Abstract
An 18-year-old man diagnosed with attention-deficit hyperactivity disorder was recently started on quetiapine in addition to regular methylphenidate, which he had been taking for a number of years. He presented with chest pain and inferolateral ST elevation, and underwent urgent coronary angiography, which showed normal coronary arteries. The initial troponin level was raised and an inpatient echocardiogram showed mild left ventricular systolic dysfunction with no evidence of regional wall motion abnormality. Cardiac MRI showed subepicardial late gadolinium enhancement, which was suggestive of myocarditis. Quetiapine and methylphenidate were discontinued and the patient was discharged home after 1 week. He was followed up within 8 weeks with complete recovery and no symptoms.
Background
Drug-induced myocarditis is a rare, yet potentially fatal complication that can occur following the administration of a number of pharmacological agents. Atypical antipsychotics have an improved tolerability profile with absence of extrapyramidal side effects and are increasingly prescribed to manage not only psychiatric conditions, but also to act as mood stabilisers, particularly in younger patients.
Although there is an awareness of the benign cardiac side effects such as hypertension and tachycardia that are seen during treatment initiation, these effects are often transient and subside without causing the patient any harm. However, the true incidence of the potential cardiotoxicity associated with these agents is unknown.
Due to the highly variable clinical presentation of drug-induced myocarditis, diagnosis is often delayed, resulting in irreversible damage to the myocardial muscle and leading to a poor prognosis for the patient. Our case highlights the fact that there is a clinical need for increased awareness of the cardiotoxic side effects associated with the newer generation antipsychotic agents and makes apparent the need for more formalised cardiovascular monitoring for patients initiated on antipsychotic therapy.
Case presentation
We present the case of an 18-year-old man known to have attention-deficit hyperactivity disorder (ADHD) for which he was taking long-term methylphenidate. Three weeks prior to his admission, the patient was started on quetiapine for comorbid ADHD with underlying bipolar affective disorder.
The patient presented with a severe central crushing chest pain that lasted for an hour, associated with nausea and vomiting. An initial ECG showed inferolateral ST elevation with reciprocal ST depression; he was transferred to our centre for primary percutaneous coronary intervention (figure 1).
Figure 1.
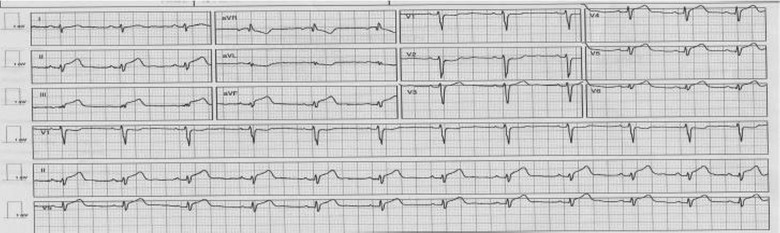
ECG showing inferolateral ST elevation of lead II, III and aVF, as well as V5 and V6 with reciprocal ST depression in V1 and V2. There was poor R wave progression and low voltage in limb leads.
Investigations
After loading with prasugrel and aspirin, the patient underwent an urgent coronary angiography, which showed unobstructed coronary arteries with Thrombolysis In Myocardial Infarction (TIMI) flow 3 in all three epicardial vessels. There was no evidence of aortic dissection. The patient denied the use of any illicit drugs or excessive alcohol intake.
On admission, blood investigations showed a rise in high-sensitive troponin I (hsTnI) of 13 175 ng/L, creatinine phosphokinase (CPK) of 1060 IU/L and total cholesterol of 4.4 mmol/L. The patient had a thrombophilia screen, which was negative with mildly raised protein C of 150 IU/mL.
An echocardiogram showed mild impairment of the left ventricular systolic function, with no evidence of regional wall motion abnormality (figures 2 and 3).
Figure 2.
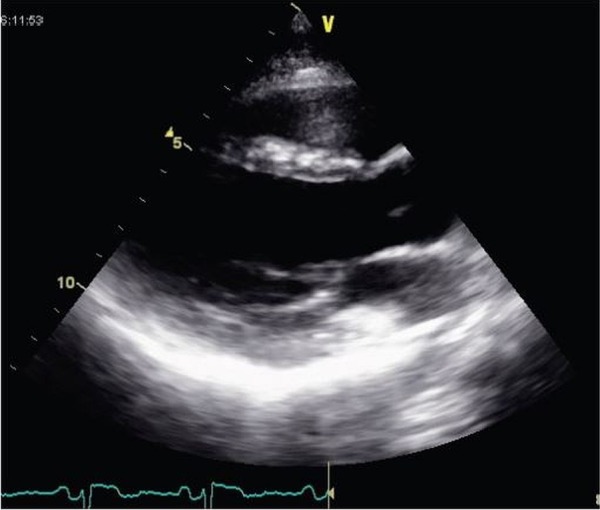
Echocardiography parasternal long-axis view showing no evidence of pericardial effusion.
Figure 3.
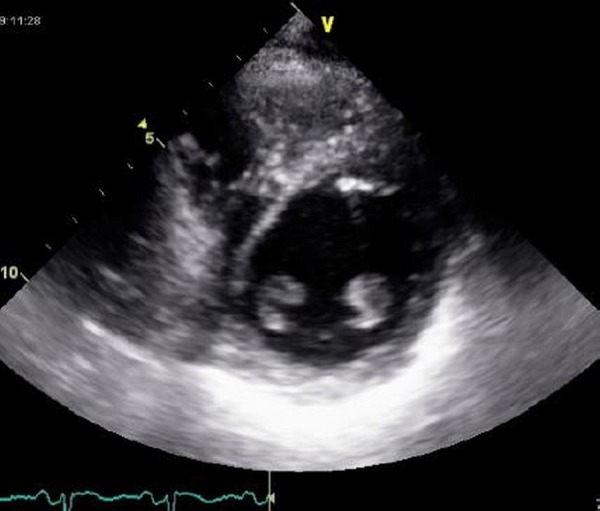
Echocardiography parasternal short-axis view showing good left ventricular function.
On the second day of admission, the patient's hsTnI levels had fallen to 5399 ng/L and he was pain free.
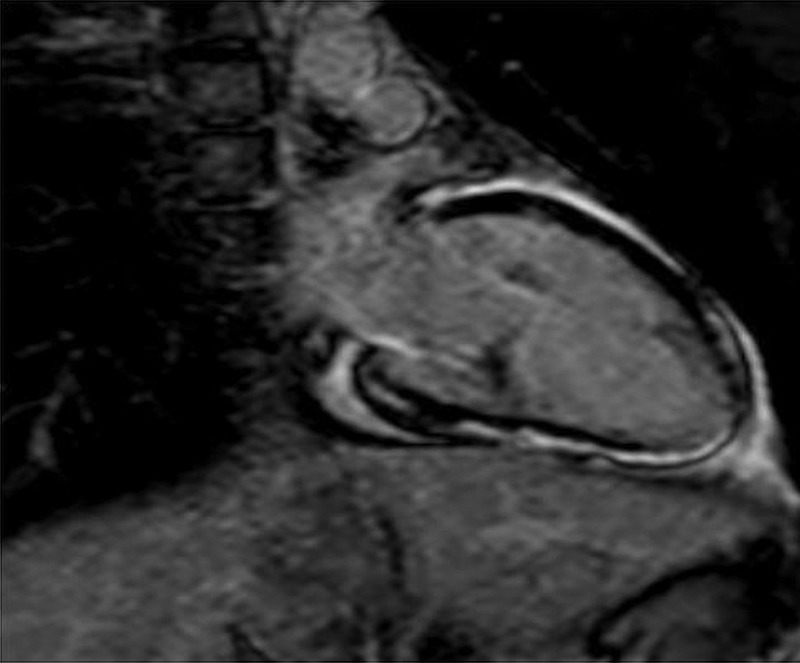
An inpatient cardiac MRI (CMR) showed mild left ventricular systolic impairment, with an estimated ejection fraction of 45%. Subepicardial late gadolinium enhancement was seen on the inferior wall, lateral wall and the apex, which was suggestive of myocarditis. There was no evidence of subendothelial gadolinium enhancement that would suggest ischaemic origin (figures 4 and 5).
Figure 4.

Cardiac MRI short-axis view showing subepicardial late gadolinium enhancement of the lateral and inferior walls, which is suggestive of myocarditis rather than coronary artery disease.
Figure 5.
Cardiac MRI vertical long-axis view showing subepicardial late gadolinium enhancement of the inferior wall and the left ventricular apex, which is suggestive of myocarditis.
Differential diagnosis
Acute ST elevation myocardial infarction
Coronary embolisation
Coronary spasm
Aortic or coronary dissection
Myocarditis
Treatment
Following the results of the investigations and a final diagnosis of myocarditis, the patient was initiated on a small dose of ramipril; methylphenidate and quetiapine were discontinued, with a referral to his psychiatric team to review the management options for his ADHD.
Outcome and follow-up
The patient was discharged home on citalopram, melatonin and ramipril with directions to his general practitioner (GP) to optimise dosing according to tolerability. Methylphenidate and quetiapine were discontinued and despite having not received any alternative psychostimulant or mood stabiliser the patient was stable in terms of his symptoms.
He was evaluated by the haematologist for the mildly raised protein C seen on admission, but this was considered non-significant.
Discussion
Myocarditis refers to an acute inflammatory process which involves the myocardium and occurs secondary to cardiac injury/insult. In terms of aetiology, a number of factors are known to contribute to this inflammatory process, including autoimmune disorders, viruses as well as the administration of several medications, for example, sulfonamides, lithium, anticonvulsants and antipsychotic agents.1–4
The association between psychiatric conditions and the accompanying increase in cardiovascular morbidity and mortality has long been recognised; however, the nature of the link between the two disease states is yet to be fully elucidated. In addition to this non-specific link, awareness exists of the increased incidence of adverse cardiac events in patients who are treated with antipsychotic medications. These range from sinus tachycardia and hypertension, which may be observed at the initiation of treatment and are often viewed as benign side effects that are transient in nature, to the more fatal instances of sudden cardiac death secondary to ventricular arrhythmias.5
Methylphenidate, a central nervous system stimulant, is indicated for the treatment of ADHD, a neurobehavioural condition that is predominantly diagnosed in children and adolescents. Cardiac adverse effects such as cardiomyopathy and pericarditis, although rare, are known to occur after treatment with methylphenidate.6
The principal mechanism of action of methylphenidate is to block the re-uptake of dopamine and norepinephrine, resulting in an increase in synaptic concentrations of dopamine.4 The transient hypertension and sinus tachycardia observed following the initiation of treatment is thought to be due to the increase in circulating catecholamines that occur as a result of methylphenidate administration.6
Prolonged tachycardia is known to cause heart failure, as demonstrated by the overexpression of β-1 receptors, which leads to apoptosis of myocardial cells and subsequently results in dilated cardiomyopathy.7
A study by Singh et al demonstrated that overstimulation of α-1 receptors can lead to myocardial hypertrophy. Persistent and sustained exposure to increased levels of circulating catecholamines results in negative remodelling that is seen in dilated cardiomyopathy.7
Our patient, prior to his admission, had been taking methylphenidate for several years, and although his admission, in our opinion, is most likely a consequence of quetiapine-induced myocarditis, it is unclear as to what extent this may have been exacerbated by the pre-existing effect of methylphenidate on the patient's heart.
The long-term safety and efficacy of methylphenidate has not been evaluated in clinical trials and, as such, the manufacturers advise caution if the drug is prescribed for more than 12 months.8 Methylphenidate should not be used indefinitely and ought to be discontinued during or after puberty; we should therefore question the long-term safety of methylphenidate in our patient and whether this could have contributed to his current admission.
As proposed in a case report by Dadfermy et al, prolonged administration and chronic exposure to methylphenidate can lead to ‘adrenergic’ susceptibility. Our patient's heart may have been primed in such a way that the administration of quetiapine acted as a stimulus for development of acute myocarditis.4
Quetiapine, is a second-generation antipsychotic that can be prescribed as an adjunct to methylphenidate for treatment-resistant ADHD in adolescents.9 Quetiapine is chemically similar to clozapine and olanzapine, both of which are known to cause cardiac hypersensitivity reactions.10 11
Myocarditis and cardiomyopathy are known to be rare, yet fatal cardiotoxic effects associated with clozapine administration. The exact pathophysiology of clozapine-induced myocarditis is unknown, but it is thought to be attributable to a type 1 hypersensitivity reaction secondary to an IgE-mediated immune response.12 13
Clozapine-induced myocarditis usually occurs within the first 6–8 weeks of treatment initiation.13 In view of our patient’s recent admission and its timing in relation to the initiation of quetiapine, it is highly probable that his admission is due to quetiapine-induced myocarditis.
There are a small number of case reports that link the administration of both methylphenidate and quetiapine to acute dilated cardiomyopathy, pericarditis and myocarditis. In a case report submitted by Roesch-Ely, a 35-year-old man with paranoid schizophrenia and no history of heart disease or cardiac risk factors was diagnosed with myocarditis on the basis of transient ST elevation on ECG and elevation of cardiac markers 2 months after the initiation of quetiapine. Since the origin of the patient's myocarditis was unknown and the only recent change to his management was the initiation of quetiapine, the drug was immediately withdrawn. Over the following days, a decrease in troponin and creatine kinase levels were observed and a definitive diagnosis of myocarditis secondary to a hypersensitivity reaction to quetiapine was made.14
In addition to the case report by Roesch-Ely, there have been reports of cardiac muscle disorders, predominantly relating to cardiomyopathy and myocarditis, in New Zealand. Of the nine cases reported, quetiapine was found to be the causative agent in five cases with clozapine the causative agent in a further two cases.15
Quetiapine-induced myocarditis results in myocardial inflammation either through direct toxic effects on myocytes/cardiac tissue or through inducing a hypersensitivity-type reaction that may present as eosinophilic myocarditis.16
Following myocardial injury, patients will often present with raised cardiac enzymes, namely troponin I or T. Both of which provide greater sensitivity and specificity than CPK, which is associated with a low predictive value and does not aid in the diagnosis of myocarditis and is therefore not recommended.2 16 17
Other non-specific markers of inflammation such as C reactive protein (CRP) or erythrocyte sedimentation rate are also elevated during the acute phase of myocarditis/inflammation. Ronaldson et al indicate that elevated CRP can, in fact, be an early warning sign of acute inflammation. CRP elevation in the context of myocarditis is known to pre-date troponin rise by 5 days and can act as an early indicator of myocarditis particularly during that time when patients may be asymptomatic or have non-specific symptoms.18
In order to aid a definitive diagnosis of myocarditis, Ronaldson et al18 advise utilising CRP measurements in addition to cardiac troponin; a combination of the two parameters will provide 100% sensitivity for myocarditis.
An echocardiogram is currently recommended as the initial diagnostic tool in patients with suspected myocarditis, the findings of which can often be varied and non-specific.17 Typical findings on echocardiography include evidence of impaired left ventricular systolic function, and segmental or regional wall motion abnormalities may be present.3
Endomyocardial biopsy (EMB) was once thought to be the gold standard diagnostic test, since it provides definitive evidence of acute myocardial inflammatory infiltrate, to differentiate myocarditis from cardiomyopathy.19 However, it is an invasive test with a major limitation due to the number of false negative results reported following biopsy.17 20
Cardiac MRI is a non-invasive alternative to EMB; it can localise and quantify the degree and nature of myocardial injury, for example, it can identify oedema, hyperaemia or fibrosis sustained secondary to the inflammation associated with myocarditis.18 19 Cardiac MRI will diagnose myocardial inflammation and myocyte injury in 80% of cases; there is a close correlation between regions of abnormal signal on MRI and regions of myocarditis.4 17
In line with current recommendations, as with all hypersensitivity-type reactions, the underlying cause must be identified and eliminated. For our patient we omitted his mood stabiliser medication in addition to advising bed rest for at least 6 weeks.17
The mainstay of treatment after withdrawal of the offending drug(s) is supportive care. AHA/ACC and ESC recommendations regarding management, following initial haemodynamic stabilisation are those that would be initiated for patients with left ventricular systolic dysfunction; ACE inhibitors and β-blockers.21
While myocarditis may be a rare side effect, the consequences of missed/late diagnosis can be fatal for the patient. A delay in diagnosis can lead to irreversible damage to the ventricles and a poor prognosis for the patient with untreated myocarditis, with a mortality rate of 50%, with half of those deaths occurring suddenly and unexpectedly.3 4
There is currently an absence of any definitive guidance regarding cardiovascular monitoring for patients started on/following dose optimisation of antipsychotic medications. Based on our literature search and review of the small number of published case reports, we propose weekly ECG monitoring and assessment of CRP and cardiac troponin measurements following the initiation of treatment with antipsychotic medication or following a dose change, for a period of 4 weeks. Since we know that drug-induced myocarditis, particularly with clozapine, usually occurs within 21 days of initiation/dose change, monitoring over a 4-week period would seem reasonable.3
This will allow for proactive monitoring and surveillance of an individual's predisposition to myocardial injury and will facilitate early detection of impending myocarditis.
Learning points.
Myocarditis refers to acute inflammation of the myocardium and its aetiology is usually viral in origin, however, autoimmune conditions have also been implicated as well as hypersensitivity reactions secondary to drug administration.
Myocarditis may be under-reported or underdiagnosed due to the variable symptoms on presentation that are often non-specific.
A high index of clinical suspicion of myocarditis should be maintained particularly in younger patients, even with no previous history/risk factors for cardiac disease, who present with chest pain while on antipsychotic medication.
More rigorous monitoring, particularly early on in treatment, is necessary to pre-empt and prevent long-term damage that may occur as a consequence of myocarditis to prevent progression to cardiomyopathy. This will require closer liaison between cardiology and psychiatry specialties, particularly during the first few weeks following the initiation/dose change of antipsychotic therapy.
Footnotes
Contributors: NK and NW were involved in data collection and drafted the paper. SM revised the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Schultheiss HP, Kuhl U, Cooper LT. The management of myocarditis. Eur Heart J 2011;32:2616–25. 10.1093/eurheartj/ehr165 [DOI] [PubMed] [Google Scholar]
- 2.Munshi TA, Volochniouk D, Hassan T et al. Clozapine-induced myocarditis: is mandatory monitoring warranted for its early recognition? Case Rep Psychiatry 2014;2014:513108 10.1155/2014/513108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldman L. Chapter 60 diseases of the myocardium and endocardium In: Goldman's Cecil medicine. Goldman L, Schafer AI, eds. Elsivier Publishing, 2012. [Google Scholar]
- 4.Cooper LT. Myocarditis. N Eng J Med 2009;360:1526–38. 10.1056/NEJMra0800028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ray WA, Chung CP, Murray KT et al. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med 2009;360:225–35. 10.1056/NEJMoa0806994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dadfermy S, Dixon J. A case of acute cardiomyopathy and pericarditis associated with methylphenidate. Cardiovasc Toxicol 2009;9:49–52. 10.1007/s12012-009-9033-7 [DOI] [PubMed] [Google Scholar]
- 7.Singh K, Xiao L, Remondino A et al. Adrenergic regulation of cardiac myocyte apoptosis. J Cell Physiol 2001;189:257–65. 10.1002/jcp.10024 [DOI] [PubMed] [Google Scholar]
- 8.Summary of Product Characteristics—Methylphenidate XL (Concerta) http://www.medicines.org.uk (accessed 24 Mar 2014).
- 9.Kronenberger WG, Giauque AL, Lafata DE et al. Quetiapine addition in methylphenidate treatment-resistant adolescents with co-morbid ADHD, conduct/oppositional-defiant disorder, and aggression: a prospective, open-label study. J Child Adolesc Psychopharmacol 2007;17:334–47. 10.1089/cap.2006.0012 [DOI] [PubMed] [Google Scholar]
- 10.Jensen VF, Gotzsche O. Allergic myocarditis in clozapine treatment. Ugeskr Laeger 1995;156:4151–2. [PubMed] [Google Scholar]
- 11.Raz A, Bergman R, Eilam O et al. A case report of olanzapine-induced hypersensitivity syndrome. Am J Med Soc 2001;321:156–8. 10.1097/00000441-200102000-00008 [DOI] [PubMed] [Google Scholar]
- 12.Hagg S, Spigset O, Bate A et al. Myocarditis related to clozapine treatment. J Clin Psychopharmacol 2001;21:382–8. 10.1097/00004714-200108000-00005 [DOI] [PubMed] [Google Scholar]
- 13.Kilian J, Kerr K, Lawrence C et al. Myocarditis and cardiomyopathy associated with clozapine. Lancet 1999;354:1841–5. 10.1016/S0140-6736(99)10385-4 [DOI] [PubMed] [Google Scholar]
- 14.Roesch-Ely D, Van Einsiedel R, Kathöfer S et al. Myocarditis with Quetiapine. Am J Psychiatry 2002;159:1607–8. (accessed 26 Feb 2014) 10.1176/appi.ajp.159.9.1607-a [DOI] [PubMed] [Google Scholar]
- 15.Quetiapine and cardiac muscle disorders. Rev Prescrire 2013;33:350. [PubMed] [Google Scholar]
- 16.Baughman KL. Diagnosis of myocarditis: death of Dallas criteria. Circulation 2006;113:593–5. 10.1161/CIRCULATIONAHA.105.589663 [DOI] [PubMed] [Google Scholar]
- 17.Mangani JW, Dec W. Myocarditis current trends in diagnosis and treatment. Circulation 2006;113:876–90. 10.1161/CIRCULATIONAHA.105.584532 [DOI] [PubMed] [Google Scholar]
- 18.Ronaldson KJ, Fitzgerald PB, Taylor AJ et al. Observations from 8 cases of clozapine rechallenge after development of myocarditis. J Clin Psychiatry 2012;73:252–4. 10.4088/JCP.11l07467 [DOI] [PubMed] [Google Scholar]
- 19.Ansari A, Maron BJ, Bernstson DG. Drug-induced toxic myocarditis. Tex Heart Inst J 2003;30:76–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar P, Clark M. Kumar and Clark's clinical medicine. 7th edn Saunders Ltd, 2009. [Google Scholar]
- 21.Cooper LT, Baughman KL, Feldman AM et al. The role of endomyocardial biopsy in the management of cardiovascular disease; a scientific statement from the American Heart Association, the American College of Cardiology, and The European Society of Cardiology. J Am Coll Cardiol 2007;50:1914–31. 10.1016/j.jacc.2007.09.008 [DOI] [PubMed] [Google Scholar]


