Abstract
Lichen planus pemphigoides (LPP) is a rare autoimmune bullous disorder that is rarer in children characterized by bullae on lichen planus like papules and the normal looking skin. Clinical, histopathological and direct immunoflourescence evaluation is important for the diagnosis of this entity. We report a case of LPP in a 5-year-old girl child probably triggered by an episode of preceding varicella. Diagnosis was confirmed by histopathology and immunofluorescence examination. Histological findings were typical of lichen planus from the biopsy taken from a violaceous to erythematous papule and characteristic of bullous pemphigoid in the biopsy taken from a bullous lesion with evidence of immunoglobulin G and C3 deposition along the basement membrane zone on direct immunofluorescence.
Keywords: Bullous pemphigoid, childhood lichen planus pemphigoides, lichen planus, varicella
INTRODUCTION
Lichen planus pemphigoides (LPP), an extremely rare entity in children is a controversial disease characterized by the coexistence of lichen planus and tense bullae, in which the bullae may occur on both clinically normal skin as well as the pre-existing lichen planus papules.[1] The lesions are histologically characterized by a subepidermal split along with features of classical lichen planus. Linear deposits of immunoglobulin G and C3 along the basement membrane zone (BMZ) are noted on immunofluorescence of peribullous skin. Males are more commonly affected and the incidence is more in the third and fourth decades. The disease may run a protracted course, requiring systemic corticosteroids.
CASE REPORT
A 5-year-old female child presented with two months history of tense fluid filled lesions. Two weeks prior to appearance of these lesions, she had dark coloured, scaly, itchy skin lesions over her trunk and extremities. Fluid filled lesions appeared on normal skin as well as over the pre-existing scaly lesions. She recently had an episode of chickenpox one month prior to the scaly skin lesions. Physical examination revealed multiple erythematous-to-violaceous papules and plaques varying in size from 0.3 mm to 5 cm distributed over the trunk and the extremities [Figures 1 and 2]. Multiple tense bullae are distributed predominantly over the upper and lower extremities, a few of them hemorrhagic. Hyperkeratotic plaques with fissures were present over the central aspects of both the palms and soles in addition to a few deep-seated vesicular lesions [Figure 3]. There was no oral involvement.
Figure 1.

Multiple erythematous to violaceous papules, plaques and tense bullae over both normal skin and violaceous lesions distributed on the trunk
Figure 2.

Violaceous papules, plaques and tense hemorrhagic bullae over the extremities
Figure 3.

Hyperkeratotic plaques with fissures over the central aspects of both the palms and soles in addition to few deep seated vesicular lesions
Skin biopsies were taken from two sites: one from an intact bulla and the second from an erythematous papule. Histopathology of the bullous lesion revealed orthokeratosis, hypergranulosis, acanthosis, and subepidermal bulla with no acantholytic cells [Figure 4a]. Adjacent basal cells showed liquefactive degeneration with scattered mixed inflammatory infiltrate of lymphocytes and occasional plasma cells in the upper dermis [Figure 4b]. Apoptotic keratinocytes or civatte bodies were scattered in the epidermis [Figure 5]. Biopsy from the papule revealed hyperkeratosis, hypergranulosis, acanthosis with pointed rete ridges, focal basal cell degeneration, melanin incontinence, perivascular and periappendageal inflammatory infiltrate of eosinophils, neutrophils and mononuclear cells. Direct immunoflourescence of biopsy drawn from peribullous skin revealed immunoglobulin G (IgG) and C3c deposition at BMZ and C3c deposition at appendages and vessel walls consistent with the diagnosis of LPP. Routine hemogram, urinalysis and chest X-ray are within normal limits.
Figure 4.
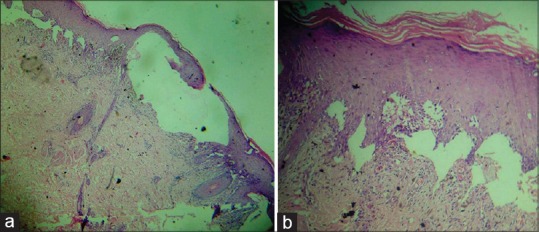
(a) Biopsy from the bullous lesion revealing orthokeratosis, hypergranulosis, acanthosis, subepidermal bullae with no acantholytic cells (b) Epidermis adjacent to the bulla showing basal cells liquefactive degeneration with scattered mixed inflammatory infiltrate of lymphocytes and occasional plasma cells in the upper dermis
Figure 5.
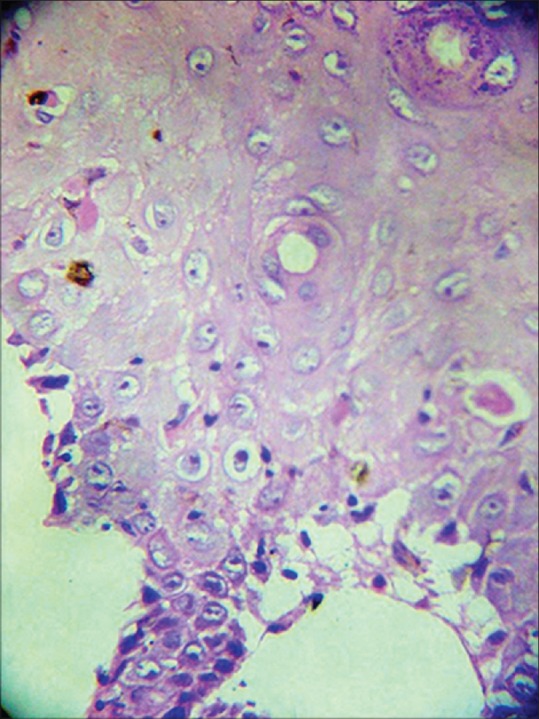
Apoptotic keratinocytes or civatte bodies scattered in the epidermis with liquefactive degeneration of the basal layer
The patient was treated with oral prednisolone 20 mg daily and showed significant clinical improvement within a span of 10 days. She is currently on maintenance dose of prednisolone and follow up.
DISCUSSION
LPP has been a controversial entity since 1892 when Kaposi first coined the term “lichen ruber pemphigoides” to describe a case of typical lichen planus complicated by widespread bullous eruption.[2] It is a rare immunobullous disorder characterized by evolution of vesiculobullous skin lesions in patients with active lichen planus. LPP usually affects adults and is extremely uncommon in children.
The exact etiology is unknown but some authors consider LPP as a heterogeneous group of subepidermal autoimmune blistering disorders occurring in association with lichen planus. Many cases of LPP in the literature have demonstrated IgG autoantibodies to either one or both the 180 kD bullous pemphigoid antigen (BPAg2, type-XVII collagen) and the 230 kD pemphigoid antigens (BPAg1).[3,4,5]
A recent review of the literature on pediatric LPP revealed the mean age of onset of childhood LPP to be 12 years with a male to female ratio of 3:1 and a mean time lag between lichen planus and the development of LPP to be 7.9 weeks.[6] Vesiculobullous lesions are common on the extremities with palmoplantar involvement seen in about 50% cases.[6] Case reports of childhood LPP being triggered by viral exanthems such as varicella have been reported[7] as in our case where an episode of varicella preceded bullous lesions by 45 days. The concept of “epitope spreading” explains the development of autoimmune skin disorders[8] where a primary autoimmune or inflammatory process may cause tissue damage which causes the release and exposure of a previously “sequestered” antigen, leading to a secondary autoimmune response against the newly released antigen. The combination of basal cell injuries caused by the lichenoid process together with varicella may have exposed BMZ components, triggering the secondary development of autoantibodies. Histologically, LPP is characterized by features of both classical lichen planus and subepidermal bullae. Direct and indirect immunofluorescence features of childhood LPP are similar to those in adults. Linear deposits of IgG and C3 along the BMZ characterize the direct immunofluorescence of peribullous skin.[9,10] Topical corticosteroids, oral dapsone or oral corticosteroids cause resolution of LPP[6] We report this case in view of the rare association of LPP with a preceding episode of varicella infection, indicating the heterogeneous nature of the disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Davis AL, Bhogal BS, Whitehead P, Frith P, Murdoch ME, Leigh IM, et al. Lichen planus pemphigoides: Its relationship to bullous pemphigoid. Br J Dermatol. 1991;125:263–71. doi: 10.1111/j.1365-2133.1991.tb14753.x. [DOI] [PubMed] [Google Scholar]
- 2.Kaposi M. Lichen ruber pemphigoides. Arch Derm Syphilol (Berlin) 1892;24:343–6. [Google Scholar]
- 3.Demirçay Z, Baykal C, Demirkesen C. Lichen planus pemphigoides: Report of two cases. Int J Dermatol. 2001;40:757–9. doi: 10.1046/j.1365-4362.2001.01334.x. [DOI] [PubMed] [Google Scholar]
- 4.Sakuma-Oyama Y, Powell AM, Albert S, Oyama N, Bhogal BS, Black MM. Lichen planus pemphigoides evolving into pemphigoid nodularis. Clin Exp Dermatol. 2003;28:613–6. doi: 10.1046/j.1365-2230.2003.01401.x. [DOI] [PubMed] [Google Scholar]
- 5.Hsu S, Ghohestani RF, Uitto J. Lichen planus pemphigoides with IgG autoantibodies to the 180 kd bullous pemphigoid antigen (type XVII collagen) J Am Acad Dermatol. 2000;42:136–41. doi: 10.1016/s0190-9622(00)90024-0. [DOI] [PubMed] [Google Scholar]
- 6.Cohen DM, Ben-Amitai D, Feinmesser M, Zvulunov A. Childhood lichen planus pemphigoides: A case report and review of the literature. Pediatr Dermatol. 2009;26:569–74. doi: 10.1111/j.1525-1470.2009.00988.x. [DOI] [PubMed] [Google Scholar]
- 7.İlknur T, Akarsu S, Uzun S, Özer E, Fetil E. Heterogeneous disease: A child case of lichen planus pemphigoides triggered by varicella. J Dermatol. 2011;38:707–10. doi: 10.1111/j.1346-8138.2011.01220.x. [DOI] [PubMed] [Google Scholar]
- 8.Chan LS, Vanderlugt CJ, Hashimoto T, Nishikawa T, Zone JJ, Black MM, et al. Epitope spreading: Lessons from autoimmune skin diseases. J Invest Dermatol. 1998;110:103–9. doi: 10.1046/j.1523-1747.1998.00107.x. [DOI] [PubMed] [Google Scholar]
- 9.Mora RG, Nesbitt LT, Jr, Brantley JB. Lichen planus pemphigoides: Clinical and immunofluorescent findings in four cases. J Am Acad Dermatol. 1983;8:331–6. doi: 10.1016/s0190-9622(83)70035-6. [DOI] [PubMed] [Google Scholar]
- 10.Gawkrodger DJ, Stavropoulos PG, McLaren KM, Buxton PK. Bullous lichen planus and lichen planus pemphigoides – Clinico-pathological comparisons. Clin Exp Dermatol. 1989;14:150–3. doi: 10.1111/j.1365-2230.1989.tb00914.x. [DOI] [PubMed] [Google Scholar]


