Abstract
Klippel-Trenaunay syndrome (KTS) is a cutaneous capillary malformation on a limb in association with soft tissue swelling with or without bony hypertrophy and atypical varicosity. The capillary malformation associated with KTS is port wine stain. Angiokeratoma circumscriptum naeviforme (ACN) is a congenital variant of angiokeratoma commonly present on the lower limb as a hyperkeratotic plaque. ACN is rarely associated with KTS. We report a case of ACN with soft tissue hypertrophy and deep venous malformation (possibly a variant of Klippel-Trenaunay) in a 4-year-old male child.
Keywords: Angiokeratoma circumscriptum neviforme, Klippel-Trenaunay syndrome, deep venous malformation
INTRODUCTION
Klippel-Trenaunay syndrome (KTS) is characterized by the triad of port wine stain, venous and lymphatic malformation, and soft tissue hypertrophy of the affected extremity. Depending on the type of vessel involved and its flow characteristics KTS is classified as a slow flow complex combined capillary venous or capillary venous lymphatic malformation.[1] Angiokeratomas are cutaneous vascular hyperkeratotic lesions. The current classification of angiokeratomas distinguishes between localized and systemic forms. The localized variants are solitary angiokeratoma, Fordyce's angiokeratoma, angiokeratoma of Mibelli and angiokeratoma circumscriptum naeviforme (ACN).[2] The systemic form, angiokeratoma corporis diffusum, is usually associated with an inborn error of metabolism. Among all the types, ACN is the rarer and the only congenital variant of angiokeratoma.[2] The lesions of ACN are bluish red, well defined and are classically seen on the lower extremity in a unilateral distribution.[3] ACN has been rarely reported in association with KTS.[2,3]
CASE REPORT
A 4-year-old male child presented with complaints of a linear eruption on his right leg since birth. His parents gave history of pain and several episodes of bleeding from the lesion after trauma. There were no symptoms suggestive of bleeding from other sites. On examination, there were multiple hyperkeratotic discrete and closely aggregated papules and plaques of varying size on an erythematous base arranged linearly along the lateral aspect of the right thigh extending up to the knee joint [Figures 1 and 2]. Confluent verrucous plaques were present at the knee joint. The lesions did not blanch on diascopy. There was no bruit over the skin lesions. The circumference of right thigh was greater than that of the left. Prominent superficial veins were seen on dorsum of right leg [Figure 3]. X-ray right thigh showed soft tissue hypertrophy [Figure 4]. Right lower limb arteriovenous (AV) Doppler revealed a hypoplastic right lower limb deep venous system with compensatory dilatation of the superficial venous system. Magnetic resonance imaging (MRI) angiography of both lower limbs was performed. It revealed a normal arterial system on either side. The superficial femoral vein, popliteal vein, anterior tibial and posterior tibial vein on right side were hypoplastic along with thickening of subcutaneous tissue and associated dilatation and malformation of the superficial venous system [Figures 5 and 6]. The deep venous system of the left lower limb was normal in caliber. Histological examination revealed numerous dilated thin walled, congested capillaries mainly in the papillary dermis and very few in reticular dermis. Overlying epidermis showed compact hyperkeratosis, irregular acanthosis with elongated rete ridges consistent with diagnosis of angiokeratoma [Figures 7 and 8]. On the basis of clinical, histological and radiological findings, a diagnosis of KTS with ACN was made.
Figure 1.

Dilated superficial venous system
Figure 2.

Verrucous plaque with soft tissue hypertrophy
Figure 3.

Prominent superficial veins on dorsum of foot
Figure 4.

Plain radiograph showing soft tissue hypertrophy
Figure 5.
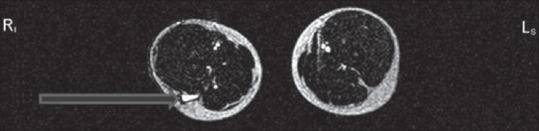
Magnetic resonance imaging angiography showing dilated superficial veins on the right side
Figure 6.
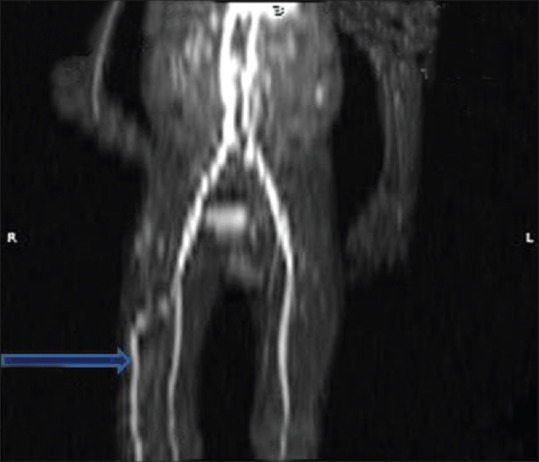
Dilated superficial venous system
Figure 7.
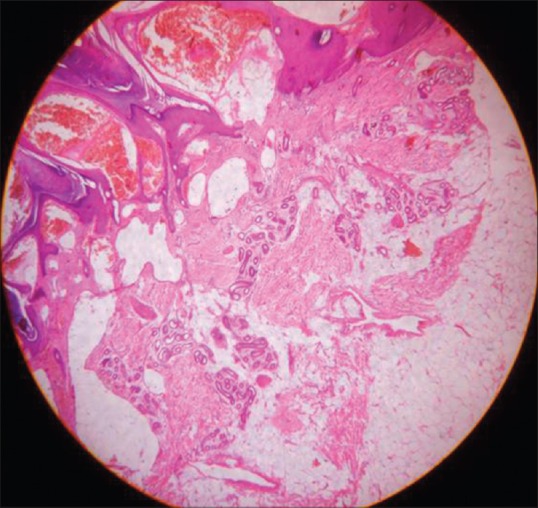
Hyperkeratotic epidermis with congested capillaries in papillary dermis with normal deep dermis and subcutaneous tissue
Figure 8.
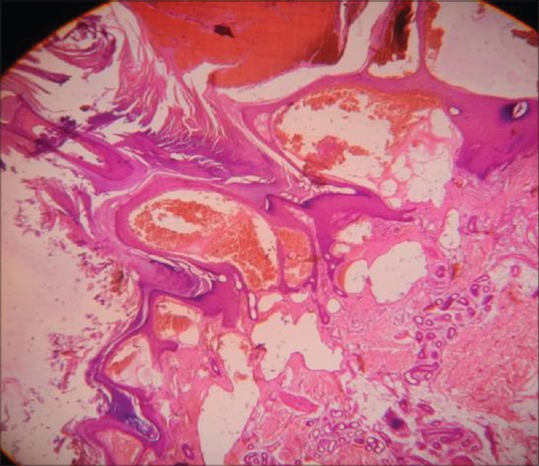
Hyperkeratotic epidermis with dilated congested capillaries in papillary dermis
DISCUSSION
In 1900, two French physicians Maurice Klippel and Paul Trenaunay described two patients with hemangiomatous lesions of the skin with associated bone and soft tissue hypertrophy and coined the term naevus variqueux osteohypertrophique.[4] In 1907, Parkes Weber reported the association of KTS with AV fistula and called it hemangiectatic hypertrophy.[5] In 1965, Lindenauer proposed that the syndrome originally described by Klippel and Trenaunay without AV malformation be considered as a specific entity the KTS and the one associated with AV fistula be designated as Parkes Weber syndrome.[5] In a study of 252 patients with KTS at the Mayo Clinic, 63% had all three features of KTS. Port wine stains were found in 98% of patients, venous malformations in 72% and limb hypertrophy in 67% patients.[6] Two of the three features were noted in 37% of patients. The port wine stain is apparent at birth and usually involves the affected limb, often stopping at the midline with a sharp linear border.[3] The nevus may involve the whole of one side of the body and may sometimes be present on the contralateral limb.[7] A forme fruste presentation of KTS without the cutaneous nevus has also been described.[8] Varicose veins may be obvious at birth, but frequently become evident after walking starts.[9] The venous abnormalities of the deep venous system that occur in KTS include aneurysmal dilatation, duplication, aplasia, and hypoplasia.[10] Popliteal and femoral vein are the most commonly affected veins. Patients with at least two of the three cardinal features have been classified as having an incomplete form of KTS.[4]
Fabry described the first case of angiokeratoma circumscriptum in 1915.[11] The term ACN was proposed by Dammert.[12] It is the only congenital variant and is more common in women and is usually unassociated with systemic disease.[13] The lesions are classically seen on lower extremity in a unilateral distribution. The lesions are well defined confluent keratotic papules that become verrucous with age. They bleed on trauma and spontaneous resolution does not occur. The histopathological finding is same irrespective of the type of angiokeratoma and consist of numerous thin walled congested capillaries mainly in the papillary dermis underlying an epidermis that shows variable degree of acanthosis with elongation of rete ridges and hyperkeratosis.[14] Unusual variants of ACN described in literature are along the lines of Blaschko,[15] and a systematized band like pattern.[16] Rare associations are KTS and Cobbs syndrome. Verrucous hemangioma clinically resembles angiokeratoma but they can be differentiated histopathologically as the former involves the dermis and the subcutaneous fat and the latter involves only the dermis.[17] Our case showed typical clinical features of ACN, which was confirmed by histopathologic examination. The absence of involvement of the deep dermis differentiated it from verrucous hemangioma. Associated soft tissue hypertrophy and deep venous malformation on MRI are classical features of KTS. There are very few case reports of association of KTS with ACN in world literature.[18,19] Schimpf and Wehberg in their study have reported three cases of ACN on the lower limb associated with soft tissue hypertrophy.[19] Bone hypertrophy was present in two cases, varicose veins in one case and only one case had associated port wine stain on the back. The case reported by Odeh had ACN of the right leg associated with soft tissue hypertrophy and bone hypoplasia of the right half of pelvis.[18] Varicose veins and portwine stain were absent. Somasundaram et al. described a case of angiokeratoma associated with soft tissue hypertrophy. They preferred the term hemangiectatic hypertrophy as there was no associated bony and venous abnormalities of KTS.[20] To the best of our knowledge, this is the first case report of this rare association from India.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Moss C, Shahdulla H. Naevi and other developmental defects. In: Burn T, Breathnach S, Cox N, editors. Rooks Text Book of Dermatology. 8th ed. UK: Wiley Blackwell; 2010. pp. 18–60. [Google Scholar]
- 2.Amladi S. Nevi and other developmental defects. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3rd ed. India: Bhalani Publishing House; 2008. p. 206. [Google Scholar]
- 3.James JD, Berger TG, Elston DM. Dermal and subcutaneous tumours. In: James JD, Berger TG, Elston DM, editors. Andrews Diseases of the Skin. Clinical Dermatology. 11th ed. Philadelphia: Saunders Elsevier; 2011. pp. 576–8. [Google Scholar]
- 4.Zea MI, Hanif M, Habib M, Ansari A. Klippel-Trenaunay syndrome: A case report with brief review of literature. J Dermatol Case Rep. 2009;3:56–9. doi: 10.3315/jdcr.2009.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindenauer SM. The Klippel-Trenaunay syndrome: Varicosity, hypertrophy and hemangioma with no arteriovenous fistula. Ann Surg. 1965;162:303–14. doi: 10.1097/00000658-196508000-00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacob AG, Driscoll DJ, Shaughnessy WJ, Stanson AW, Clay RP, Gloviczki P. Klippel-Trénaunay syndrome: Spectrum and management. Mayo Clin Proc. 1998;73:28–36. doi: 10.1016/S0025-6196(11)63615-X. [DOI] [PubMed] [Google Scholar]
- 7.Baskerville PA, Ackroyd JS, Lea Thomas M, Browse NL. The Klippel-Trenaunay syndrome: Clinical, radiological and haemodynamic features and management. Br J Surg. 1985;72:232–6. doi: 10.1002/bjs.1800720331. [DOI] [PubMed] [Google Scholar]
- 8.Jolobe OM. Klippel-Trenaunay syndrome. Postgrad Med J. 1996;72:347–8. doi: 10.1136/pgmj.72.848.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Viljoen DL. Klippel-Trenaunay-Weber syndrome (angio-osteohypertrophy syndrome) J Med Genet. 1988;25:250–2. doi: 10.1136/jmg.25.4.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mavili E, Ozturk M, Akcali Y, Donmez H, Yikilmaz A, Tokmak TT, et al. Direct CT venography for evaluation of the lower extremity venous anomalies of Klippel-Trenaunay syndrome. AJR Am J Roentgenol. 2009;192:W311–6. doi: 10.2214/AJR.08.1151. [DOI] [PubMed] [Google Scholar]
- 11.Bruce DH. Angiokeratoma circumscriptum and angiokeratoma scroti. Report of a case. Arch Dermatol. 1960;81:388–93. doi: 10.1001/archderm.1960.03730030046007. [DOI] [PubMed] [Google Scholar]
- 12.Mittal R, Aggarwal A, Srivastava G. Angiokeratoma circumscriptum: A case report and review of the literature. Int J Dermatol. 2005;44:1031–4. doi: 10.1111/j.1365-4632.2005.02252.x. [DOI] [PubMed] [Google Scholar]
- 13.Lynch PJ, Kosanovich M. Angiokeratoma circumscriptum. Arch Dermatol. 1967;96:665–8. [PubMed] [Google Scholar]
- 14.Elder DE. In: Lever's Histopathology of the Skin. 10th ed. Rosalie E, Johnson BL, Murphy GF, editors. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 1011. [Google Scholar]
- 15.Ghorpade A. Naevoid blaschkoid red-blue lesions in an Indian boy. Angiokeratoma corporis naeviforme along the lines of Blaschko. Clin Exp Dermatol. 2010;35:e79–80. doi: 10.1111/j.1365-2230.2009.03512.x. [DOI] [PubMed] [Google Scholar]
- 16.Bechara FG, Happle R, Altmeyer P, Grabbe S, Jansen T. Angiokeratoma circumscriptum arranged in a systematized band-like pattern suggesting mosaicism. J Dermatol. 2006;33:489–91. doi: 10.1111/j.1346-8138.2006.00115.x. [DOI] [PubMed] [Google Scholar]
- 17.Pavithra S, Mallya H, Kini H, Pai GS. Verrucous hemangioma or angiokeratoma? A missed diagnosis. Indian J Dermatol. 2011;56:599–600. doi: 10.4103/0019-5154.87171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Odeh F. Angiokeratoma corporis circumscriptum naeviforme associated with angiodysplasia (Klippel-Trenaunay-Weber syndrome) Z Hautkr. 1979;54:701–6. [PubMed] [Google Scholar]
- 19.Schimpf A, Wehberg H. Angiokeratoma naeviforme. Relations to Klippel-Trenaunay-Weber syndrome. Z Haut Geschlechtskr. 1969;44:905–13. [PubMed] [Google Scholar]
- 20.Somasundaram V, Premalatha S, Rao NR, Razack EM, Zahra A. Hemangiectatic hypertrophy with angiokeratoma circumscriptum. Int J Dermatol. 1988;27:45–6. doi: 10.1111/j.1365-4362.1988.tb02337.x. [DOI] [PubMed] [Google Scholar]


