Abstract
Alcohol and tobacco abuse are the main risk factors for esophageal squamous cell carcinoma (ESCC), but other conditions that induce chronic irritation of the esophageal mucosa have also been attributed to it. For example, long-standing achalasia increases 16 times the risk of developing ESCC. We report the case of a patient with long-standing achalasia who developed ESCC. Although this complication is infrequent, it should be remembered by clinicians who treat patients with achalasia to detect early stages cancer.
Background
Achalasia is relatively a rare condition with an annual incidence rate from 0.5 to 1.2 per 100 000.1 This condition is a motility disorder of the esophagus, of unknown aetiology, which results in degeneration of the myenteric nerve plexus of the esophageal wall. The characteristics of achalasia include loss of esophageal peristalsis and failure of relaxation of the lower esophageal sphincter, particularly during swallowing.2 Although achalasia is a relatively rare condition, it carries a risk of complications, including mega-esophagus,3 aspiration pneumonia4 and esophageal cancer.5
Alcohol and tobacco use are the main risks factors for esophageal squamous cell carcinoma (ESCC), but other conditions that induce chronic irritation of the esophageal mucosa have also been associated, such as nutritional deficiencies, infectious agents (ie, papillomavirus), radiation therapy (RT) and achalasia.6 Long-standing achalasia increases 16 times the risk for develop ESCC.
Case presentation
A 60-year-old man was referred to our unit for evaluation of 6 months of progressive dysphagia. He had been diagnosed with achalasia 20 years prior and, at that time, three endoscopic dilation sessions were performed and he was discharged without any follow-up protocol. He remained asymptomatic for 16 years, but in the past 4 years he experienced mild dysphagia with solids but no other alarm signs such as anaemia or weight loss. In the past 6 months, the patient's dysphagia had worsened with weight loss of 5 kg.
Investigations
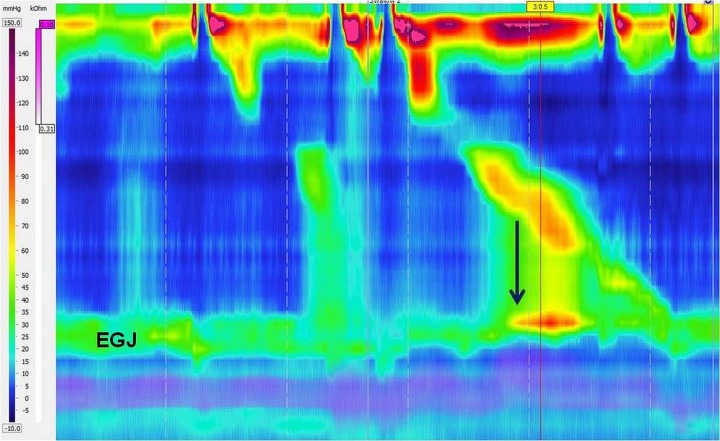
A barium esophagogram showed the pathognomonic ‘bird's beak’ appearance of the distal esophagus with dilation of the esophagus proximally, and high-resolution esophageal manometry showed impaired esophagogastric junction (EGJ) relaxation with segmental pressurisation between the peristaltic contraction and the EGJ, suggesting EGJ outflow obstruction according to the Chicago classification (figure 1). Oral endoscopy was performed showing an esophagus with abundant fluid and food debris. After profuse aspiration, a sigmoid aspect of the esophagus was found and at 30 cm from dental arch, an irregular and nodular lesion was found (figure 2). Mucosal biopsies were taken and, histologically, a moderately differentiated squamous cell carcinoma was reported (figure 2). A chest CT scan was performed showing a dilated esophagus with contrast medium remaining in the distal part and, underneath, an important thickening of its wall conditioning a distal stenosis (figure 3). According to the TNM classification the patient was at stage IIIA.
Figure 1.
A representative esophageal high-resolution manometry plot of a wet swallow showing impaired esophagogastric junction (EGJ) relaxation with segmental pressurisation (black arrow) between the peristaltic contraction and the EGJ, suggesting EGJ outflow obstruction.
Figure 2.
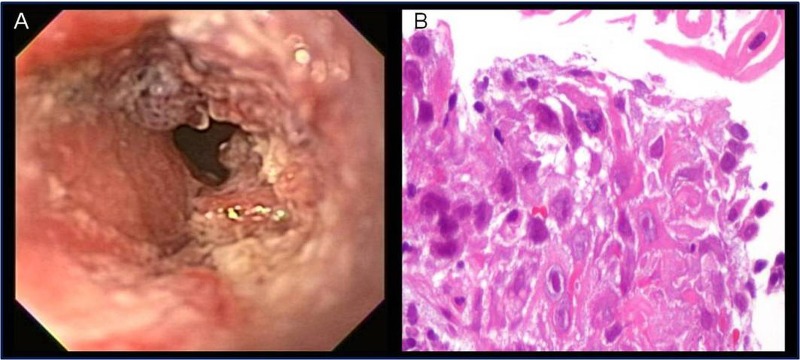
Endoscopic (A) and histological (B) appearance of esophageal squamous cell carcinoma.
Figure 3.
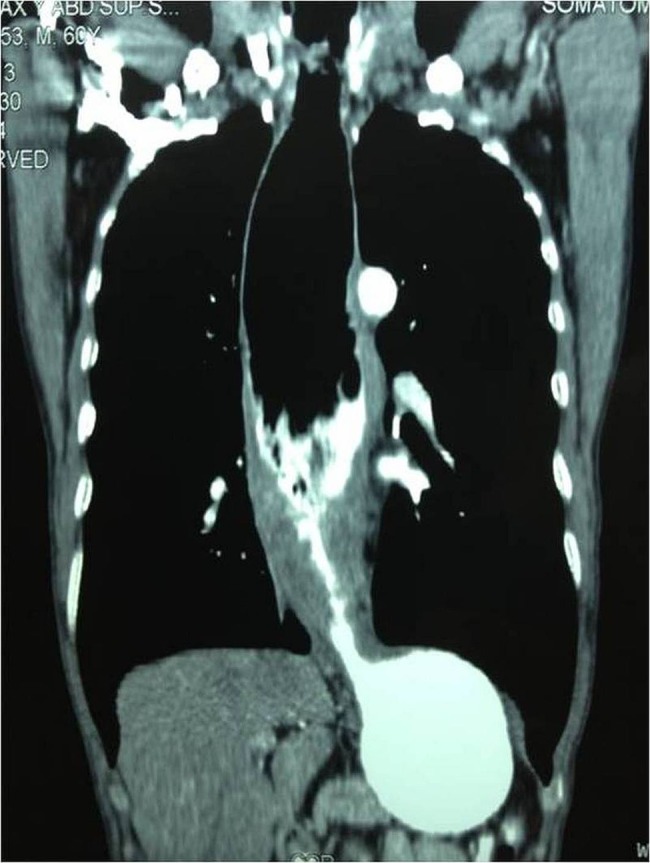
CT scan showing a dilated esophagus with contrast medium remaining in the distal part and, underneath, an important thickening of its wall conditioning a distal stenosis.
Differential diagnosis
Late-stage achalasia, esophageal adenocarcinoma or peptic stricture.
Treatment
The patient was eligible for chemoradiation with cisplatin/5FU and external RT doses of 45–50.4 Gy in 25–28 fractions.
Outcome and follow-up
The patient is in his third month of chemoradiation and his performance status is better with significant improvement of symptoms.
Discussion
Esophageal cancer is an infrequent complication of achalasia. Among a large case series it ranges from 0.4% to 9.2%.1 6–8 One review found that the prevalence of esophageal cancer in achalasia was 3%, corresponding to a 50-fold increased risk,5 while a prior review reported increased risks ranging from 0-fold to 33-fold greater than the general population.9 Most cases of esophageal cancer in patients with achalasia correspond to ESSC; however, there have been cases of adenocarcinoma associated with Barrett’s esophagus.
The theory explaining the development of ESCC in patients with achalasia is that the food stasis promotes acid lactic production and fermentation, which stays in the distal portion of the esophagus, causing slow and continuous damage to the esophageal mucosa. The risk is increased in achalasia of more than 15 years of evolution.10 Tumours usually arise in a widely dilated esophagus and, when detected, are large and at an advanced stage.11
The development of Barrett’s esophagus and adenocarcinoma in patients with achalasia has been described in patients who have undergone myotomy and esophageal dilations. This phenomenon is due to constant exposure of the esophagus to acid reflux.12 A recent study found that 8.2% of 331 patients with achalasia developed Barrett's esophagus over a period of up to 25 years.13
Esophageal malignancies should be suspected in a previously treated patient with achalasia with symptomatic recurrence after a long asymptomatic period, as in our case. Although a regular surveillance programme for esophageal cancer as standard practice in patients with achalasia is controversial, awareness of this association should be inculcated in clinicians who treat patients with achalasia to detect early stages of cancer.
We believe that our report is relevant because, in a patient with long-standing achalasia, although it is logical to consider disease recurrence, clinicians should not miss the possibility of ESCC.
Learning points.
Long-standing achalasia has been described as a risk factor for esophageal squamous cell carcinoma, with a risk 16 times higher than in the general population.
Esophageal malignancies should be suspected in a previously treated patient with achalasia with symptomatic recurrence after a long-standing asymptomatic period.
There is a need for an endoscopic screening programme in patients with achalasia to detect the development of esophageal cancer.
Footnotes
Twitter: Follow Arturo Meixueiro-Daza at @mexpera
Contributors: SR-G and JMR-T contributed to the outlining of the study, generation, collection, assembly, analysis and interpretation of the data, and writing and revision of the manuscript. AM-D contributed to the generation, collection, assembly of the data and revision of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.O'Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 2013;19:5806–12. 10.3748/wjg.v19.i35.5806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pohl D, Tutuian R. Achalasia: an overview of diagnosis and treatment. J Gastrointestin Liver Dis 2007;16:297–303. [PubMed] [Google Scholar]
- 3.Eckardt AJ, Eckardt VF. Current clinical approach to achalasia. World J Gastroenterol 2009;15:3969–75. 10.3748/wjg.15.3969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akritidis N, Gousis C, Dimos G et al. Fever, cough, and bilateral lung infiltrates. Achalasia associated with aspiration pneumonia. Chest 2003;123:608–12. 10.1378/chest.123.2.608 [DOI] [PubMed] [Google Scholar]
- 5.Dunaway PM, Wong RK. Risk and surveillance intervals for squamous cell carcinoma in achalasia. Gastrointest Endosc Clin N Am 2001;11:425–34. [PubMed] [Google Scholar]
- 6.Ribeiro U Jr, Posner MC, Safatle-Ribeiro AV et al. Risk factors for squamous cell carcinoma of the oesophagus. Br J Surg 1996;83:1174–85. 10.1002/bjs.1800830905 [DOI] [PubMed] [Google Scholar]
- 7.Zendehdel K, Nyren O, Edberg A et al. Risk of oesophageal adenocarcinoma in achalasia patients, a retrospective cohort study in Sweden. Am J Gastroenterol 2007;102:1–5. 10.1111/j.1572-0241.2007.01057.x [DOI] [PubMed] [Google Scholar]
- 8.Brücher BL, Stein HJ, Bartels H et al. Achalasia and esophageal cancer: incidence, prevalence, and prognosis. World J Surg 2001;25:745–9. 10.1007/s00268-001-0026-3 [DOI] [PubMed] [Google Scholar]
- 9.Streitz JM, Ellis FH, Gibb SP et al. Achalasia and squamous cell carcinoma of the esophagus: analysis of 241 patients. Ann Thorac Surg 1995;59:1604–9. 10.1016/0003-4975(94)00997-L [DOI] [PubMed] [Google Scholar]
- 10.Eckardt VF, Hoischen T, Bernhard G. Life expectancy, complications, and causes of death in patients with achalasia: results of a 33-year follow-up investigation. Eur J Gastroenterol Hepatol 2008;20:956–60. 10.1097/MEG.0b013e3282fbf5e5 [DOI] [PubMed] [Google Scholar]
- 11.Galeiras RM, Rascado P, Lorenzo MJ et al. Bronchopneumonia caused by a perforation in an achalasic esophagus with a focal squamous cell carcinoma. Rev Esp Enferm Dig 2009;101:439–51. 10.4321/S1130-01082009000600014 [DOI] [PubMed] [Google Scholar]
- 12.Stein HJ, Siewert JR. Barrett's esophagus: pathogenesis, epidemiology, functional abnormalities, malignant degeneration, and surgical management. Dysphagia 1993;8:276–88. 10.1007/BF01354551 [DOI] [PubMed] [Google Scholar]
- 13.Leeuwenburgh I, Scholten P, Caljé TJ et al. Barrett's esophagus and esophageal adenocarcinoma are common after treatment for achalasia. Dig Dis Sci 2013;58:244–52. 10.1007/s10620-012-2157-9 [DOI] [PubMed] [Google Scholar]