Abstract
With the rise in a number of bariatric procedures, surgeons are facing more complex and technically demanding surgical situations. Robotic digital platforms potentially provide a solution to better address these challenges. This review examines the published literature on the outcomes and complications of bariatric surgery using a robotic platform. Use of robotics to perform adjustable gastric banding, sleeve gastrectomy, roux-en-y gastric bypass (RYGB), biliopancreatic diversion with duodenal switch and revisional bariatric procedures (RBP) is assessed. A search on PubMed was performed for the most relevant articles in robotic bariatric surgery. A total of 23 articles was selected and reviewed in this article. The review showed that the use of robotics led to similar or lower complication rate in bariatric surgery when compared with laparoscopy. Two studies found a significantly lower leak rate for robotic gastric bypass when compared to laparoscopic method. The learning curve for RYGB seems to be shorter for robotic technique. Three studies revealed a significantly shorter operative time, while four studies found a longer operative time for robotic technique of gastric bypass. As for the outcomes of RBP, one study found a lower complication rate in robotic arm versus laparoscopic and open arms. Most authors stated that the use of robotics provides superior visualisation, more degrees of freedom and better ergonomics. The application of robotics in bariatric surgery seems to be a safe and feasible option. Use of robotics may provide specific advantages in some situations, and overcome limitations of laparoscopic surgery. Large and well-designed randomised clinical trials with long follow-up are needed to further define the role of digital platforms in bariatric surgery.
Keywords: Bariatric, gastric bypass, review, robotic surgery, roux-en-y, sleeve gastrectomy
INTRODUCTION
With the rise in the prevalence of obesity, the field of bariatric surgery is witnessing an ever increasing demand. Along with that, comes the challenge of operating on patients with high body mass index (BMI), revisional bariatric procedures (RBP), managing complications and reoperative abdomens. Performing bariatric surgery can be technically demanding in many situations because of large patients, large livers, thick abdominal walls and substantial visceral fat making exposure, dissection, and reconstruction difficult.[1] The super obese (SO) patients with a BMI ≥50 kg/m2 is a difficult to manage population because of limited working space, excessive torque on instruments due to thick abdominal wall, co-morbidities and high-risk anaesthesia.[2] The management of patients with super-super obesity (BMI >60 kg/m2) also remains a challenge.[3] Moreover, the surgeons encounter very difficult ergonomic positions, which can potentially be career shortening for them. The surgeons have been looking for methods to improve the patient outcomes, surgical technique and decrease complications on one hand, and reducing the number and size of incisions on the other hand.
Use of robotics in bariatric surgery has been evolving since Cadiere et al. reported the first such case in 1999.[4] Robotic surgery has provided the surgeons with the advantage of three-dimensional vision, increased dexterity and precision by downscaling surgeon's movements enabling a fine tissue dissection and filtering out physiological tremor.[5,6] It overcomes the restraint of torque on ports from thick abdominal wall, and minimises port site trauma by remote centre technology.[7] The main limitation with robotic surgery is the perceived higher cost and set-up time compared with laparoscopy. But with increased experience, it is seen that set-up times reduce, and costs may also come down as material prices reduce.[8]
METHODS
The mainstream bariatric procedures are adjustable gastric banding (AGB), sleeve gastrectomy (SG), roux-en-y gastric bypass (RYGB) and biliopancreatic diversion with duodenal switch. Using PubMed, we reviewed the published evidence of using robotics for these procedures as well as performing RBP. The search terms included bariatric surgery, robotic bariatric surgery, robotic gastric banding, robotic SG, robotic roux-en-y gastric bypass (RRYGB), robotic biliopancreatic diversion and robotic revisional bariatric surgery. The inclusion criteria were English language, original research, bariatric surgical procedures using robotics and human studies. We reviewed the data specific to each bariatric procedure and analysed it accordingly.
Robotic Adjustable Gastric Banding
Adjustable gastric banding was the first bariatric procedure performed using a robot.[4] It is technically considered the simplest of all bariatric procedures. The use of AGB has decreased tremendously all over the world because of low efficacy and high revision/complication rate associated with it. There have been few studies published in the literature looking at outcomes of robotic assistance in AGB, and showed little benefit for using the robot.[9,10,11] Edelson et al.[12] reported the largest study with 287 patients of robotic AGB compared with 120 patients who underwent laparoscopic AGB. No significant differences were found in the operating room (OR) times, hospital stay, complication rates, or excess weight loss. They did find a shorter operative time by 12 min in the robotic arm when compared for SO patients. As of now, robot is used mostly for managing complications and revising gastric band to another weight loss procedure, and this is dealt with in the section on RBP.
Robotic Sleeve Gastrectomy
Sleeve gastrectomy is increasingly becoming popular because of its low morbidity, excellent outcome and perceived technical simplicity. It is especially so in Indian sub-continent because of high prevalence of a vegetarian population, who tend to choose a restrictive procedure rather than a malabsorptive one. There are certain peculiarities in SG like it has a long staple line with the potential to leak, and a precise and safe dissection is required in the area of the left crus and hiatus entirely to mobilize the fundus. Compared to laparoscopic surgery, robotic surgery offers the possibility for endowrist, and this action facilitates the hiatal dissection and over sewing of the staple line.
Five studies have been published, which focus on robotic sleeve gastrectomy (RSG).[13,14,15,16,17] Diamantis et al.[13] published a feasibility study that included 19 patients who underwent RSG. Their mean OR time was 95.5 min and reported complication rate was zero. Ayloo et al.[14] compared 30 robotic with 39 laparoscopic SG procedures and found no difference in length of hospital stay, complication rates or excess body weight loss at 1-year. They found a significantly longer OR time for RSG (135 vs. 114 min), due to the fact that they had oversewn the staple line in the robotic arm and not in the laparoscopic arm.
Vilallonga et al.[15] reported that the learning curve of performing RSG is over by 20 cases. He also published a large comparative series on SG including 100 patients each in robotic and laparoscopic arms.[16] They found that OR time was significantly longer in a robotic group by 12 min. There was no significant difference in other peri-operative parameters or complication rate. They did found that leaks occurred only in those patients in whom they did not oversew the staple line, but used a buttress material. They concluded that RSG is a good stepping stone to robotic gastric bypass and RBP. Romero et al.[17] published their experience of 134 RSG cases and compared it with descriptive results of a systematic review of laparoscopic SG (n = 3148). The OR time was significantly higher by 12 min (P = 0.006), whereas the length of stay was lower by 1.1 days in a robotic group (P ≤ 0.005). Leaks were found in 0 RSG versus 1.97% laparoscopic SG (P = 0.101); strictures in 0 versus 0.43% (P = 0.447); bleeding in 0.7 versus 1.21% (P = 0.594); and mortality in 0 versus 0.1% (P = 0.714), respectively.
We performed a comparative study of RSG in morbidly obese (MO) versus SO patients at our centre. 11 SO patients were compared with 24 MO patients who underwent robotic SG with oversewing of the staple line in all the cases. The mean OR time was 116.3 min and mean docking time was 8.9 min. There was no significant difference in OR time, length of hospital stay or complications in between the two groups. Thus, presumably, using a robotic system overcomes many difficulties in the SO patients and enables the surgeon perform the similar procedure as in MO patients with equal precision, similar time and little or no extra effort.
Robotic Roux-en-Y Gastric Bypass
Roux-en-y gastric bypass is considered as the gold standard surgical procedure for morbid obesity by many specialists.[18,19] The overall results are good in terms of both weight loss and comorbidity resolution.[20] As RYGB involves two anastomoses (gastrojejunostomy [GJ] and jejunojejunostomy), robotic surgery is currently considered as an attractive technology that could help perform RYGB, given its well-described advantages.[21] It is also the most studied robotic bariatric procedure.
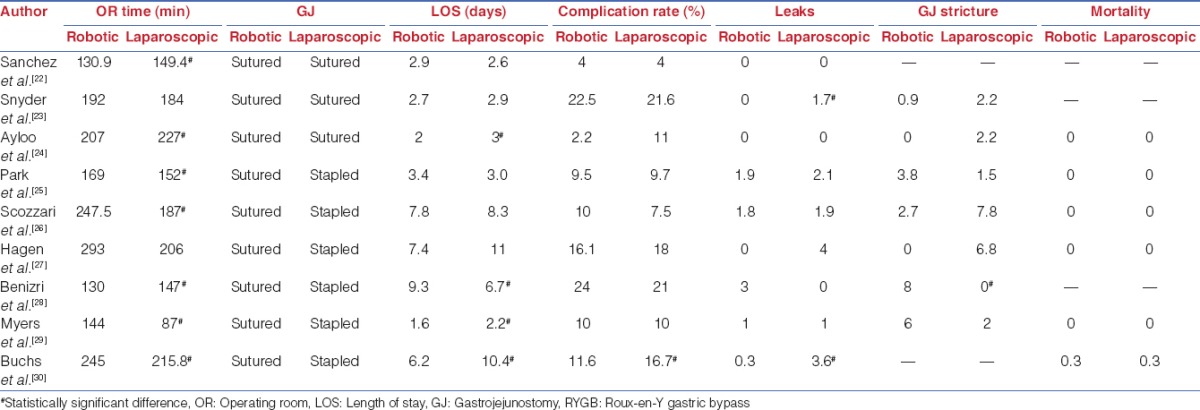
There have been nine significant published series comparing outcomes of RRYGB versus laparoscopic RYGB (LRYGB).[22,23,24,25,26,27,28,29,30] These studies represent the entire literature on RRYGB and its outcomes. For each study, we report the number of patients, mean age, mean preoperative BMI, mean OR time, type of GJ (sutured or stapled), length of hospital stay, overall complication rate, leak rate, GJ stricture rate and mortality. These results are compiled in Tables 1 and 2.
Table 1.
Robotic vs. laparoscopic RYGB: Preoperative data
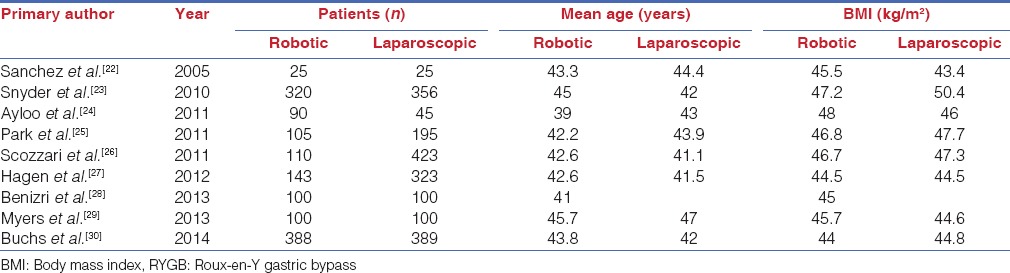
Table 2.
Robotic vs. laparoscopic RYGB: Peri-operative data
There was a total of 3337 patients in these 9 studies with 1381 in a robotic arm and 1956 in the laparoscopic arm. The mean age in RRYGB and LRYGB group was 43.3 years and 42.4 years, respectively. Average BMI was 45.8 in RRYGB patients and 46.7 in LRYGB patients.
The mean OR time was 211.9 min in robotic arm versus 185.1 min in the laparoscopic arm. Three studies report a significantly shorter operative time in a robotic group,[22,24,28] while four studies report a significantly longer operative time in a robotic arm.[25,26,29,30] This may be compounded by the fact that in all the studies, a sutured GJ was done in the robotic arm, while a stapled GJ was done in the laparoscopic arm in six out of nine studies. The average length of stay was 5 days in robotic group versus 7.1 days in the laparoscopic group. Three studies found a statistically significant shorter hospital stay in the robotic arm,[24,29,30] while one study found a significantly longer stay in the robotic arm.[28]
The overall complication rate was 12.2% in RRYGB group versus 13.3% in LRYGB group. Buchs et al.[30] found a significantly lower incidence of complication in a robotic group (11.6% vs. 16.1%). The average leak rate across studies was 0.9% in RRYGB versus 1.6% in LRYGB, while the GJ stricture rate was 3.1% in a robotic arm and 3.2% in the laparoscopic arm. Snyder et al.[23] and Buchs et al.[30] found a significantly lower leak rates in RRYGB. Benizri et al.[28] found a significantly higher GJ stricture rate for a robotic arm. The overall mortality in both groups was 0.05%.
Of all the published studies, there is only one prospectively randomized trial by Sanchez et al.[22] The other studies are either comparative studies, case series, retrospective or prospective analyses. There is a surgeon skill bias at play in the majority of these studies as it is very difficult to find a surgeon equally skilled in both robotic and laparoscopic techniques. Most of the surgeons and their teams become proficient in either of the two techniques. But large comparative studies and systematic reviews do offer some tendencies for robotic bariatric surgery.[31,32,33,34]
The learning curve of both LRYGB and RRYGB has been studied. Learning curve for LRYGB has been reported to be 75-100 cases in order to normalize complications.[35,36] Buchs et al.[21] analysed the learning curve for RRYGB and found it to be 14 cases in order to achieve mastery for a surgeon well versed in laparoscopic surgery but not in bariatric procedures. Yu et al.[37] studied complications in first 100 cases of RRYGB, and found no leaks and one reoperation. The published literature seems to suggest that the learning curve for robot assisted RYGB is shorter than laparoscopic technique.
Robotic Biliopancreatic Diversion with Duodenal Switch
Sudan et al. reported the outcomes, learning curve and technique of robotic biliopancreatic diversion with duodenal switch (RBPDDS).[38,39,40] They published experience of 47 patients who underwent this procedure with a mean BMI of 45 kg/m2 and the mean age of 38 years. The median OR time was 514 min, which decreased to 379 min in last 10 patients. There were four leaks, three conversions and no mortality in the series. The learning for RBPDDS was found to be around 50 cases after which the complications and OR time normalised.[39]
Robotic Revisional Bariatric Procedures
Revisional bariatric procedures are difficult and complex situations in which use of robotics hold a great potential. With increasing numbers of bariatric procedures, more and more patients require revisional procedures for inadequate weight loss or complications arising out of previous surgery. The anatomy in these situations is distorted which along with adhesions present a challenge to the surgeons. Complication rates of laparoscopy in these situations have been high with leak rates of 13.2% and mortality of 2%.[41] There is a couple of studies available on RBP that show better outcomes with robot assistance in these challenging cases.[42,43]
Snyder et al.[42] reviewed 99 cases that were revised using robot assistance at one centre. The mean BMI decreased from 44.8 to 29 kg/m2 after 3 years. The overall complication rate was 17% with a 90 days readmission rate of 24%. However, there was no leak, haemorrhage or mortality in the series, which is promising considering the high incidence of these complications in these situations. Buchs et al.[43] compared the outcomes of RBP performed by robotic (n = 11), laparoscopic (n = 21) and open (n = 28) method. They found that the robotic arm had fewer complications (0 vs. 14.3% for laparoscopy, vs. 10.7% for open), but took longer to perform (352 vs. 270 vs. 250 min, respectively). There were fewer conversions in robotic group (0 vs. 14.3% for laparoscopy) and a significantly shorter hospital stay (6 vs. 8 vs. 9 days, respectively).
DISCUSSION
This review of published literature reveals that the routine use of robotics in bariatric surgery is a safe and feasible option. Several studies have shown a lower complication rate with the robotic platform including leaks, haemorrhage and stricture. The advantage of robotics is perceived much more in challenging situations like RBP. However, in order to graduate to these advanced procedures, one has to move a step by step, starting with RSG and moving on to RRYGB and RBP.
The learning curve of RRYGB has also been shown to be shorter as compared to LRYGB.[21] The entire team learns with the surgeon and develops experience about patient safety precautions, OR set-up, and type of instruments needed, thus leading to better OR times with better patient outcomes. Robotic surgery is a team effort, and more so in bariatric surgery, where the role of an experienced bedside surgeon cannot be understated, as he is responsible for stapling (if robotic staplers are not used). As the main surgeon is separated from the patient, while performing robotic surgery, the assistant surgeon has to be trained enough to help him perform difficult tasks and also to take care of any emergency situation arising during the procedure. The role of a trained scrub nurse and OR technician is also very important in streamlining the conduct of the procedure and prevent any wastage of time and resources.
Another advantage, which comes with the use of the robotic system, is improved ergonomics and lesser operator fatigue. Ergonomics in laparoscopic surgery can be very challenging with big patients and uncomfortable postures, which lead to surgeon fatigue and work related musculoskeletal symptoms.[44] Robotics provides the advantage of more degrees of freedom, which is advantageous in performing difficult dissection and sutured anastomosis.
There has been a concern about cost every time use of the robotic system is considered as the direct costs are generally higher for the robotic approach in bariatric procedures like RYGB.[45] However, Hagen et al.[27] took into consideration the total costs including the complications and readmissions. They found that the cost of RRYGB was lower as compared to LRYGB when all the factors were counted for. There is also a saving due to decrease in number of laparoscopic staplers used in robotic procedures, by doing a handsewn anastomosis.
At the end of the day, the big question to be answered is whether the use of robotics is going to stay or will it perish with time like many fancy technologies. Looking at the basic concept of computer-assisted navigational surgery, robotics provides an enabling platform in between surgeon and the patient. It provides augmented and higher quality inputs from the patient to the surgeon, and his output is refined to a superior quality before reaching back to the target. According to us, this should not be analysed in terms of features of the present machine that is available for use, but in terms of the potential in the concept of using a digital interface to interact with patients and enhance the performance of the surgeon. With the advent of newer technologies in robotics like fluorescence, integration of images, virtual and augmented reality, telesurgery, single site platforms, natural orifice surgery and haptic feedback, we believe that it will provide an empowering tool to the surgeons, which can potentially change the way surgery is practiced today.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wilson EB, Sudan R. The evolution of robotic bariatric surgery. World J Surg. 2013;37:2756–60. doi: 10.1007/s00268-013-2125-3. [DOI] [PubMed] [Google Scholar]
- 2.Parikh MS, Shen R, Weiner M, Siegel N, Ren CJ. Laparoscopic bariatric surgery in super-obese patients (BMI>50) is safe and effective: A review of 332 patients. Obes Surg. 2005;15:858–63. doi: 10.1381/0960892054222632. [DOI] [PubMed] [Google Scholar]
- 3.Gagner M, Gumbs AA, Milone L, Yung E, Goldenberg L, Pomp A. Laparoscopic sleeve gastrectomy for the super-super-obese (body mass index >60 kg/m(2)) Surg Today. 2008;38:399–403. doi: 10.1007/s00595-007-3645-y. [DOI] [PubMed] [Google Scholar]
- 4.Cadiere GB, Himpens J, Vertruyen M, Favretti F. The world's first obesity surgery performed by a surgeon at a distance. Obes Surg. 1999;9:206–9. doi: 10.1381/096089299765553539. [DOI] [PubMed] [Google Scholar]
- 5.Talamini MA, Chapman S, Horgan S, Melvin WS Academic Robotics Group. A prospective analysis of 211 robotic-assisted surgical procedures. Surg Endosc. 2003;17:1521–4. doi: 10.1007/s00464-002-8853-3. [DOI] [PubMed] [Google Scholar]
- 6.Bindal V, Bhatia P, Kalhan S, Khetan M, John S, Ali A, et al. Robot-assisted excision of a large retroperitoneal schwannoma. JSLS. 2014;18:150–4. doi: 10.4293/108680813X13654754534873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cadière GB, Himpens J, Vertruyen M, Bruyns J, Germay O, Leman G, et al. Evaluation of telesurgical (robotic) NISSEN fundoplication. Surg Endosc. 2001;15:918–23. doi: 10.1007/s004640000217. [DOI] [PubMed] [Google Scholar]
- 8.Nakadi IE, Mélot C, Closset J, DeMoor V, Bétroune K, Feron P, et al. Evaluation of da Vinci Nissen fundoplication clinical results and cost minimization. World J Surg. 2006;30:1050–4. doi: 10.1007/s00268-005-7950-6. [DOI] [PubMed] [Google Scholar]
- 9.Alqahtani A. Robotic gastric banding in children and adolescents: A comparative study. Surg Endosc. 2011;25:3647–51. doi: 10.1007/s00464-011-1772-4. [DOI] [PubMed] [Google Scholar]
- 10.Moser F, Horgan S. Robotically assisted bariatric surgery. Am J Surg. 2004;188:38S–44. doi: 10.1016/j.amjsurg.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 11.Mühlmann G, Klaus A, Kirchmayr W, Wykypiel H, Unger A, Höller E, et al. DaVinci robotic-assisted laparoscopic bariatric surgery: Is it justified in a routine setting? Obes Surg. 2003;13:848–54. doi: 10.1381/096089203322618632. [DOI] [PubMed] [Google Scholar]
- 12.Edelson PK, Dumon KR, Sonnad SS, Shafi BM, Williams NN. Robotic vs. conventional laparoscopic gastric banding: A comparison of 407 cases. Surg Endosc. 2011;25:1402–8. doi: 10.1007/s00464-010-1403-5. [DOI] [PubMed] [Google Scholar]
- 13.Diamantis T, Alexandrou A, Nikiteas N, Giannopoulos A, Papalambros E. Initial experience with robotic sleeve gastrectomy for morbid obesity. Obes Surg. 2011;21:1172–9. doi: 10.1007/s11695-010-0242-8. [DOI] [PubMed] [Google Scholar]
- 14.Ayloo S, Buchs NC, Addeo P, Bianco FM, Giulianotti PC. Robot-assisted sleeve gastrectomy for super-morbidly obese patients. J Laparoendosc Adv Surg Tech A. 2011;21:295–9. doi: 10.1089/lap.2010.0398. [DOI] [PubMed] [Google Scholar]
- 15.Vilallonga R, Fort JM, Gonzalez O, Caubet E, Boleko A, Neff KJ, et al. The initial learning curve for robot-assisted sleeve gastrectomy: A surgeon's experience while introducing the robotic technology in a bariatric surgery department. Minim Invasive Surg. 2012;2012:347131. doi: 10.1155/2012/347131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vilallonga R, Fort JM, Caubet E, Gonzalez O, Armengol M. Robotic sleeve gastrectomy versus laparoscopic sleeve gastrectomy: A comparative study with 200 patients. Obes Surg. 2013;23:1501–7. doi: 10.1007/s11695-013-1039-3. [DOI] [PubMed] [Google Scholar]
- 17.Romero RJ, Kosanovic R, Rabaza JR, Seetharamaiah R, Donkor C, Gallas M, et al. Robotic sleeve gastrectomy: Experience of 134 cases and comparison with a systematic review of the laparoscopic approach. Obes Surg. 2013;23:1743–52. doi: 10.1007/s11695-013-1004-1. [DOI] [PubMed] [Google Scholar]
- 18.Schauer PR, Ikramuddin S. Laparoscopic surgery for morbid obesity. Surg Clin North Am. 2001;81:1145–79. doi: 10.1016/s0039-6109(05)70189-4. [DOI] [PubMed] [Google Scholar]
- 19.Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes Surg. 2004;14:1157–64. doi: 10.1381/0960892042387057. [DOI] [PubMed] [Google Scholar]
- 20.Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 21.Buchs NC, Pugin F, Bucher P, Hagen ME, Chassot G, Koutny-Fong P, et al. Learning curve for robot-assisted Roux-en-Y gastric bypass. Surg Endosc. 2012;26:1116–21. doi: 10.1007/s00464-011-2008-3. [DOI] [PubMed] [Google Scholar]
- 22.Sanchez BR, Mohr CJ, Morton JM, Safadi BY, Alami RS, Curet MJ. Comparison of totally robotic laparoscopic Roux-en-Y gastric bypass and traditional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2005;1:549–54. doi: 10.1016/j.soard.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Snyder BE, Wilson T, Leong BY, Klein C, Wilson EB. Robotic-assisted Roux-en-Y Gastric bypass: Minimizing morbidity and mortality. Obes Surg. 2010;20:265–70. doi: 10.1007/s11695-009-0012-7. [DOI] [PubMed] [Google Scholar]
- 24.Ayloo SM, Addeo P, Buchs NC, Shah G, Giulianotti PC. Robot-assisted versus laparoscopic Roux-en-Y gastric bypass: Is there a difference in outcomes? World J Surg. 2011;35:637–42. doi: 10.1007/s00268-010-0938-x. [DOI] [PubMed] [Google Scholar]
- 25.Park CW, Lam EC, Walsh TM, Karimoto M, Ma AT, Koo M, et al. Robotic-assisted Roux-en-Y gastric bypass performed in a community hospital setting: The future of bariatric surgery? Surg Endosc. 2011;25:3312–21. doi: 10.1007/s00464-011-1714-1. [DOI] [PubMed] [Google Scholar]
- 26.Scozzari G, Rebecchi F, Millo P, Rocchietto S, Allieta R, Morino M. Robot-assisted gastrojejunal anastomosis does not improve the results of the laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2011;25:597–603. doi: 10.1007/s00464-010-1229-1. [DOI] [PubMed] [Google Scholar]
- 27.Hagen ME, Pugin F, Chassot G, Huber O, Buchs N, Iranmanesh P, et al. Reducing cost of surgery by avoiding complications: The model of robotic Roux-en-Y gastric bypass. Obes Surg. 2012;22:52–61. doi: 10.1007/s11695-011-0422-1. [DOI] [PubMed] [Google Scholar]
- 28.Benizri EI, Renaud M, Reibel N, Germain A, Ziegler O, Zarnegar R, et al. Perioperative outcomes after totally robotic gastric bypass: A prospective nonrandomized controlled study. Am J Surg. 2013;206:145–51. doi: 10.1016/j.amjsurg.2012.07.049. [DOI] [PubMed] [Google Scholar]
- 29.Myers SR, McGuirl J, Wang J. Robot-assisted versus laparoscopic gastric bypass: Comparison of short-term outcomes. Obes Surg. 2013;23:467–73. doi: 10.1007/s11695-012-0848-0. [DOI] [PubMed] [Google Scholar]
- 30.Buchs NC, Morel P, Azagury DE, Jung M, Chassot G, Huber O, et al. Laparoscopic versus robotic Roux-en-Y gastric bypass: Lessons and long-term follow-up learned from a large prospective monocentric study. Obes Surg. 2014 Jun 26; doi: 10.1007/s11695-014-1335-6. DOI 10. 1007/s11695-014-1335-6. [DOI] [PubMed] [Google Scholar]
- 31.Markar SR, Karthikesalingam AP, Venkat-Ramen V, Kinross J, Ziprin P. Robotic vs. Laparoscopic Roux-en-Y gastric bypass in morbidly obese patients: Systematic review and pooled analysis. Int J Med Robot. 2011;7:393–400. doi: 10.1002/rcs.414. [DOI] [PubMed] [Google Scholar]
- 32.Fourman MM, Saber AA. Robotic bariatric surgery: A systematic review. Surg Obes Relat Dis. 2012;8:483–8. doi: 10.1016/j.soard.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 33.Kim K, Hagen ME, Buffington C. Robotics in advanced gastrointestinal surgery: The bariatric experience. Cancer J. 2013;19:177–82. doi: 10.1097/PPO.0b013e318289dd15. [DOI] [PubMed] [Google Scholar]
- 34.Toro JP, Lin E, Patel AD. Review of robotics in foregut and bariatric surgery. Surg Endosc. 2014 Jun 28; doi: 10.1007/s00464-014-3646-z. DOI 10. 1007/s00464-014-3646-z. [DOI] [PubMed] [Google Scholar]
- 35.Schauer P, Ikramuddin S, Hamad G, Gourash W. The learning curve for laparoscopic Roux-en-Y gastric bypass is 100 cases. Surg Endosc. 2003;17:212–5. doi: 10.1007/s00464-002-8857-z. [DOI] [PubMed] [Google Scholar]
- 36.Oliak D, Ballantyne GH, Weber P, Wasielewski A, Davies RJ, Schmidt HJ. Laparoscopic Roux-en-Y gastric bypass: Defining the learning curve. Surg Endosc. 2003;17:405–8. doi: 10.1007/s00464-002-8820-z. [DOI] [PubMed] [Google Scholar]
- 37.Yu SC, Clapp BL, Lee MJ, Albrecht WC, Scarborough TK, Wilson EB. Robotic assistance provides excellent outcomes during the learning curve for laparoscopic Roux-en-Y gastric bypass: Results from 100 robotic-assisted gastric bypasses. Am J Surg. 2006;192:746–9. doi: 10.1016/j.amjsurg.2006.08.038. [DOI] [PubMed] [Google Scholar]
- 38.Sudan R, Puri V, Sudan D. Robotically assisted biliary pancreatic diversion with a duodenal switch: A new technique. Surg Endosc. 2007;21:729–33. doi: 10.1007/s00464-006-9171-y. [DOI] [PubMed] [Google Scholar]
- 39.Sudan R, Bennett KM, Jacobs DO, Sudan DL. Multifactorial analysis of the learning curve for robot-assisted laparoscopic biliopancreatic diversion with duodenal switch. Ann Surg. 2012;255:940–5. doi: 10.1097/SLA.0b013e31824c1d06. [DOI] [PubMed] [Google Scholar]
- 40.Sudan R, Podolsky E. Totally robot-assisted biliary pancreatic diversion with duodenal switch: Single dock technique and technical outcomes. Surg Endosc. 2014 Jul 2; doi: 10.1007/s00464-014-3653-0. DOI 10. 1007/s00464-014-3653-0. [DOI] [PubMed] [Google Scholar]
- 41.Patel S, Szomstein S, Rosenthal RJ. Reasons and outcomes of reoperative bariatric surgery for failed and complicated procedures (excluding adjustable gastric banding) Obes Surg. 2011;21:1209–19. doi: 10.1007/s11695-010-0234-8. [DOI] [PubMed] [Google Scholar]
- 42.Snyder B, Wilson T, Woodruff V, Wilson E. Robotically assisted revision of bariatric surgeries is safe and effective to achieve further weight loss. World J Surg. 2013;37:2569–73. doi: 10.1007/s00268-013-1968-y. [DOI] [PubMed] [Google Scholar]
- 43.Buchs NC, Pugin F, Azagury DE, Huber O, Chassot G, Morel P. Robotic revisional bariatric surgery: A comparative study with laparoscopic and open surgery. Int J Med Robot. 2014;10:213–7. doi: 10.1002/rcs.1549. [DOI] [PubMed] [Google Scholar]
- 44.Esposito C, El Ghoneimi A, Yamataka A, Rothenberg S, Bailez M, Ferro M, et al. Work-related upper limb musculoskeletal disorders in paediatric laparosco pic surgery. A multicenter survey. J Pediatr Surg. 2013;48:1750–6. doi: 10.1016/j.jpedsurg.2013.01.054. [DOI] [PubMed] [Google Scholar]
- 45.Curet MJ, Curet M, Soloman H, Lui G, Morton JM. Comparison of hospital charges between robotic, laparoscopic stapled, and laparoscopic hand sewn Roux-en-Y gastric bypass. J Robot Surg. 2009;3:75–8. doi: 10.1007/s11701-009-0143-9. [DOI] [PubMed] [Google Scholar]


