Abstract
Context:
F-18 fluorodeoxyglucose (F-18 FDG) positron emission tomography/computed tomography (PET/CT) scan and hypothyroidism.
Aims:
The aim was to determine whether the intensity of diffuse thyroid gland uptake on F-18 FDG PET/CT scans predicts the severity of hypothyroidism.
Materials and Methods:
A retrospective analysis of 3868 patients who underwent F-18 FDG PET/CT scans, between October 2012 and June 2013 in our institution for various oncological indications was done. Out of them, 106 (2.7%) patients (79 females, 27 males) presented with bilateral diffuse thyroid gland uptake as an incidental finding. These patients were investigated retrospectively and various parameters such as age, sex, primary cancer site, maximal standardized uptake value (SUVmax), results of thyroid function tests (TFTs) and fine-needle aspiration cytology results were noted. The SUVmax values were correlated with serum thyroid stimulating hormone (S. TSH) levels using Pearson's correlation analysis.
Statistical Analysis Used:
Pearson's correlation analysis.
Results:
Clinical information and TFT (serum FT3, FT4 and TSH levels) results were available for 31 of the 106 patients (27 females, 4 males; mean age 51.5 years). Twenty-six out of 31 patients (84%) were having abnormal TFTs with abnormal TSH levels in 24/31 patients (mean S. TSH: 22.35 μIU/ml, median: 7.37 μIU/ml, range: 0.074-211 μIU/ml). Among 7 patients with normal TSH levels, 2 patients demonstrated low FT3 and FT4 levels. No significant correlation was found between maximum standardized uptake value and TSH levels (r = 0.115, P > 0.05).
Conclusions:
Incidentally detected diffuse thyroid gland uptake on F-18 FDG PET/CT scan was usually associated with hypothyroidism probably caused by autoimmune thyroiditis. Patients should be investigated promptly irrespective of the intensity of FDG uptake with TFTs to initiate replacement therapy and a USG examination to look for any suspicious nodules.
Keywords: Chronic lymphocytic thyroiditis, diffuse thyroid fluorodeoxyglucose uptake, hypothyroidism, maximal standardized uptake value, positron emission tomography, serum thyroid stimulating hormone, thyroid function tests
INTRODUCTION
F-18 fluorodeoxyglucose (F-18 FDG) positron emission tomography (PET) has established itself in the field of oncology with its multiple indications in wide variety of cancers. Since the study, usually, covers base of the skull to mid-thigh region, clinically unexpected and incidental hypermetabolic lesions are frequently found. Accurate interpretation of such findings can impact the clinical management and overall health of the patient. Thyroid gland usually shows either low or absent FDG uptake.[1,2] This observation is in keeping with the suggestion that free fatty acids are the preferred substrates for the thyroid gland[3]—Supported by studies on animal models[4] and cell cultures.[5]
We come across a sizeable number of patients with incidental thyroid gland uptake on PET/computed tomography (CT) scans. Incidental FDG thyroid uptake on PET falls into two distinct categories: Focal and diffuse. According to previous reports, focal thyroid uptake or “incidentaloma” is detected in 1-4% of cases and is associated with malignancy in 20-50% of cases.[6,7,8,9,10] Studies on incidental diffuse thyroid gland uptake on PET or PET/CT have reported incidences ranging from 0.6% to 3.5%.[11,12,13,14,15,16,17,18]
Although initially some authors[19,20] stated that diffuse thyroid gland uptake may be a normal variant, several other studies[11,12,13,14,15,16,17,18] done later associate such uptake with autoimmune thyroiditis or hypothyroidism. Kurata et al.[12] stressed upon the fact that although diffuse FDG uptake usually indicates Hashimoto's thyroiditis, the risk of thyroid cancer must be recognized in both diffuse FDG uptake and diffuse-plus-focal FDG uptake on PET scan.
The correlation between the intensity of FDG uptake and severity of thyroiditis has not been studied extensively. Karantanis et al.[15] in their study found no significant correlation between maximal standardized uptake value (SUVmax) and degree of hypothyroidism. Lee et al.[17] however found a close correlation between the degree of incidental diffuse thyroid uptake on F-18 FDG PET and increased serum thyroid stimulating hormone (S. TSH) levels.
The purpose of this study was to determine the clinical significance of incidental diffuse thyroid gland uptake and to ascertain whether the magnitude of FDG uptake in thyroid gland predicts the severity of hypothyroidism.
MATERIALS AND METHODS
Between October 2012 and June 2013, a total of 3868 patients underwent F-18 FDG PET/CT scans in our institution for various oncological indications. All subjects voluntarily consented for the scan after obtaining information including potential benefits, radiation exposure and costs.
Out of them, 106 (2.7%) patients (79 females, 27 males) presenting with bilateral diffuse thyroid gland uptake were studied. Patients with focal thyroid uptake and those having a history of thyroid cancer were excluded. These 106 patients were investigated retrospectively and various parameters like age, sex, primary cancer site, intensity of FDG uptake and its semi-quantitative measurement in form of SUVmax, results of thyroid function tests (TFTs) and fine-needle aspiration cytology (FNAC) results were noted. This review was done through a detailed study of their hospital electronic medical records. Patients with previous history of hypothyroidism and patients who were on thyroid hormone therapy were also included in the study. For the purpose of statistical analysis, we selected only those patients having TFTs measured within 8 weeks of the PET/CT study. The relationship between the levels of S. TSH and the SUVmax of thyroid gland was studied using bi-variate analysis.
Positron emission tomography/computed tomography
Standard procedures for patient preparation and PET/CT acquisition were followed. Patients were instructed to fast and not consume anything, except for water, for at least 4 h before the administration of F-18 FDG. Intravenous fluids containing dextrose were withheld for 4-6 h prior to tracer administration. Patients were administered 8-10 mCi of F-18 FDG intravenously, provided blood glucose levels were <150 mg/dl. They were instructed to remain seated or recumbent after F-18 FDG administration to avoid muscular uptake. Image acquisition was done 60 min after F-18 FDG administration from skull base to mid-thigh (a transmission scan using CT followed by 2 min per bed emission scan) using Biograph 40 LSO advanced PET/CT scanner (Siemens, Knoxville, TN). The system consists of a 40-slice, spiral CT (Siemens Somatom Emotion) and is optimized for use in whole-body oncology. PET data were obtained in 3D mode, with attenuation correction calculated from co-registered CT images. The PET/CT scanner was subjected to daily quality control evaluation before the start of acquisition. The studies were reconstructed using a default vendor-implemented iterative reconstruction algorithm.
Image analysis
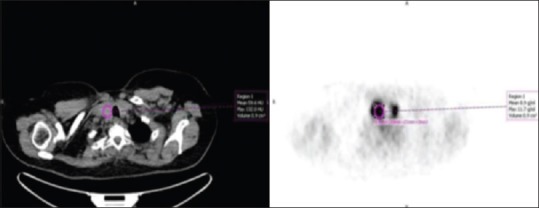
Positron emission tomography/computed tomography scan images were interpreted by two experienced nuclear medicine physicians. The intensity level was set manually, with liver being set at a light gray level. Distinctly increased F-18 FDG uptake in the thyroid, resulting in visualization of both thyroid lobes on the 3-dimensional maximum-intensity-projection images, was used as a criterion for inclusion [Figure 1]. Thyroid uptake was always then confirmed on axial CT images [Figure 2] or fused PET/CT images. Inclusion was decided by consensus of both the physicians.
Figure 1.

Trans-axial and maximal intensity projection (MIP) positron emission tomography images of a patient showing diffuse thyroid gland fluorodeoxyglucose uptake (dotted line). Visualisation of diffuse thyroid uptake on MIP images was the sole criterion for inclusion of patient in the study
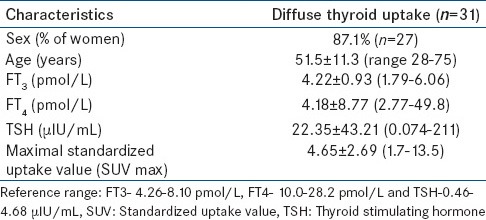
Figure 2.
Thyroid uptake was always then confirmed on axial computed tomography images (left). A circular region of interest with a fixed diameter was placed over the region of highest intensity in each lobe of the thyroid gland to calculate maximal standardized uptake value (right)
Uptake in the thyroid was measured semi-quantitatively as SUVmax corrected for body weight. The SUV is the decay-corrected ratio between measured uptake in the region of interest and the expected uptake if F-18 FDG were distributed evenly throughout the body. A circular region of interest with a fixed diameter was placed over the region of highest intensity in each lobe of the thyroid, and uptake was automatically quantified as SUVmax [Figure 2].
Laboratory evaluation
The thyroid function statuses were characterized based on in vitro TFTs, comprising of serum free tri-iodo thyronine (FT3), free thyroxine (FT4) and thyroid stimulating hormone (TSH) levels. All TFTs were performed at laboratory of our hospital accredited by national accreditation board for testing and calibration laboratories. S. TSH, FT3, and FT4 were measured using an automated, competitive chemi-luminescent immunoassay (ECIq instrumentation; VITROS). Hypothyroidism was diagnosed on the basis of a low level of serum FT4 or FT3 and a high level of TSH. Hyperthyroidism was diagnosed in subjects with a high level of serum FT4 or FT3, and a low level of TSH.
Statistical analysis
The correlation between S. TSH and SUVmax was determined using Pearson's correlation coefficient. A commercial software package (PASW Statistics 18, SPSS Inc., Chicago, IL, USA) was used for all the analyses, and P < 0.05 were considered as statistically significant. All data were expressed as mean ± standard deviation.
RESULTS
Between October 2012 and June 2013, 3868 patients underwent F-18 FDG PET/CT scan for various oncological indications. Patients with focal thyroid uptake and those having a history of thyroid cancer were excluded. The prevalence of incidental diffuse thyroid FDG uptake was 2.7% (106 of 3868) on FDG-PET/CT. Seventy-nine of them were females (74.5%) and twenty-seven males (25.5%). The incidence of diffuse thyroid uptake on FDG PET/CT was significantly higher in females (female:male ratio of 2.9:1). The finding of diffusely increased thyroid uptake was reported on the PET scan as “suggestive of thyroiditis.”
Thyroid function test results [Table 1] were available for 31 of the 106 patients (27 females, 4 males and mean age 51.5 ± 11.3 years). FNAC result was available in 1 patient. These patients were enrolled in the study. Thyroid antibody levels were not measured in any patient.
Table 1.
Subject demographic, thyroid function test and SUV max results in patients showing diffuse thyroid uptake
Twenty-six out of 31 patients (84%) were having abnormal TFTs [Table 2] with abnormal TSH levels in 24/31 patients (mean S. TSH: 22.35 ± 43.21 μIU/ml, median: 7.37 μIU/ml, range: 0.074-211 μIU/ml). Of these 24 patients, 22 patients (70.9%) were having increased S.TSH levels suggestive of hypothyroidism, whereas TSH levels were low in 2 patients [Figure 3]. In 4 of these 24 patients, S. TSH levels were in the range of 71.3-211 μIU/ml suggestive of overt hypothyroidism. In 7 patients with normal TSH levels, 2 patients had low FT3 and FT4 levels. Majority of patients under study (approximately 60%) showed normal serum FT3 and FT4 levels [Table 2]. However, mean serum FT3 and FT4 levels were below the lower limit of normal reference range [Table 1].
Table 2.
Thyroid functional status of patients showing diffuse thyroid uptake on 18F-FDG PET/CT
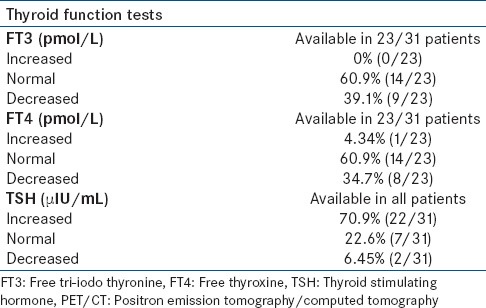
Figure 3.
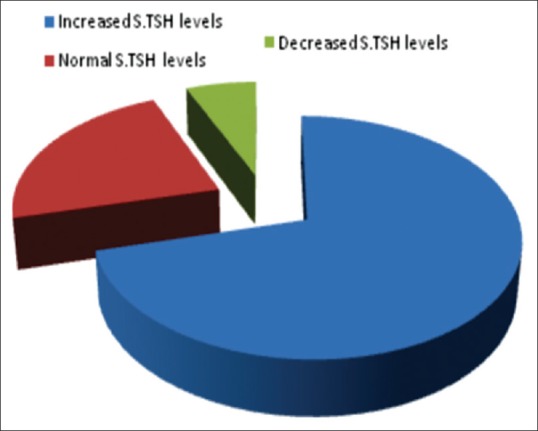
Division of patients based on serum thyroid stimulating hormone levels
Thyroid function tests were performed prior to PET/CT scan in 8/31 patients. All these patients were detected with high S. TSH levels at that time indicative of hypothyroidism. On carefully examining the medical records of these patients, we found that 5 patients were started on replacement thyroxine hormone prior to undergoing PET/CT examination. In 1 patient, thyroxine was not started because TSH levels were marginally higher, and patient was asymptomatic. This patient was kept on follow-up. In 2 patients, no record of thyroid medication was available. In 23/31 patients, TFTs were evaluated for the first time after PET/CT examination.
In 1 patient FNAC was done following ultrasonographic examination of the neck which showed papillary thyroid carcinoma in the background of lymphocytic thyroiditis. However, no focal thyroid gland uptake was seen in this patient.
No significant correlation was found between maximum standardized uptake value and TSH levels (Pearson's correlation coefficient [r] = 0.115, P > 0.05).
DISCUSSION
The expanding use of PET in clinical practice underlines the need to clarify the clinical significance of and further evaluate incidental findings. Studies carried out earlier on incidental diffuse thyroid gland uptake on PET or PET/CT have reported incidences ranging from 0.6% to 3.5%[9,11,12,13,14,15,16,17,18]. Yasuda et al.[13] reported diffuse F-18 FDG uptake in the thyroid in 36 (3.3%) of 1102 healthy subjects who underwent PET as part of a cancer screening program in Japan. Kim et al.[9] found, in a retrospective study, diffuse thyroid uptake in 45 (1.1%) of 4136 patients undergoing PET for non-thyroid-related malignancies. Are et al.[18] in their study reported that 162/8800 patients (1.8%) demonstrated diffuse thyroid uptake, and only 2 of them (1.2%) were found to have malignancy. Our study found an incidence of 2.7% (106/3868 patients) of incidental diffuse thyroid gland uptake on F-18 FDG PET/CT.
Most of these studies attributed this phenomenon to “autoimmune/hashimoto's thyroiditis” or more specifically “hypothyroidism.”[14,15,16,17] In a study by Kurata et al.[12] all subjects with diffuse FDG uptake were diagnosed as having Hashimoto's thyroiditis. Chen[14] reported that diffuse intense uptake and higher SUV levels are a clue to a diagnosis of chronic thyroiditis, especially for those with hypothyroidism. In a recent study by Lee et al.[17] S. TSH levels were significantly higher in group with diffuse thyroid FDG uptake than in the control group. In our study, 26 out of 31 patients (84%) were having abnormal thyroid function results. Features of hypothyroidism, i.e., low serum FT3, FT4 and high TSH levels were noted in 24/31 patients (77.4%) with 4 patients presenting with overt hypothyroidism. Mean serum FT3, FT4 and TSH levels also indicate the presence of hypothyroidism in majority of study population [Table 1]. These findings suggest strong clinical correlation between diffuse thyroid gland FDG uptake and hypothyroidism. Hence, our results are concordant with the studies done in the past in this regard.
2/31 patients with diffuse FDG uptake demonstrated low S. TSH levels. This could be explained by the fact that early phases of thyroiditis may show features of thyrotoxicosis, i.e., Hashi-toxicosis.
Five patients were found to have a prior history of hypothyroidism, and these patients were already taking thyroxine replacement therapy. However, these patients also demonstrated diffusely increased FDG uptake in thyroid gland. Whether adequate thyroid hormone replacement reduces, the intensity of FDG uptake in thyroid gland is difficult to ascertain based on the findings of our study due to insufficient patient number and unavailability of follow-up PET/CT scans. A prospective analysis with a higher number of patients is warranted to study this phenomenon.
Clinical significance of intensity of FDG uptake and it's correlation with severity of thyroiditis has not been studied extensively. Karantanis et al.[15] in their study found no significant correlation between SUV values and degree of hypothyroidism (S. TSH) or serum thyroperoxidase (TPO) levels. Lee et al.[17] found a close correlation between the degree of incidental diffuse thyroid uptake on F-18 FDG PET and increased S. TSH levels. However, in this study[17] degree of thyroid uptake was determined using a visual grading system rather than quantitative measurement in the form of SUVmax. Our study found no significant correlation between SUVmax and S. TSH levels (Pearson's correlation coefficient = 0.115, P > 0.05). The fact that we did not find any significant correlation between the levels of F-18 FDG uptake in the thyroid and TSH levels in the serum suggests that even mild or low F-18 FDG uptake in the thyroid gland should not be ignored. Such uptake may be associated with overt or subclinical hypothyroidism requiring thyroid hormone therapy, dose adjustment, or further evaluation.
In 1 out of 106 patients, FNAC was done following ultrasonographic examination of the neck, which showed papillary thyroid carcinoma in the background of lymphocytic thyroiditis. However, no focal thyroid gland uptake was seen in this patient. Kurata et al.[12] in their study have reported cases of papillary thyroid carcinoma associated with Hashimoto's thyroiditis in patients showing diffuse FDG thyroid uptake and diffuse plus focal thyroid uptake and suggested that risk of thyroid cancer must be recognized in both diffuse FDG uptake and diffuse-plus-focal FDG uptake on PET scan.[12]
Since, ours was a retrospective study histopathological correlation was not possible in all the patients as it was performed in only 1 patient by the clinician. Thyroid uptake was persisting in most of the patients who underwent follow-up PET CT study. However, in the absence of follow up data, findings in our study are initial inferences that need confirmation on follow-up.
CONCLUSION
Incidentally detected diffuse thyroid gland uptake on F-18 FDG PET/CT scans is, usually, associated with hypothyroidism probably caused by benign lymphocytic (Hashimoto's) thyroiditis. As the study found no significant correlation between intensity of FDG uptake and severity of hypothyroidism, hence, patients demonstrating even mild or low diffuse thyroid gland FDG uptake on PET/CT should be promptly investigated with TFTs to initiate replacement therapy and a USG examination to look for any suspicious nodules.
ACKNOWLEDGMENT
Amita Gupta, Praveen Sharma, Ratnam Sengupta, Amit Pandey.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nakamoto Y, Tatsumi M, Hammoud D, Cohade C, Osman MM, Wahl RL. Normal FDG distribution patterns in the head and neck: PET/CT evaluation. Radiology. 2005;234:879–85. doi: 10.1148/radiol.2343030301. [DOI] [PubMed] [Google Scholar]
- 2.Bogsrud TV, Lowe V. Normal variants and pitfalls in whole-body PET imaging with 18F FDG. Appl Radiol. 2006;35:16–30. [Google Scholar]
- 3.Field J. Intermediary metabolism of the thyroid. In: Astwood EB, Greep RO, editors. American Physiological Society Handbook of Physiology: Endocrinology. Thyroid. Sec. 7. III. Washington: DC: American Physiological Society; 1974. –147.pp. 59 [Google Scholar]
- 4.Hosaka Y, Tawata M, Kurihara A, Ohtaka M, Endo T, Onaya T. The regulation of two distinct glucose transporter (GLUT1 and GLUT4) gene expressions in cultured rat thyroid cells by thyrotropin. Endocrinology. 1992;131:159–65. doi: 10.1210/endo.131.1.1319316. [DOI] [PubMed] [Google Scholar]
- 5.Gould GW, Thomas HM, Jess TJ, Bell GI. Expression of human glucose transporters in Xenopus oocytes: Kinetic characterization and substrate specificities of the erythrocyte, liver, and brain isoforms. Biochemistry. 1991;30:5139–45. doi: 10.1021/bi00235a004. [DOI] [PubMed] [Google Scholar]
- 6.Bae JS, Chae BJ, Park WC, Kim JS, Kim SH, Jung SS, et al. Incidental thyroid lesions detected by FDG-PET/CT: Prevalence and risk of thyroid cancer. World J Surg Oncol. 2009;7:63. doi: 10.1186/1477-7819-7-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi JY, Lee KS, Kim HJ, Shim YM, Kwon OJ, Park K, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: Clinical significance and improved characterization. J Nucl Med. 2006;47:609–15. [PubMed] [Google Scholar]
- 8.Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC, Brunt LM, et al. Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery. 2001;130:941–6. doi: 10.1067/msy.2001.118265. [DOI] [PubMed] [Google Scholar]
- 9.Kim TY, Kim WB, Ryu JS, Gong G, Hong SJ, Shong YK. 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: High prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope. 2005;115:1074–8. doi: 10.1097/01.MLG.0000163098.01398.79. [DOI] [PubMed] [Google Scholar]
- 10.Shie P, Cardarelli R, Sprawls K, Fulda KG, Taur A. Systematic review: Prevalence of malignant incidental thyroid nodules identified on fluorine-18 fluorodeoxyglucose positron emission tomography. Nucl Med Commun. 2009;30:742–8. doi: 10.1097/MNM.0b013e32832ee09d. [DOI] [PubMed] [Google Scholar]
- 11.Chen W, Parsons M, Torigian DA, Zhuang H, Alavi A. Evaluation of thyroid FDG uptake incidentally identified on FDG-PET/CT imaging. Nucl Med Commun. 2009;30:240–4. doi: 10.1097/MNM.0b013e328324b431. [DOI] [PubMed] [Google Scholar]
- 12.Kurata S, Ishibashi M, Hiromatsu Y, Kaida H, Miyake I, Uchida M, et al. Diffuse and diffuse-plus-focal uptake in the thyroid gland identified by using FDG-PET: Prevalence of thyroid cancer and Hashimoto's thyroiditis. Ann Nucl Med. 2007;21:325–30. doi: 10.1007/s12149-007-0030-2. [DOI] [PubMed] [Google Scholar]
- 13.Yasuda S, Shohtsu A, Ide M, Takagi S, Takahashi W, Suzuki Y, et al. Chronic thyroiditis: Diffuse uptake of FDG at PET. Radiology. 1998;207:775–8. doi: 10.1148/radiology.207.3.9609903. [DOI] [PubMed] [Google Scholar]
- 14.Chen YK, Chen YL, Cheng RH, Yeh CL, Lee CC, Hsu CH. The significance of FDG uptake in bilateral thyroid glands. Nucl Med Commun. 2007;28:117–22. doi: 10.1097/MNM.0b013e328013eaf7. [DOI] [PubMed] [Google Scholar]
- 15.Karantanis D, Bogsrud TV, Wiseman GA, Mullan BP, Subramaniam RM, Nathan MA, et al. Clinical significance of diffusely increased 18F-FDG uptake in the thyroid gland. J Nucl Med. 2007;48:896–901. doi: 10.2967/jnumed.106.039024. [DOI] [PubMed] [Google Scholar]
- 16.Liu Y. Clinical significance of thyroid uptake on F18-fluorodeoxyglucose positron emission tomography. Ann Nucl Med. 2009;23:17–23. doi: 10.1007/s12149-008-0198-0. [DOI] [PubMed] [Google Scholar]
- 17.Lee JY, Choi JY, Choi YH, Hyun SH, Moon SH, Jang SJ, et al. Diffuse thyroid uptake incidentally found on 18F-fluorodeoxyglucose positron emission tomography in subjects without cancer history. Korean J Radiol. 2013;14:501–9. doi: 10.3348/kjr.2013.14.3.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Are C, Hsu JF, Schoder H, Shah JP, Larson SM, Shaha AR. FDG-PET detected thyroid incidentalomas: Need for further investigation? Ann Surg Oncol. 2007;14:239–47. doi: 10.1245/s10434-006-9181-y. [DOI] [PubMed] [Google Scholar]
- 19.Gordon BA, Flanagan FL, Dehdashti F. Whole-body positron emission tomography: Normal variations, pitfalls, and technical considerations. AJR Am J Roentgenol. 1997;169:1675–80. doi: 10.2214/ajr.169.6.9393189. [DOI] [PubMed] [Google Scholar]
- 20.Shreve PD, Anzai Y, Wahl RL. Pitfalls in oncologic diagnosis with FDG PET imaging: Physiologic and benign variants. Radiographics. 1999;19:61–77. doi: 10.1148/radiographics.19.1.g99ja0761. [DOI] [PubMed] [Google Scholar]


