Abstract
Background
Oral breathing causes many changes in the facial anatomical structures in adult patients. In this study we aimed to determine the effects of long-term oral breathing (>5 years) on the maxillary sinus volumes among adult male patients.
Material/Methods
We accessed medical records of 586 patients who had undergone cone beam computed tomography (CBCT) for any reason between September 2013 and April 2014. Patients who had undergone cone-beam dental volumetric tomography scans for any reason and who had answered a questionnaire about breathing were screened retrospectively. Cone beam dental volumetric tomography (I-Cat, Imaging Sciences International, Hatfield, PA, USA) was used to take the images of the maxillo-facial area at a setting of 120 kVp and 3.7 mA. This study involved male patients older than 21 years of age.
Results
The study included a total of 239 male patients, of which 68 were oral breathers and 171 were nasal breathers. The mean age of the oral breathers was 48.4 years and that of the nasal breathers was 46.7 years and the difference was not statistically significant (p>0.05). The mean maxillary sinus volumes of the oral and nasal breathers were 9043.49±1987.90 and 10851.77±2769.37, respectively, and the difference in maxillary sinus volume between the 2 groups was statistically significant (p<0.001).
Conclusions
The volume of maxillary sinus in oral breathers (>5 years) was significantly lower than in nasal breathers, but it remains unclear whether this is due to malfunctioning of the nasal cavity or due to the underlying pathological condition.
MeSH Keywords: Cone-Beam Computed Tomography; Imaging, Three-Dimensional; Maxillary Sinus; Mouth Breathing
Background
Breathing requires the free flow of air through the nose in normal conditions. Essential for proper growth and development of the craniofacial complex, nasal respiration is primordial [1]. However, due to nasal septum deviations, craniofacial deformities, tumors, or habit; oral breathing may replace nasal breathing for supplementation or a mixed breathing [2]. Oral breathing is regarded as a pathological condition because it may cause health problems such as changes in orofacial muscle tone, dry mouth, occlusal changes, chewing and swallowing pattern deviations, dental caries, periodontal diseases, and speech and sleep disorders [3,4]. Oral breathing has been reported to have a prevalence of over 50% among children [5,6].
Anatomically, the nasal cavity and maxillary sinuses share a common bony wall and the sinuses are thought to be able to act as zones of accommodation for variations in nasal cavity diameter, which can be altered by breathing pattern [7]. The maxillary and mandibular intercanine and intermolar distances have been also shown to present significant differences between patients with different breathing patterns [8]. It has been determined that, if the causes of oral breathing are not corrected before the growth stages, this breathing pattern may have serious effects [9].
Cone beam computed tomography (CBCT) provides multiplanar images that can allow radiologists to inspect the entire volume of the acquired image [10]. The introduction of the CBCT exam is widely regarded as one of the greatest advances in recent years in diagnostic imaging in dentistry. CBCT examination of the maxilla anatomy is commonly requested during implant placement in the posterior maxilla [11].
In the literature, studies of the effects of oral breathing are generally focused on children. In this study, we aimed to determine the effects of long-term (>5 years) oral breathing on maxillary sinus volumes among male adults older than the 21 years of age.
Material and Methods
Generating data
Our study included medical records of a total of 586 patients who underwent CBCT for any reason between September 2013 and April 2014. From these 586 patients, we excluded 184 patients who had irregular breathing, declined to answer the questionnaire, had facial trauma or craniofacial anomalies, had systemic diseases, or who were younger than 21 years of age, as well as all 163 females. The study was approved by the Dicle University Medical Faculty Ethics Committee.
The present study included a retrospective analysis of medical records. Patients were asked about breathing habits during the last 5 years and they were included in the study if their breathing habits had not changed and if they had not undergone any treatment for breathing problems during this period. The questionnaire included questions about oral breathing during sleep and while awake. For patients who claimed to have oral breathing, 2 examiners (K.S.A and B.G.) performed further testing to confirm this with various diagnostic assessments such as water holding test, mirror condensation test, and cotton wisp test [12]. If any of these verification tests did yielded a negative result, the CBCT data of the patient were not included in the oral breathers group.
Patients who indicated they were oral breathers during sleeping or during day and night for longer than 5 years were selected. These 2 patient groups were evaluated together as the oral breathing group because the oral breathers during sleep indicated that they were also oral breathing sometimes during effort.
I-Cat imaging
Cone-beam dental volumetric tomography (I-Cat, Imaging Sciences International, Hatfield, PA, USA) was used to take images of the maxilla-facial area at a setting of 120 kVp and 3.7 mA. Images were obtained within 10 s (actual exposure time was 9 s). Each scan involved a number of separate, small, individual exposures (up to 440 frames) taken over 360°, with a voxel size of 0.300 mm.
MIMICS
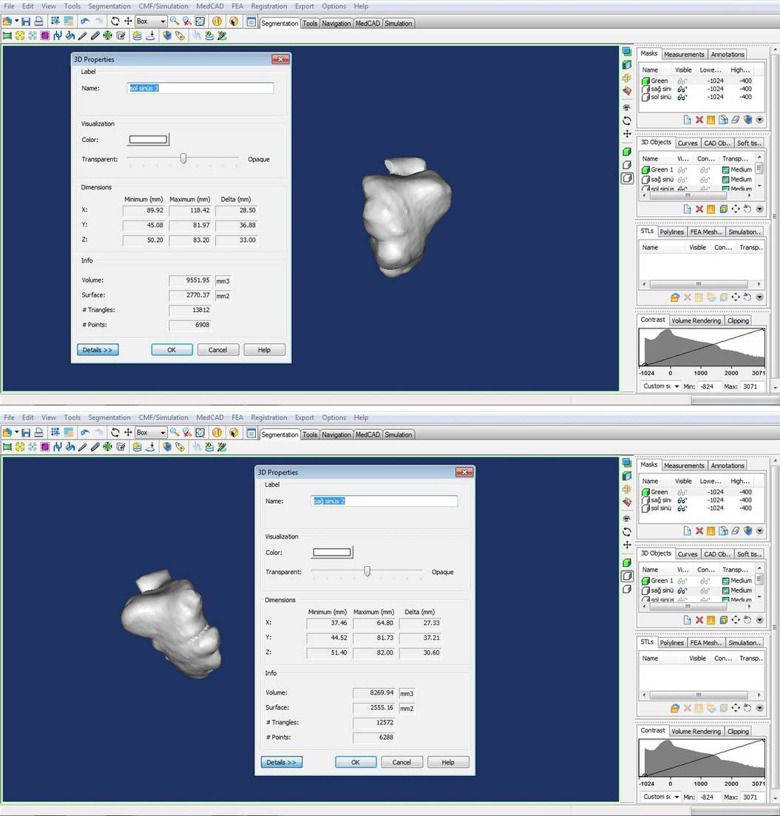
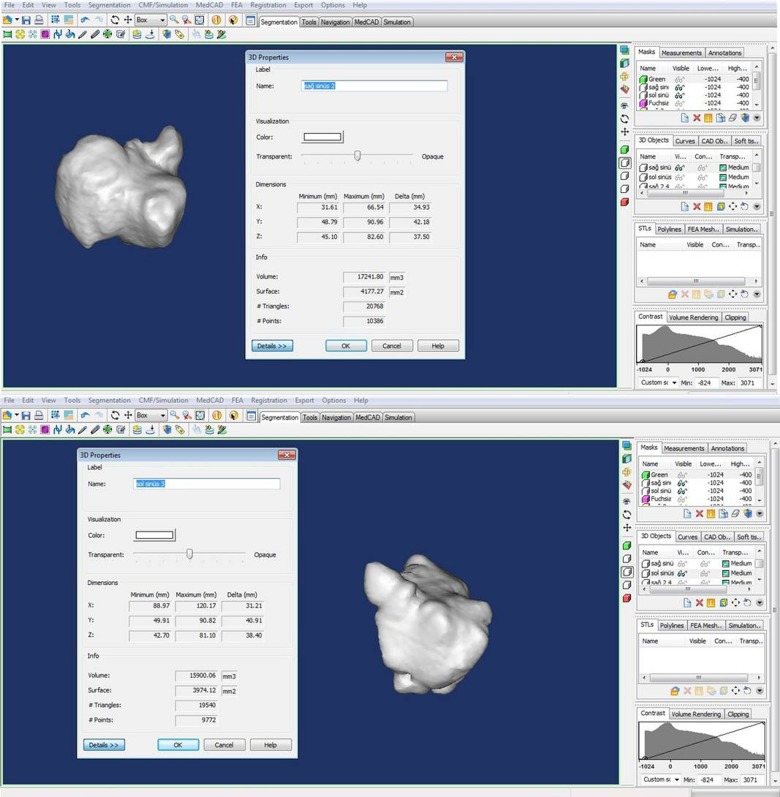
MIMICS 16.0 software (Materialise, Leuven, Belgium) is a link between the scanner data (CT, MRT, CBCT) and a simple virtual 3D representation. The data from CBCT scans were segmented slice-by-slice, rendered to create a 3-dimensional model of the maxillary sinus and evaluated by MIMICS 16.0 software. The data from CBCT scans were converted and segmented, using manual thresholds, by MIMICS 16.0 software. The threshold is necessary to create a first separation of the anatomical structures (bone, soft tissue, and sinus). A mask is generated for each structure and makes it possible to proceed within the work flow. The masks can be edited slice by slice by simply adding or removing voxels manually. Bone, soft tissue, and sinus were separated using the above-mentioned functions. For evaluating, separated sinus volume were distinguished from anatomical structures. Right and left maxillary sinus volumes of each patient were determined and the average of these 2 volumes was recorded for each patient (Figures 1–5).
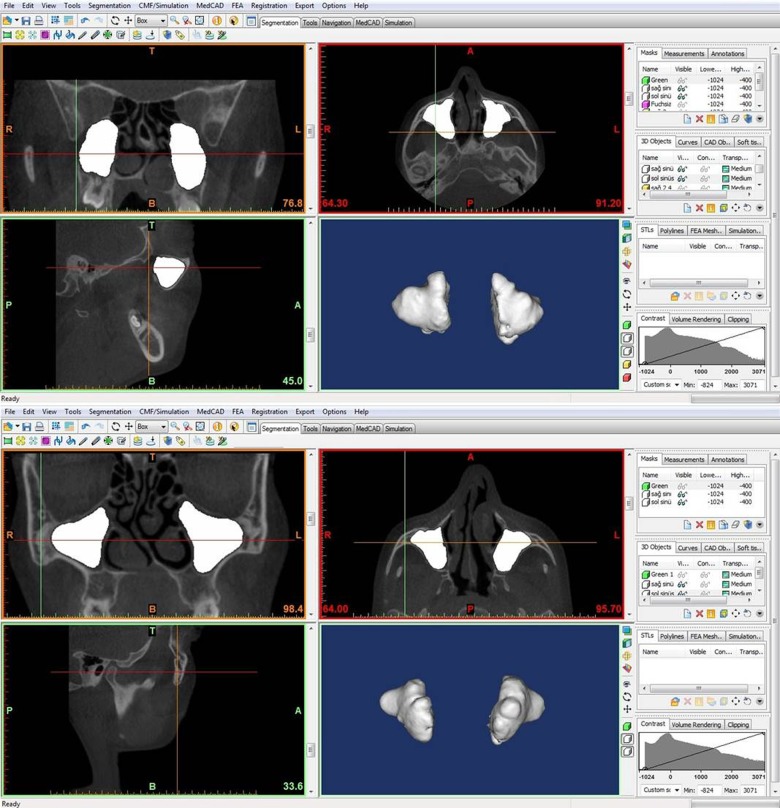
Figure 1.
The screen in determination of 3D sinus volume using MIMICS program in 2 samples of CBCT of the cases included in the study. The screen above is a sample CBCT of oral breathers and the screen below is a sample CBCT of nasal breathers.
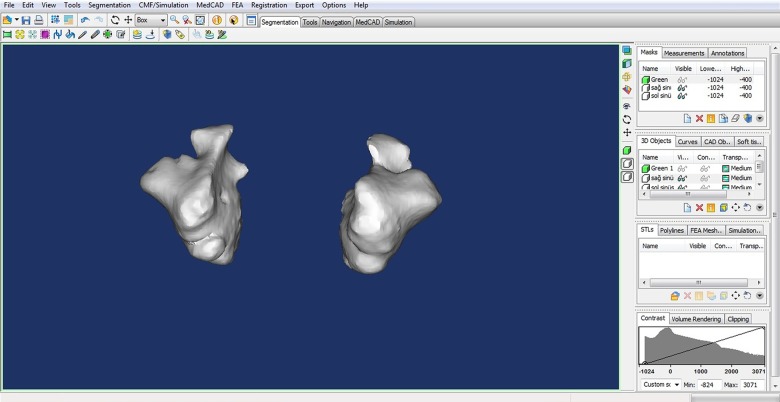
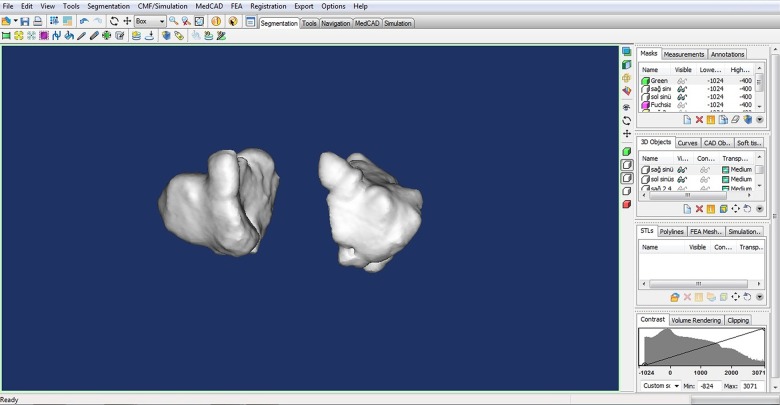
Figure 5.
An example of the 3D appearance of maxillary sinuses from the oral breathers group using the MIMICS program.
Statistical analysis
Statistical analyses were performed using SPSS 18.0 software (SPSS, Inc, Chicago, IL) and the data are expressed as mean ± standard deviation. Comparison of mean maxillary sinus volume data between groups was done using the t test. A p value of <0.05 was considered to be statistically significant.
Results
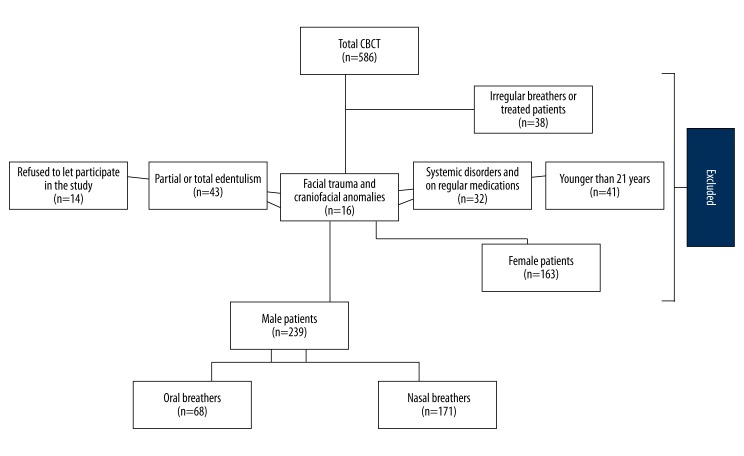
We included 239 male patients (Figure 6). Among those, 68 were oral breathers and 171 were nasal breathers. Age distribution of study participants is summarized in Table 1. Most of the patients were 50–59 years of age. The mean age of the oral breathers was 48.4 years and that of the nasal breathers was 46.7 years; the difference was not statistically significant (p>0.05).
Figure 6.
Distribution of study participants.
Table 1.
Age distribution of the study participants.
| Ages | Number of patients |
|---|---|
| <21 | 93 |
| 21–30 | 77 |
| 31–40 | 106 |
| 41–50 | 177 |
| 51–61 | 78 |
| >61 | 17 |
The mean maxillary sinus volume of the oral and nasal breathers were 9043.49±1987.90 mm3 and 10851.77±2769.37 mm3, respectively, and the difference in maxillary sinus volume between the 2 groups was statistically significant (p<0.001) (Table 2). The overall comparison between oral and nasal breathers showed that maxillary sinus volume showed a mean reduction in oral breathers (Figures 1, 4, 5). Due to oral breathing, the shape of the maxillary sinus may be affected. In oral breathing, changes have been observed in the maxilla and maxillary sinus.
Table 2.
The mean maxillary sinus volume of study participants.
| Mouth breathers (n: 68) | Nasal breathers (n: 171) | p | |
|---|---|---|---|
| Maxillary sinus volume (mm3) | 9043.49 ±1987.90 | 10851.77 ±2769.37 | <0.001 |
Figure 4.
From the oral breathers group, an example of the screen of left and right sinus for the measurement of maxillary sinus volume using the MIMICS program.
Discussion
In this study we have determined that the mean maxillary sinus volume decreases significantly in oral breathers compared with nasal breathers among adults with a constant breathing pattern of more than 5 years. To the best of our knowledge, this is the first study determining maxillary sinus volumes in different breathers with CBCT using the MIMICS program.
Our findings are in line with the results of Tikku et al., who had also reported smaller maxillary sinus volumes among oral breathers compared with the nasal breathers on 50 patients 12–14 years of age [12]. Tikku et al. calculated the maxillary sinus volume using a manual segmentation method from CBCT scans of 25 normal breathers and 25 oral breathers and determined the mean maxillary sinus volumes as 12.712±1.619 cm3 and 11.598±1.520 cm3 for nasal and oral breathers, respectively [12]. MIMICS software is better than manual segmentation, which Tikku et al. used. MIMICS software has many advantages over manual segmentation and other imaging software. These advantages are being user-friendly, providing quick and easy segmentation, best segmentation control and sensitivity, having tools to correct segmentation in 2D slices, and having threshold interval units (grey levels) compatible with other imaging software.
The influence of breathing pattern on craniofacial growth has been reported in many studies [13,14]. Oral breathers were reported to have longer faces [15]. Malhotra et al. reported that all subjects with oral-breathing habit exhibited significant increase in facial height, mandibular plane angle, and gonial angle [16]. In another study on 30 patients with a mean age of 13.1 years [17], the oral breathers showed reductions in facial, maxillary, and mandibular widths; nasion-sella-gnathion angle; and facial index. In a recent study, oral-breathing children were determined to have an increase in anterior lower facial height, the hyoid bone in a more elevated position, and more class II malocclusion compared to nose-breathing children [18]. Faria et al. studied 35 children ages 7–10 years and found a significant relationship in greater maxillo-mandibular retroposition and superior gonial angles in the oral breathers. However, in this study, any significant differences in other parameters, such as the inclination of the incisors or the distance and height of molars, were not determined [19]. Harari et al. reported that oral breathers demonstrated considerable backward and downward rotation of the mandible, increased overjet, increase in the mandible plane angle, a higher palatal plane, and narrowing of both upper and lower arches at the level of canines and first molars compared to the nasal breathers group [3].
Oral breathing was determined to reduce the vertical effect on the posterior teeth, which can affect the vertical position of posterior teeth negatively, leading to malocclusion [20]. Similarly, in a recent study, oral breathing was reported to decrease the chewing activity and to reduce the vertical effect upon posterior teeth [21]. Oral breathers were shown to have narrower hard palate at the level of second premolars and first molars, and deeper palate in the level of second premolars, when compared to nasal breathers [22].
In our study groups, the maxillary sinus showed growth and variations with pneumatization. The reduction in sinus volume may be due to either or both of these reasons: 1) chronic inflammation is prone to appear in the poorly growing maxillary sinus, which thickens the bony wall of the paranasal sinus, thereby inducing reduction in total volume; and 2) ethmoid infundibulum and middle meatus are narrowed by inflammation of the ostiomeatal complex and by bony anatomic variations in the nasal cavity, leading to impaired pneumatization of the paranasal sinus. Both causes appears logical but it is difficult to say whether this reduction in volume is due to the anatomical structure of maxillary sinus being affected due to unsuitable functioning of nasal cavity and inadequate pneumatization, or due to the underlying chronic inflammation.
The maxillary sinus, which occupies the upper two-thirds of the maxillary bone, functions to lighten the weight of the skull, to give resonance to the voice, and to warm and moisten inspired air [23]. Some factors have been reported to affect the maxillary sinus volume. Although there may be some differences during growth periods, in adulthood, males have larger sinuses than females. A significant difference of the maxillary sinus volume between males and females has been reported, but we only included males in the present study [24,25]. Although some reports suggested that the maxillary sinus volume increases with age, other studies did not find a significant effect of age on maxillary sinus volume [26,27]. Since we only included adults older than 21 years and the mean ages of the 2 groups were similar, we could not study the effects of age on maxillary sinus volume. However, Ariji et al. have described the correlation between craniocaudal diameter of the maxillary sinus, and body height and body weight [28]. We did not record the body height or weight of the subjects included in this study and this may be a limitation.
Although a large dose of ionizing radiation is delivered by medical computed tomography, CBCT technology has achieved considerable reduction of absorbed radiation doses, with equal image qualities and less artifacts for visualizing the maxillofacial structures compared to traditional CT imaging [29,30].
Conclusions
The volume of maxillary sinus in oral breathers (>5 years) was significantly smaller than in nasal breathers, but it remains unclear whether this is because of unsuitable functioning of the nasal cavity or is due to the underlying pathological condition. Therefore, it is difficult to say which is the main causative factor. Since oral breathing is a common condition, studies of the outcomes of this decline are warranted.
Figure 2.
From the nasal breathers group, an example of the screen of left and right sinus for the measurement of maxillary sinus volume using the MIMICS program.
Figure 3.
An example of the 3D appearance of maxillary sinuses from the nasal breathers group using the MIMICS program.
Acknowledgements
The authors thank the School of Dentistry, University of Dicle, and Dicle University Scientific Projects Coordination Office for software support.
Footnotes
Source of support: Departmental sources
References
- 1.Proffit WR, Fields HW, Server DM. Contemporary Orthodontics. 4th ed. St. Louis: Mosby; 2007. [Google Scholar]
- 2.Barros JRC, Becker HMG, Pinto JA. Avaliação de atopia em crianças respiradoras bucais atendidas em centro de referência. J Pediatr. 2006;82(6):458–64. [Google Scholar]
- 3.Harari D, Redlich M, Miri S, et al. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. Laryngoscope. 2010;120:2089–93. doi: 10.1002/lary.20991. [DOI] [PubMed] [Google Scholar]
- 4.Bakor SF, Pereira JC, Frascino S, et al. Demineralization of teeth in mouth-breathing patients undergoing maxillary expansion. Braz J Otorhinolaryngol. 2010;76:709–12. doi: 10.1590/S1808-86942010000600007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abreu RR, Rocha RL, Lamounier JA, Guerra AF. Etiology, clinical manifestations and concurrent findings in mouth-breathing children. J Pediatr (Rio J) 2008;84(6):529–35. doi: 10.2223/JPED.1844. [DOI] [PubMed] [Google Scholar]
- 6.Felcar JM, Bueno IR, Massan AC, et al. Prevalence of mouth breathing in children from an elementary school. Cien Saude Colet. 2010;15(2):437–44. doi: 10.1590/S1413-81232010000200020. [DOI] [PubMed] [Google Scholar]
- 7.Holton N, Yokley T, Butaric L. The morphological interaction between the nasal cavity and maxillary sinuses in living humans. Anat Rec (Hoboken) 2013;296(3):414–26. doi: 10.1002/ar.22655. [DOI] [PubMed] [Google Scholar]
- 8.Retamoso LB, Knop LA, Guariza Filho O, Tanaka OM. Facial and dental alterations according to the breathing pattern. J Appl Oral Sci. 2011;19(2):175–81. doi: 10.1590/S1678-77572011000200015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Defabjanis P. Impact of nasal airway obstruction on dentofacial development and sleep disturbances in children: preliminary notes. J Clin Pediatr Dent. 2003;27:95–100. doi: 10.17796/jcpd.27.2.27934221l1846711. [DOI] [PubMed] [Google Scholar]
- 10.Carter L, Farman AG, Geist J, et al. American Academy of Oral and Maxillofacial Radiology Executive Opinion Statement on Performing and Interpreting Diagnostic Cone Beam Computed Tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:561–62. doi: 10.1016/j.tripleo.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Rege IC, Sousa TO, Leles CR, Mendonça EF. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health. 2012;12:30. doi: 10.1186/1472-6831-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tikku T, Khannaemail R, Sachan K, et al. Dimensional changes in maxillary sinus of mouth breathers. J Oral Biology and Craniofacial Research. 2013;3(1):9–14. doi: 10.1016/j.jobcr.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weissheimer A, Menezes LM, Sameshima GT, et al. Imaging software accuracy for 3-dimensional analysis of the upper airway. Am J Orthod Dentofacial Orthop. 2012;142(6):801–13. doi: 10.1016/j.ajodo.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 14.Bosma JF. Maturation of function of the oral and pharyngeal region. Am J Orthod. 1963;49:94–104. [Google Scholar]
- 15.Góis EG1, Ribeiro-Júnior HC, Vale MP, et al. Influence of nonnutritive sucking habits, breathing pattern and adenoid size on the development of malocclusion. Angle Orthod. 2008;78(4):647–58. doi: 10.2319/0003-3219(2008)078[0647:IONSHB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Tourne LP. The long face syndrome and impairment of the nasopharyngeal airway. Angle Orthod. 1990;60:7–76. doi: 10.1043/0003-3219(1990)060<0167:TLFSAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Malhotra S, Pandey RK, Nagar A, et al. The effect of mouth breathing on dentofacial morphology of growing child. J Indian Soc Pedod Prev Dent. 2012;30(1):27–31. doi: 10.4103/0970-4388.95572. [DOI] [PubMed] [Google Scholar]
- 18.Bakor SF, Enlow DH, Pontes P, De Biase NG. Craniofacial growth variations in nasal-breathing, oral-breathing, and tracheotomized children. Am J Orthod Dentofacial Orthop. 2011;140(4):486–92. doi: 10.1016/j.ajodo.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 19.Chung Leng Muñoz I, Beltri Orta P. Comparison of cephalometric patterns in mouth breathing and nose breathing children. Int J Pediatr Otorhinolaryngol. 2014;78(7):1167–72. doi: 10.1016/j.ijporl.2014.04.046. [DOI] [PubMed] [Google Scholar]
- 20.Faria PT, de Oliveira Ruellas AC, Matsumoto MA, et al. Dentofacial morphology of mouth breathing children. Braz Dent J. 2002;13:129–32. doi: 10.1590/s0103-64402002000200010. [DOI] [PubMed] [Google Scholar]
- 21.Hsu HY, Yamaguchi K. Decreased chewing activity during mouth breathing. J Oral Rehabil. 2012;39(8):559–67. doi: 10.1111/j.1365-2842.2012.02306.x. [DOI] [PubMed] [Google Scholar]
- 22.Ikenaga N, Yamaguchi K, Daimon S. Effect of mouth breathing on masticatory muscle activity during chewing food. J Oral Rehabil. 2013;40(6):429–35. doi: 10.1111/joor.12055. [DOI] [PubMed] [Google Scholar]
- 23.Berwig LC, Silva AM, Côrrea EC, et al. Hard palate dimensions in nasal and mouth breathers from different etiologies. J Soc Bras Fonoaudiol. 2011;23(4):308–14. doi: 10.1590/s2179-64912011000400004. [DOI] [PubMed] [Google Scholar]
- 24.Dargaud J, Cotton F, Buttin R, Morin A. The maxillary sinus: evolution and function in aging. Morphologie. 2003;87(276):17–22. [PubMed] [Google Scholar]
- 25.Sahlstrand-Johnson P, Jannert M, Strömbeck A, Abul-Kasim K. Computed tomography measurements of different dimensions of maxillary and frontal sinuses. BMC Med Imaging. 2011;11:8. doi: 10.1186/1471-2342-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martınez RG, Swennen GRJ. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011;76:1–11. doi: 10.1016/j.ijom.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 27.Ariji Y, Kuroki T, Moriguchi S, et al. Age changes in the volume of the human maxillary sinus: a study using computed tomography. Dentomaxillofac Radiol. 1994;23(3):163–68. doi: 10.1259/dmfr.23.3.7835518. [DOI] [PubMed] [Google Scholar]
- 28.Ariji Y, Ariji E, Yoshiura K, Kanda S. Computed tomographic indices for maxillary sinus size in comparison with the sinus volume. Dentomaxillofac Radiol. 1996;25(1):19–24. doi: 10.1259/dmfr.25.1.9084281. [DOI] [PubMed] [Google Scholar]
- 29.Loubele M, Bogaerts R, Van Dijck E, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009;71:461–68. doi: 10.1016/j.ejrad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:106–14. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]