Abstract
Objective
Methadone maintenance treatment (MMT) has been implemented in China since 2004 and has expanded into a nationwide programme. This study aims to evaluate changes in social functioning, family relations and drug-related criminal behaviour among MMT clients in China.
Design
Systematic review and meta-analysis.
Methods
Both English and Chinese literature databases, including PubMed, Chongqing VIP Chinese Science and Technology Journals Database (CQVIP), China National Knowledge Infrastructure (CNKI) and Wanfang Data, were comprehensively searched over the period 2004–2014 for studied indicators. Study selection, quality assessment and data extraction were conducted according to the PRISMA (preferred reporting items for systematic reviews and meta-analyses) Statement. Meta-analyses were conducted using Comprehensive Meta-Analysis Biostat software.
Results
Thirty-eight articles were included in this review (1 in English and 37 in Chinese). The self-reported arrest rate decreased from 13.1% (95% CI 9.1% to 18.5%) at baseline to 3.4% (95% CI 1.5% to 7.7%) and 4.3% (95% CI 1.6% to 11.4%) after 6 and 12 months of MMT intervention, respectively. The rate of drug selling decreased from 7.6% (95% CI 3.8% to 14.8%) at baseline to 1.9% (95% CI 0.6% to 6.2%) and 3.0% (95% CI 1.0% to 8.9%) after 6 and 12 months of intervention, respectively. Similarly, the rates of selling sex for drugs and drug-related crime decreased from 5.3% (95% CI 2.4% to 11.1%) and 9.9% (95% CI 6.8% to 14.2%) at baseline to 1.1% (95% CI 0.5% to 2.3%) and 3.4% (95% CI 2.5% to 4.5%) at 6 months, then to 0.8% (95% CI 0.3% to 1.9%) and 3.4% (95% CI 0.8% to 13.1%) at 12 months after treatment initiation, respectively. In contrast, the rate of employment of clients and the proportion of clients having a good relationship with their family increased substantially from 26.4% (95% CI 22.9% to 30.1%) and 37.9% (95% CI 32.0% to 44.2%) to 41.6% (95% CI 36.6% to 48.0%) and 59.6% (95% CI 48.1% to 70.2%) at 6 months, then to 59.8% (95% CI 52.4% to 66.8%) and 75.0% (95% CI 69.0% to 80.2%) at 12 months after treatment initiation, respectively.
Conclusions
MMT has significantly reduced criminal activity, and improved employment rate and social well-being, of clients of the MMT programme. MMT is an effective measure to help drug users to resume societal and familial functions in China.
Keywords: PUBLIC HEALTH
Strengths and limitations of this study.
-
▪
This is the first study to review how methadone maintenance treatment (MMT) intervention can influence change in social functioning and family relations among drug users in MMT clinics in China.
-
▪
This study evaluated, through a meta-analysis of published literature since 2004 in China, changes in drug-related criminal behaviour and improvements in social functioning and family relations among drug users before and after initiating MMT interventions.
-
▪
The number of studies is limited and may lead to problems about representativeness of the large drug user population in China.
Introduction
Illicit drug misuse is a social and public health issue internationally. It not only increases the risk of transmission of diseases due to HIV and hepatitis C virus,1 2 but also increases drug-related criminal activity, family problems and healthcare expenditure.3 4 Heroin is the most common drug used among drug users in both developed and developing countries.5–7 Methadone maintenance treatment (MMT) has been found to be an effective harm-reduction programme for drug users.8–10 Methadone is a safe, low-cost and convenient generic drug for treatment of opioid dependence.11 12 It has effectively reduced drug-related mortality13–15 and drug-related crimes and helped drug users to resume social and familial functions.16–25
In 2004, eight outpatient MMT clinics were established in China.26 27 By 2012, these had expanded into a nationwide programme encompassing more than 756 clinics, covering 28 Chinese provinces. It has been shown that the eight pilot MMT clinics have significantly improved social functioning among MMT clients. The annual employment rate reportedly increased from 22.9% to 40.6% (p<0.01, compared with the baseline survey) and the proportion of clients with a harmonious relationship with their families increased from 49.6% to 65.8% (p<0.01) after MMT for 12 months. Self-reported criminal behaviour of clients also decreased from 20.7% to 3.8% (p<0.01).24 Similar benefits of MMT have also been reported in other countries. For instance, the employment rate for MMT clients in Malaysia increased from 70.1% to 77.6% after 2 years of treatment.28 A retrospective study in the UK also showed that the total number of convictions, theft and fraud convictions, and weeks spent in prison per year were reduced by 39.3% (p=0.03), 52.17% (p<0.001) and 82.8% (p=0.002), respectively.29
Numerous studies have reported improvements in social and family well-being among MMT clients in China, but a systematic review that synthesises all these effects is lacking. Through a meta-analysis of published literature since 2004 in China, this study aimed to evaluate changes in drug-related criminal behaviour and improvements in social functioning and family relations among drug users before and after MMT intervention.
Methods
Data sources
We conducted a systematic review of published peer-reviewed research articles by searching the following databases: PubMed, Chongqing VIP Chinese Science and Technology Journals Database (CQVIP), China National Knowledge Infrastructure (CNKI) and Wanfang Data from January 2004 to October 2014. Keywords used in the database search were (‘Methadone’ OR ‘Methadone maintenance treatment’ OR ‘Methadone maintenance therapy’ OR ‘Methadone maintenance’ OR ‘MMT’) AND (‘Crime’ OR ‘Criminal rates’ OR ‘Employment’ OR ‘Family relationship’ OR ‘Social functions’) AND (‘China’ OR ‘China mainland’ OR ‘Chinese’). We also performed a manual search of the reference lists of published articles. This review was reported according to the PRISMA (preferred reporting items for systematic reviews and meta-analyses) statement issued in 2009.30
Inclusion/exclusion criteria
Studies were eligible for inclusion in this systematic review if they met the following criteria: (1) articles published in Chinese or English; (2) study reported social functioning or family relations among clients in MMT programme at baseline and follow-up; (3) study characteristics, such as study location, investigation period, duration of intervention and sample size, were reported. Pre- and post-intervention studies among MMT clients were also included. Exclusion criteria were: (1) review papers; (2) non-peer-reviewed local/government reports; (3) conference abstracts and presentations; (4) dissertations.
Study selection
Selected studies were evaluated by two independent investigators (H-MS, X-YL) according to the inclusion and exclusion criteria. Any disagreement between the investigators was resolved by discussion. If the same study data were published in both English and Chinese, the articles published in Chinese were excluded from this study. In cases where multiple studies were found to use the same data source, we selected the first published study for inclusion in the meta-analysis.
Quality assessment
Two independent investigators used a validated quality assessment tool for observational studies31 to assess the quality of studies. The following eight items were assessed to calculate a total quality score: (1) clear definition of the target population; (2) representativeness of probability sampling; (3) sample characteristics matching the overall population; (4) adequate response rate; (5) method of data collection; (6) reliability of survey measures/instruments; (7) validity of survey measures/instruments; (8) appropriate statistical methods. Each item was scored 0 for ‘No’ and 1 for ‘Yes’. The total quality score ranged from 0 to 8 (see online supplementary table S1).
Data extraction
Two independent investigators extracted the following information from all eligible studies: first author, year of publication, study location, investigation period, gender composition, age, sample size, duration of intervention, proportion of drug-related criminal activities (including drug trafficking, drug selling, robbery and theft to maintain drug habit), employment rate and relationship with family among clients on MMT at baseline and follow-up of treatment.
Statistical analysis
Meta-analyses were carried out with the Comprehensive Meta-Analysis software (V2.0; Biostat, Englewood, New Jersey, USA). The effect rates of pooled estimates and 95% CIs were determined based on random-effects models. Heterogeneity tests were performed using the Cochran Q test (p<0.10 represents statistically significant heterogeneity) and I2 statistic. Potential publication bias was measured by the Begg and Mazumdar rank correlation (p<0.05 represents statistically significant publication bias).
Results
Trial flow/flow of included studies
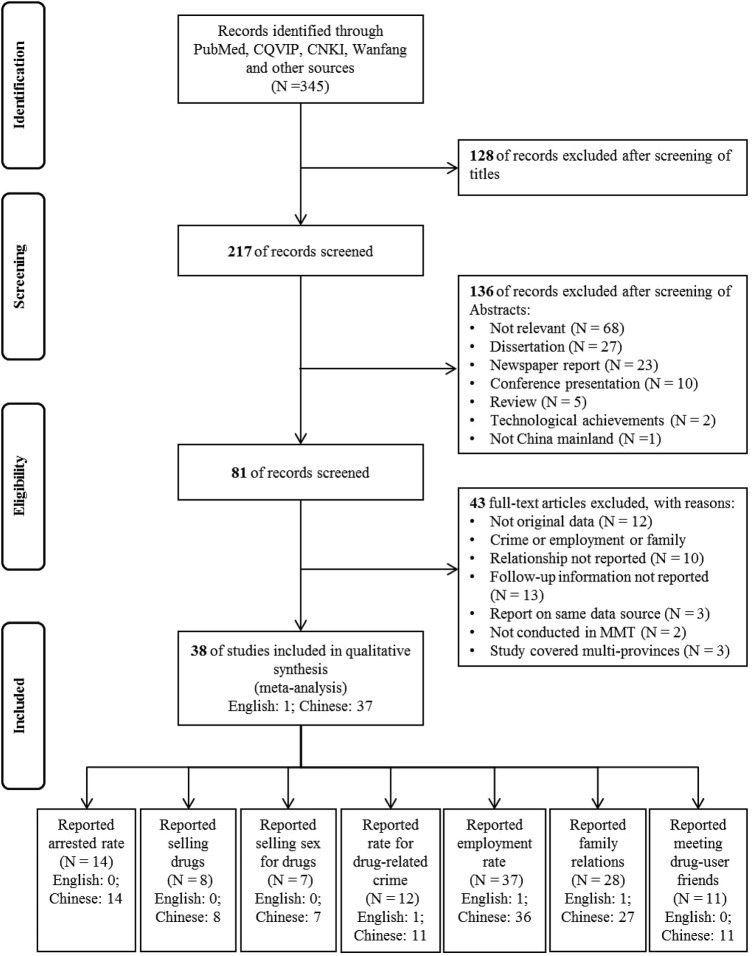
According to our initial search strategies, 345 articles were identified from four electronic databases. We excluded 128 irrelevant articles after title screening. The remaining 217 abstracts were screened by two independent investigators (H-MS, X-YL), and 136 articles were excluded. The remaining 81 articles were eligible for full-text screening; of these, 43 were excluded. A total of 38 articles were therefore eligible and included in this review (1 in English, 37 in Chinese). Twenty-two studies reported changes in criminal activities (14 reported rate of arrest, 8 reported sale of drugs , 7 reported selling sex for drugs, and 12 reported rate of drug-related crime), and 37 studies reported changes in relationships with family and friends (37 reported employment rate, 28 reported relationship with family and 11 reported relationship with friends) (figure 1).
Figure 1.
Flow chart for selection of studies. CNKI, China National Knowledge Infrastructure; CQVIP, Chongqing VIP Chinese Science and Technology Journals Database; MMT, methadone maintenance treatment.
Study characteristics
The sample size of MMT clients reported in the eligible studies ranged from 65 to 13 310 (median 320.5; IQR 120–651.5). A total of 30 239 participants were included in this review, and about 76.2% were male. The mean age of all MMT clients was 34.42 years (range 18–62 years). Of the 38 eligible articles, almost half of the studies (44.8%) were conducted in the provinces with high HIV prevalence (>20%),32 33 including Yunnan, Sichuan, Guangdong, Xinjiang, Guizhou and Guangxi. The follow-up period of MMT intervention ranged from 6 to 48 months, and the majority were followed-up within 12 months (86.8%). Twenty studies were prospective cohort studies, and the others were retrospective.
Criminal activities
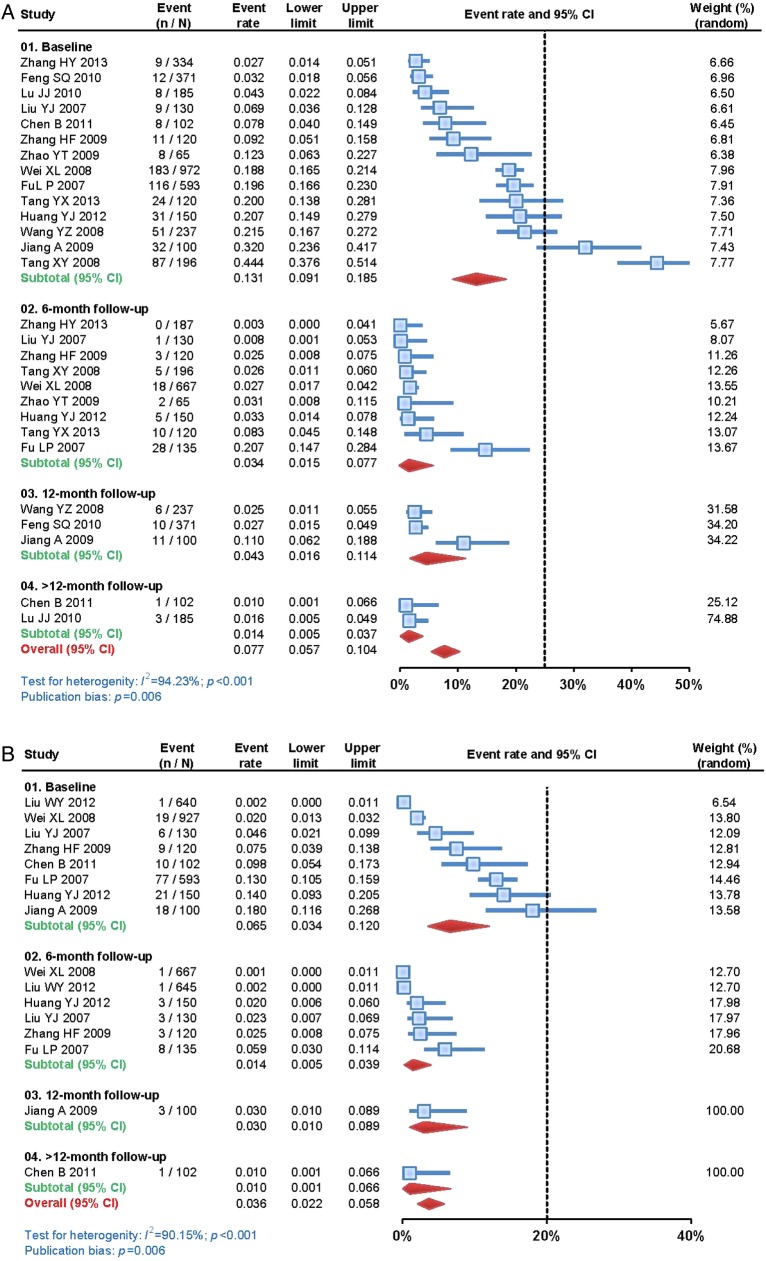
Criminal activity among MMT clients had significantly decreased after MMT intervention. The self-reported arrest rate decreased from 13.1% (95% CI 9.1% to 18.5%) at baseline (table 1 and figure 2A) to 3.4% (95% CI 1.5% to 7.7%), 4.3% (95% CI 1.6% to 11.4%) and 7.7% (95% CI 5.7% to 10.4%) at 6, 12 and 36 months follow-up. About 7.6% (95% CI 3.8% to 14.8%) of the clients had sold drugs before receiving the MMT intervention (table 1 and figure 2B). This rate had decreased to 1.9% (95% CI 0.6% to 6.2%) after 6 months, 3.0% (95% CI 1.0% to 8.9%) after 12 months and 1.0% (95% CI 0.1% to 6.6%) after 36 months. The proportion of clients selling sex for drugs decreased from 5.3% (2.4% to 11.1%) at baseline to 1.1% (0.5% to 2.3%) at 6 months and 0.8% (0.3% to 1.9%) at 12 months (table 1 and figure 2C). The rate of drug-related crime also decreased from 9.9% (6.8% to 14.2%) at baseline to 3.4% (2.5% to 4.5%) at 6 months and 3.4% (0.8% to 13.1%) at 12 months (table 1 and figure 2D). Ten studies reported that the rate of drug-related crime decreased from 1.1–30.34% to 0.5–3.7%. In addition, six studies reported that the rate of selling sex for drugs decreased from 1.9–24.0% to 0.5–1.5% after the MMT intervention.
Table 1.
Comparison of social functioning and family relations before and after initiation of MMT
| Baseline (admission to MMT) | Post-intervention period |
|||
|---|---|---|---|---|
| 6 months | 12 months | >12 months | ||
| Arrest rate | 13.1% (9.1% to 18.5%) | 3.4% (1.5% to 7.7%) | 4.3% (1.6% to 11.4%) | 7.7% (5.7% to 10.4%) |
| Proportion selling drugs | 6.5% (3.4% to 12.0%) | 1.4% (0.5% to 3.9%) | 3.0% (1.0% to 8.9%) | 1.0% (0.1% to 6.6%) |
| Proportion selling sex for drugs | 5.3% (2.4% to 11.1%) | 1.1% (0.5% to 2.3%) | 0.8% (0.3% to 1.9%) | 1.0% (0.1% to 6.6%) |
| Rate of drug-related crime | 9.9% (6.8% to 14.2%) | 3.4% (2.5% to 4.5%) | 3.4% (0.8% to 13.1%) | 3.3% (2.1% to 5.3%) |
| Employment rate | 26.1% (23.6% to 28.8%) | 47.3% (40.9% to 53.8%) | 54.7% (47.4% to 61.9%) | 45.5% (37.2% to 54.1%) |
| Proportion with good family relations | 39.7% (35.1% to 44.6%) | 63.3% (54.7% to 71.1%) | 72.1% (65.1% to 78.2%) | 83.2% (77.8% to 87.6%) |
| Proportion in daily contact with former drug-user friends | 25.3% (18.9% to 33.0%) | 4.0% (2.4% to 6.4%) | 7.7% (1.4% to 33.2%) | 1.0% (0.1% to 6.6%) |
MMT, methadone maintenance treatment.
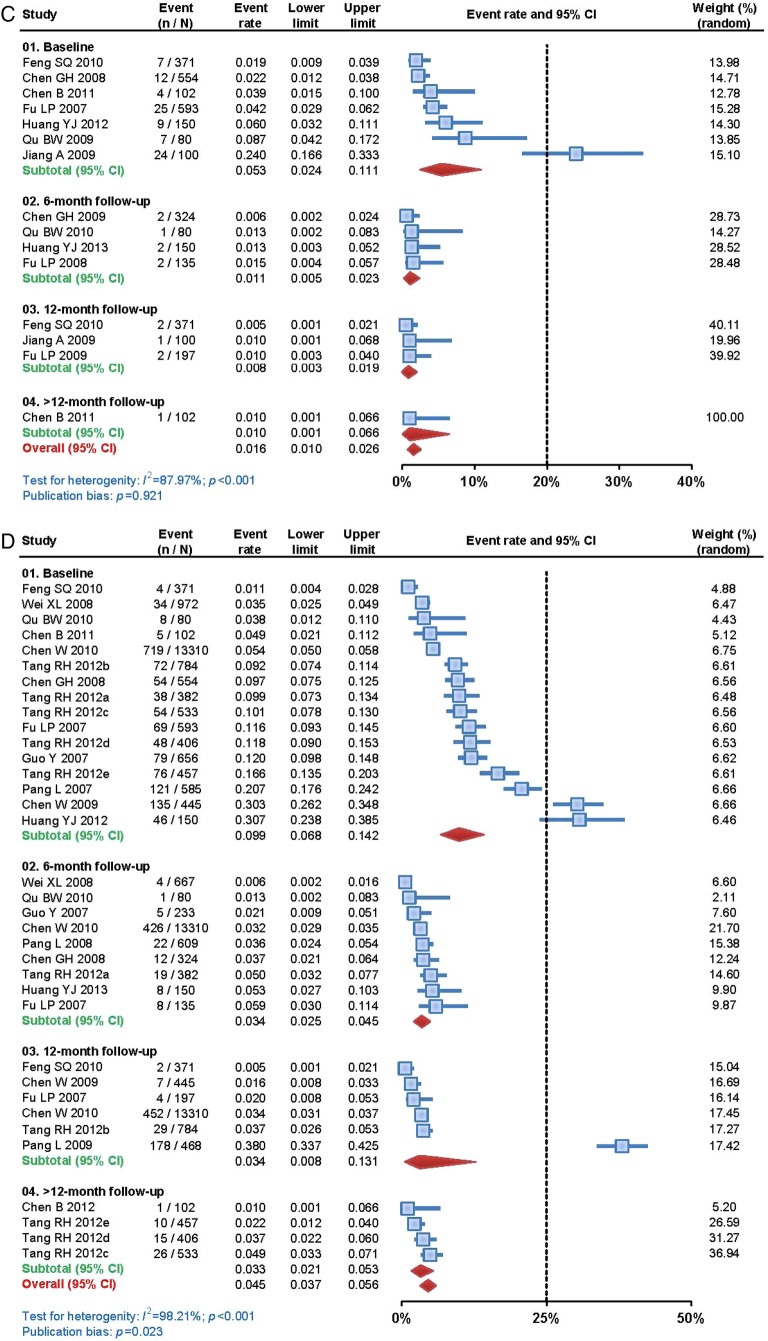
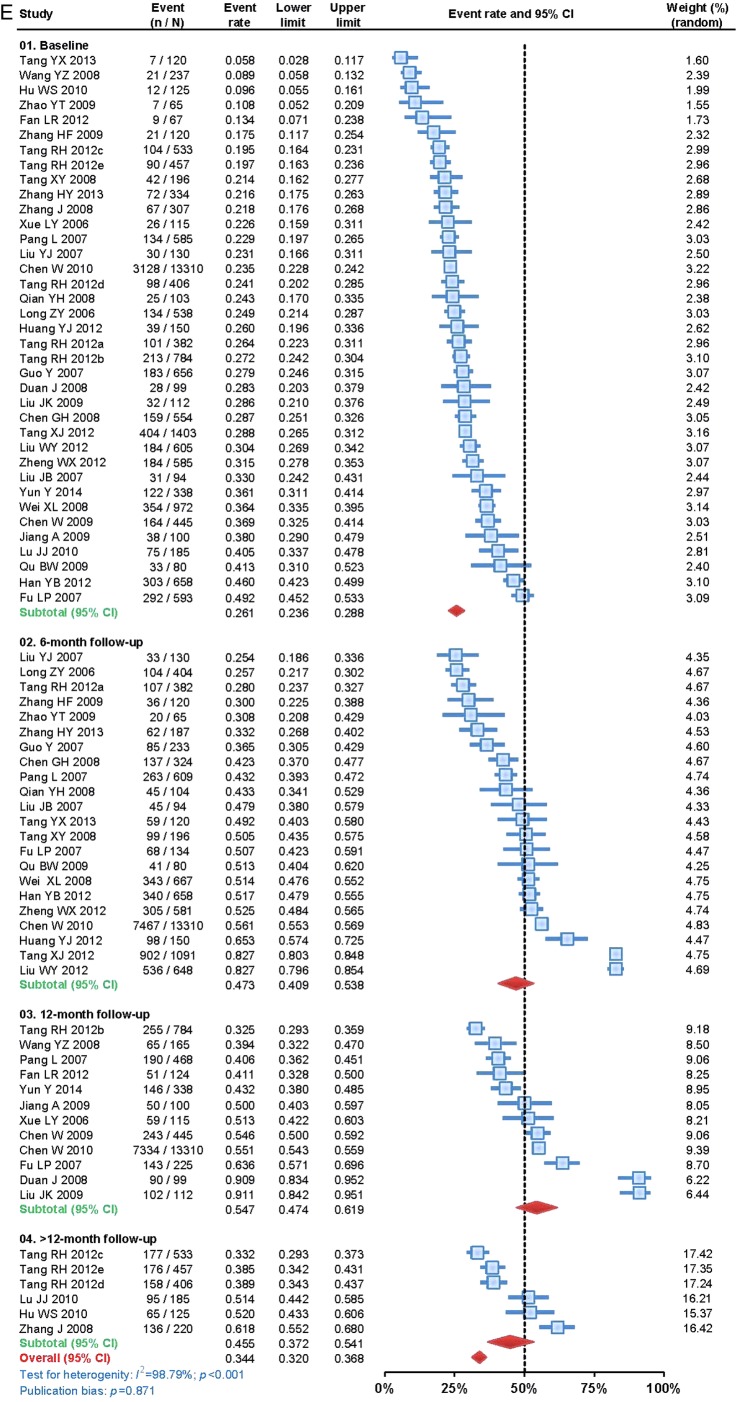
Figure 2.
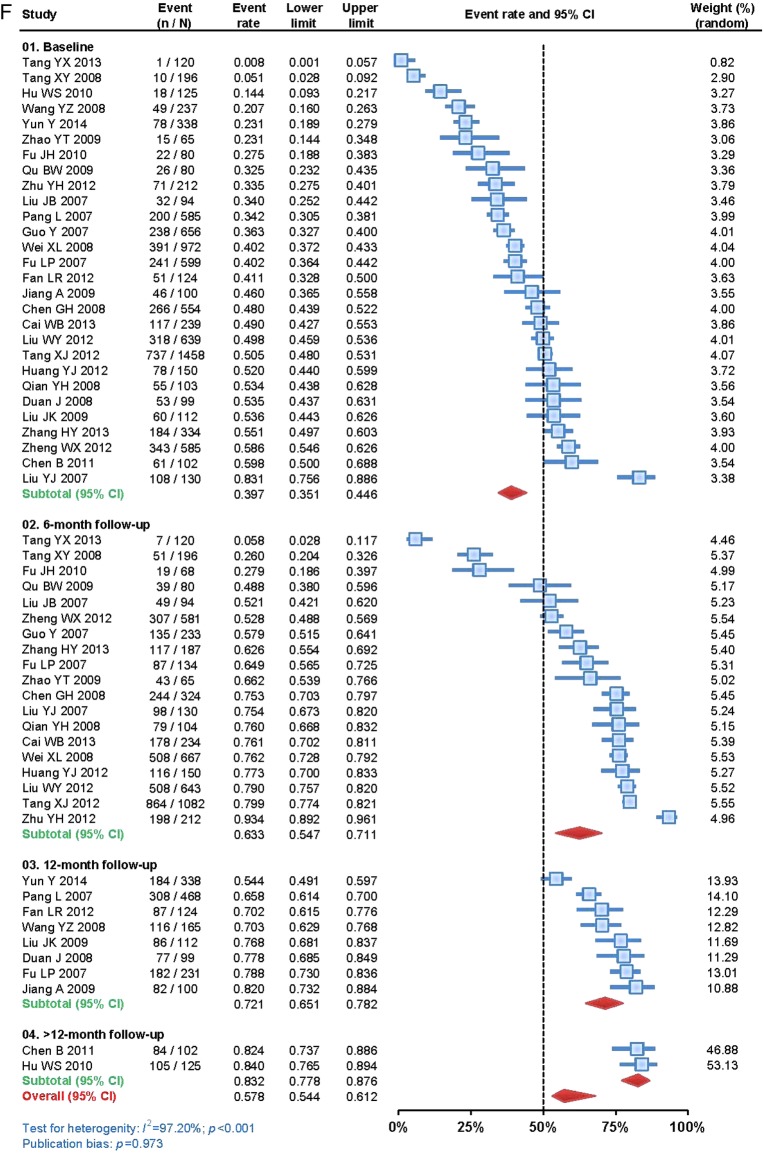
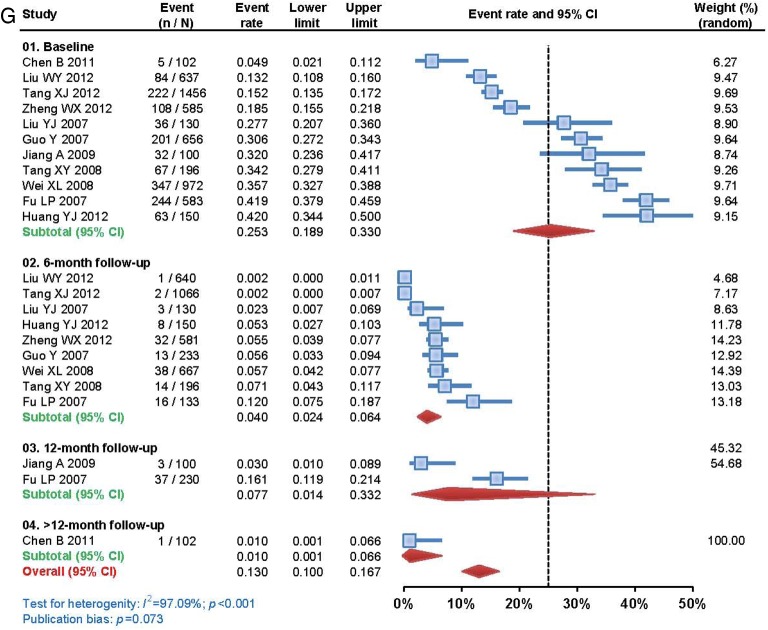
Changes in criminal activity, social well-being and family relations in Chinese clients at various intervention periods before and after initiation of methadone maintenance treatment (MMT): (A) rate of arrest by police; (B) rate of drug selling; (C) rate of selling sex for drugs; (D) rate of drug-related crime; (E) employment rate; (F) proportion having good relationship with family; (G) proportion having contact with former drug-user friends on a daily basis.
Figure 2.
Continued.
Figure 2.
Continued.
Figure 2.
Continued.
Figure 2.
Continued.
Social functioning
The rate of employment among clients improved after they had received MMT. The overall employment rate increased from 26.4% (95% CI 22.9% to 30.1%) at baseline (table 1 and figure 2E) to 41.6% (95% CI 36.6% to 48.0%) after 6 months of treatment, and further to 59.8% (95% CI 52.4% to 66.8%) after 12 months, but decreased slightly to 55.4% (95% CI 48.2% to 62.3%) after >12 months of treatment.
Family relations
Family relations among clients also improved after they had received MMT. In addition, only 37.9% (95% CI 32.0% to 44.2%) (table 1 and figure 2F) of drug users reported having a good relationship with their family before receiving MMT interventions; however, this rate increased significantly to 59.6% (95% CI 48.1% to 70.2%) after 6 months, 75.0% (95% CI 69.0% to 80.2%) after 12 months and 83.2% (95% CI 77.8% to 87.6%) after >12 months of treatment.
Contact with former drug-user friends
About 31.0% of clients (95% CI 25.7% to 36.8%) (table 1 and figure 2G) met their drug-user friends every day at baseline; however, the rate of daily contact with former drug-user friends decreased to 6.5% (95% CI 4.4% to 9.4%), 7.7% (95% CI 1.4% to 33.2%) and 1.0% (95% CI 0.1% to 6.6%) after 6, 12 and >12 months of intervention, respectively.
Quality assessment
All studies reported the study period, study location and sample size. All studies reached a total quality score of 3 or higher (out of a total of 8). The mean quality score was 3.97, indicating a reasonably good quality for our selected studies (see online supplementary table S1).
Discussion
To the best of our knowledge, this is the first study to review the effect of MMT on criminal activity, social functioning and family relations among MMT clients in China. Our findings indicate that MMT significantly decreased self-reported arrest rate, frequency of selling drugs, drug-related crime, selling sex for drugs, and likelihood of meeting former drug-user friends. In contrast, it improved employment rate and family relations. These findings are consistent with other international studies in England, Lithuania and Israel.34–37 In particular, a meta-analysis conducted by Marsch38 showed that 85% of drug users who received MMT decreased drug-related crime. A systematic review conducted by Holloway et al39 also showed that criminal behaviour was reduced in MMT clients compared with non-MMT drug users. Despite these positive results, policy makers who have strong moral reservations about MMT would emphasise the physically dependent nature of methadone and ongoing spending of public funds on a population deemed ‘socially evil’ in many settings.40 Further studies are necessary to evaluate other aspects of MMT, including structural barriers and cost-effectiveness of the programme, to help inform relevant policies in the future.
We have demonstrated improved employment rates and family relations among MMT clients in China. Consistently, a study conducted in the USA also indicated a significant improvement in employment outcomes with an integrated drug counselling and employment programme for MMT clients.41 In addition, a Swedish study showed that over 80% of people with severe heroin addiction obtained new jobs and were reintegrated into society after receiving MMT.42 In a separate study, Blix followed 345 heroin users for 24 years over the period 1966–1989 in Sweden; a 70–80% employment rate among MMT clients was reported.42 Interestingly, our meta-analysis indicated the best employment outcome at 12 months after treatment initiation, and the rate started to decline when treatment continued beyond 12 months. This finding is echoed by results of an early survey of the first eight pilot MMT clinics in China.43 A plausible explanation is that employed clients are more likely to drop out of the treatment programme, which leads to a declining employment rate among those who keep going with treatment. Further, family relations of clients improved during the course of MMT. With reduced symptoms of addiction, clients are able to resume family duties and re-establish relationships with other family members.44 45
Several limitations to this study should be noted. First, by the end of 2012, there were 756 MMT clinics in China, covering 28 Chinese provinces, but 13 provinces did not publish any reports on the related characteristics of social and familial relationships, and this limits our analysis in these regions. Second, only eight studies reported on clients who sold drugs, and this small number of studies may have resulted in information bias in our study. Third, owing to the small number of available studies, we pooled all study estimates beyond 12 months of follow-up in this analysis. Fourth, substantial heterogeneity existed between studies because of different study methodologies, method of recruitment and sampling sizes in different studies. Our meta-analyses could not take all of these variations across individual studies into account. Fifth, a limited number of studies reported relevant characteristics of social and familial relationships in recent years and the reports’ delay in publication may also have biased our findings.
Conclusions
The MMT programme in China has conclusively been shown to be effective in reducing criminal activity and improving employment outcome and social well-being of its clients. The MMT programme should not only focus on reducing drug misuse, but other advisory and intervention services, such as Voluntary Counselling and Testing of HIV, psychological therapy, and family intervention, should also be integrated into the programme.46 47 In parallel, clients should be encouraged to make use of rehabilitation facilities to improve their own awareness in order to safeguard their rights and interests. MMT may serve as a valuable opportunity to reduce drug-related harm among drug users and enable them to return to society as healthy and productive individuals.
Supplementary Material
Acknowledgments
The authors thank all the study participants and staff. Additional thanks go to Yan-xian Liang and Ya-fei Wang (Department of Epidemiology and Health Statistic, School of Public Health, Nantong University) for data analysis.
Footnotes
Contributors: EPFC, LZ and XZ designed the study. H-MS and X-YL performed the data collection and provided the first draft of the manuscript. TL, YX, Y-HL and TT performed data analysis. LZ and EPFC assisted with data interpretation. EPFC, LZ and XZ provided critical revision for important intellectual content. All authors read and approved the final version of the manuscript.
Funding: This work was supported by grants from Round 8 of the Australian Leadership Awards (ALA) Fellowships Program and Overseas Scholarship of Jiangsu Government, China and the National Natural Science Foundation of China (81373060).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Zhuang X, Liang Y, Chow EP et al. HIV and HCV prevalence among entrants to maintenance treatment clinics in China: a systematic review and meta-analysis. BMC Infect Dis 2012;12:130 10.1186/1471-2334-12-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhuang X, Wang Y, Chow EP et al. Risk factors associated with HIV/HCV infection among entrants in methadone maintenance treatment clinics in China: A systematic review and meta-analysis. Drug Alcohol Depend 2012;126:286–95. 10.1016/j.drugalcdep.2012.05.028 [DOI] [PubMed] [Google Scholar]
- 3.Kulsudjarit K. Drug problem in southeast and southwest Asia. Ann N Y Acad Sci 2004;1025:446–57. 10.1196/annals.1316.055 [DOI] [PubMed] [Google Scholar]
- 4.Qian HZ, Schumacher JE, Chen HT et al. Injection drug use and HIV/AIDS in China: review of current situation, prevention and policy implications. Harm Reduct J 2006;3:4 10.1186/1477-7517-3-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ball AL, Rana S, Dehne KL. HIV prevention among injecting drug users: responses in developing and transitional countries. Public Health Rep 1998;113:S170–S81. [PMC free article] [PubMed] [Google Scholar]
- 6.Stimson GV. Has the United Kingdom averted an epidemic of HIV-1 among drug injectors? Addiction 1996;91:1085–9. 10.1046/j.1360-0443.1996.91810892.x [DOI] [PubMed] [Google Scholar]
- 7.Ttrathdee SA, Vlahov D. The effectiveness of needle exchange programs: a review of the science and policy. AIDScience 2001;1:1–31. [Google Scholar]
- 8.Dole VP, Nyswander M. A medical treatment for diacetylmorphine (heroin) addiction. JAMA 1965;193:646 10.1001/jama.1965.03090080008002 [DOI] [PubMed] [Google Scholar]
- 9.Isbell H, Vogel VH. The addiction liability of methadon (amidone,dolophine,10820) and its use in the treatment of the morphine abstinence syndrome. Am J of psychiatry 1949;105:909 10.1176/ajp.105.12.909 [DOI] [PubMed] [Google Scholar]
- 10.Parrino MW. State methadone treatment guidelines. US Department of Health and Human Services, Public Health Service, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment 1993.
- 11.Gambashidze N, Sikharulidze Z, Piralishvili G et al. Evaluation of pilot methadone maintenance therapy in Georgia (Caucasus). Georgian Med News 2008;160:25–30. [PubMed] [Google Scholar]
- 12.Tran BX, Ohinmaa A, Duong AT et al. Changes in drug use are associated with health-related quality of life improvements among methadone maintenance patients with HIV/AIDS. Qual Life Res 2012;21:613–23. 10.1007/s11136-011-9963-y [DOI] [PubMed] [Google Scholar]
- 13.Ball JC, Ross A. The effectiveness of methadone maintenance treatment: patients, programs, services, and outcome. New York: Springer-Verlag Publishing, 1991. [Google Scholar]
- 14.Dole VP, Joseph H. Long-term outcome of patients treated with methadone maintenance. Ann N Y Acad Sci 1978;311: 181–96. 10.1111/j.1749-6632.1978.tb16775.x [DOI] [PubMed] [Google Scholar]
- 15.Gearing FR, Schweitzer MD. An epidemiologic evaluation of long-term methadone maintenance treatment for heroin addiction. Am J Epidemiol 1974;100:101. [DOI] [PubMed] [Google Scholar]
- 16.Appel PW, Joseph H, Kott A et al. Selected in-treatment outcomes of long-term methadone maintenance treatment patients in New York State. Mt Sinai J Med 2001;68:55–61. [PubMed] [Google Scholar]
- 17.Bertschy G. Methadone maintenance treatment: an update. Eur Arch Psychiatry Clin Neurosci 1995;245:114–24. 10.1007/BF02190738 [DOI] [PubMed] [Google Scholar]
- 18.Fiellin DA, O'Connor PG, Chawarski M et al. Methadone maintenance in primary care: a randomized controlled trial. JAMA 2001;286:1724–31. 10.1001/jama.286.14.1724 [DOI] [PubMed] [Google Scholar]
- 19.Hartel DM, Schoenbaum EE. Methadone treatment protects against HIV infection: two decades of experience in the Bronx, New York City. Public Health Reports 1998;113:107–15. [PMC free article] [PubMed] [Google Scholar]
- 20.Hubbard RL, Craddock SG, Flynn PM et al. Overview of 1-year follow-up outcomes in the drug abuse treatment outcome study (DATOS). Psychol Addict Behav 1997;11:261–78. 10.1037/0893-164X.11.4.261 [DOI] [Google Scholar]
- 21.Joseph H, Woods J. A point in time: the impact of expanded methadone maintenance treatment on citywide crime and public health in New York City 1971–1973. Arch public health 1995;53:215–31. [Google Scholar]
- 22.Joseph H, Stancliff S, Langrod J. Methadone maintenance treatment (MMT): a review of historical and clinical issues. Mt Sinai J Med 2000;67:347–64. [PubMed] [Google Scholar]
- 23.Michels II, Stover H, Gerlach R. Substitution treatment for opioid addicts in Germany. Harm Reduct J 2007;4:5 10.1186/1477-7517-4-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pang L, Hao Y, Mi GD et al. Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS 2007;21:S103–7. 10.1097/01.aids.0000304704.71917.64 [DOI] [PubMed] [Google Scholar]
- 25.Ward J, Hall W, Mattick RP. Role of maintenance treatment in opioid dependence. Lancet 1999;353:221–6. 10.1016/S0140-6736(98)05356-2 [DOI] [PubMed] [Google Scholar]
- 26.Wu Z. Landmark government methadone maintenance program in mainland China. 15th International AIDS Conference; 2004. [Google Scholar]
- 27.Wu Z. Methadone maintenance program in mainland China: from pilot to scale-up. International Conference on the Reduction of Drug Related Harm; 20–24 2005. [Google Scholar]
- 28.Musa R, Bakar AZA, Khan UA. Two-year outcomes of methadone maintenance therapy at a clinic in Malaysia. Asia Pac J Public Health 2012;24:826–32. 10.1177/1010539511404396 [DOI] [PubMed] [Google Scholar]
- 29.Keen J, Rowse G, Mathers N et al. Can methadone maintenance for heroin-dependent patients retained in general practice reduce criminal conviction rates and time spent in prison? Br J Gen Pract 2000;50:48. [PMC free article] [PubMed] [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boyle MH. Guidelines for evaluating prevalence studies. Evid Based Met Health 1998;1:37–9. 10.1136/ebmh.1.2.37 [DOI] [Google Scholar]
- 32.Guo W, Qu SQ, Ding ZW et al. Situations and trends of HIV and syphilis infections among drug users in China, 1995–2009. Chin J Epidemiol 2010;31:666–9. [PubMed] [Google Scholar]
- 33.Jia MH, Luo HB, Ma YL et al. The HIV epidemic in Yunnan province, China, 1989–2007. J Acqui Immune Defic Syndr 2010;53:S34–40. 10.1097/QAI.0b013e3181c7d6ff [DOI] [PubMed] [Google Scholar]
- 34.Connock M, Juarez-Garcia A, Jowett S et al. Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation: Gray on behalf of the National Coordinating Centre for Health Technology Assessment. Health Technol Assess 2007;11:1–171, iii–iv. [DOI] [PubMed] [Google Scholar]
- 35.Mutasa H. Risk factors associated with noncompliance with methadone substitution therapy (MST) and relapse among chronic opiate users in an Outer London community. J Adv Nurs 2001;35:97–107. 10.1046/j.1365-2648.2001.01826.x [DOI] [PubMed] [Google Scholar]
- 36.Padaiga Z, Subata E, Vanagas G. Outpatient methadone maintenance treatment program. Quality of life and health of opioid-dependent persons in Lithuania. Medicina (Ka-unas) 2007;43:235–41. [PubMed] [Google Scholar]
- 37.Ponizovsky AM, Grinshpoon A. Quality of life among heroin users on buprenorphine versus methadone maintenance. Am J Drug Alcohol Abuse 2007;33:631–42. 10.1080/00952990701523698 [DOI] [PubMed] [Google Scholar]
- 38.Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: a meta-analysis. Addiction 1998;93:515–32. 10.1046/j.1360-0443.1998.9345157.x [DOI] [PubMed] [Google Scholar]
- 39.Holloway KR, Bennett TH, Farrington DP. The effectiveness of drug treatment programs in reducing criminal behavior: a meta-analysis. Psicothema 2006;18:620–9. [PubMed] [Google Scholar]
- 40.Shi J, Zhao LY, Epstein DH et al. The effect of methadone maintenance on illicit opioid use, human immunodeficiency virus and hepatitis C virus infection, health status, employment, and criminal activity among heroin abusers during 6 months of treatment in China. J Addict Med 2007;1:186 10.1097/ADM.0b013e318156cc19 [DOI] [PubMed] [Google Scholar]
- 41.Coviello DM, Zanis DA, Wesnoski SA et al. An integrated drug counseling and employment intervention for methadone clients. J Psychoactive Drugs 2009;41:189–97. 10.1080/02791072.2009.10399912 [DOI] [PubMed] [Google Scholar]
- 42.Blix O. Methadone maintenance programs in Sweden. JAMA 1989;261:2202 10.1001/jama.1989.03420150052034 [DOI] [PubMed] [Google Scholar]
- 43.Pang L, Mi GD, Wang CH et al. Evaluation of first 8 pilot methadone maintenance treatment clinics in China. Chin J Exp Clin Virol 2007;21:2–4. [PubMed] [Google Scholar]
- 44.Chen B, Zhou BQ, Zhang HY et al. Effective Evaluation of Methadone Maintenance Treatment Among Drug Users in Zhuhai. Pract Prev Med 2011;18:364–5. [Google Scholar]
- 45.Chen GH, Yang HT, Qian XC et al. Effectiveness evaluation of six month community-based methadone treatment in Jiangsu Province. Chin J AIDS STD 2008;14:590–3. [Google Scholar]
- 46.Judd LL, Marston MG, Attkisson C et al. Effective medical treatment of opiate addiction. National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. JAMA 1998;280:1936–43. 10.1001/jama.280.22.1936 [DOI] [PubMed] [Google Scholar]
- 47.Magura S, Nwakeze PC, Demsky SY. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction 1998;93:51–60. 10.1046/j.1360-0443.1998.931516.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.