Abstract
Background
Overweight is one of the major public health problems in Brazil; it is associated with dyslipidemia, which is an important risk factor for cardiovascular diseases.
Objective
To evaluate the lipid profile of residents of the municipality of São Paulo, state of São Paulo, according to the nutritional status.
Methods
Data from the population-based cross-sectional study ISA-Capital 2008 on a sample of residents of São Paulo were used. Participants were categorized into groups according to body mass index and age range. The levels of total cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, and non-HDL cholesterol were measured. The association between lipid profile, nutricional status, and waist circumference was investigated. The data were processed using the survey mode of the Stata 11.0 software.
Results
The prevalence of any type of dyslipidemia in the population was 59.74%, with low HDL-cholesterol dyslipidemia being the most common type. Not overweight individuals had higher mean levels of HDL-cholesterol and lower levels of LDL-cholesterol, total cholesterol, triglycerides, and non-HDL cholesterol when compared with the overweight group. The rate of inadequacy of these variables was higher in the overweight individuals, regardless of the age group, to the exception of LDL-cholesterol in the adults and elderly. A higher prevalence of isolated hypertriglyceridemia was observed in individuals with higher waist circumference among the adults and the total population.
Conclusion
The results indicate an association between dyslipidemia and overweight in the population of the city of São Paulo. The most prevalent dyslipidemia in this population was low HDL-cholesterol.
Keywords: Dyslipidemias/epidemiology, Prevalence, Statistical Analysis, Nutritional Status, Obesity/complications
Introduction
Overweight and obesity, characterized by excessive accumulation of adipose tissue in the body, represent a growing epidemiological problem worldwide and a great challenge to public health in several countries1. In Brazil, the prevalence of overweight [body mass index (BMI) ≥ 25 kg/m2] in men and women aged 20-59 years, increased from 18.5% to 50.1% and from 28.7% to 48.0%, respectively, between 1975 and 2009. In addition, the prevalence of obesity (BMI ≥30 kg/m2) in the adult population has increased from 2.8% to 12.4% in men and from 8.0% to 16.9% in women2. This increase is a cause for concern because overweight is a risk factor for various health disorders3,4 and causes a significant increase in direct and indirect costs4,5.
Several studies have indicated a relationship between excessive body fat and risk for diseases that increase morbidity and mortality, including cardiovascular diseases, which are among the main leading causes of death worldwide1,4,6,7. Another consequence of overweight is dyslipidemia6, which is defined by the presence of at least one alteration in the lipid profile: increased serum levels of low-density lipoprotein cholesterol (LDL-c) and triglycerides (TG) and/or decreased levels of high-density lipoprotein cholesterol (HDL-c). The increase in the number of these alterations is positively correlated with the development of atherosclerosis, which is a chronic inflammatory disease closely related to elevated serum levels of total cholesterol (TC) and leads to thickening of the medial and intimal layers of arterial walls and reduced arterial elasticity8-10.
The epidemiological evaluation of the lipid profile is an important tool for the promotion of health policies aimed at preventing and reducing cardiovascular risk factors in the general population10,11. Considering the major effects of obesity on health, the objective of the present study was to assess the lipid profile of adolescents, adults, and elderly in the municipality of São Paulo, state of São Paulo, according to the nutritional status.
Methods
Data from the cross-sectional study population ISA-Capital 2008 on a representative sample of residents of São Paulo were used12. In this study, 2,691 adolescents (aged 12−19 years), adults (aged 20−59 years), and elderly (aged ≥ 60 years) of both sexes were interviewed. Blood biochemistry was performed in 748 residents (158 adolescents, 302 adults, and 288 elderly). Of them, 29 residents were excluded because of incomplete socioeconomic, anthropometric, and biochemical data; and eventually, 719 (157 adolescents, 299 adults, and 263 elderly) were analyzed. The loss of sampling data from ISA-Capital 2008 occurred randomly in all the strata evaluated, without any bias regarding sex, age, income, and level of schooling13. In addition, weight was recalculated for the sample with biochemical data to ensure that the results were representative of the population of São Paulo.
Data were collected by means of home visits between September 2008 and March 2009 using structured questionnaires containing pre-coded questions that were administered by trained interviewers. The items included per capita family income, classified as up to one minimum salary (MS) and more than one MS, according to the value in effect in 2008 (R$ 415.00), and the years of schooling of the family head, categorized as ≤ 9 years and ≥ 10 years.
Anthropometric and biochemical data were obtained during home visits by qualified nurses. Weight, height3, and waist circumference (WC)14 were measured, and biological samples were collected15. For blood collection, the individuals were instructed to fast for 12 hours before and to abstain from alcohol for 3 days before the test as well as to avoid physical activity or effort on the day of the test. The nutritional status was assessed according to the cut-off BMI [BMI = weight (kg)/[height (m)]2] values proposed by the World health Organization (WHO)16 for adolescents and adults3, and by the Pan American Health Organization (PAHO)17 for the elderly. The nutritional status was analyzed as per the following categories: not overweight, including individuals with low and normal weight; and overweight, including overweight and obese individuals. The cut-off point used for WC was 102 cm for men and 88 cm for women14.
The biochemical variables TC, HDL-c, LDL-c, and serum TG were measured using the enzyme-colorimetric method. The values for non-HDL cholesterol were obtained by subtracting HDL-c from TC values. For sample categorization, cut-off points for inadequacy were used, according to the V Brazilian Guideline on Dyslipidemia18. The lipid profile of adolescents was considered inadequate when serum HDL-c level <45 mg/dL, LDL-c level ≥ 130 mg/dL, TC level ≥170 mg/dL, and TG level ≥ 130 mg/dL. For the adults and elderly, the cut-off points for inadequacy were the following: HDL-c levels ≤40 mg/dL in men and ≤ 50 mg/dL in women, LDL-c levels ≥ 160 mg/dL, TC levels ≥ 200 mg/dL, and TG levels ≥ 150 mg/dL.
The Wald test was used to compare the mean levels of the lipid variables according to the nutritional status of the population under study. Pearson's chi-square test was used to compare the prevalence of dyslipidemia among overweight and not overweight individuals and among those with adequate and inadequate WC. Quantitative variables were expressed as mean and standard error, and the qualitative variables as numbers and percentages. The analyses were performed using the survey mode in the Stata statistical software, version 11.0, to ensure that the obtained results would be representative of the total population of the municipality of São Paulo. The level of significance was set at 5%.
The participants signed an informed consent form. O trabalho foi aprovado pelo Comitê de Ética em Pesquisa da Faculdade de Saúde Pública (OF.COEP 056/13) e financiado pela Secretaria Municipal da Saúde de São Paulo, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), processo 503128/2010-4, e Fundação de Amparo à Pesquisa do Estado de São Paulo (Fapesp), processos 2009/15831-0 e 2012/24743-0.
Results
Table 1 shows the profile of the population under study, according to sex, socioeconomic status (per capita family income and level of schooling of the family head), and anthropometric factors (BMI and WC) according to the age group. Approximately half of the study population (49.81%) had normal weight and 46.01% were overweight. Furthermore, 84.04% of the adolescents had an adequate nutritional status, whereas 37.28% elderly were obese. With regard to central obesity, 48.33% of the total population had an inadequate WC, which was higher among the elderly (74.68%). The presence of any type of dyslipidemia was observed in 59.74% of the study population.
Table 1.
Profile of the study population; São Paulo, state of São Paulo, 2008, according to the age group*
| Adolescents | Adults | Elderly | Total | |||||
|---|---|---|---|---|---|---|---|---|
| % | 95% CI* | % | 95% CI* | % | 95% CI* | % | 95% CI* | |
| Gender | ||||||||
| Male | 50.1 | 41.4-58.8 | 48.2 | 42.0-54.4 | 39.6‡ | 33.5-46.0 | 47.1 | 42.7-51.5 |
| Female | 49.9 | 41.2-58.6 | 51.8 | 45.6-58.0 | 60.4‡ | 54.0-66.5 | 52.9 | 48.5-57.3 |
| Per capita family income† | ||||||||
| ≤1 MS | 60.5‡ | 51.3-69.0 | 37.6‡ | 29.5-46.5 | 37.9‡ | 30.0-46.4 | 40.5‡ | 34.0-47.2 |
| >1 MS | 39.5‡ | 31.0-48.7 | 62.4‡ | 53.6-70.5 | 62.2‡ | 53.7-70.0 | 59.5‡ | 52.8-66.0 |
| Level of schooling of the family head | ||||||||
| ≤ 9 years | 41.2‡ | 33.8-48.9 | 43.4 | 33.1-54.3 | 64.3‡ | 55.4-72.3 | 46.3 | 38.4-54.5 |
| ≥10 years | 58.9‡ | 51.1-66.2 | 56.6 | 45.7-66.9 | 35.7‡ | 27.8-44.6 | 53.7 | 45.5-61.7 |
| BMI | ||||||||
| Low weight | 2.5 | 0.1-6.9 | 2.2 | 1.0-4.7 | 15.1 | 11.3-19.9 | 4.2 | 2.9-6.0 |
| Eutrophy | 84.0 | 76.6-89.5 | 46.8 | 41.1-52.6 | 36.6 | 30.9-42.7 | 49.8 | 45.6-54.1 |
| Overweight | 11.0 | 6.7-17.5 | 31.1 | 25.6-37.1 | 11.1 | 7.2-16.6 | 25.6 | 21.2-30.5 |
| Obesity | 2.4 | 1.0-6.0 | 20.0 | 15.1-25.9 | 37.3 | 32.5-42.3 | 20.5 | 16.9-24.5 |
| Waist circumference | ||||||||
| Adequate | 80.0‡ | 70.7-86.8 | 52.4 | 46.2-58.6 | 25.3‡ | 20.1-31.4 | 51.7 | 47.1-56.2 |
| Inadequate | 20.1‡ | 13.2-29.3 | 47.6 | 41.4-53.8 | 74.7‡ | 68.6-79.9 | 48.3 | 43.8-52.9 |
| Dyslipidemia | ||||||||
| Absence | 44.3 | 35.6-53.3 | 39.7‡ | 33.5-46.2 | 39.7‡ | 32.9-46.9 | 40.3‡ | 35.8-44.8 |
| Presence | 55.7 | 46.7-64.4 | 60.3‡ | 53.8-66.5 | 60.3‡ | 53.1-67.1 | 59.7‡ | 55.2-64.2 |
| Total | 12.3 | 9.7-15.6 | 72.4 | 68.2-76.2 | 15.3 | 12.5-18.7 | 100.0 | |
Weighted values according to sampling design;
MS was R$ 415.00 at the time of the study;
significant difference (95% CI) between the categories of the dichotomous variables, by age group. The results are expressed as percentages and 95% CI. 95% CI: 95% confidence interval; MS: minimum salary; BMI: body mass index.
The mean levels of the biochemical variables HDL-c, LDL-c, CT, TG, and non-HDL cholesterol were measured according to the nutritional status (overweight and not overweight) in the total population and according to age group to take into account the physiological differences between the age groups (Table 2).
Table 2.
Mean, standard error, and p value of the levels of lipid variables in the residents of São Paulo, state of São Paulo, in 2008, according to nutritional status
| Variables | Not overweight | Overweight | p value | Total | |||
|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | ||
| Total population | |||||||
| HDL-c | 50 | 1 | 45 | 1 | 0.001 | 48 | 1 |
| LDL-c | 104 | 3 | 116 | 3 | 0.002 | 110 | 2 |
| TC | 175 | 3 | 194 | 3 | 0.000 | 184 | 2 |
| TG | 104 | 5 | 164 | 10 | 0.000 | 132 | 6 |
| Non-HDL | 125 | 3 | 148 | 3 | 0.000 | 135 | 2 |
| Adolescents | |||||||
| HDL-c | 47 | 1 | 41 | 1 | 0.002 | 47 | 1 |
| LDL-c | 74 | 2 | 83 | 5 | 0.105 | 76 | 2 |
| TC | 137 | 3 | 145 | 7 | 0.281 | 138 | 2 |
| TG | 75 | 3 | 105 | 10 | 0.006 | 79 | 3 |
| Non- HDL | 89 | 2 | 104 | 6 | 0.023 | 91 | 2 |
| Adults | |||||||
| HDL-c | 50 | 2 | 45 | 1 | 0.003 | 48 | 1 |
| LDL-c | 109 | 4 | 115 | 3 | 0.171 | 112 | 3 |
| TC | 181 | 5 | 192 | 4 | 0.034 | 187 | 3 |
| TG | 109 | 8 | 167 | 12 | 0.000 | 139 | 8 |
| Non- HDL | 130 | 4 | 148 | 4 | 0.001 | 139 | 3 |
| Elderly | |||||||
| HDL-c | 55 | 1 | 49 | 1 | 0.001 | 52 | 1 |
| LDL-c | 124 | 4 | 129 | 4 | 0.338 | 126 | 3 |
| TC | 202 | 4 | 210 | 5 | 0.232 | 206 | 3 |
| TG | 121 | 4 | 162 | 11 | 0.000 | 141 | 6 |
| Non-HDL | 148 | 4 | 161 | 5 | 0.048 | 154 | 3 |
HDL-c: high-density lipoprotein; LDL-c: low-density lipoprotein; SE: standard error; TC: total cholesterol; TG: triglycerides.
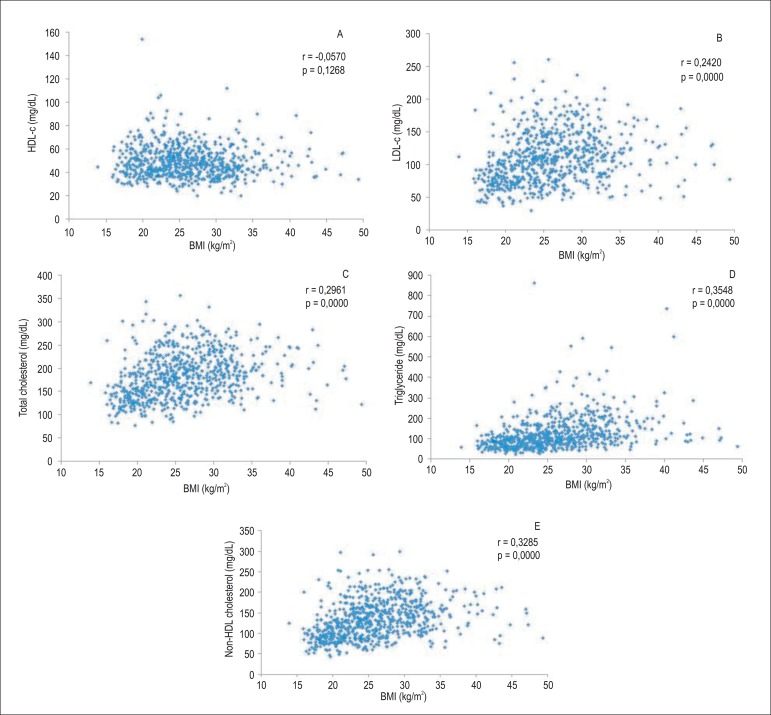
When data of the total population were analyzed continuously, a positive correlation was observed between the lipid variables LDL-c, TC, TG, non-HDL cholesterol and BMI; however, the correlation was not significant for HDL-c (Figure 1). In addition, a positive correlation was observed between the lipid variables LDL-c, TC, TG, non-HDL cholesterol and WC (Figure 2).
Figure 1.
Scatter plots of the correlation between high-density lipoprotein cholesterol (HDL-c) (A), low-density lipoprotein cholesterol (LDL-c) (B), total cholesterol (C), triglycerides (D), non-HDL cholesterol (E) and body mass index (BMI) in the total population. São Paulo (SP), 2008.
Figure 2.
Scatter plots of the correlation between high-density lipoprotein cholesterol (HDL-c) (A), low-density lipoprotein cholesterol (LDL-c) (B), total cholesterol (C), triglycerides (D), non-HDL cholesterol (E) and waist circumference (WC) in the total population. São Paulo (SP), 2008.
Table 3 shows a higher prevalence of inadequacy of the recommended lipid profile parameters in overweight individuals. A higher percentage of dyslipidemia was observed in overweight adults and elderly in all categories, but this difference was not significant for LDL-c (isolated hypercholesterolemia) in both age groups. The adolescent group was not assessed separately because of the low prevalence of dyslipidemia (1.02%) but was included in the calculation of the total population.
Table 3.
Prevalence of dyslipidemia In overweight and not overweight Individuals, São Paulo (SP), 2008
| Adults | Elderly | Total population* | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lipid variables | Not EW | EW | p value | Not EW | EW | p value | Not EW | EW | p value | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| Low HDL | 54 (31.8) | 78 (47.3) | 0.03 | 28 (20.1) | 50 (41.1) | 0.01 | 148 (33.4) | 143 (46.9) | 0.021 | 291 (39.6) |
| Isolated hypercholesterolemia | 11 (6.8) | 16 (9.7) | 0.30 | 26 (19.2) | 25 (22.3) | 0.63 | 38 (7.4) | 44 (11.8) | 0.058 | 82 (9.4) |
| Isolated hypertriglyceridemia | 17 (10.6) | 64 (45.3) | 0.00 | 38 (26.0) | 58 (46.8) | 0.00 | 60 (11.6) | 128 (44.7) | 0.000 | 188 (26.8) |
| Mixed hyperlipidemia | 5(3.2) | 14 (10.6) | 0.01 | 11 (6.9) | 19 (18.1) | 0.01 | 17 (3.2) | 35 (11.7) | 0.000 | 52 (7.1) |
| Any dyslipidemia | 77 (47.0) | 112 (73.1) | 0.00 | 73 (51.4) | 82 (69.9) | 0.01 | 220 (48.4) | 214 (73.0) | 0.000 | 434 (59.7) |
Total population includes adolescents, adults, and elderly; EW: overweight; HDL: high-density lipoprotein.
Table 4, shows the prevalence of dyslipidemia according to the adequacy of WC in the total population and by age group. A higher prevalence of any type of dyslipidemia was observed in individuals with inadequate WC, and was statistically significant for low HDL-c among the adults and elderly, for isolated hypertriglyceridemia in adults and the total population, and for any type of dyslipidemia in adults and the total population. The adolescent category was not assessed separately because of the low prevalence of dyslipidemia (1.02%) but was included in the calculation of the total population.
Table 4.
Prevalence of dyslipidemia according to the adequacy of the waist circumference (WC) by age group, São Paulo (SP), 2008
| Adults | Elderly | Total* | Total* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WC adequacy† | WC inadequacy‡ | p value | WC adequacy† | WC Inadequacy‡ | p value | WC adequacy† | WC inadequacy‡ | p value | ||
| Lipid variables | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||
| Low HDL-c | 58 (33.6) | 74 (46.4) | 0.05 | 13 (19.0) | 65 (34.0) | 0.05 | 135 (35.8) | 156 (43.6) | 0.121 | 291 (39.6) |
| Isolated hypercholesterolemia | 12 (7.5) | 15 (9.1) | 0.62 | 14 (19.1) | 27 (21.2) | 0.75 | 27(7.1) | 55 (11.9) | 0.102 | 82 (9.4) |
| Isolated hypertriglyceridemia | 28 (19.3) | 53 (38.2) | 0.00 | 18 (27.1) | 78 (39.1) | 0.15 | 51 (17.0) | 13.7 (37.4) | 0.000 | 188 (26.8) |
| Mixed hyperlipidemia | 9(7.2) | 10 (6.8) | 0.92 | 7 (8.8) | 23 (14.6) | 0.36 | 17 (6.0) | 35(8.3) | 0.368 | 52 (7.1) |
| Any dyslipidemia | 84 (51.2) | 105 (70.4) | 0.00 | 35 (48.8) | 120 (64.2) | 0.06 | 187 (51.6) | 247 (68.5) | 0.001 | 434 (59.7) |
Total population included adolescents, adults, and elderly;
adequate WC: ≤ 102 cm in men and ≤ 88 cm in women;
inadequate WC: > 102 cm in men and > 88 cm in women.
Discussion
The results of the present study indicate an association between overweight and dyslipidemia in a sample population in the city of São Paulo. The most prevalent dyslipidemia in the study population was low HDL-c.
Several studies in Brazil have reported that overweight and obesity are associated with dyslipidemia6,10,19,20. In the present study, considering the total population, the mean lipid levels were within those recommended by the V Brazilian Guidelines on Dyslipidemia and Atherosclerosis Prevention18, with the exception of TG in overweight individuals and for HDL-c, when considering the cut-off point for women. Previous studies have demonstrated that, although overweight individuals can have higher levels of TC than normal-weight individuals, the main dyslipidemia associated with the accumulation of adipose tissue is characterized by elevated TG and decreased HDL-c levels19,21-24.
The number of deaths by cardiovascular disease has increased in Brazil mainly because of elevated BMI9 (Figure 1). A study conducted with adolescents in Campina Grande (PB) showed an association between BMI and TC and its LDL fraction6. Santos et al25 and Liberato et al26 reported a negative correlation between HDL-c and BMI.
Another condition associated with dyslipidemia is abdominal obesity27-29. The results of the present study are in line with those of Rezende et al30 and Alvarez et al31, who demonstrated an association between WC and cardiovascular risk factors.
International studies indicate that dyslipidemia is a global problem. Data from the National Health and Nutrition Examination Survey (NHANES) showed that 12.9% of North American adults have elevated TC levels (≥ 240 mg/dL) and 17.4% of these adults have low HDL-c levels (< 40 mg/dL)32. In a population-based study conducted in Shanghai, China, with 14,385 adults of both sexes, 36.5% of the population had dyslipidemia, 3.8% had mixed hyperlipidemia, 24.9% had isolated hypertriglyceridemia, 3.2% had isolated hypercholesterolemia, and 4.7% had low HDL-c33. Dyslipidemia was associated with BMI, WC, age, and gender, as observed in the present study.
In the present study, 59.74% of the population of São Paulo (overweight and not overweight) had dyslipidemia (Table 1). Of these individuals, 39.58% had low HDL-c levels, 9.39% had elevated LDL-c levels (isolated hypercholesterolemia), 26.82% had elevated TG levels (isolated hypertriglyceridemia), and 7.13% had mixed hyperlipidemia. Furthermore, this population was characterized considering the increased LDL-c and TG levels, and mixed hyperlipidemia was defined as TG levels ≥ 400 mg/dL and TC levels ≥ 200 mg/dL. Another population-based cross-sectional study conducted in São Paulo in 2001-2002 demonstrated that the total prevalence of dyslipidemia, adjusted for age, in the age group 15-59 years was 8.1% for TC (≥ 240 mg/dL), 27.1% for HDL-c (< 40 mg/dL), and 14.4% for TG (≥ 200 mg/dL)34. A study that evaluated a population sample from Rio de Janeiro showed that the prevalence of any type of dyslipidemia was 24.2%, with 18.3% for low HDL-c (< 40 mg/dL), 3.5% for elevated LDL-c (≥ 160 mg/dL), 4.2% for isolated hypercholesterolemia (≥ 240 mg/dL), and 17.1% for isolated hypertriglyceridemia (≥ 200 mg/dL)10. The prevalence in these studies was lower than that found in the present study; however, those authors did not analyze the correlation between these variables and the nutritional status of the population. The prevalence differences between the present study and other studies may be explained by the cut-off points used to determine dyslipidemia, which were higher for TC, TG, and HDL-c in women because the authors of those studies followed the recommendations in force at the time. In the present study, the updated criteria proposed in the V Brazilian Guideline on Dyslipidemia and Atherosclerosis Prevention of the Brazilian Society of Cardiology18 were used, and took into account the differences between age groups for adults and elderly as well as gender. In addition, this result may be due to lifestyle changes that have occurred in recent years. The current dietary pattern, the so-called "Western diet," which is high in fats, cholesterol, refined sugar, and low in fiber35, and a sedentary lifestyle36 are factors that contribute to the increased prevalence of dyslipidemia.
According to the results of the present study, low HDL-c was the major contributor to dyslipidemia in this population. Diet and lifestyle changes, such as weight loss, decreased intake of saturated and trans fatty acids, exercise, and smoking cessation have a significant impact on HDL-c levels18. With regard to cardiovascular risk, the primary therapeutic goal in cases of dyslipidemia is LDL-c because the prevalence of this type of dyslipidemia was low in the total population (9.39%), whereas that of low HDL-c was 39.58%.
Although smoking is established to be a major health problem, its global use remains high. Brazil is the second largest producer of tobacco in the world and the largest exporter of leaf tobacco; however, it has managed to resist this trend37. The prevalence of tobacco use in the population aged ≥18 years in São Paulo is 21.5% and 23.8% among men. No significant difference in the smoking prevalence between 2008 (21.5%) and 2003 (21.2%) in the general population of both genders was observed38.
An epidemiological study conducted in São Paulo showed that only one third of the population performs any type of physical activity, which indicates a high prevalence of sedentarism36. A formative analysis of the local environmental factors associated with overweight in adults residing in São Paulo showed an inverse correlation between the prevalence of overweight and the density of parks and public sport facilities. Most parks are concentrated in the central and richest area of the city, which exhibits the lowest obesity rate and higher physical activity39. This scenario is a cause of concern because physical activity is a decisive factor for the increase in HDL-c levels.
A limitation of the present study was the fact that the individuals using medications to control dyslipidemia or other drugs that could interfere with the lipid profile were not excluded. However, these individuals represented only 7.13% of the sample group.
It is essential to investigate the prevalence of dyslipidemia and obesity in the population with the aim of promoting preventive and curative measures for cardiovascular diseases. Because São Paulo is the most populous city in the Brazil40, the results of this study are an important analysis instrument for the creation or remodeling of public health programs to improve the health of the population in all age groups.
Conclusion
Obesity and its consequences have major negative effects on the health of the Brazilian population. The results of the present study indicate an association between dyslipidemia and overweight in the residents of São Paulo. In addition, the most prevalent dyslipidemia in this population was low HDL-c.
Acknowledgments
We are grateful to São Paulo Research Foundation (FAPESP), processes 2009/15831-0 and 2012/24743-0, and the National Council for Scientific and Technological Development (CNPq), process 503128/2010-4, for funding the research. We also thank the Grupo de Avaliação do Consumo for the support during the development of the study and for providing data from the ISA-Capital study.
Funding Statement
This study was funded by Secretaria Municipal de Saúde, CNPq - nº473100/2009-6 e FAPESP - nº 2009/15831-0.
Footnotes
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conception and design of the research and Acquisition of data: Marchioni DML, Fisberg RM; Analysis and interpretation of the data: Garcez MR, Pereira JL, Fontanelli MM, Marchioni DML, Fisberg RM; Statistical analysis: Pereira JL, Fontanelli MM; Obtaining financing: Fisberg RM; Writing of the manuscript: Garcez MR; Critical revision of the manuscript for intellectual content: Pereira JL, Fontanelli MM, Marchioni DML, Fisberg RM.
Sources of Funding
This study was funded by Secretaria Municipal de Saúde, CNPq - nº473100/2009-6 e FAPESP - nº 2009/15831-0.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Shepherd A. Obesity: prevalence, causes and clinical consequences. Nurs Stand. 2009;23(52):51–57. doi: 10.7748/ns.23.52.51.s52. [DOI] [PubMed] [Google Scholar]
- 2.Instituto Brasileiro de Geografia e Estatistica . Pesquisa de orçamentos familiares 2008-2009: antropometria e estado nutricional de crianças, adolescentes e adultos no Brasil. Rio de Janeiro: 2010. [Google Scholar]
- 3.World Health Organization . Physical status: the use and interpretation of anthropometry: report of a WHO expert committee. Geneva: 1995. [PubMed] [Google Scholar]
- 4.World Health Organization . Obesity: preventing and managing the global epidemic: report of a WHO consultation on obesity. Geneva: 1998. [PubMed] [Google Scholar]
- 5.Wolf AM, Colditz GA. Current estimates of the economic cost of obesity in the United States. Obes Res. 1998;6(2):97–106. doi: 10.1002/j.1550-8528.1998.tb00322.x. [DOI] [PubMed] [Google Scholar]
- 6.Carvalho DF, Paiva AA, Melo AS, Ramos AT, Medeiros JS, Medeiros CC, et al. Perfil lipídico e estado nutricional de adolescentes. Rev Bras Epidemiol. 2007;10(4):491–498. [Google Scholar]
- 7.Swain C, Sacher P. Child obesity: a manageable condition. Nurse Prescribing. 2009;7(1):14–18. [Google Scholar]
- 8.Pereira JA, Rondó PH, Lemos JO, de Oliveira E, Rocha C, Hipólito C. Nutritional status and lipid profile of young children in Brazil. J Trop Pediatr. 2013;59(1):54–58. doi: 10.1093/tropej/fms035. [DOI] [PubMed] [Google Scholar]
- 9.Sposito AC, Caramelli B, Fonseca FA, Bertolami MC, Afiune A, Neto, Souza AD, et al. Sociedade Brasileira de Cardiologia IV Diretriz brasileira sobre dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol. 2007;88(supl 1):1–18. [Google Scholar]
- 10.de Souza LJ, Souto JT, Filho, de Souza TF, Reis AF, Gicovate C, Neto, Bastos DA, Côrtes VA, et al. Prevalence of dyslipidemia and risk factors in Campos dos Goytacazes, in the Brazilian State of Rio de Janeiro. Arq Bras Cardiol. 2003;81(3):249–264. doi: 10.1590/s0066-782x2003001100005. [DOI] [PubMed] [Google Scholar]
- 11.Li P, Yang F, Xiong F, Huo T, Tong Y, Yang S, et al. Nutritional status and risk factors of overweight and obesity for children aged 9-15?years in Chengdu, Southwest China. BMC Public Health. 2012;12:636–636. doi: 10.1186/1471-2458-12-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.São Paulo. Secretaria Municipal da Saúde de São Paulo . Coordenação de epidemiologia e informação; CEInfo/SMS/PMSP. Boletim nº 1. Sep, 2010. [Google Scholar]
- 13.Selem SS, Castro MA, César CL, Marchioni DM, Fisberg RM. Validade da hipertensão autorreferida associa-se inversamente com escolaridade em brasileiros. Arq Bras Cardiol. 2013;100(1):52–59. doi: 10.1590/s0066-782x2012005000119. [DOI] [PubMed] [Google Scholar]
- 14.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. (WHO) Europe: guidelines on hand hygiene in healthcare. Geneva: 2009. [Google Scholar]
- 16.World Health Organization. (WHO) Europe: the challenge of obesity in the WHO European Region and the Strategies for Response. Geneva: 2007. [Google Scholar]
- 17.Wold Health Organization. (WHO) Anales da 36ª Reunión del Comité Asesor de Investigaciones en salud. Encuesta multicentrica: salud, bien estar y envejecimiento (SABE) en América Latina y el Caribe. Washington (DC): 2001. [Google Scholar]
- 18.Xavier HT, Izar MC, Faria JR, Neto, Assad MH, Rocha VZ, Sposito AC, Sociedade Brasileira de Cardiologia V Diretriz brasileira de dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol. 2013;101(4) supl. 1:1–22. doi: 10.5935/abc.2013S010. [DOI] [PubMed] [Google Scholar]
- 19.Pereira PB, Arruda IK, Cavalcanti AM, Diniz Ada S. Perfil lipídico em escolares de Recife - PE. Arq Bras Cardiol. 2010;95(5):606–613. doi: 10.1590/s0066-782x2010005000136. [DOI] [PubMed] [Google Scholar]
- 20.Rabelo LM, Viana RM, Schimith MA, Patin RV, Valverde MA, Denadai RC, et al. Fatores de risco para doença aterosclerótica em estudantes de uma universidade privada em São Paulo - Brasil. Arq Bras Cardiol. 1999;72(5):569–580. doi: 10.1590/s0066-782x1999000500004. [DOI] [PubMed] [Google Scholar]
- 21.Sociedade Brasileira de Cardiologia Diretrizes para cardiologistas sobre excesso de peso e doença cardiovascular dos Departamentos de Aterosclerose, Cardiologia Clínica e FUNCOR. Arq Bras Cardiol. 2002;78(supl.1):1–13. [PubMed] [Google Scholar]
- 22.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Health CW., Jr Body mass index and mortality in a prospective cohort of US adults. N Eng J Med. 1999;341(15):1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 23.Lotufo PA. Mortalidade precoce por doenças do coração no Brasil: comparação com outros paises. Arq Bras Cardiol. 1998;70(5):321–325. doi: 10.1590/s0066-782x1998000500003. [DOI] [PubMed] [Google Scholar]
- 24.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart. Circulation. 1983;67(5):968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 25.Santos CM, Silva CS, Araújo EC, Arruda IKG, Diniz AS, Cabral PC. Perfil lipídico e glicídico de pacientes atendidos em ambulatório e sua correlação com índices antropométricos. Rev Port Cardiol. 2013;32(1):35–34. doi: 10.1016/j.repc.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Liberato SC, Maple-Brown L, Bressan J, Hills AP. The relationships between body composition and cardiovascular risk factors in young Australian men. Nutr J. 2013;12:108–108. doi: 10.1186/1475-2891-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clinical Guidelines on the Identification. Evaluation.and Treatment of Overweight and Obesity in Adults The evidence Report National Institutes of Health. Obes Res. 1998;6(6) Suppl. 2:51S–209S. Erratum in: Obes Res 1998 Nov;6(6):464.. [PubMed] [Google Scholar]
- 28.Zhu S, Wang Z, Heshka S, Heo M, Faith MS, Heymsfields SB, et al. Waist circumference and obesity-associated risk factors among whites in the third National Health and Nutrition Examination Survey: clinical action thresholds. Am J Clin Nutr. 2002;76(4):743–749. doi: 10.1093/ajcn/76.4.743. [DOI] [PubMed] [Google Scholar]
- 29.Misra A, Vikram NK. Clinical and pathophysiological consequences of abdominal adiposity and abdominal adipose tissue depots. Nutrition. 2003;19(5):457–466. doi: 10.1016/s0899-9007(02)01003-1. [DOI] [PubMed] [Google Scholar]
- 30.Rezende FA, Rosado LE, Ribeiro Rde C, Vidigal Fde C, Vasques AC, Bonard IS, et al. Índice de massa corporal e circunferência abdominal: associação com fatores de risco cardiovascular. Arq Bras Cardiol. 2006;87(6):728–734. doi: 10.1590/s0066-782x2006001900008. [DOI] [PubMed] [Google Scholar]
- 31.Alvarez MM, Vieira ACR, Sicheri R, Veiga GV. Associação das medidas antropométricas de localização de gordura central com os componentes da síndrome metabólica em uma amostra probabilística de adolescentes de escolas públicas. Arq Bras Endocrinol Metabol. 2008;52(4):649–657. doi: 10.1590/s0004-27302008000400011. [DOI] [PubMed] [Google Scholar]
- 32.Ogden CL, Carroll MD, Kit BK, Flegal KM, Centers for Disease Control and Prevention . Prevalence of obesity in the United States, 2009-2010. NCHS Data Brief; Atlanta: January . 2012. 2012. [PubMed] [Google Scholar]
- 33.Wu JY, Duan XY, Li L, Dai F, Li Y, Li X, et al. Dyslipidemia in Shanghai, China. Prev Med. 2010;51(5):412–415. doi: 10.1016/j.ypmed.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 34.Marcopito LF, Rodrigues SS, Pacheco MA, Shirassu MM, Goldfeder AJ, Moraes MA. Prevalência de alguns fatores de risco para doenças crônicas na cidade de São Paulo. Rev Saúde Pública. 2005;39(5):738–745. doi: 10.1590/s0034-89102005000500007. [DOI] [PubMed] [Google Scholar]
- 35.Fisberg RM, Slater B, Barros RR, Lima FD, Cesar CL, Carandina L, et al. Índice de qualidade da dieta: avaliação da adaptação e aplicabilidade. Rev Nutr. 2004;17(3):301–318. [Google Scholar]
- 36.Mello MT, Fernandez AC, Tufik S. Levantamento epidemiológico da prática de atividade física na cidade de São Paulo. Rev Bras Med Esporte. 2000;6(4):119–124. [Google Scholar]
- 37.Cavalcante TM. O controle do tabagismo no Brasil: avanços e desafios. Rev Psiq Clin. 2005;32(5):283–300. [Google Scholar]
- 38.São Paulo . Secretaria Municipal da Saúde de São Paulo.Boletim ISA - Capital 2008. Inquérito de Saúde: primeiros resultados. São Paulo: CEInfo; 2010. [Google Scholar]
- 39.Jaime PC, Duran AC, Sarti FM, Lock K. Investigating environmental determinants of diet, physical activity, and overweight among adults in Sao Paulo, Brazil. J Urban Health. 2011;88(3):567–581. doi: 10.1007/s11524-010-9537-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Instituto Brasileiro de Geografia e Estatística [Acesso em 2013 jun 27];[Internet]. Censo demográfico 2010. Disponível em: http://www.censo2010.ibge.gov.br/sinopse/index.php?uf=35&dados=0.