTCU plus LPS, respectively, and received the chemopreventive agent BioResponse diindolylmethane (DIM, 10 µmol/g diet) in AIN-93G/M powder diet until the end of the study. Mice in groups 1–4 were maintained on non-supplemented diet. Body weights and food consumption were determined weekly throughout the study. Upon termination of the study at week 26, mice were euthanized with an overdose of carbon dioxide, the lungs harvested and preserved in 10% buffered formalin for histopathological analyses of the tumors. The experimental design of the tumor bioassay is depicted in Fig. 1.
Figure 1.
Experimental design to determine LSCC induction by NTCU and LPS, alone and in combination, and inhibitory effects of dietary DIM. Female A/J mice, 5–6 weeks old, were intranasally treated with NTCU and LPS, once a week, and given DIM in the diet throughout the study. Twenty-six weeks after the initial treatment with NTCU/LPS/DIM, mice were terminated with an overdose of carbon dioxide.
To harvest lung tissues for Western immunoblotting or qRT-PCR assay, mice (three/group) were treated with vehicle, LPS, NTCU, NTCU plus LPS, and NTCU plus LPS plus DIM as described above. At week 10, lungs tissues were harvested and either kept on dry ice (for immunoblotting assay) or preserved in RNA latter (for qRT-PCR assay) until stored at −80 °C. The rationale for the short treatment time was that whereas early changes in gene/protein expression could be most likely drivers of the carcinogenesis process, changes in gene/protein expression after formation of the tumors are difficult to interpret as they might be causes or consequences of tumorigenesis.
Histopathological analysis of mouse lung tissues
The multiplicity and incidence of the different lung lesions, including hyperplasia, metaplasia, carcinoma in situ (dysplasia was included in this category), and LSCC were analyzed by Dr. Ming You`s group at the Medical College of Wisconsin as described previously (7). Briefly, serial tissue sections (4-µm each) were made from formalin-fixed lungs, and 1 in every 20 sections (approximately 100 µm apart) was stained with Hematoxylin and Eosin and examined under a light microscope. All cross-sectional cuts of bronchioles were counted on all of the slides.
Quantitative RT-PCR (QRT-PCR) analysis of cytokines in mouse lungs
Total RNA was extracted from mouse lung tissues using the miRNeasy Mini Kit (Qiagen, Valencia, CA) according to the manufacturer’s instruction. The purity and integrity of the RNA preparations were confirmed by spectrophotometry and Agilent Bioanalyzer. RNA(1 µg) was reverse transcribed to cDNA in 20 µL reaction using the QuantiTect Reverse Transcription Kit(Qiagen, Valencia, CA). The first-stand cDNA amplification mixture was diluted to 40 µL with nuclease-free water and stored at −20 °C until use.
Quantification of mRNAs was performed on Applied Biosystems 7900HT Fast Real-Time PCR System with 384-Well Block Module (Life Technologies, Carlsbad, CA) using QuantiTect SYBR Green PCR Kit (Qiagen, Valencia, CA) and gene-specific primers (Table 1). Twenty-five nanogram of cDNA sample was added to a 10 µL reaction and the final concentration of each primer was 0.5 µM. For the PCR amplification, a program of initial denaturation at 95 °C for 15 min, followed by 40 cycles consisting of denaturation at 94 °C for 15 sec, annealing at 55 °C for 30 sec and elongation at 70 °C for 34 sec was used.
Table 1.
Primer sets used for the QRT-PCR analysis
| Gene | Forward primer | Reverse primer | Amplicon length, bp |
|---|---|---|---|
| mus TNF-α | TATGGCTCAGGGTCCAACTC | CTCCCTTTGCAGAACTCAGG | 174 |
| mus IL-6 | ACGGCCTTCCCTACTTCACA | CATTTCCACGATTTCCCAGA | 129 |
| mus IL-1α | GCAACGGGAAGATTCTGAAG | TGACAAACTTCTGCCTGACG | 177 |
| Δmus Actb | CGTGCGTGACATCAAAGAGAA | TGGATGCCACAGGATTCCAT | 201 |
| mus IFN-γ | ACTGGCAAAAGGATGGTGAC | GCTGATGGCCTGATTGTCTT | 98 |
| mus IL12a | ATGACCCTGTGCCTTGGTAG | GAAGCAGGATGCAGAGCTTC | 241 |
| mus IL12b | AAGGAACAGTGGGTGTCCAG | GGCAAACCAGGAGATGGTTA | 196 |
Reference gene
All samples were normalized to an internal control gene, β-actin (Actb). Comparative Ct method was used to assess the relative gene expression. Values were expressed as relative units compared to the vehicle control mouse lung tissue and the respective standard errors of the mean.
STAT3- and NF-κB- DNA binding Assay
To determine if STAT3 and NF-κB binding to DNA is modulated by the different treatments, we used the TransAM transcription factor assay (Active Motif, CA), a non-radioactive transcription factor ELISA kit that facilitate the study of transcription factor activation, and the Odyssey Infrared electrophoretic mobility shift assay (EMSA) Kit (LI-COR, Lincoln, NB), which is an excellent alternative method to radioisotopic and chemiluminescent EMSA detection methods.
Ten µg of nuclear protein extract prepared from mouse lung tissues were diluted in complete lysis buffer and added into each well coated with oligonucleotide containing STAT3 or NF-κB consensus binding site. Under the assay conditions, STAT3 or NF-κB subunit proteins in nuclear extract bind to the oligonucleotide, and STAT3 or p65 was detected by using a primary antibody specific to the proteins followed by incubation with horseradish peroxidase conjugated secondary antibody and colorimetric reading at 450 nm. Wild type consensus oligonucleotide (CO) was used as a competitor to prevent STAT3 or NF-κB binding to the probe immobilized on the plate. In order to monitor the specificity of the assay, nuclear protein extracts (5 µg) from HepG2 cells, stimulated with IL6 for STAT3, and Jurkat cells, stimulated with TPA for NF-κB, were used as positive control samples. Three independent experiments were performed with triplicate samples. Error bars represent standard deviation.
Western blot analysis of mouse lung tissues
Mouse lung tissues were homogenized in a buffer containing protease and phosphatase inhibitors and 100 µg of protein from tissue lysates were electrophoresed on a 4–12 % Novex Tris–glycine gel (Invitrogen, Carlsbad, CA), and transferred to a polyvinylidene difluoride (PVDF) membrane (Bio-Rad). After blocking with 5% non-fat powdered milk in tris-buffered saline (TBS) containing 0.05% Tween20 (TBST), the membrane was incubated with appropriate primary antibody at 4°C overnight. Subsequently, the membrane was washed with TBST and incubated with horseradish peroxidase conjugated secondary antibody for 1 h at room temperature. The protein-antibody complexes were detected by enhanced chemiluminescence (ECL kit) in accordance with the manufacturer’s directions (Pierce, Rockford, IL). Biotinylated protein ladder (Cell Signaling Technology) was loaded into the left lane of each gel and used as the molecular weight marker to detect the target band correctly. All membranes were stripped and re-probed with anti-β-actin (1:1000) to check for differences in the amount of protein loaded in each lane. For each protein, at least three western assays were carried out. For quantitative determination of protein levels, densitometry measurements of Western blot bands were performed using digitalized scientific software program UN-SCAN-IT software (Silk Scientific, Orem,Utah).
Statistical Analyses
Statistical analyses were performed using one way ANOVA and 2-tailed t-test in Graphpad Prism 4 software (Graphpad, La Jolla, CA). Data for Western immunoblotting, EMSA and cytokine gene expression are reported as mean ± standard deviation of triplicate determinations. *, P < 0.05.
Results
Chronic LPS treatment enhanced NTCU-induced LSCC in mice and dietary administration of DIM suppressed these effects
Average food consumption per mouse was 2.2 to 2.6 g/day and dietary administration of DIM did not cause ill health effects, nor did it reduce food consumption or body weight gain, indicating that, at the dose level given, the agent is well tolerated.
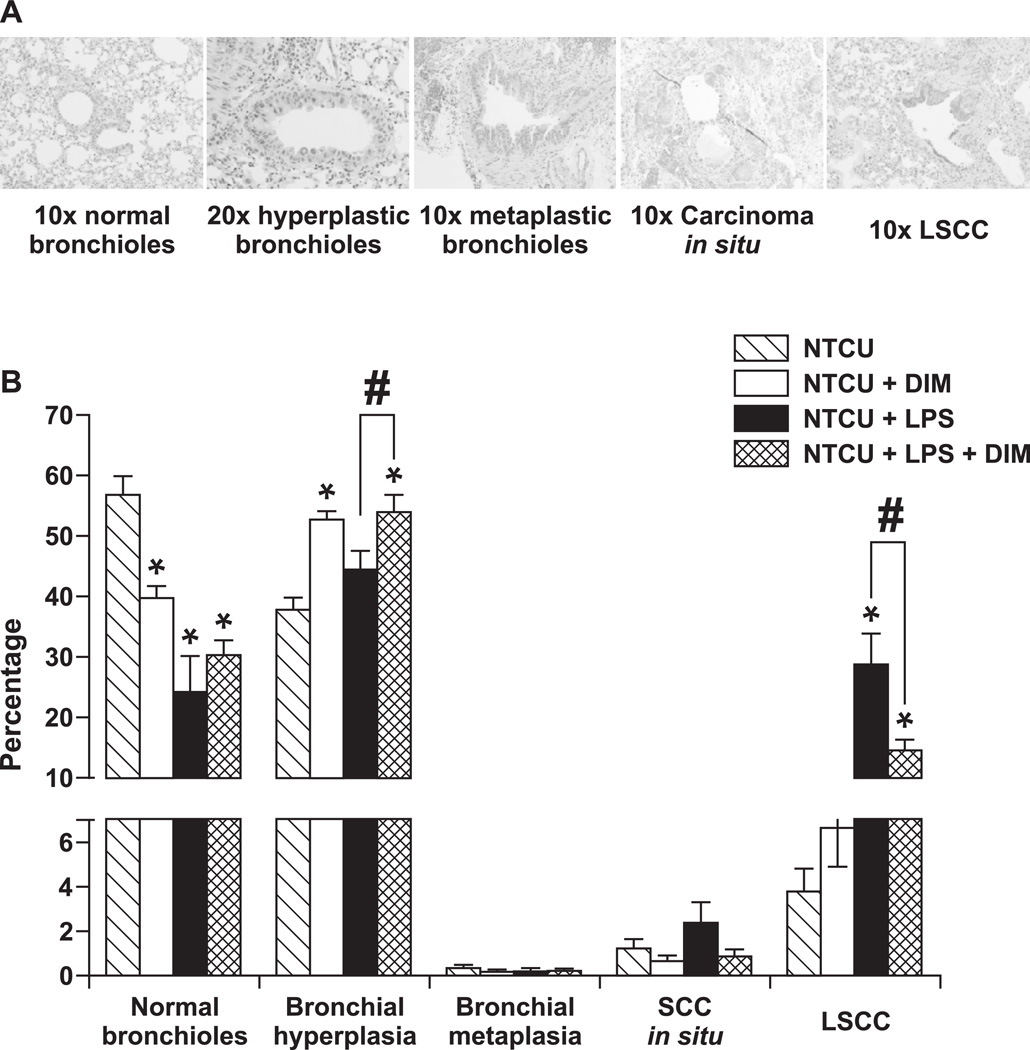
Since chronic inflammation plays a multifaceted role in tumorigenesis, including initiation, promotion and progression (17), we sought to examine if chronic treatment with the potent inflammatory agent LPS enhances the development of NTCU-induced pulmonary preneoplastic lesions and LSCC in mice. Images of normal bronchial epithelium, bronchial preneoplastic lesions (hyperplasia, metaplasia, carcinoma in situ) and LSCC and the incidence of the lesions in the various groups of mice are depicted in Figs. 2a and 2b, respectively. In mice treated with NTCU alone, the percentages of normal bronchioles, and bronchioles with hyperplasia, metaplasia, carcinoma in situ and LSCC were 57.8 ± 8.8%, 37.8 ± 5.7%, 0.3 ± 0.4%, 1.2 ± 1.2% and 3.8 ± 2.9%, respectively. Upon dietary administration of DIM, only the incidence of hyperplastic lesions was significantly modulated (increased by 28%). Compared to the group treated with NTCU alone, in mice treated with NTCU plus LPS, the percentage of normal bronchioles decreased by about 2-fold (24.3 ± 17.7% versus 56.8 ± 8.8%), whereas that of LSCC increased by about 9-fold (28.8 ± 15.4% versus 3.8 ± 2.9%). Dietary administration of DIM to mice treated with NTCU plus LPS slightly increased the percentage of normal bronchi and bronchial hyperplasia (30.4 ± 7.4% versus 24.3 ± 7.7% and 54.0 ± 9.0% versus 44.5 ± 9.4%, respectively), but decreased the incidence of carcinoma in situ (0.9 ± 1.0% versus 2.4 ± 2.8%) and LSCC (14.6 ± 5.5% versus 28.8 ± 5.4%). However, only the effect of DIM on LSCC was statistically significant. Mice treated with vehicle control (physiological saline) or LPS alone did not exhibit any abnormal lesion.
Figure 2.
Incidences of bronchial preneoplastic lesions and LSCC in mice treated with NTCU or NTCU + LPS and inhibitory effects of DIM on LSCC development. As mouse LSCC does not form visible solid nodules on the surface of the lung, serial tissue sections were made from each formalin-fixed lung and 1 in every 20 sections was stained with H&E. To assess specific effects of the different treatments on each histopathologic stage, all of the bronchioles in each given slide were counted and grouped into 5 categories based on normal, hyperplasia, metaplasia, carcinoma in situ (dysplasia was included in this category), and invasive SCC. The number in each category was then converted into percentage. *, P < 0.05, compared to NTCU group; *, P < 0.05, compared to NTCU group; # P < 0.05, NTCU/LPS vs NTCU/LPS/DIM.
Combinatory treatment with NTCU and LPS enhanced the expression of inflammatory cytokines
Inflammation is mediated by a variety of soluble factors, including cytokines and therefore we compared the expression of different cytokines among the various treatment groups. These results are shown in Table 2. Compared to the group treated with the vehicle, NTCU treatment significantly increased the expression of IL-6 (2.9-fold increase), whereas LPS significantly increased the expression of IL-6, TNFα, IFN γ, and IL-12b (5.1-, 3.4-, 5.0-, and 3.0-fold increase, respectively). Treatment of the mice with a combination of NTCU and LPS dramatically and significantly increased the expression of IL-1 α, IL-6, TNFα, IFN γ and IL-12b (7.4-, 30.4-, 21.2-, 7.3- and 3.7-fold increase compared to vehicle control group, respectively). Dietary administration of DIM to mice treated with a combination of NTCU and LPS did not significantly modulate the expression of any of the cytokines.
Table 2.
Expression of cytokine genes in lung tissues of mice treated with vehicle control, NTCU and/or LPS, and NTCU + LPS + DIMa
| IL-1α | IL-6 | TNFα | IFN γ | IL-12a | IL-12b | |
|---|---|---|---|---|---|---|
| Healthy control (n=5) | 1.0 ± 0.13 | 1.0 ± 0.09 | 1.0 ± 0.14 | 1.0 ± 0.26 | 1.0 ± 0.15 | 1.0 ± 0.15 |
| NTCU (n=6) | 0.6 ± 0.05b | 2.9 ± 0.16b | 0.9 ± 0.17 | 1.1 ± 0.32 | 0.6 ± 0.05b | 1.4 ± 0.23 |
| LPS (n=5) | 1.4 ± 0.37 | 5.1 ± 0.68b | 3.4 ±0.87b | 5.0 ± 1.66 | 0.2 ± 0.07b | 3.0 ± 0.47b |
| NTCU+LPS (n=6) | 7.4 ± 1.55c,d | 30.4 ± 6.77c,d | 21.2 ± 3.27c,d | 7.3 ± 1.55c | 1.2 ± 0.20c,d | 3.7 ± 0.60d |
| NTCU+LPS+DIM (n=6) | 8.6 ± 2.22 | 45.4 ± 10.03 | 22.5 ± 4.86 | 13.3 ± 3.40 | 1.5 ± 0.30 | 5.1 ± 0.91 |
Female A/J mice were treated with NTCU and LPS, alone or in combination, as described in the materials and methods section and maintained on control or DIM-supplemented diet. At week 10, mice were euthanized with an overdose of carbon dioxide, lung tissue harvested in RNA latter and used for QRT-PCR-based analysis of IL-1α, IL-6, TNFα, IFN γ, IL-12a and IL-12b expression.
p < 0.05, compared to vehicle control;
p < 0.05, compared to the NTCU group;
p < 0.05, compared to the LPS group.
Combinatory treatment with NTCU and LPS activated inflammatory pathways and these effects were suppressed by DIM
Components of the inflammatory pathway, including NF-κB, STAT3, and COX-2 play major roles in enhancing tumorigenesis (18–20). Therefore, we sought to assess if NTCU and LPS, alone or in combination, modulate the level of these proteins and whether dietary administration of DIM suppresses these effects.
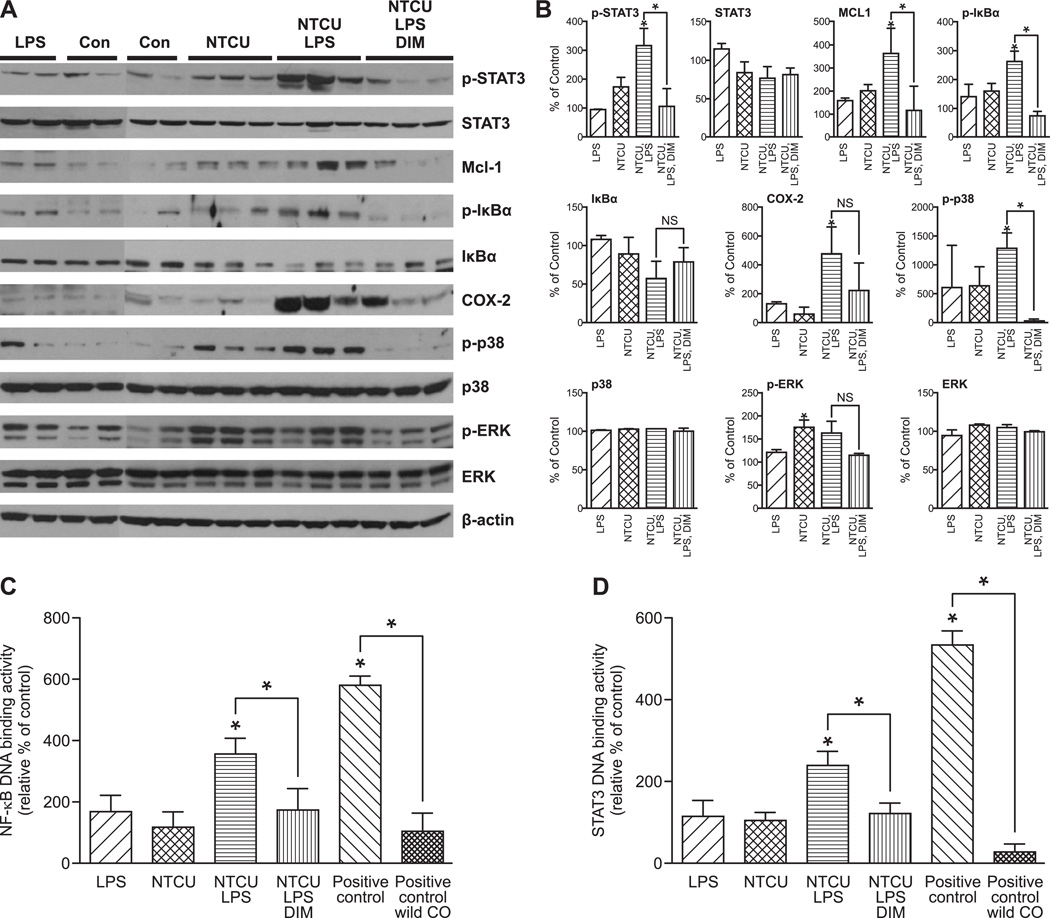
To examine the effect of NTCU and LPS, alone or in combination, on the NF-κB pathway, we assessed, by Western immunoblotting, the level of total and phosphorylated IκBα, whose phosphorylation by IκB kinase results in activation and nuclear translocation of NF-κB. Compared to the group treated with vehicle, neither LPS alone nor NTCU alone significantly modulated the level of total IκBα or phospho- IκBα (Figs. 3a and 3b). However, combinatory treatment with NTCU and LPS significantly decreased the level of IκBα (2-fold) but increased phospho- IκBα (2–5 fold). Dietary administration of DIM reversed the effects of NTCU plus LPS on IκBα and phospho- IκBα expression. To corroborate activation of the NF-κB pathway by NTCU and LPS and inhibition by DIM, we performed an ELISA-based EMSA assay which measures NF-κB-DNA binding. As depicted in Fig. 3c, compared to the vehicle group, the combination of NTCU and LPS significantly increased NF-κB-DNA binding by more than 3-fold, whereas DIM restored the level of NF-κB-DNA binding to that of the vehicle control group. Treatment with LPS alone increased NF-κB-DNA binding slightly, albeit non-significantly, whereas the level in the NTCU group was similar to the vehicle group. The expression of COX-2, one of the downstream effectors of the NF-κB pathway known to catalyze the formation of cancer promoting prostaglandins, was significantly increased (about 5-fold) by the combination of NTCU and LPS. DIM did not significantly suppress these effects.
Figure 3.
Effects of NTCU and LPS, alone and in combination, on inflammation-related proteins and modulation of these effects by dietary DIM. A, Mouse lung tissue levels of NF-κB, STAT3, p-38 and ERK activation and expression of Mcl-1 and COX-2, downstream effectors of NF-κB and STAT3, respectively, were determined by Western immunoblotting as described in the materials and methods section. B, quantification of the western blot results. Densitometry measurements of Western blot bands were performed using digitalized scientific software program UN-SCAN-IT software. Effects of NTCU and/or LPS on NF-κB-DNA binding (C) and STAT3-DNA binding (D) tissues as determined by ELISA-based EMSA assays (Active motif). Values are presented as mean ± SD. *, P < 0.05.
We also assessed, by Western immuoblotting, the effect of NTCU and LPS on the level of total STAT3, phosphorylated STAT3 and Mcl-1, an antiapoptotic protein regulated by STAT3. Only the combination of NTCU and LPS significantly increased STAT3 phosphorylation (3-fold) and Mcl-1 expression (about 3.5 fold), without affecting the level of total STAT3. DIM restored these changes to the level in the vehicle control (Figs. 3a and 3b). Likewise, in ELISA-based EMSA assays, the combination of NTCU and LPS significantly increased STAT3-DNA binding by more than 2-fold and DIM reversed STAT3-DNA binding to the level measured in the vehicle control group (Fig. 3d).
Among MAPK proteins, ERK phosphorylation was increased by LPS and NTCU, alone and in combination. However, only the effect of NTCU was significant. On the other hand, the level of p38 phosphorylation was increased 5-fold upon treatment with NTCU alone or LPS alone and 12-fold by the combination of NTCU and LPS. DIM almost completely reversed NTCU plus LPS-induced p38 phosphorylation (Figs. 3a and 3b).
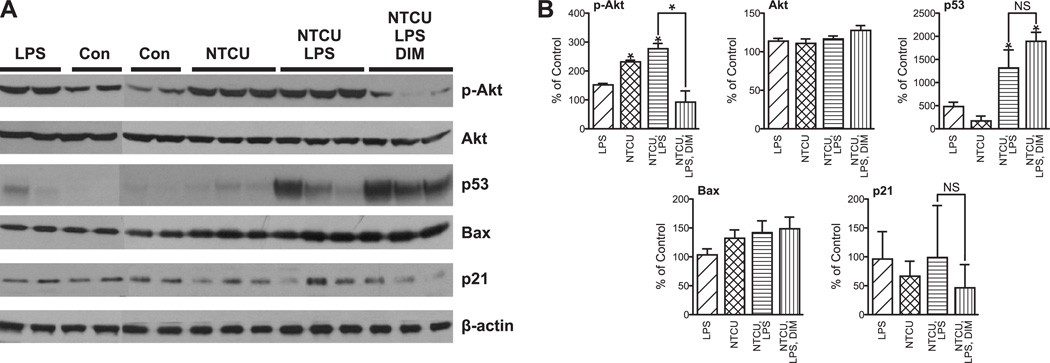
Combinations of NTCU and LPS increased levels of phospho-Akt and p53 and DIM suppressed the effect on phosphor-Akt
Alterations in the expression of Akt (21–24) and p53 (25–27) are commonly observed in LSCC. Therefore, we sought to examine modulation of the level of these proteins in our mouse model of LSCC and the potential reversal of these effects by DIM. Compared to the level in the vehicle control group, LPS alone and NTCU plus LPS increased p53 expression in lung tissues by 5-fold and 12-fold, respectively. Despite the marked increase in the expression of p53, levels of Bax and p21, downstream effectors of p53, did not change and dietary administration of DIM did not modulate the level of p53 (Figs. 4a and 4b). Moreover, no change was observed in the cleavage of PARP, a marker of apoptosis (data not shown). DIM did not significantly modulate NTCU plus-LPS induced p53 overexpression. Compared to the level in the vehicle group, the level of phospho-Akt was increased by LPS, NTCU and NTCU + LPS, but only the effects of NTCU (2.3 fold) and NTCU plus LPS (2.8 fold) were significant (Figs. 4a and 4b). Dietary administration of DIM restored the expression of phospho-Akt in NTCU plus LPS group to the level measured in the vehicle group. None of the treatments modulated the level of total Akt.
Figure 4.
Effects of NTCU and LPS, alone and in combination, on Akt and p53 proteins. A, Levels of total and phosphorylated Akt, p53, Bax and p21 in NTCU and/or LPS-treated mouse lung tissues were determined by Western immunoblotting as described in the materials and methods section. B, quantification of the western blot results. Densitometry measurements of Western blot bands were performed using digitalized scientific software program UN-SCAN-IT software. Values are presented as mean ± SD. *, P < 0.05.
Discussion
In the present study, we showed that LPS, a potent inflammatory agent contained in tobacco and tobacco smoke (14,15) enhanced LSCC induced by NTCU, a halogenated nitrosoalkylurea, and these effects were paralleled by significant induction of inflammatory cytokines, activation of pro-inflammatory and pro-oncogenic NF-κB and STAT3 signaling pathways and overexpression of p53 and phospho Akt. In mice treated with NTCU alone, only the incidence of bronchial hyperplasia, a reactive and reversible change, was significantly increased, whereas LPS-treated mice did not show any abnormal lesions. Dietary administration of DIM to mice treated with a combination of NTCU and LPS significantly reduced the incidence of LSCC and suppressed activation of NF-κB and STAT3 signaling pathways and expression of Akt. DIM increased the percentage of normal bronchioles (30.4 ± 7.4% versus 24.3 ± 7.7%) and bronchial hyperplasia (54.0 ± 9.0% versus 44.5 ± 9.4%), but decreased NTCU + LPS-induced LSCC (from 28.8 ± 5.4% in the NTCU + LPS group to 14.6 ± 5.5% in the NTCU + LPS + DIM group), suggesting that suppression of damage to the normal bronchiole and inhibition of progression of bronchial cell hyperplasia could be the reason for the reduced incidence of LSCC lesions, thus, providing a rationale for further development of DIM as a chemopreventive agent against LSCC.
Animal models of inflammation driven-LSCC are highly needed for a thorough understanding of the molecular links between chronic inflammation and LSCC and to identify safe and effective chemopreventive agents. Since tobacco smoking has a stronger association with LSCC than other non-small cell lung cancers (9–11) and it is also the main cause of COPD (28), a risk factor for LSCC, tobacco smoke appears to be the most ideal agent to induce inflammation-driven LSCC in animal models. However, earlier studies in mice showed that tobacco smoke induces only the adenocarcinoma histological subtype of lung cancer (29,30). On the other hand, NTCU has been consistently shown to induce LSCC in mice when administered topically at a dose of 40 mmol/L, (7,31–34). In the present study, in order to develop a mouse model of inflammation-driven LSCC that closely resembles human LSCC, mice were treated with a lower dose of NTCU (about 100-fold lower than the dose used in previous studies) and a COPD-like air way inflammation was induced via repetitive exposure to LPS. Previous studies with mice have shown that LPS-induced inflammatory and pathologic changes closely mimic those observed in human COPD (35,36) and repetitive exposure of NNK-pretreated mice to LPS doubled lung tumor multiplicity, markedly increased tumor size and increased peritumoral accumulation of macrophages (37). In the present study, combinatory treatment with a lower dose of NTCU (0.5 mmol/L, about 100-fold lower than the dose used in previous studies) and LPS was as potent as or even more potent than the standard dose of NTCU (40 mmol/L) (29,30) in inducing LSCC. The higher potency of NTCU plus LPS to induce LSCC could be ascribed partly to the direct delivery of the agents to the lung, the target organ, and partly to the tumor initiating/promoting effects of LPS-induced pulmonary inflammation.
Epidemiological evidence indicates that up to 25% of all cancers are related to chronic inflammation induced by bacterial or viral infections, toxic chemicals such as tobacco smoke, autoimmune disease or obesity (38). Molecular mechanisms through which chronic inflammation induces cancer include aberrant inflammatory cytokine and chemokine expression, activation of NF-κB and STAT3 signaling pathways and increased COX-2 (39). In the present study, whereas administration of LPS or NTCU alone caused a small increase in the expression of inflammatory cytokines, combinatory treatment with NTCU and LPS hugely increased the expression of most cytokines, in particular, IL-6 and TNFα (30-and 21-fold increase). TNFα and IL-6 are few of the best characterized cytokines regarding their protumourigenic effects and their involvement in cancer is owing to their ability to activate the oncogenic transcription factors NF-κB (TNFα) and STAT3 (IL-6) in epithelial cells (40–42). TNFα is secreted by several types of cells, including epithelial and inflammatory cells, and once released, it binds to TNF receptor (TNFR) superfamily proteins and activates NF-κB, activator protein-1 (AP-1), and MAPK p38 and ERK 1/2, which, cooperatively, induce a variety of inflammatory genes, including COX-2 and inducible nitrogen oxide synthase (41,43). Similarly, IL-6 binds to the gp130/IL6R heterodimeric receptor and activates the Janus kinase/STAT3 signaling pathway (44). In line with the above reports, combinatory treatment with NTCU and LPS, parallel to significant induction of TNFα and IL-6, activated NF-κB, STAT3, MAPK p38 and ERK1/2, enhanced NF-κB- and STAT3-DNA binding, and increased expression of COX-2.
In line with previous reports in which alterations of Akt and p53 have been consistently shown during the development of LSCC (5,21–27), lung tissues from mice treated with a combination of NTCU and LPS exhibited activation of Akt and overexpression of p53. Akt is a serine/threonine kinase which plays a critical role in the growth and survival of cancer cells and is activated in a signaling cascade downstream of Ras and phosphoinositide-3-kinase (45). Numerous studies have revealed higher levels of activated Akt in bronchial preneoplastic lesions (21–24), supporting that Akt activation is as an early event in lung cancer development. Similar findings have been reported for p53 (25–27), an important tumor suppressor protein involved in cell cycle regulation, DNA repair and apoptosis. However, given that p53 is a tumor suppressor protein, it is not clear why its expression increases in premalignant tissues. One reason could be that p53 mutates in preneoplastic tissues and the mutant p53 gene gives rise to a stable mutant protein (46,47). Mutant p53 proteins not only lose their tumor suppressive activities but often gain additional oncogenic functions that endow cells with growth and survival advantages (47). Although we have not determined p53 gene mutational status in our mouse lung tissues, Western immunoblotting analysis of p21 and Bax, two important downstream effectors of p53, as well as PARP cleavage, a marker of apoptosis, showed no changes. This indicates that the p53 gene might have lost its wild type status. The reason for the higher expression of p53 in lung tissues of mice treated with LPS alone is unclear as the agent did not cause any histological changes in lung tissues. However, LPS-induced oxidative stress may also induce p53 mutation as has been reported in nontumorous colon tissue of subjects with ulcerative colitis (48).
DIM is generated in the acidic environment of the stomach following dimerization of indole-3-carbinol (I3C) monomers present in commonly consumed Brassica vegetables such as cabbage, Brussels sprouts, Broccoli, and cauliflower. Consistent results from preclinical cancer chemoprevention studies have indicated that DIM induces apoptosis and suppresses proliferation of cancer cells, alters angiogenesis, invasion, metastasis and epigenetic behavior of cancer cells by acting on several targets, including Ah receptor, NF-κB, Wnt, Akt, mTOR, Nrf-2, and androgen receptor (49). Recently, we showed that DIM induced pronounced antiproliferative and apoptotic effects in premalignant and malignant bronchial cells via suppression of the PI3K/Akt signaling pathway (50). In this study, DIM significantly reduced NTCU plus LPS-induced LSCC, probably via suppression of the pro-inflammatory and pro-oncogenic NF-κB and STAT3 signaling pathways and their target genes such as COX-2 and Mcl-1, respectively, and the pro-survival Akt pathway. However, DIM did not reduce the expression of inflammatory cytokines and the reason for this is unclear.
Assuming A/J mice (25 g body weight) consume 2.5 g diet per day, the dose of DIM used in the present study (10 µmol/g diet) would be equivalent to 250 mg/kg body weight. Using allometric scaling, this translates to a dose of about 1, 400 mg/day for a 70 Kg human. However, the calculated human dose might have been overestimated given the inaccuracies in mouse food consumption measurements. In a recent clinical trial (49), DIM was administered at a dose of 300 mg twice daily (total daily dose of 600 mg) and found to be well tolerated.
In conclusion, in the present study, we showed that combinatory treatment with NTCU and LPS caused in mice a higher incidence of LSCC than NTCU alone and this effect was paralleled by COPD-like chronic inflammation manifested by induction of inflammatory cytokines, activation of inflammatory signaling pathways and pathways involved in cell growth and survival. Dietary administration of DIM significantly reduced the incidence of NTCU plus LPS-induced LSCC and inflammatory reactions. Thus, our inflammation-driven NTCU model of LSCC is suitable to study the efficacy of chemopreventive agents against LSCC. The findings from the present study indicate that DIM is a promising agent for the chemoprevention of human LSCC and studies should be initiated to test its efficacy in clinical trials.
Acknowledgments
We want to express our indebtedness to Bob Carlson for his help in formatting the figures and to Dr. Michael Zeligs for kindly providing us BioResponse DIM.
Grant Support: This study was supported by NCI/NIH grant (R21CA164235-01A1) to FK.
Footnotes
Conflict of Interest Statement: We confirm that there are no known conflicts of interest associated with this publication.
Reference List
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 3.Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001;18:1059–1068. doi: 10.1183/09031936.01.00275301. [DOI] [PubMed] [Google Scholar]
- 4.Wistuba II. Histologic evaluation of bronchial squamous lesions: any role in lung cancer risk assessment? Clin Cancer Res. 2005;11:1358–1360. doi: 10.1158/1078-0432.CCR-04-2156. [DOI] [PubMed] [Google Scholar]
- 5.Cancer Genome Atlas Research Network (CGARN) Comprehensive genomic characterization of squamous cell lung cancers. Nature. 2012;489:519–525. doi: 10.1038/nature11404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imielinski M, Berger AH, Hammerman PS, Hernandez B, Pugh TJ, Hodis E, et al. Mapping the hallmarks of lung adenocarcinoma with massively parallel sequencing. Cell. 2012;150:1107–1120. doi: 10.1016/j.cell.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Zhang Z, Yan Y, Lemon WJ, LaRegina M, Morrison C, et al. A chemically induced model for squamous cell carcinoma of the lung in mice: histopathology and strain susceptibility. Cancer Res. 2004;64:1647–1654. doi: 10.1158/0008-5472.can-03-3273. [DOI] [PubMed] [Google Scholar]
- 8.Skillrud DM, Offord KP, Miller RD. Higher risk of lung cancer in chronic obstructive pulmonary disease. A prospective, matched, controlled study. Ann Intern Med. 1986;105:503–507. doi: 10.7326/0003-4819-105-4-503. [DOI] [PubMed] [Google Scholar]
- 9.Papi A, Casoni G, Caramori G, Guzzinati I, Boschetto P, Ravenna F, et al. COPD increases the risk of squamous histological subtype in smokers who develop non-small cell lung carcinoma. Thorax. 2004;59:679–681. doi: 10.1136/thx.2003.018291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caramori G, Casolari P, Cavallesco GN, Giuffre S, Adcock I, Papi A. Mechanisms involved in lung cancer development in COPD. Int J Biochem Cell Biol. 2011;43:1030–1044. doi: 10.1016/j.biocel.2010.08.022. [DOI] [PubMed] [Google Scholar]
- 11.Purdue MP, Gold L, Jarvholm B, Alavanja MCR, Ward MH, Vermeulen R. Impaired lung function and lung cancer incidence in a cohort of Swedish construction workers. Thorax. 2007;62:51–56. doi: 10.1136/thx.2006.064196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malkinson AM. Role of inflammation in mouse lung tumorigenesis: a review. Exp Lung Res. 2005;31:57–82. doi: 10.1080/01902140490495020. [DOI] [PubMed] [Google Scholar]
- 14.Hasday JD, Bascom R, Costa JJ, Fitzgerald T, Dubin W. Bacterial endotoxin is an active component of cigarette smoke. Chest. 1999;115:829–835. doi: 10.1378/chest.115.3.829. [DOI] [PubMed] [Google Scholar]
- 15.Larsson L, Pehrson C, Dechen T, Crane-Godreau M. Microbiological components in mainstream and sidestream cigarette smoke. Tob Induc Dis. 2012;10:13–17. doi: 10.1186/1617-9625-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Korsgren M, Linden M, Entwistle N, Cook J, Wollmer P, Andersson M, et al. Inhalation of LPS induces inflammatory airway responses mimicking characteristics of chronic obstructive pulmonary disease. Clin Physiol Funct Imaging. 2012;32:71–79. doi: 10.1111/j.1475-097X.2011.01058.x. [DOI] [PubMed] [Google Scholar]
- 17.Rakoff-Nahoum S. Why cancer and inflammation? Yale J Biol Med. 2006;79:123–130. [PMC free article] [PubMed] [Google Scholar]
- 18.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kyriakis JM, Avruch J. Mammalian MAPK signal transduction pathways activated by stress and inflammation: a 10-year update. Physiol Rev. 2012;92:689–737. doi: 10.1152/physrev.00028.2011. [DOI] [PubMed] [Google Scholar]
- 20.Grivennikov SI, Karin M. Dangerous liaisons: STAT3 and NF-kappaB collaboration and crosstalk in cancer. Cytokine Growth Factor Rev. 2010;21:11–19. doi: 10.1016/j.cytogfr.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsao AS, McDonnell T, Lam S, Putnam JB, Bekele N, Hong WK, et al. Increased phospho-AKT (SeR473)) expression in bronchial dysplasia: implications for lung cancer prevention studies. Cancer Epidemiol Biomarkers Prev. 2003;12:660–664. [PubMed] [Google Scholar]
- 22.Tichelaar JW, Zhang Y, leRiche JC, Biddinger PW, Lam S, Anderson MW. Increased staining for phospho-Akt, p65/RELA and cIAP-2 in pre-neoplastic human bronchial biopsies. BMC Cancer. 2005;5:155. doi: 10.1186/1471-2407-5-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Massion PP, Taflan PM, Shyr Y, Rahman SMJ, Yildiz P, Shakthour B, et al. Early involvement of the phosphatidylinositol 3-kinase/Akt pathway in lung cancer progression. Am J Respir Crit Care Med. 2004;170:1088–1094. doi: 10.1164/rccm.200404-487OC. [DOI] [PubMed] [Google Scholar]
- 24.Gustafson AM, Soldi R, Anderlind C, Scholand MB, Qian J, Zhang X, et al. Airway PI3K pathway activation is an early and reversible event in lung cancer development. Sci Transl Med. 2010;2:26. doi: 10.1126/scitranslmed.3000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Piyathilake CJ, Frost AR, Manne U, Weiss H, Heimburger DC, Grizzle WE. Nuclear accumulation of p53 is a potential marker for the development of squamous cell lung cancer in smokers. Chest. 2003;123:181–186. doi: 10.1378/chest.123.1.181. [DOI] [PubMed] [Google Scholar]
- 26.Inage Y, Ogata T, Yamamoto T, Akaogi E, Horiguchi H, Kamma H, et al. Topographical analysis of p53 expression and DNA ploidy in early bronchial squamous cell carcinoma and preneoplastic lesions. Lung Cancer. 2001;34:351–361. doi: 10.1016/s0169-5002(01)00262-8. [DOI] [PubMed] [Google Scholar]
- 27.Martin B, Verdebout JM, Mascaux C, Paesmans M, Rouas G, Verhest A, et al. Expression of p53 in preneoplastic and early neoplastic bronchial lesions. Oncol Rep. 2002;9:223–229. [PubMed] [Google Scholar]
- 28.Rennard SI. COPD: overview of definitions, epidemiology, and factors influencing its development. Chest. 1998;113:235S–241S. doi: 10.1378/chest.113.4_supplement.235s. [DOI] [PubMed] [Google Scholar]
- 29.Balansky R, Ganchev G, Iltcheva M, Steele VE, D'Agostini F, De Flora S. Potent carcinogenicity of cigarette smoke in mice exposed early in life. Carcinogenesis. 2007;28:2236–2243. doi: 10.1093/carcin/bgm122. [DOI] [PubMed] [Google Scholar]
- 30.Wang Y, Rouggly L, You M, Lubet R. Animal models of lung cancer characterization and use for chemoprevention research. Prog Mol Biol Transl Sci. 2012;105:211–226. doi: 10.1016/B978-0-12-394596-9.00007-X. [DOI] [PubMed] [Google Scholar]
- 31.Rehm S, Lijinsky W, Singh G, Katyal SL. Mouse bronchiolar cell carcinogenesis. Histologic characterization and expression of Clara cell antigen in lesions induced by N-nitrosobis-(2-chloroethyl) ureas. Am J Pathol. 1991;139:413–422. [PMC free article] [PubMed] [Google Scholar]
- 32.Hudish TM, Opincariu LI, Mozer AB, Johnson MS, Cleaver TG, Malkoski SP, et al. N-Nitroso-tris-chloroethylurea induces premalignant squamous dysplasia in mice. Cancer Prev Res (Phila) 2012;5:283–289. doi: 10.1158/1940-6207.CAPR-11-0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan J, Zhang Q, Li K, Liu Q, Wang Y, You M. Chemoprevention of lung squamous cell carcinoma by ginseng. Cancer Prev Res (Phila) 2013;6:530–539. doi: 10.1158/1940-6207.CAPR-12-0366. [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Zhang Z, Garbow JR, Rowland DJ, Lubet RA, Sit D, et al. Chemoprevention of lung squamous cell carcinoma in mice by a mixture of Chinese herbs. Cancer Prev Res (Phila) 2009;2:634–640. doi: 10.1158/1940-6207.CAPR-09-0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vernooy JHJ, Dentener MA, van Suylen RJ, Buurman WA, Wouters EFM. Long-term intratracheal lipopolysaccharide exposure in mice results in chronic lung inflammation and persistent pathology. Am J Respir Cell Mol Biol. 2002;26:152–159. doi: 10.1165/ajrcmb.26.1.4652. [DOI] [PubMed] [Google Scholar]
- 36.Kharitonov SA, Sjobring U. Lipopolysaccharide challenge of humans as a model for chronic obstructive lung disease exacerbations. Contrib Microbiol. 2007;14:83–8100. doi: 10.1159/000107056. [DOI] [PubMed] [Google Scholar]
- 37.Melkamu T, Qian X, Upadhyaya P, O'Sullivan MG, Kassie F. Lipopolysaccharide enhances mouse lung tumorigenesis: a model for inflammation-driven lung cancer. Vet Pathol. 2013;50:895–902. doi: 10.1177/0300985813476061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hussain SP, Harris CC. Inflammation and cancer: an ancient link with novel potentials. Int J Cancer. 2007;121:2373–2380. doi: 10.1002/ijc.23173. [DOI] [PubMed] [Google Scholar]
- 39.Schetter AJ, Heegaard NHH, Harris CC. Inflammation and cancer: interweaving microRNA, free radical, cytokine and p53 pathways. Carcinogenesis. 2010;31:37–49. doi: 10.1093/carcin/bgp272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolf JS, Chen Z, Dong G, Sunwoo JB, Bancroft CC, Capo DE, et al. IL (interleukin)-1alpha promotes nuclear factor-kappaB and AP-1-induced IL-8 expression, cell survival, and proliferation in head and neck squamous cell carcinomas. Clin Cancer Res. 2001;7:1812–1820. [PubMed] [Google Scholar]
- 41.Balkwill F. Tumour necrosis factor and cancer. Nat Rev Cancer. 2009;9:361–371. doi: 10.1038/nrc2628. [DOI] [PubMed] [Google Scholar]
- 42.Bromberg JF, Wrzeszczynska MH, Devgan G, Zhao Y, Pestell RG, Albanese C, et al. Stat3 as an oncogene. Cell. 1999;98:295–303. doi: 10.1016/s0092-8674(00)81959-5. [DOI] [PubMed] [Google Scholar]
- 43.Weber A, Wasiliew P, Kracht M. Interleukin-1beta (IL-1beta) processing pathway. Sci Signal. 2010;3:cm2. doi: 10.1126/scisignal.3105cm2. [DOI] [PubMed] [Google Scholar]
- 44.Heinrich PC, Behrmann I, Haan S, Hermanns HM, Muller-Newen G, Schaper F. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem J. 2003;374:1–20. doi: 10.1042/BJ20030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nicholson KM, Anderson NG. The protein kinase B/Akt signalling pathway in human malignancy. Cell Signal. 2002;14:381–395. doi: 10.1016/s0898-6568(01)00271-6. [DOI] [PubMed] [Google Scholar]
- 46.Inoue K, Kurabayashi A, Shuin T, Ohtsuki Y, Furihata M. Overexpression of p53 protein in human tumors. Med Mol Morphol. 2012;45:115–123. doi: 10.1007/s00795-012-0575-6. [DOI] [PubMed] [Google Scholar]
- 47.Rivlin N, Brosh R, Oren M, Rotter V. Mutations in the p53 tumor suppressor gene: important milestones at the various steps of tumorigenesis. Genes Cancer. 2011;2:466–474. doi: 10.1177/1947601911408889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hussain SP, Amstad P, Raja K, Ambs S, Nagashima M, Bennett WP, Shields PG, Ham AJ, Swenberg JA, Marrogi AJ, Harris CC. Increased p53 mutation load in noncancerous colon tissue from ulcerative colitis: a cancer-prone chronic inflammatory disease. Cancer Res. 2000;60:3333–3337. [PubMed] [Google Scholar]
- 49.Banerjee S, Kong D, Wang Z, Bao B, Hillman GG, Sarkar FH. Attenuation of multi-targeted proliferation-linked signaling by 3,3'-diindolylmethane (DIM): from bench to clinic. Mutat Res. 2011;728:47–66. doi: 10.1016/j.mrrev.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Qian X, Song JM, Melkamu T, Upadhyaya P, Kassie F. Chemoprevention of lung tumorigenesis by intranasally administered diindolylmethane in A/J mice. Carcinogenesis. 2013;34:841–849. doi: 10.1093/carcin/bgs390. [DOI] [PMC free article] [PubMed] [Google Scholar]