Abstract
Objective:
To assess postoperative pain in endodontic therapy and its association with clinical factors such as gender, age, tooth type, pulpal diagnosis, and preoperative pain, length of obturation and sealer extrusion.
Study Design:
Cross-Sectional study.
Place and Duration of Study:
Dental section of the Aga khan university hospital, Karachi, Pakistan from January to December 2009.
Methodology:
One hundred and forty patients (140) requiring endodontic therapy for molar and premolar teeth were included in this study. Local Anesthesia (2% Lidocain with 1:80,000 Epinephrine) was administered. The tooth was isolated with rubber dam. Access cavity was prepared with the help of round carbide No. 2 bur. Canal preparation was completed using crown-down technique. Access was sealed with sterile dry cotton pallet and restored temporarily with double layer of Glass ionomer cement and Cavit. After one week patients were recalled and access was re-opened, obturation was done using cold lateral condensation technique. Ca(OH)2 based sealer was used. Postoperative radiographs were taken. Patients were recalled after 24 hours and postobturation pain was recorded using Visual analogue scale (VAS).Data was obtained on a structured Performa. χ2 test was used for statistical analysis.
Results:
Pain was present in 42.9% of patients. Females more frequently experienced pain (65%) than males (35%). Preoperative pain was found to be significantly associated with postoperative pain (p value < 0.001). Obturation length was not found to be significantly associated with postoperative pain (p value 1.0). Sealer extrusion was not found to be significantly associated with postoperative (P value 0.547).
Keywords: Root canal treatment, Root canal obturation, Cold lateral condensation Technique, Postoperative pain
INTRODUCTION
Endodontic therapy or root canal treatment (RCT) is performed to manage pain and eliminate infection from teeth. Pain is a personal and subjective experience (1). Generally appropriate diagnosis and relevant treatment procedures are successful in effecting a cure (2). Postoperative pain after RCT has been reported from 1.9%-48% (3, 4). Post-treatment pain severity demonstrated a steady decrease in post operative pain prevalence over time (5). It is considered to be associated with periapical inflammatory response. It may persist from few hours to many days after endodontic therapy (3). The factors responsible for postoperative pain are unclear. Mechanical, chemical and microbial factors may be responsible for peri-radicular inflammation (6).
Pain is a subjective experience and difficult to quantify and standardize. Pain is influenced by many factors e.g. personality, behavior, physical and psychological factors. Numerical, verbal and visual analogue scales are used in most clinical studies (7). A categorical scale composed of no pain, mild, moderate, intense and unbearable pain was used in this study (Fig. 1). The categorical scale in spite of its simplicity is considered to be a reliable and reproducible measuring tool for clinical pain trials (8).
Figure 1.
Scales for pain measurement.
The purpose of endodontic therapy is to perform complete debridement and obturation of root canal system and to preserve the natural dentition. Its objective is to eliminate pulpal and peri-radicular microorganisms (9). Understanding the etiology of postoperative pain after obturation may greatly help clinicians to adopt strategies to prevent such highly distressing phenomenon (10).
The purpose of this study is to assess association of clinical factors such as gender, age, tooth type, preoperative pulpal diagnosis, and preoperative pain, length of obturation and sealer extrusion with postoperative pain in endodontic therapy.
MATERIALS AND METHODS
After obtaining permission from Ethical Review Committee of the institute One hundred and forty patients (140) visiting dental section, the Aga Khan University Hospital, Karachi, Pakistan were included in this study. Maxillary and mandibular molar and premolar teeth requiring endodontic therapy were included in this study. Third molar teeth were excluded. Patients previously on analgesics or antibiotic medications were excluded.
Preoperative pain was assessed by the application of cold (1,1,1,2 Tetrafluoroethane, TrueFlex, Ortho Technology, Inc, Tampa, Florida) and hot gutta-percha (Associated Dental Products Ltd, Kemdent Works, UK) and recorded as symptomatic or asymptomatic tooth. Pulp diagnosis was made on the basis of history and detailed clinical and radiographic examination as acute pulpitis, chronic pulpitis, pulpal necrosis and pulpal necrosis with apical periodontitis.
2% lidocain with 1:80,000 epinephrine local anesthesia (Xylestein, 3MESPE AG, Seefeld, Germany) was administered. The tooth was isolated by means of rubber dam (SafeTouch, AR Medicon Inc. Qubec, Canada). Access cavity was prepared with the help of roundcarbide No.2 bur and enlarged with Endo Z bur (Dentsply International, York, PA). Canal orifices were located and canal patency was checked with #10 K-file (Mani, Inc. Japan). Coronal and middle third was enlarged with S-1 and S-2 Protaper files (Dentsply Mallifer, Ballaigus, Switzerland). Canal orifices were enlarged with the help of Gates-Glidden burs G1-G3 (Mani, Inc. Japan). Determination ofworking length was made with Root ZX apex locator (J Morita Europe GVBH, Frankfurt, Germany) and with radiographs. Canals were prepared and shaped using crown down techniques with both manual and rotary instrumentation. During whole insturmenation RC Prep (Premier Dental Products Co. PA. USA) was used as canal lubricant and 5.25% Na HOCl was used as an irrigation solution. The canals orifices were protected with sterile dry cotton palletandthe access cavities weresealed temporarily with a double seal of Glass ionomercement (GC Corporation, Tokyo, Japan) andCavit (Meta Biomed Co. Gun Chongbuk Korea).
After one week patientswere recalled and the canals were re-opened, and obturation was performed using cold lateral condensation technique. Postoperative radiographs were taken. Radiographic length of root canal filling and sealer extrusion was recorded. Patients were recalled 24 hours after obturationand. Each patient received instructions on how to use a 10-cm visual analogue scale (VAS) to record postoperative pain (11). Immediately after each patient self recorded his/her pain, he/she was informed about the aim of the study. After that this score was transferred to a numerical value between 0 and 10 and to a verbal scale (none, mild, moderate, intense and unbearable) (Fig. 1).
Results were analyzed using SPSS 19.0. χ2 test was used for statistical analysis at 95% confidence interval. A p value of less than 0.05 was taken as statistically significant.
RESULTS
Postoperative pain after obturation during the follow –up period of 24 hours was recorded. Pain was present in 42.9%. The pain experienced was mild, moderate, andintense in 22.1%, 18.6% and 0.7% of the casesrespectively. 1.4% of patients experienced unbearable pain (Fig. 2). Frequency and percentages of gender, tooth type, preoperative pain, and diagnosis is presented in Table 1.
Figure 2.
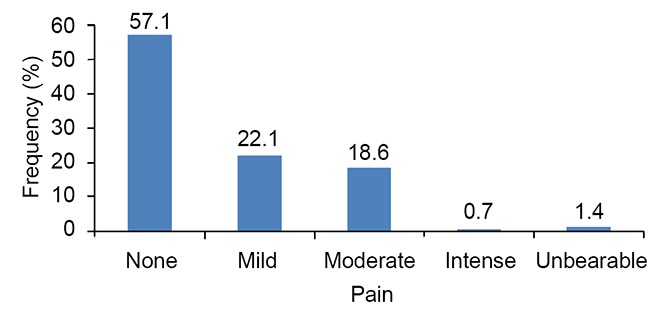
Frequency of postoperative pain.
Table 1.
Frequency and distribution of clinical variables
| Gender | Male n (%) | 59 (42.1%) |
| Female n (%) | 81 (57.9%) | |
| Type of Teeth | Mandibular Molars n (%) | 70 (50%) |
| Mandibular Premolars n (%) | 16 (11.4%) | |
| Maxillary Molars n (%) | 38 (27.1%) | |
| Maxillary Premolars n (%) | 16 (11.4%) | |
| Preoperative Pain | Asymptomatic n (%) | 72 (51.4%) |
| Symptomatic n (%) | 68 (48.6%) | |
| Diagnosis | Acute Pulpitis n (%) | 36 (25.7%) |
| Chronic Pulpitis n (%) | 35 (24%) | |
| Pulpal Necrosis n (%) | 14 (10%) | |
| Pulpal Necrosis with Apical Periodontitis n (%) | 55 (39.3%) |
Gender is not associated with postoperative painsignificantly (p value 0.167). More females (65%) experienced post-operative pain than males (35%). Pain was observed less frequently inmaxillary molars (28.3%) than inmandibular molars (47.6%). Association oftype of tooth withpostobtuartion pain was not found significant (p value 0.297) (Table 2).
Table 2.
Association of postoperative pain with other clinical variables
| Clinical Variables | Post operative pain absent | Post operative pain present | P Value | |
|---|---|---|---|---|
|
| ||||
| Gender | Males | 47.5% | 35% | 0.167 |
| Females | 52.5% | 65% | ||
| Type of tooth | Mandibular Molars | 52.5% | 47.6% | 0.297 |
| Mandibular Premolars | 7.5% | 16.7% | ||
| Maxillary Molars | 26.3% | 28.3% | ||
| Maxillary Premolars | 13.8% | 8.3% | ||
| Preoperative pain | Asymptomatic | 77.5% | 16.7% | <0.001 |
| Symptomatic | 22.5% | 83.3% | ||
| Diagnosis | Acute Pulpitis | 21.3% | 31.7% | 0.431 |
| Chronic Pulpitis | 26.3% | 23.3% | ||
| Pulpal necrosis | 12.5% | 6.7% | ||
| Pulpal necrosis with apical periodontitis | 40% | 38.3% | ||
| Length of Obturation | within 2mm | 91.3% | 91.7% | 1.0 |
| short | 5% | 5% | ||
| overextended | 3.8% | 3.3% | ||
| Sealer extrusion | Present | 21.3% | 26.7% | 0.547 |
| Absent | 78.8% | 73.3% | ||
Chi Square test (Fisher’s Exact test where applicable) is used at 95% confidence interval, α =5%.
83.3% preoperative symptomatic teeth presented with postoperative pain as compared to 16.7% asymptomatic teeth that presented with postoperative pain (Table 2). Preoperative pain was found to be significantly associated with postoperative pain (p value < 0.001).Obturation length was not significantly associated with post-operative pain (p value 1.00) (Table 2).
Sealer extrusion is not associated significantly with postoperative pain (P value 0.547).
DISCUSSION
In this study a visual analogue scale was used to assess postoperative pain. This is a valid and reliable method which has been widely used in endodontic literature (12-14). Patients were informed the aim of the study after self recorded their pain level. In this manner, the Hawthorne effect i.e. the mere awareness of participants in an investigation can alter the way in which a person behaves, was minimized (15).
There are few studies to assess postoperative pain in endodontic therapy (16, 17). Results of this study showed that postoperative pain was absent in 57.1% but 22.1 % felt mild pain and 18.6% have moderate pain. Our results are comparable to other studies, Segura-Egea et al reported moderate to intense pain in 12% (16).
Greater pain has been reported in women than men (17). Reduced pain threshold is being observed in females than males (18). According to Polycarpou et al. female gender was considered important risk factor associated with persistent pain after endodontic therapy (13). This study also supports these reports. In this study, females more frequently experienced pain (65%) than males (35%).
Tooth type is not associated significantly with postoperative pain in this study (p value 0.297). Similar results are found in other studies (19, 21). Mandibular molars had greater moderate pain (50%) than maxillary molars (34.6%). These results are similar to other studies that described greater moderate pain in mandibular molars than maxillary molars. (16, 21) Results of this study disagrees with Ryan et al (22), who presented gender (female) and tooth type (molars) as factors that significantly influenced postoperative pain.
This study showed that teeth with acute pulpitis (34.5%) had greater moderate pain than teeth with chronic pulpitis (23.1%), pulp necrosis (11.5%) and apical periodontitis (30.8%). These results are similar to Dummer et al. (23) who found that 87% of patients who suffered from acute pulpitis reported severe pain.
In this study preoperative pain is associated significantly with postoperative pain (p value < 0.001). Teeth presented with preoperative pain more frequently experienced postoperative pain (83.3%) than previously asymptomatic teeth (16.7%). Similar results were found by Abdel Hameed et al. (24) which showed greater incidence of postoperative pain (15.9%)in preoperatively symptomatic teeth than in asymptomatic teeth (7.1%). Association of preoperative pain with postoperative pain has been documented in other studies as well (3, 21, 25). Sealer extrusion had not any association with postoperative pain (p value 0.547).
CONCLUSION
Female gender, mandibular molar teeth and presence of preoperative symptoms are risk factors associated with postoperative pain in endodontic therapy. A significant association of presence of preoperative symptoms with postoperative pain was observed.
REFERENCES
- 1.Yu VS, Messer HH, Yee R, Shen L. Incidence and impact of painful exacerbations in a cohort with post-treatment persistent endodontic lesions. J. Endod. 2012 Jan;38(1):41–46. doi: 10.1016/j.joen.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Oshima K, Ishii T, Ogura Y, Aoyama Y, et al. Clinical investigation of patients who develop neuropathic tooth pain after endodontic procedures. J. Endod. 2009 Jul;35(7):958–961. doi: 10.1016/j.joen.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Siqueira JF, Jr., Rocas IN, Favieri A, Machado AG, et al. Incidence of postoperative pain after intracanal procedures based on an antimicrobial strategy. J. Endod. 2002 Jun;28(6):457–460. doi: 10.1097/00004770-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Harrison JW, Baumgartner JC, Svec TA. Incidence of pain associated with clinical factors during and after root canal therapy. Part 2. Postobturation pain. J. Endod. 1983 Oct;9(10):434–438. doi: 10.1016/S0099-2399(83)80259-3. [DOI] [PubMed] [Google Scholar]
- 5.Pak JG, White SN. Pain prevalence and severity before, during, and after root canal treatment: A systematic review. J. Endod. 2011 Apr;37(4):429–438. doi: 10.1016/j.joen.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 6.El Mubarak AH, Abu-bakr NH, Ibrahim YE. Postoperative pain in multiple-visit and single-visit root canal treatment. J. Endod. 2010 Jan;36(1):36–39. doi: 10.1016/j.joen.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Siqueira JF., Jr Reaction of periradicular tissues to root canal treatment: benefits and drawbacks. Endod Topics. 2005;10:123–147. [Google Scholar]
- 8.Attar S, Bowles WR, Baisden MK, Hodges JS, et al. Evaluation of pretreatment analgesia and endodontic treatment for postoperative endodontic pain. J. Endod. 2008 Jun;34(6):652–655. doi: 10.1016/j.joen.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 9.Torabinejad M. Philadelphia: Saunders; 2002. Endodontics: Principles and practice. [Google Scholar]
- 10.Siqueira JF., Jr Microbial causes of endodontic flare-ups. Int. Endod J. 2003 Jul;36(7):453–463. doi: 10.1046/j.1365-2591.2003.00671.x. [DOI] [PubMed] [Google Scholar]
- 11.Huskinsson EC. Measurement of pain. Lancet. 2003;2:1127–1131. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 12.Hargreaves KM, Keiser K. Local anesthetic failure in endodontics: mechanisms and management. Endod Topics. 2002;1:26–39. [Google Scholar]
- 13.Polycarpou N, Ng YL, Canavan D, Moles DR, et al. Prevalence of persistent pain after endodontic treatment and factors affecting its occurrence in cases with complete radiographic healing. Int. Endod J. 2005 Mar;38(3):169–178. doi: 10.1111/j.1365-2591.2004.00923.x. [DOI] [PubMed] [Google Scholar]
- 14.Sathorn C, Parashos P, Messer H. The prevalence of postoperative pain and flare-up in single- and multiple-visit endodontic treatment: a systematic review. Int. Endod J. 2008;41:91–99. doi: 10.1111/j.1365-2591.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 15.De Amici D, Klersy C, Ramajoli F, Brustia L, et al. Impact of the Hawthorne effect in a longitudinal clinical study: the case of anesthesia. Control Clin. Trials. 2000 Apr;21(2):103–114. doi: 10.1016/s0197-2456(99)00054-9. [DOI] [PubMed] [Google Scholar]
- 16.Segura-Egea JJ, Cisneros-Cabello R, Llamas-Carreras JM, Velasco-Ortega E. Pain associated with root canal treatment. Int. Endod J. 2009 Jul;42(7):614–620. doi: 10.1111/j.1365-2591.2009.01562.x. [DOI] [PubMed] [Google Scholar]
- 17.Georgopoulou M, Anastassiadis P, Sykaras S. Pain after chemomechanical preparation. Int. Endod J. 1986 Nov;19(6):309–314. doi: 10.1111/j.1365-2591.1986.tb00495.x. [DOI] [PubMed] [Google Scholar]
- 18.Unruh AM, Ritchie J, Merskey H. Does gender affect appraisal of pain and pain coping strategies? Clin. J. Pain. 1999;15:31–40. doi: 10.1097/00002508-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Liddell A, Locker D. Gender and age differences in attitudes to dental pain and dental control. Community Dent Oral Epidemiol. 1997 Aug;25(4):314–318. doi: 10.1111/j.1600-0528.1997.tb00945.x. [DOI] [PubMed] [Google Scholar]
- 20.Harrison JW, Gaumgartner JC, Svec TA. Incidence of pain associated with clinical factors during and after root canal therapy. Part 1. Interappointment pain. J. Endod. 1983 Sep;9(9):384–387. doi: 10.1016/s0099-2399(83)80190-3. [DOI] [PubMed] [Google Scholar]
- 21.Yesilsoy C, Koren LZ, Morse DR, Rankow H, et al. Post-endodontic obturation pain: a comparative evaluation. Quintessence Int. 1988 Jun;19(6):431–438. [PubMed] [Google Scholar]
- 22.Ryan JL, Jureidini B, Hodges JS, Baisden M, et al. Gender differences in analgesia for endodontic pain. J. Endod. 2008 May;34(5):552–556. doi: 10.1016/j.joen.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Dummer PM, Hicks R, Huws D. Clinical signs and symptoms in pulp disease. Int. Endod J. 1980 Jan;13(1):27–35. doi: 10.1111/j.1365-2591.1980.tb00834.x. [DOI] [PubMed] [Google Scholar]
- 24.El Mubarak AH, Abu-bakr NH, Ibrahim YE. Postoperative pain in multiple-visit and single-visit root canal treatment. J. Endod. 2010 Jan;36(1):36–39. doi: 10.1016/j.joen.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Goreva LA, Petrikas A. Postobturation pain associated with endodontic treatment. Stomatologiia (Mosk) 2004;83(2):14–16. [PubMed] [Google Scholar]


