Abstract
Purpose.
To assess longitudinal change in refractive, keratometric, and internal astigmatism in a sample of students from a population with a high prevalence of with-the-rule (WTR) astigmatism and to determine the optical origins of changes in refractive astigmatism.
Methods.
A retrospective analysis of longitudinal measurements of right eye refractive and keratometric astigmatism in Tohono O'odham Native American children was conducted. Changes in refractive and keratometric astigmatism per year were compared in a younger cohort (n = 1594, 3 to <11 years old) and an older cohort (n = 648, 11 to <19 years old). Data were analyzed in clinical notation (Cyl) and vector notation (J0, J45).
Results.
On average, refractive astigmatism (means: 1.19 diopters [D] Cyl, +0.54 J0, +0.03 J45) resulted primarily from WTR corneal astigmatism (means: +0.85 J0, −0.02 J45) and against-the-rule (ATR) internal astigmatism (means: −0.31 J0, +0.05 J45). Mean longitudinal changes in astigmatism were statistically significant (younger cohort −0.02 D/y Cyl; older cohort +0.06 D/y Cyl). In the younger cohort, astigmatism decreased with age in low and moderate astigmats (<3.00 D) and increased with age in high astigmats (≥3.00 D). In the older cohort, astigmatism increased with age across all levels of astigmatism. Longitudinal changes in keratometric and internal astigmatism were negatively correlated in both cohorts.
Conclusions.
Cross-sectional data suggest the presence of a constant ATR contribution from internal astigmatism (0.60 D Cyl) that is close to the 0.50 D ATR constant reported by Javal and others. Highly astigmatic 3- to <11-year-old children and children older than age 11 years show a small (not clinically significant) increase in astigmatism with age. A negative correlation between changes in keratometric astigmatism and internal astigmatism suggests an active compensation that may contribute to the stability of astigmatism in Tohono O'odham children.
Keywords: astigmatism, refractive error development, children, Native American
Native American children from a tribe with a high prevalence of astigmatism show little change in astigmatism with age. Longitudinal data suggest that internal compensation for keratometric astigmatism may contribute to the stability of astigmatism in Tohono O'odham children.
Introduction
Research conducted over the past 15 years has yielded a large longitudinal database on refractive development in Tohono O'odham children. There is a high prevalence of astigmatism among elementary school children who are members of this Native American tribe.1–4 The high prevalence of refractive astigmatism in Tohono O'odham children is present in infancy and persists at least through elementary school.1,2,4–7 A longitudinal study of corneal astigmatism in 960 Tohono O'odham children aged 6 months through 7 years showed that in early development (6 months to <3 years), astigmatism decreased in children with high astigmatism (−0.37 diopters [D]/y) and remained stable in children with little or no astigmatism (+0.05 D/y).7 From age 3 through 7 years, astigmatism decreased in children with both high astigmatism (−0.11 D/y) and low/no astigmatism (−0.03 D/y).7 A detailed account of changes in astigmatism beyond age 7 years in this population has not yet been reported. However, a recent report on change in spherical equivalent (M) in a longitudinal sample of Tohono O'odham students ages 3 to 18 years showed that rate of change in M with age was significantly greater for children who were hyperopic (M ≥ +2.00) prior to age 5.5 years, consistent with continued emmetropization into the school years. In addition, higher levels of refractive astigmatism were associated with predicted myopia onset (M ≤ −0.75 D) by age 18 years.8
Astigmatism in Tohono O'odham children arises primarily from the cornea and is almost always with-the-rule (WTR, plus cylinder axis at or near 90°; Ref. 9 and Twelker JD, et al. IOVS 2013;53:ARVO E-Abstract 5962). In Tohono O'odham preschool children, magnitude of refractive (total) astigmatism tends to be less than that of keratometric astigmatism due to approximately 0.75 D against-the-rule (ATR) internal astigmatism.9 This relation, specifically the relation between keratometric and refractive (total) astigmatism, was originally described by Javal in 189010,11: Refractive Astigmatism = 1.25(Keratometric Astigmatism) − 0.50 D × 90.
A more recent empirically based modification of Javal's rule suggests that WTR and ATR refractive astigmatism can be predicted by subtracting an ATR constant (0.50 D) from the magnitude of keratometric astigmatism, with little or no adjustment based on magnitude of keratometric astigmatism.10
Little is known about how the relation between keratometric and internal astigmatism changes with development in childhood. For example, it is not known if magnitude of ATR internal astigmatism remains constant with age or if it is correlated with changes in keratometric astigmatism. A finding that the magnitude of ATR internal astigmatism increases with increasing WTR keratometric astigmatism, or decreases with decreasing keratometric astigmatism, could reflect an active process of compensation and explain why refractive astigmatism tends to remain stable in Tohono O'odham children, as well as other populations of children.12–14 Many studies have noted a “compensation” of corneal astigmatism by internal astigmatism, and a similar observation has been reported for other aberrations.11,15–21 A finding that changes in magnitude of ATR internal astigmatism are not correlated with changes in keratometric astigmatism would suggest that the “compensation” observed in Tohono O'odham preschoolers is reflective of a passive compensation resulting from a constant amount of internal ATR astigmatism that, in this population of predominantly WTR astigmats, results in a reduction in the total astigmatism.
In the present study, we used a large longitudinal database on refractive development in Tohono O'odham children to retrospectively describe change in refractive astigmatism and its components (keratometric and internal astigmatism) in Tohono O'odham children from age 3 to <19 years. These data extend our previous longitudinal reports on astigmatism in this population to a much larger age range, allowing us to compare results in younger and older school-age children.7 In addition, we extend our previous cross-sectional analysis of the relation between refractive astigmatism and its components (keratometric and internal astigmatism) in preschoolers to a larger age range and to a longitudinal sample,9 allowing us to assess the hypothesis that change in internal astigmatism may be negatively correlated with change in amount of keratometric astigmatism, resulting in stable levels of refractive astigmatism with age.
Methods
Subjects
Subjects were participants in longitudinal studies of visual development in Tohono O'odham children. Informed consent was obtained from a parent or guardian or from the subject (if age 18). Assent was obtained from subjects once they reached first grade. This research followed the tenets of the Declaration of Helsinki and was approved by the Tohono O'odham Nation and the University of Arizona Institutional Review Board. This study was conducted in a manner compliant with the Health Insurance Portability and Accountability Act.
Procedures
Data were collected as part of a series of studies of Tohono O'odham children (conducted from 1997–2012) and were analyzed retrospectively. In each study, after a baseline exam, follow-up exams were attempted at least yearly until the end of the study or until subjects reached the oldest grade of eligibility for a given study. At each study encounter (exam), cycloplegic eye examination and autorefraction were conducted. Cycloplegia was accomplished through one of three protocols: proparacaine 0.5%, 2% cyclopentolate, and 1% cyclopentolate; proparacaine 0.5%, two drops of 1% cyclopentolate; proparacaine 0.5%, 1% tropicamide, 1% cyclopentolate. At least 30 minutes after administering eye drops, autorefraction and keratometry were conducted with a handheld Retinomax Autorefractor (KPlus or KPlus2 model; Nikon, Inc., Tokyo, Japan). The Retinomax was used in plus cylinder notation, regular (rather than quick) measurement mode. The validity and reproducibility of Retinomax measurements in this population have previously been reported.22
Data Analysis and Prediction
Data from encounters were included in analyses if the subject was age 3 to <19 years on the date of encounter and right eye cycloplegic Retinomax autorefraction with a confidence of 8 or higher was obtained.23
To determine if any clinically relevant developmental changes occur early or later in childhood, we divided our sample into two cohorts that each covered an 8-year age range (roughly corresponding to preschool/grade school and middle/high school), with the age cutoff occurring at the estimated age of onset of myopia (M ≤ −0.75) for children in this cohort (10.52 years).8 Analyses were conducted on three groups of subjects: (1) the full dataset (subjects with ≥2 encounters and ≥1 year of follow-up between 3 and <19 years of age); (2) a younger cohort (subjects with ≥2 encounters and ≥1 year of follow-up between 3 and <11 years of age); and (3) an older cohort (subjects with ≥2 encounters and ≥1 year of follow-up between 11 and <19 years of age). All subjects in the younger and older cohorts were also represented in the full dataset.
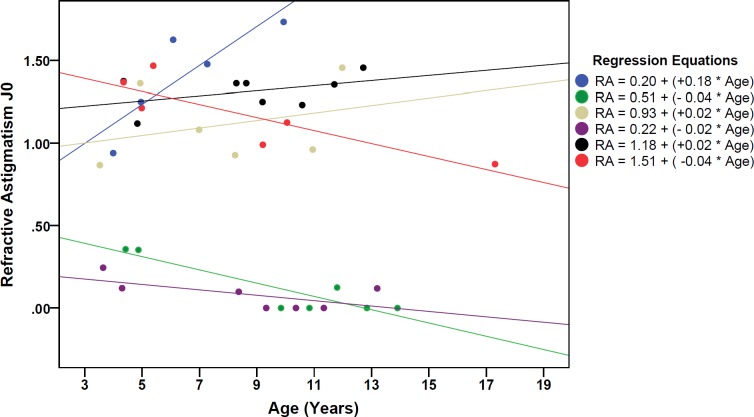
Right eye measurements of refractive astigmatism, keratometric astigmatism, internal astigmatism (calculated as refractive astigmatism − keratometric astigmatism), and spherical equivalent (M) were included in analyses. Astigmatism data were analyzed in clinical notation (Cyl, representing magnitude of astigmatism without regard to axis) and in vector notation (J0 [Jackson cross-cylinder with axes at 180° and 90°] and J45 [Jackson cross-cylinder with axes at 45° and 135°]).24 Inclusion of J0 and J45 allowed for analysis of astigmatism while taking into account axis. Positive J0 values represent WTR astigmatism (90° in plus cylinder notation); negative J0 values represent ATR astigmatism (180° in plus cylinder notation). Positive J45 values represent astigmatism at axis 135° in plus cylinder notation, and negative J45 values represent astigmatism at axis 45° in plus cylinder notation. For each subject, and for each of these measures, a regression line was fitted, and slopes (representing estimated change per year, D) were calculated using the subject's longitudinal data (see Fig. 1). Slopes were used in analyses examining longitudinal change in astigmatism. Only summary analyses of M data are provided, as a previous report includes detailed analysis and interpretation of longitudinal change in M for this sample.8
Figure 1.
Examples of raw J0 data from six subjects. To estimate change in astigmatism with age, individual regression equations were generated based on each subject's longitudinal data. Slope values represent change per year. Analyses of longitudinal change in refractive error were conducted using slope values from each subject's regression data for each component of refractive error (refractive astigmatism, keratometric astigmatism, internal astigmatism, spherical equivalent). RA in regression equations represents refractive astigmatism.
Analysis of Longitudinal Change in Astigmatism.
T-tests were conducted on the full, younger, and older cohorts to determine if mean slope (change/y, D) was significantly different from 0 for each measure of astigmatism (refractive, keratometric, and internal astigmatism measurements of Cyl, J0, and J45). Multivariate analysis of covariance (ANCOVA) was used on the full dataset to determine if slopes for measures of astigmatism differed by magnitude of baseline refractive astigmatism (Cyl, low/no astigmatism [0 to <1.00 D], moderate astigmatism [1 to <3.00 D], or high astigmatism [≥3.00 D]). A second ANCOVA was used to determine if slopes for measures of astigmatism differed across cohort (younger compared to older) and/or magnitude of baseline refractive astigmatism. Years of follow-up and number of observations were included in ANCOVAs as covariates.
Analysis of the Relation Between Keratometric Astigmatism and Internal Astigmatism.
Baseline J0 and J45 data were examined to determine if internal astigmatism showed a compensatory relation with keratometric astigmatism. Positive J0 values represent WTR astigmatism; negative J0 values represent ATR astigmatism; and a difference in sign (plus versus minus) between keratometric and internal astigmatism J0 values indicates that axes are orthogonal in the horizontal/vertical meridian. Similarly, positive J45 values represent astigmatism at axis 135° in plus cylinder notation; negative J45 values represent astigmatism at axis 45° in plus cylinder notation; and a difference in sign between keratometric and internal astigmatism J45 values indicates that axes are orthogonal in the oblique meridian. Correlation analyses were conducted on baseline keratometric and internal astigmatism data to determine if the magnitude of internal astigmatism was dependent upon magnitude of keratometric astigmatism.
Regression coefficients for prediction of refractive astigmatism (dependent variable) from keratometric astigmatism (independent variable) were calculated. The constant and slope represent the influence of internal astigmatism. A regression constant significantly different from 0 would reflect a constant contribution from internal astigmatism, and a slope significantly different from 1 would indicate that the contribution from internal astigmatism is dependent upon amount of keratometric astigmatism. Analyses were conducted on the full, younger, and older cohorts including all subjects and on subsets of subjects with significant WTR astigmatism (J0 ≥ +0.50).
Analysis of the Relation Between Change in Keratometric Astigmatism and Change in Internal Astigmatism With Age.
Correlation analyses on keratometric astigmatism slope (D/y) and internal astigmatism slope (D/y) for the full, younger, and older cohorts were conducted on J0 and J45 data. A positive correlation would indicate that changes in keratometric and internal astigmatism occur in the same direction (both increasing or both decreasing). A significant negative correlation would indicate that changes in keratometric astigmatism occur in conjunction with compensatory changes in internal astigmatism. For example, keratometric astigmatism may show increasing WTR astigmatism while internal astigmatism shows a reduction in WTR astigmatism or an increase in ATR astigmatism.
Results
The full longitudinal dataset included 2176 subjects (9403 subject encounters). Age at first encounter was 3 to <5, 5 to <7, 7 to <9, 9 to <11, 11 to <13, 13 to <15, and 15 years or older in 1027, 517, 144, 220, 207, 50, and 11 subjects, respectively. The younger cohort included 1594 subjects, and the older cohort included 648 subjects. A sample summary is provided in Table 1. The younger cohort had significantly more years of follow-up and encounters than the older cohort. The younger cohort also had significantly greater magnitude of Cyl and more positive J0 measures of refractive and keratometric astigmatism than the older cohort. The older cohort had significantly more negative J0 for internal astigmatism and J45 keratometric astigmatism and significantly more positive J45 refractive and internal astigmatism than the younger cohort. M significantly differed across cohorts: Mean M was hyperopic in the younger cohort (+0.93 D) and myopic in the older cohort (−0.44 D). Years of follow-up and number of encounters were included as covariates in subsequent ANCOVAs comparing the cohorts.
Table 1.
Summary of Sample Characteristics and Baseline Refractive Error
|
Variable |
Full Dataset |
Younger Cohort |
Older Cohort |
Younger vs. Older Cohort
P
Value |
| N | 2176 | 1594 | 648 | - |
| Mean baseline age (SEM) | 6.35 (0.06) | 4.96 (0.04) | 12.19 (0.05) | - |
| Mean final age (SEM) | 10.68 (0.08) | 8.11 (0.05) | 14.26 (0.06) | - |
| Mean follow-up years (SEM) | 4.33 (0.07) | 3.15 (0.05) | 2.07 (0.06) | 0.000 |
| Mean encounters (SEM) | 3.51 (0.04) | 3.18 (0.03) | 2.61 (0.03) | 0.000 |
| Mean Cyl (SEM) | ||||
| Refractive | +1.19 (0.03) | +1.26 (0.03) | +1.08 (0.06) | 0.002 |
| Keratometric | +1.79 (0.02) | +1.85 (0.03) | +1.71 (0.05) | 0.007 |
| Internal | −0.60 (0.01) | −0.60 (0.01) | −0.64 (0.02) | 0.084 (NS) |
| Mean J0 (SEM) | ||||
| Refractive | +0.54 (0.01) | +0.58 (0.02) | +0.47 (0.03) | 0.000 |
| Keratometric | +0.85 (0.01) | +0.89 (0.01) | +0.82 (0.02) | 0.007 |
| Internal | −0.31 (0.01) | −0.31 (0.01) | −0.35 (0.01) | 0.002 |
| Mean J45 (SEM) | ||||
| Refractive | +0.03 (0.01) | +0.03 (0.01) | +0.05 (0.01) | 0.032 |
| Keratometric | −0.02 (0.01) | −0.01 (0.01) | −0.04 (0.01) | 0.004 |
| Internal | +0.05 (0.00) | +0.04 (0.00) | +0.10 (0.01) | 0.000 |
| Mean baseline M (SEM) | +0.72 (0.03) | +0.93 (0.03) | −0.44 (0.06) | 0.000 |
NS, not significant; SEM, standard error of measurement.
Analysis of Longitudinal Change in Astigmatism
Results of t-tests conducted to determine if mean slopes (estimates of change per year) were significantly different from 0 are provided in Table 2. Analyses yielded the following results:
Table 2.
Mean Slope for Measurements of Refractive Error (Change per Year, D)
|
Variable |
Full Dataset |
Younger Cohort |
Older Cohort |
Younger vs. Older Cohort
P
Value |
| Mean Cyl slope (SEM) | ||||
| Refractive | +0.007 (0.004) | −0.019* (0.005) | +0.064* (0.010) | P < 0.001 |
| Keratometric | −0.000 (0.004) | −0.028* (0.006) | +0.042* (0.008) | P < 0.001 |
| Internal | +0.007 (0.005) | +0.009 (0.006) | +0.022§ (0.010) | NS |
| Mean J0 slope (SEM) | ||||
| Refractive | +0.004 (0.002) | −0.008‡ (0.003) | +0.031* (0.005) | P < 0.001 |
| Keratometric | −0.006† (0.002) | −0.021* (0.003) | +0.019* (0.004) | P < 0.001 |
| Internal | +0.010* (0.002) | +0.013* (0.003) | +0.012† (0.005) | NS |
| Mean J45 slope (SEM) | ||||
| Refractive | +0.002 (0.002) | +0.000 (0.003) | −0.004 (0.004) | NS |
| Keratometric | +0.004 (0.002) | −0.008‡ (0.003) | +0.031* (0.005) | P < 0.001 |
| Internal | +0.011* (0.002) | +0.006† (0.003) | +0.010† (0.004) | NS |
| Baseline M (SEM)* | −0.166* (0.006) | −0.127* (0.008) | −0.245* (0.013) | P < 0.001 |
Bold italic values indicate means that are significantly different from 0 based on t-test analysis.
P < 0.001 for comparison of mean slope to 0.
P < 0.02 for comparison of mean slope to 0.
P < 0.005 for comparison of mean slope to 0.
P < 0.03 for comparison of mean slope to 0.
-
Cyl:
For measurements of Cyl, positive slope represents an increase in astigmatism magnitude with age, and negative slope represents a decrease in astigmatism magnitude with age. Mean slopes for the full dataset did not significantly differ from 0. There was a significant negative slope for younger cohort measurements of refractive (−0.02 D/y) and keratometric astigmatism (−0.03 D/y) and a significant positive slope in older cohort measurements of refractive, keratometric, and internal astigmatism (+0.06, +0.04, and +0.02 D/y; Table 2, bold italic values). The younger and older cohorts differed significantly on mean slope for refractive and keratometric astigmatism;
-
J0:
For measurements of J0, positive slope represents a shift toward increasing WTR astigmatism and/or reduction in ATR astigmatism. There was a significant negative mean slope for keratometric astigmatism (−0.01 D/y) and a significant positive mean slope for internal astigmatism (+0.01 D/y) in the full dataset. The younger cohort had significant negative slopes for refractive (−0.01 D/y) and keratometric astigmatism (−0.02 D/y), and a significant positive slope for internal astigmatism (+0.01 D/y). The older cohort had significant positive slopes for refractive, keratometric, and internal astigmatism (+0.03, +0.02, and +0.01 D/y). The younger and older cohorts differed significantly on mean slope for refractive and keratometric astigmatism;
-
J45:
For measurements of J45, positive slope represents increasing astigmatism at axis 135° and/or reduction in astigmatism at axis 45°. There was a significant positive mean slope for internal astigmatism (+0.01 D/y) in the full dataset. The younger cohort had a significant negative slope for keratometric astigmatism (−0.01 D/y) and a significant positive slope (+0.01 D/y) for internal astigmatism. The older cohort had significant positive slopes for keratometric and internal astigmatism (+0.03 and +0.01 D/y). The younger and older cohorts differed significantly on mean slope for keratometric astigmatism; and
-
M:
There was a significant negative mean slope (shift toward more myopia with age) in the full, younger, and older cohort datasets for measurements of M. Mean slope was significantly more negative in the older cohort (−0.24 D/y) than in the younger cohort (−0.13 D/y).
Relation Between Baseline Astigmatism Magnitude (Cyl) and Longitudinal Change in Astigmatism
Results of the ANCOVA conducted on the full dataset (Table 3, bold italic values represent significant comparisons) yielded statistically significant effects of amount of baseline astigmatism on mean refractive and keratometric astigmatism Cyl and J0 slope and mean keratometric astigmatism J45 slope. Post hoc analyses indicated that mean refractive and keratometric astigmatism Cyl slopes for high astigmats were significantly more positive than for low/nonastigmats and moderate astigmats. Mean refractive and keratometric astigmatism J0 slope and keratometric astigmatism J45 slope were significantly more positive for high astigmats than for moderate astigmats.
Table 3.
Summary of Mean Astigmatism Slope (D/Y) for the Full, Younger, and Older Cohorts by Amount of Baseline Refractive Astigmatism
|
Astigmatism Measurement |
Baseline Refractive Astigmatism, |
Full Dataset |
Younger Cohort |
Older Cohort |
|||
|
D Cyl |
Mean Slope |
SEM |
Mean Slope |
SEM |
Mean Slope |
SEM |
|
| Cyl | |||||||
| Refractive | <1.00 D | 0.008 | 0.005 | −0.022 | 0.006 | 0.063 | 0.011 |
| P < 0.001* | 1.00 to <3.00 D | −0.013 | 0.009 | −0.044 | 0.011 | 0.072 | 0.025 |
| P < 0.003† | ≥3.00 D | 0.046 | 0.014 | 0.065 | 0.017 | 0.057 | 0.033 |
| Keratometric | <1.00 D | −0.004 | 0.005 | −0.039 | 0.006 | 0.044 | 0.009 |
| P < 0.05* | 1.00 to <3.00 D | −0.006 | 0.010 | −0.035 | 0.012 | 0.045 | 0.020 |
| P < 0.02† | ≥3.00 D | 0.030 | 0.010 | 0.039 | 0.013 | 0.028 | 0.027 |
| Internal | <1.00 D | 0.012 | 0.006 | 0.017 | 0.007 | 0.019 | 0.012 |
| NS* | 1.00 to <3.00 D | −0.006 | 0.010 | −0.009 | 0.012 | 0.027 | 0.022 |
| NS† | ≥3.00 D | 0.016 | 0.011 | 0.027 | 0.015 | 0.029 | 0.027 |
| J0 | |||||||
| Refractive | <1.00 D | 0.005 | 0.002 | −0.009 | 0.003 | 0.031 | 0.005 |
| P < 0.007* | 1.00 to <3.00 D | −0.005 | 0.005 | −0.021 | 0.006 | 0.037 | 0.014 |
| P < 0.002† | ≥3.00 D | 0.019 | 0.007 | 0.032 | 0.009 | 0.022 | 0.018 |
| Keratometric | <1.00 D | −0.004 | 0.002 | −0.022 | 0.003 | 0.021 | 0.005 |
| P < 0.006* | 1.00 to <3.00 D | −0.016 | 0.006 | −0.032 | 0.007 | 0.019 | 0.010 |
| P < 0.007† | ≥3.00 D | 0.010 | 0.006 | 0.014 | 0.008 | 0.006 | 0.014 |
| Internal | <1.00 D | 0.009 | 0.003 | 0.013 | 0.003 | 0.009 | 0.006 |
| NS* | 1.00 to <3.00 D | 0.011 | 0.006 | 0.011 | 0.007 | 0.018 | 0.011 |
| NS† | ≥3.00 D | 0.009 | 0.006 | 0.018 | 0.008 | 0.015 | 0.014 |
| J45 | |||||||
| Refractive | <1.00 D | 0 | 0.001 | −0.001 | 0.002 | −0.001 | 0.003 |
| NS* | 1.00 to <3.00 D | 0.002 | 0.004 | 0.002 | 0.005 | −0.016 | 0.010 |
| NS† | ≥3.00 D | 0.011 | 0.010 | −0.001 | 0.014 | 0.001 | 0.020 |
| Keratometric | <1.00 D | 0.005 | 0.002 | −0.009 | 0.003 | 0.031 | 0.005 |
| P < 0.007* | 1.00 to <3.00 D | −0.005 | 0.005 | −0.021 | 0.006 | 0.037 | 0.014 |
| P < 0.002† | ≥3.00 D | 0.019 | 0.007 | 0.032 | 0.009 | 0.022 | 0.018 |
| Internal | <1.00 D | 0.009 | 0.003 | 0.005 | 0.003 | 0.009 | 0.005 |
| NS* | 1.00 to <3.00 D | 0.013 | 0.004 | 0.004 | 0.005 | 0.008 | 0.009 |
| NS† | ≥3.00 D | 0.020 | 0.005 | 0.017 | 0.007 | 0.018 | 0.014 |
Bold italic values indicate significant post hoc comparisons across levels of baseline astigmatism.
For full dataset, P value for main effect of baseline refractive astigmatism Cyl.
For younger and older cohort data, P value for interaction between cohort and baseline refractive astigmatism Cyl.
ANCOVA conducted to determine if mean slope varied by cohort and level of baseline refractive astigmatism (Cyl) yielded significant interactions between cohort and baseline refractive astigmatism for refractive and keratometric astigmatism measurements of Cyl and J0 slope, and measurements of keratometric astigmatism J45 slope (Table 3, bold italic values indicate significant comparisons). Post hoc analyses indicated that for the younger cohort, mean refractive and keratometric astigmatism Cyl and J0 slopes and keratometric astigmatism J45 slope were significantly more positive for high astigmats than for low/nonastigmats and moderate astigmats. For the older cohort there were no significant effects of magnitude of baseline refractive astigmatism on mean slope for any measure of astigmatism.
Analysis of the Relation Between Keratometric Astigmatism and Internal Astigmatism at Baseline
Table 1 shows that for J0, mean internal astigmatism was ATR and mean keratometric astigmatism was WTR (i.e., positive J0 for keratometric astigmatism and negative J0 for internal astigmatism), reducing the overall magnitude of WTR refractive astigmatism. A similar relation existed between keratometric J45 and internal J45. The same patterns were seen in the full, younger, and older cohorts.
Baseline keratometric and internal astigmatism measurements of J0 were positively correlated, indicating that greater amounts of WTR keratometric astigmatism were not associated with greater amounts of ATR internal astigmatism but rather were associated with lesser amounts of ATR internal astigmatism (Table 4). In contrast, measurements of J45 were negatively correlated, indicating that the greater amounts of keratometric astigmatism were associated with greater amounts of orthogonal (opposite in sign) internal astigmatism.
Table 4.
Summary of Correlations Between Baseline Keratometric Astigmatism and Internal Astigmatism by Sample and Astigmatism Measurement (J0 and J45)
|
Measure |
Full |
Younger Cohort |
Older Cohort |
|||
|
r |
P |
r |
P |
r |
P |
|
| J0 | +0.081 | 0.000 | +0.048 | 0.058, NS | +0.211 | 0.000 |
| J45 | −0.489 | 0.000 | −0.500 | 0.000 | −0.406 | 0.000 |
Bold italic values indicate correlations that are significantly different from 0.
All regressions for prediction of refractive astigmatism from keratometric astigmatism were statistically significant (P values < 0.001, Table 5). All constants and slopes were significantly different from 0. T statistics were used to determine if slopes were significantly different from 1. Results indicated that the J0 slope for the younger cohort, J0 slopes for subjects in the full, younger, and older cohort subjects with significant WTR astigmatism (J0 ≥ 0.50, Table 5, right side), and J45 slope for the older cohort subjects with significant WTR astigmatism were not significantly different from 1 (P > 0.05; Table 5, bold italic values).
Table 5.
Regression Coefficients for Prediction of Baseline Refractive Astigmatism (Dependent Variable) From Baseline Keratometric Astigmatism (Independent Variable)
|
Dataset |
Dependent Variable: Refractive Astigmatism |
All Subjects |
Subjects With Baseline Refractive J0 ≥ 0.50 |
||||
|
Constant |
Slope |
r2 |
Constant |
Slope |
r2 |
||
| Full | J0 | −0.343 | +1.036 | 0.847 | −0.244 | +1.037 | 0.814 |
| J45 | +0.043 | +0.676 | 0.578 | +0.098 | +0.842 | 0.744 | |
| Younger cohort | J0 | −0.329 | +1.021 | 0.841 | −0.220 | +1.011 | 0.807 |
| J45 | +0.034 | +0.678 | 0.595 | +0.084 | +0.826 | 0.753 | |
| Older cohort | J0 | −0.416 | +1.085 | 0.884 | −0.259 | +1.056 | 0.813 |
| J45 | +0.082 | +0.714 | 0.553 | +0.197 | +0.953 | 0.788 | |
Bold italic values indicate slopes that are not significantly different from 1 (P > 0.05).
Analysis of the Relation Between Change in Keratometric Astigmatism and Change in Internal Astigmatism With Age
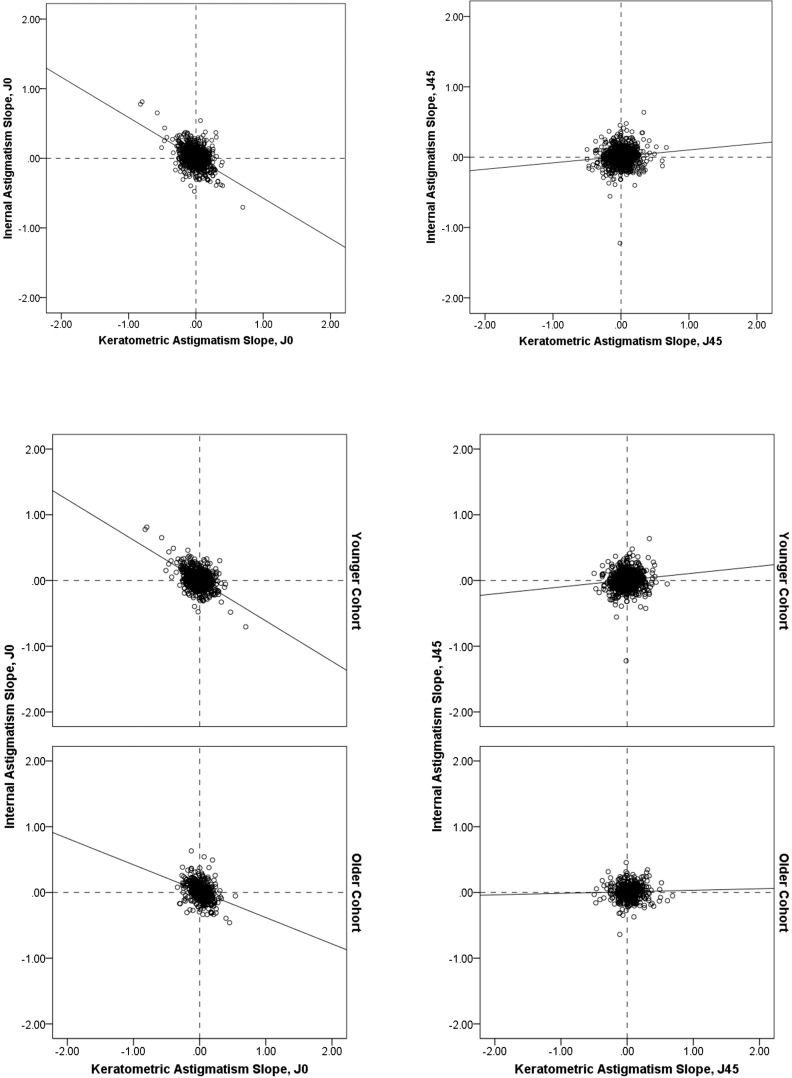
Correlation analyses conducted on keratometric astigmatism and internal astigmatism slope data yielded significant negative correlations for J0 (P values < 0.001; Table 6, bold italic values, Fig. 2). For J45, there were weak but significant positive correlations in the full dataset and the younger cohort (r values only slightly greater than 0.10). There was a single extreme outlier for J0 in the full dataset and in the younger cohort dataset (not shown in Fig. 2). When this subject was excluded, correlations were −0.38 for J0 and +0.11 for J45 in the full dataset (P values < 0.001) and were −0.41 for J0 (P < 0.001) and 0.03 for J45 (not significant) in the younger cohort.
Table 6.
Summary of Correlations Between Keratometric Astigmatism Slope (D/Y) and Internal Astigmatism Slope (D/Y) by Sample and Astigmatism Measurement
|
Sample Measure |
Full |
Younger Cohort |
Older Cohort |
|||
|
r |
P |
r |
P |
r |
P |
|
| J0 | −0.582 | 0.000 | −0.625 | 0.000 | −0.348 | 0.000 |
| J45 | +0.103 | 0.000 | +0.112 | 0.000 | +0.030 | 0.447, NS |
Bold italic values represent statistically significant correlations.
Figure 2.
Scatterplots of slope data for keratometric astigmatism (x-axis) and internal astigmatism (y-axis) measurements of J0 (left) and J45 (right) for the full dataset (top) and for the younger cohort (center) and older cohort (bottom). Positive slope for J0 reflects shift toward increasing with-the-rule/decreasing against-the-rule astigmatism; negative slope for J0 indicates shift toward decreasing with-the-rule/increasing against-the-rule astigmatism.
Discussion
The results of the present study provide the first detailed report on longitudinal changes in refractive astigmatism and its components beyond age 7 years in Tohono O'odham children, and provide insight into the origins and mechanisms responsible for the overall stability of astigmatism in this population. Key findings include the following:
-
1.
Overall, longitudinal changes in astigmatism were statistically but not clinically significant (younger cohort −0.02 D/y; older cohort +0.06 D/y) (Table 2);
-
2.
In the younger cohort, astigmatism decreased with age in low and moderate astigmats (−0.02 D/y and −0.04 D/y for refractive Cyl) and increased with age in high astigmats (+0.06 D/y). In the older cohort, astigmatism increased with age across all levels of astigmatism (Table 3);
-
3.
Mean keratometric astigmatism was 1.19 D WTR (+0.54 J0), and mean internal astigmatism was 0.60 D ATR (−0.31 J0). Magnitude of internal astigmatism was close to the 0.50 D ATR constant reported by Javal and others.10,11 Internal astigmatism was consistent across age groups (Table 1) and magnitude of keratometric astigmatism (Table 3); and
-
4.
Changes with age in keratometric and internal J0 were negatively correlated in both cohorts, suggesting that changes in internal astigmatism may actively compensate for changes in keratometric astigmatism and contribute to the overall stability of WTR refractive astigmatism in childhood (Table 6).
Longitudinal Change in Refractive Astigmatism
We observed no significant change in Cyl and J0 with age in the full dataset (age 3 to <19 years) (Table 2). However, this finding is likely due to the fact that the direction of change was opposite for the younger and older cohorts (decrease in the younger cohort and increase in the older cohort). We also observed that in the younger cohort, astigmatism tended to show a reduction with age in low and moderate astigmats (−0.02 and −0.04 D/y for refractive Cyl) and an increase in high astigmats (+0.06 D/y), whereas the older cohort showed a consistent increase in refractive astigmatism across levels of baseline refractive astigmatism (+0.06, +0.07, and +0.06 D/y for refractive Cyl in no/low, moderate, and high astigmats, respectively) (Table 3). The data suggest that highly astigmatic younger children, and children older than age 11 years, have a tendency to show an increase in astigmatism with age. However, all mean changes observed were small (0.07 D/y or less for refractive astigmatism) and support the conclusion that astigmatism in this population tends to be clinically stable from age 3 to <19 years.
Relation Between J0 Keratometric Astigmatism and J0 Internal Astigmatism at Baseline
Baseline J0 data showed an average WTR keratometric astigmatism of 0.85 D and an average ATR internal astigmatism of 0.31 D (Table 1), resulting in WTR refractive astigmatism (J0 +0.54 D). J0 measurements of keratometric and internal astigmatism (Table 4) were positively correlated, indicating a decrease in ATR internal astigmatism with increasing level of ATR keratometric astigmatism. However, correlations were weak, and the relation explained little variability (r2 values < 0.05). Regression analyses predicting baseline refractive astigmatism from keratometric astigmatism provided further evidence of the independence of magnitude of WTR keratometric astigmatism and ATR internal astigmatism (Table 5). The constant and slope in these regressions represent the influence of internal astigmatism. For WTR astigmatism (J0), regression constants were significantly less than 0, reflecting a fixed component of internal compensation. Regression slopes tended to be close to 1 (not significantly different from 1 for subjects with significant WTR astigmatism, Table 5), indicating that magnitude of ATR internal astigmatism was not dependent upon magnitude of WTR keratometric astigmatism. In the present study, the constant for subjects with clinically significant WTR astigmatism (subjects with refractive J0 ≥ 0.50, equivalent to 1.00 D WTR astigmatism in clinical notation) is approximately −0.25 D of J0 (equivalent to 0.50 D ATR astigmatism in clinical notation). These results are consistent with modifications of Javal's rule specifying that the relation between keratometric astigmatism and refractive astigmatism is best described as magnitude of keratometric astigmatism minus an ATR constant of 0.50 D.10 The ATR internal astigmatism constant appeared to “compensate” for WTR keratometric astigmatism in the present study, resulting in lower levels of WTR refractive astigmatism. However, because the magnitude of internal astigmatism is not negatively correlated with the magnitude of keratometric astigmatism, the data suggest a consistent ATR contribution from internal astigmatism—a passive compensation that can be attributed to the fact that our sample consists primarily of children with high WTR keratometric astigmatism. This regression constant is less than in a previous report on preschoolers from this population that indicated a constant of approximately 0.75 D ATR internal astigmatism.9
Shankar and Bobier19 obtained results similar to our cross-sectional findings in their sample of Canadian preschool children: They reported a predominance of WTR astigmatism (69% in children with ≥1.00 D) that was primarily keratometric in origin, a positive mean J0 for keratometric astigmatism (WTR), and a negative mean J0 for internal astigmatism (ATR). They also observed that the magnitude of ATR internal astigmatism did not increase with the magnitude of WTR keratometric astigmatism. The regression results for our sample were similar to results reported in a recent study of 1004 Singaporean schoolchildren 7 to 13 years old16:
Tong et al.16:
Refractive J0 = 1.04 × Keratometric J0 − 0.34,
Refractive J45 = 0.68 × Keratometric J45 − 0.04;
Present study:
Refractive J0 = 0.93 × Keratometric J0 − 0.28,
Refractive J45 = 0.64 × Keratometric J45 − 0.01.
However, regression slopes differed from results reported by Huynh et al.21 for a sample of 12-year-old Australian children, in which slopes were 0.65 for J0 and 0.40 for J45. The findings of Huynh et al.21 also differed from our results in that those authors found that the contribution of internal astigmatism was related to the magnitude of keratometric astigmatism. The differences in findings across studies may be due to the fact that the present study and the studies by Shankar and Bobier19 and Tong et al.16 included populations in which astigmatism was predominantly WTR, compared to the population studied by Huynh et al.,21 in which axis was WTR in just 40% of children with astigmatism ≥ 1.00 D.
Relation Between J45 Keratometric Astigmatism and J45 Internal Astigmatism at Baseline
Oblique astigmatism in Tohono O'odham children tends to be minimal (Table 1). However, the J45 data showed significant negative correlations between keratometric and internal astigmatism at baseline, indicating, for example, that as J45 keratometric becomes more positive/less negative, J45 internal becomes more negative/less positive (Table 4). This finding suggests the presence of an oblique axis compensation that is tied to amount of keratometric astigmatism. Regression slopes were significantly less than 1, and constants tended to be positive and closer to 0 than J0 regression constants, again suggesting that internal compensation is tied to magnitude of keratometric J45, although regressions were much more strongly predictive for J0 than for J45 (see r2 values, Table 5). This tendency of oblique internal astigmatism to compensate for oblique keratometric astigmatism may contribute to the overwhelming prevalence of WTR astigmatism in this population. It may also serve to maximize visual acuity in the presence of astigmatism by reducing the oblique component of refractive astigmatism. Oblique axis astigmatism has been associated with poorer visual performance than WTR or ATR astigmatism.25,26 Our J45 regression slope results are similar to the findings of Tong et al.16 and Huynh et al.21
Relation Between Change in Keratometric Astigmatism and Change in Internal Astigmatism With Age
One of the unique contributions of the present study is analysis of the relation between changes in internal and keratometric astigmatism during childhood development. For the full cohort, results showed significant negative correlations between change in keratometric J0 (slope) and change in internal J0 (slope) for the full, younger, and older cohort datasets (Table 6). This indicates that change in keratometric astigmatism was balanced by opposite (compensatory) changes in internal astigmatism, resulting in little change in refractive astigmatism. The data did not show a similar compensatory relation between change in keratometric J45 (slope) and change in internal J45 (slope).
The present study has several strengths, including a large sample of children with WTR astigmatism, a longitudinal dataset that spans a wide age range, and use of consistent measurement methods throughout the study and across age. One of the limitations of the present study is the extent to which the findings can be generalized to other populations or to children with ATR or oblique astigmatism.
A second limitation is that we did not directly measure the contribution of individual internal structures that result in internal astigmatism and therefore cannot make any strong conclusions regarding the origins of internal astigmatism and its changes with development. Internal astigmatism can arise from the depth of the anterior chamber, the curvature and thickness of the crystalline lens, or a tilting of the lens. The contribution of the posterior cornea also could not be evaluated in the present study. Keratometry uses the keratometric index of refraction (1.3375) to estimate (based on average values for the population) the optical refracting power of the cornea, incorporating as an estimate the average radius of curvature for the back surface of the cornea (with negative optical power, a consequence of the concave shape of the back surface of the cornea having a slightly higher index of refraction as compared to the aqueous). However, it is not clear if the population average value used in the keratometric index of refraction accurately describes the relation between the total astigmatism (as measured with the autorefractor) and the astigmatism that is predicted by keratometry, especially across a wide range of corneas with various levels of astigmatism. The relative contributions of the anterior and posterior cornea are not known, although it has been suggested that the posterior corneal surface may have a compensatory role.15 Ongoing studies in which we directly measure longitudinal changes in anterior and posterior corneal surfaces will allow us to more precisely explore the optical origins of astigmatism and compensation in this population.
In conclusion, the data indicate that highly astigmatic younger children and children older than age 11 years have a tendency to show a small increase in astigmatism with age but that changes observed were not clinically significant. The data also provide important clues as to the origins of astigmatism and the factors that affect stability and change in astigmatism in this population. The cross-sectional J0 data are consistent with modifications of Javal's rule, showing that the magnitude of ATR internal astigmatism is a constant and is not correlated with magnitude of keratometric astigmatism.10 The longitudinal J0 data show that changes in keratometric astigmatism are strongly correlated with the opposite (compensatory) changes in internal astigmatism. This suggests the presence of a compensation that may arise from a structure mechanically linked to the cornea. This information is essential if any future clinical interventions to treat astigmatism in childhood or alter the course of increasing astigmatism during childhood are to be investigated. However, caution should be used in generalizing these data to astigmatism other than WTR astigmatism.
Acknowledgments
The authors thank the children and families, the Tohono O'odham Nation, the Tohono O'odham Early Childhood Head Start Program, the Baboquivari School District, the Bureau of Indian Affairs Office of Indian Education Programs (BIA OIEP), and the San Xavier Mission School for their participation. Study oversight is provided by a National Institutes of Health/National Eye Institute Data Monitoring and Oversight Committee.
Presented in part at the annual meeting of the Association for Research in Vision and Ophthalmology, Seattle, Washington, United States, May 2013.
Supported by National Institutes of Health/National Eye Institute Grants U10-EY13153 and U10-EY08893 and by Research to Prevent Blindness.
Disclosure: E.M. Harvey, None; J.M. Miller, None; J.D. Twelker, None; D.L. Sherrill, None
References
- 1. Kershner RM, Brick DC. Prevalence of high corneal astigmatism in Papago school children. Invest Ophthalmol Vis Sci. 1984; 25 (suppl): 217. 6698743 [Google Scholar]
- 2. Dobson V, Tyszko RM, Miller JM, Harvey EM. Astigmatism, amblyopia, and visual disability among a Native American population. In: Vision Science and Its Applications. Vol 1. OSA Technical Digest Series. Washington, DC: Optical Society of America; 1996: 139–142. [Google Scholar]
- 3. Dobson V, Miller JM, Harvey EM, Sherrill DL. Prevalence of astigmatism, astigmatic anisometropia, and glasses wearing among preschool- and school-age Native American children. In: Vision Science and Its Applications. Vol 1. OSA Technical Digest Series. Washington, DC: Optical Society of America; 1999: 177–180. [Google Scholar]
- 4. Harvey EM, Dobson V, Miller JM. Prevalence of high astigmatism, eyeglass wear, and poor visual acuity among Native American grade-school children. Optom Vis Sci. 2006; 83: 206–212. [DOI] [PubMed] [Google Scholar]
- 5. Harvey EM, Dobson V, Clifford-Donaldson CE, Green TK, Messer DH, Miller JM. Prevalence of astigmatism in Native American infants and children. Optom Vis Sci. 2010; 87: 400–405. [DOI] [PubMed] [Google Scholar]
- 6. Harvey EM, Dobson V, Miller JM, et al. Prevalence of corneal astigmatism in Tohono O'odham Native American children 6 months to 8 years of age. Invest Ophthalmol Vis Sci. 2011; 52: 4350–4355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harvey EM, Miller JM, Schwiegerling J, Sherrill D, Messer DH, Dobson V. Developmental changes in anterior corneal astigmatism in Tohono O'odham Native American infants and children. Ophthalmic Epidemiol. 2013; 20: 102–108. [DOI] [PubMed] [Google Scholar]
- 8. Twelker JD, Miller JM, Sherrill DL, Harvey EM. Astigmatism and myopia in Tohono O'odham Native American children. Optom Vis Sci. 90: 1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dobson V, Miller JM, Harvey EM. Corneal and refractive astigmatism in a sample of 3- to 5-year-old children with a high prevalence of astigmatism. Optom Vis Sci. 1999; 76: 855–860. [DOI] [PubMed] [Google Scholar]
- 10. Grosvenor T, Quintero S, Perrigin DM. Predicting refractive astigmatism: a suggested simplification of Javal's rule. Am J Optom Physiol Opt. 1988; 65: 292–297. [PubMed] [Google Scholar]
- 11. Javal E. Memoires d'Ophthalmometrie. Masson G. ed Paris: Librarie de l'Academie de Medecine; 1890: 130–131. [Google Scholar]
- 12. Friedman NE, Mutti DO, Zadnik K. Corneal changes in schoolchildren. Optom Vis Sci. 1996; 73: 552–557. [DOI] [PubMed] [Google Scholar]
- 13. Zhao J, Mao J, Luo R, Li F, Munoz SR, Ellwein LB. The progression of refractive error in school-age children: Shunyi district, China. Am J Ophthalmol. 2002; 134: 735–743. [DOI] [PubMed] [Google Scholar]
- 14. Tong L, Saw SM, Lin Y, Chia KS, Koh D, Incidence Tan D. and progression of astigmatism in Singaporean children. Invest Ophthalmol Vis Sci. 2004; 45: 3914–3918. [DOI] [PubMed] [Google Scholar]
- 15. Artal P, Guirao A, Berrio E, Williams DR. Compensation of corneal aberrations by the internal optics of the human eye. J Vis. 2001; 1: 1–8. [DOI] [PubMed] [Google Scholar]
- 16. Tong L, Carkeet A, Saw S, Tan DTH. Corneal and refractive error astigmatism in Singaporean schoolchildren: a vector-based Javal's rule. Optom Vis Sci. 2001; 78: 881–887. [DOI] [PubMed] [Google Scholar]
- 17. Artal P, Berrio E, Guirao A, Piers P. Contribution of the cornea and internal surfaces to the change of ocular aberrations with age. J Opt Soc Am A Opt Image Sci Vis. 2002; 19: 137–143. [DOI] [PubMed] [Google Scholar]
- 18. He JC, Gwiazda J, Thorn F, Held R. Wave-front aberrations in the anterior corneal surface and the whole eye. J Opt Soc Am A Opt Image Sci Vis. 2003; 20: 1155–1163. [DOI] [PubMed] [Google Scholar]
- 19. Shankar S, Bobier WR. Corneal and lenticular components of total astigmatism in a preschool sample. Optom Vis Sci. 2004; 81: 536–542. [DOI] [PubMed] [Google Scholar]
- 20. Kelly JE, Mihashi T, Howland HC. Compensation of corneal horizontal/vertical astigmatism, lateral coma, and spherical aberration by internal optics of the eye. J Vis. 2004; 4: 262–271. [DOI] [PubMed] [Google Scholar]
- 21. Huynh SC, Kifley A, Rose KA, Morgan IG, Mitchell P. Astigmatism in 12-year-old Australian children: comparisons with a 6-year-old population. Invest Ophthalmol Vis Sci. 2007; 48: 73–82. [DOI] [PubMed] [Google Scholar]
- 22. Harvey EM, Miller JM, Dobson V, Tyszko R, Davis AL. Measurement of refractive error in Native American preschoolers: validity and reproducibility of autorefraction. Optom Vis Sci. 2000; 77: 140–149. [DOI] [PubMed] [Google Scholar]
- 23. Vision in Preschoolers Study Group. Impact of confidence number on the screening accuracy of the Retinomax autorefractor. Optom Vis Sci. 2007; 84: 181–188. [DOI] [PubMed] [Google Scholar]
- 24. Miller JM. Clinical applications of power vectors. Optom Vis Sci. 2009; 86: 599–602. [DOI] [PubMed] [Google Scholar]
- 25. Miller JM, Teodoro MR, Lane L, Schwiegerling J. Detection of Sloan Crowded Single Letters (SCSL) in the presence of induced refractive error. In: Vision Science and Its Applications. OSA Technical Digest Series. Washington, DC: Optical Society of America; 2001: 47–50. [Google Scholar]
- 26. Kobashi H, Kamiya K, Shimizu K, Kawamorita T, Uozato H. Effect of axis orientation on visual performance in astigmatic eyes. J Cataract Refract Surg. 2012; 38: 1352–1359. [DOI] [PubMed] [Google Scholar]