Abstract
Background
Cardiovascular urgencies are frequent reasons for seeking medical care. Prompt and accurate medical diagnosis is critical to reduce the morbidity and mortality of these conditions.
Objective
To evaluate the use of a pocket-size echocardiography in addition to clinical history and physical exam in a tertiary medical emergency care.
Methods
One hundred adult patients without known cardiac or lung diseases who sought emergency care with cardiac complaints were included. Patients with ischemic changes in the electrocardiography or fever were excluded. A focused echocardiography with GE Vscan equipment was performed after the initial evaluation in the emergency room. Cardiac chambers dimensions, left and right ventricular systolic function, intracardiac flows with color, pericardium, and aorta were evaluated.
Results
The mean age was 61 ± 17 years old. The patient complaint was chest pain in 51 patients, dyspnea in 32 patients, arrhythmia to evaluate the left ventricular function in ten patients, hypotension/dizziness in five patients and edema in one patient. In 28 patients, the focused echocardiography allowed to confirm the initial diagnosis: 19 patients with heart failure, five with acute coronary syndrome, two with pulmonary embolism and two patients with cardiac tamponade. In 17 patients, the echocardiography changed the diagnosis: ten with suspicious of heart failure, two with pulmonary embolism suspicious, two with hypotension without cause, one suspicious of acute coronary syndrome, one of cardiac tamponade and one of aortic dissection.
Conclusion
The focused echocardiography with pocket-size equipment in the emergency care may allow a prompt diagnosis and, consequently, an earlier initiation of the therapy.
Keywords: Echocardiography; Diagnostic Equipment, Emergency Medical Services; Diagnostic Imaging
Introduction
Emergency care services play an important role in the treatment of cardiac emergencies, such as acute coronary syndrome (ACS), aortic dissection, acute cardiac failure, arrhythmias, cardioembolic stroke, and cardiac tamponade; the rapid recognition and treatment of these conditions are fundamental to better outcomes1,2.
Data from the United States indicate that approximately 10% patients who seek these services present with chest pain or dyspnea3 as their chief complaint, and ischemic and nonischemic heart diseases are the leading causes of hospitalization after emergency care3. Although many advances have been made in diagnosing such conditions, some patients with ACS are discharged without receiving the correct diagnosis4, which consequently increases their mortality5,6.
Echocardiography is a noninvasive, low-cost and reproducible examination7 that has great diagnostic and prognostic value in patients with suspected ACS8 and acute cardiac failure2. It also assists in determining the appropriate therapy for patients with arrhythmias9,10.
Recent technological advances in the field of ultrasound have made it possible to build echocardiography equipment just slightly larger than a smart phone that fits in the pocket of a lab coat, permitting its quick use in an emergency at the patient's bedside.
The aim of this study was to describe our initial experience using an ultra-portable echocardiography device to perform focused cardiac ultrasound (FoCUS) in the emergency department; our objective was also to observe the number of cases in which the initial clinical diagnosis was confirmed or was altered after the cardiac ultrasound, and describe any technical difficulties related to the use of this device.
Methods
The patients in the study were adults who sought treatment from the emergency department in a tertiary hospital for the chief complaint of chest pain, dyspnea, or palpitations, and whose diagnosis was questioned after the initial assessment. The initial assessment consisted of the assessment the medical history, physical examination, electrocardiography (ECG) reading. Patients with known cardiac or pulmonary disease were excluded, as were those with ischemic changes in ECG (ST-segment depression or elevation) or fever (axillary temperature ≥ 37.8ºC).
All participants signed an informed consent form and the study was approved by the institution's Ethics Committee (process registration number 16723413.7.0000.5505).
Ultra-portable FoCUS
FoCUS scans were carried out using the ultra-portable Vscan device (GE Healthcare, Milwaukee, Wisconsin, USA) shown in Figure 1, and were performed by a single cardiologist. FoCUS scans were was carried out in a targeted manner and at the patient's bedside shortly after the initial clinical evaluation and ECG reading, with the goal of resolving doubts about the diagnosis. Subjective analysis was performed on the two-dimensional images and color flow mapping, focusing on the following aspects: the dimensions of the cavities, global systolic function, evaluation of segmental and global contractility of the left ventricle (LV), right ventricular systolic function, anatomical appearance of the mitral and aortic valves, presence of significant mitral and aortic valve regurgitation, presence of indirect signs of pulmonary hypertension (dilatation of the right chambers, bulging of the interventricular septum to the left, dilatation of the pulmonary trunk), presence of pericardial effusion, assessment of the dimensions of the thoracic aorta (ascending aorta and aortic arch), and presence of a dissection line.
Figure 1.
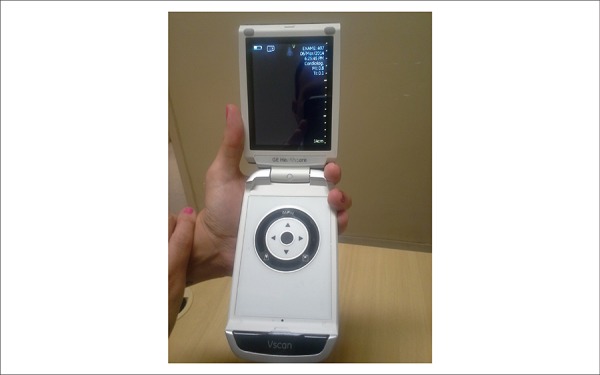
Vscan device (GE Healthcare) used in this study.
Statistical analysis
The statistical calculations were performed using Microsoft Excel 2010. Continuous data were presented as mean ± standard deviation and categorical data were presented as percentages.
Results
One hundred patients were evaluated: 54 were male, with an average age of 61 ± 17 years (range: 15-95 years).
The most common chief complaint among the study participants was chest pain (n = 52), followed by dyspnea (n = 32), palpitations (n = 10), dizziness/unease associated with hypotension (n = 5), and lower limb edema (n = 1), as can be seen in Table 1.
Table 1.
Chief complaint prompting patients to seek emergency care
| Chief complaint | n = 100 |
|---|---|
| Chest pain | 52 |
| Dyspnea | 32 |
| Palpitations | 10 |
| Dizziness/hypotension | 5 |
| Lower limb edema | 1 |
The most frequent diagnosis after assessment of medical history, physical examination, and ECG reading was of ACS (n = 51), followed by cardiac failure (n = 29), pulmonary embolism (n = 4), cardiac effusion or cardiac tamponade (n = 3), shock of undetermined etiology (n = 2), and aortic dissection (n = 1). In addition, in 10 patients with arrhythmias (seven with atrial fibrillation, two with ventricular tachycardia, and one with junctional tachycardia), FoCUS was used to assess LV systolic function to assist in guiding therapy (Table 2).
Table 2.
Main diagnostic hypotheses after assessment of medical history, physical examination, and ECG reading
| Initial Suspected Diagnosis | n = 100 |
|---|---|
| Acute coronary syndrome | 51 |
| Heart failure | 29 |
| Arrhythmia | 10 |
| Pulmonary embolism | 4 |
| Cardiac effusion/cardiac tamponade | 3 |
| Shock of undetermined etiology | 2 |
| Aortic dissection | 1 |
In all patients, it was possible to obtain good-quality images using the ultra-portable FoCUS device.
Of the 90 patients with uncertain initial diagnosis, the suspected clinical diagnosis at admission was confirmed using FoCUS in 28 (31%) of them (Table 3); 19 (68%) patients with cardiac failure, five (18%) with ACS, two (7%) with pulmonary embolism and two (7%) with cardiac tamponade.
Table 3.
Patients in whom the initial diagnosis was confirmed by ultra-portable cardiac ultrasound (n = 28)
| Definitive Final Diagnosis | |
|---|---|
| n (%) | |
| Heart failure | 19 (68) |
| Acute coronary syndrome | 5 (18) |
| Pulmonary embolism | 2 (7) |
| Cardiac tamponade | 2 (7) |
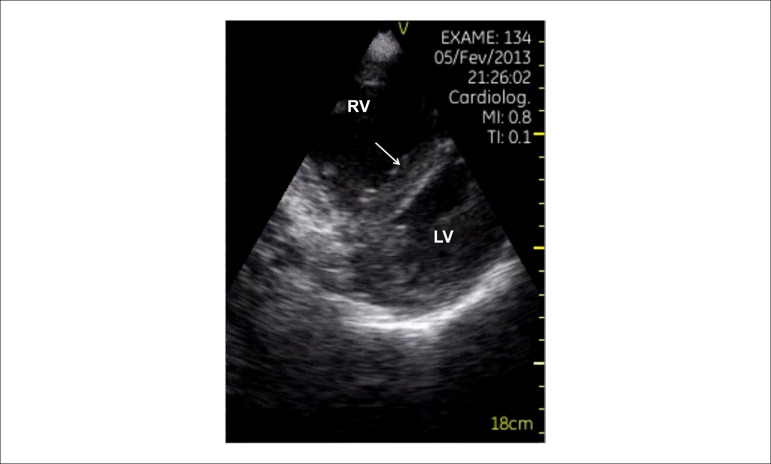
In one of the patients with cardiac failure and significant systolic dysfunction in LV, a blood clot was observed in the apical region of LV (Figures 2 - 4).
Figure 2.
Patient complaining of dyspnea. Portable cardiac ultrasound revealed dilated cardiomyopathy with systolic dysfunction of the left ventricle (LV) and a thrombus in apical region (arrow) in the apical window.
Figure 4.
Dilatation of the right ventricle (RV) and rectification of the interventricular septum in the parasternal view, in a patient with dyspnea and suspected pulmonary thrombosis.
Figure 3.
Significant pericardial effusion (DP) in the subcostal plane showing signs of restricted ventricular filling in a patient with cardiac tamponade. RV: right ventricle; LV: left ventricle.
Furthermore, of these 90 patients with uncertain diagnoses after initial assessment, FoCUS led to a change in the initial diagnosis in 17 (19%) of them (Table 4). In 10 patients with an initial suspected diagnosis of cardiac failure, the ultrasound showed neither systolic dysfunction nor indirect signs of diastolic dysfunction (enlarged left atrium or LV hypertrophy), although it was possible to identify other cardiac causes for the observed cardiac failure (hypertrophic cardiomyopathy and severe aortic stenosis) in two of these patients. In the remaining patients with suspicion of pulmonary embolism (two cases), shock of undetermined etiology (two cases), and cardiac tamponade (one case), FoCUS yielded normal results, ruling out cardiac causes. In the two patients with suspected pulmonary embolism, the suspected diagnosis was of intermediate level and with normal results from the FoCUS exam, this hypothesis was clinically discarded. In one patient with chest pain and suspected ACS, the ultrasound findings were compatible with pericarditis (pericardial thickening associated with discrete stroke); in one patient with suspected aortic dissection, no dilatation of the aorta, dissection lines, or aortic insufficiency were seen in the ultrasound; only significant LV hypertrophy was observed.
Table 4.
Patients in whom the diagnostic hypothesis was changed after ultra-portable cardiac ultrasound (n = 17)
| Initial diagnostic hypothesis | Diagnosis after ultrasound |
|---|---|
| Heart failure (n = 10) | COPD (n = 4) |
| ARF with hypervolemia (n = 2) | |
| Pneumonia (n = 1) | |
| Severe aortic stenosis (n = 1) | |
| Hypertrophic cardiomyopathy (n = 1) | |
| Anxiety (n = 1) | |
| Pulmonary embolism (n = 2) | COPD (n =1) |
| Pneumonia (n =1) | |
| Shock of undetermined etiology (n = 2) | Septic shock (n = 2) |
| Acute coronary syndrome (n = 1) | Pericarditis |
| Cardiac tamponade (n = 1) | Dehydration |
| Aortic dissection (n = 1) | Postprandial angina |
COPD: chronic obstructive pulmonary disease; ARF: acute renal failure.
Of the 10 patients who arrived at the emergency department with sudden-onset symptomatic arrhythmias (seven with atrial fibrillation, two with ventricular tachycardia, and one with junctional tachycardia), LV systolic dysfunction was observed in four, atrial fibrillation in two, and ventricular tachycardia in two; the remainder showed normal systolic LV function.
In 45 (50%) of the 90 patients with uncertain diagnoses after the initial assessment, the ultra-portable FoCUS did not yield data that confirmed or changed the initial diagnostic hypothesis, and other supporting examinations were necessary.
Discussion
This study allowed us to demonstrate the great utility of cardiac ultrasound done with ultra-portable equipment at the bedside in a clinical emergency department. It was performed in patients who had no certain diagnosis after assessment of the medical history, physical examination, and ECG reading. The ultra-portable FoCUS allowed to confirm diagnosis of 31% patients, and led to a change in the original diagnosis in 19% patients.
The greatest clinical benefit of using FoCUS in this sample was the confirmation or ruling out of the diagnosis of cardiac failure due to LV dysfunction, because it was possible to diagnose other cardiac diseases (aortic stenosis and hypertrophic cardiomyopathy) as the cause of cardiac failure in two patients.
In patients with suspected pulmonary embolism, FoCUS permitted a faster diagnosis in approximately half the patients, and consequently therapy was initiated more quickly. The cases with suspected cardiac tamponade were similar: two of three patients had their diagnosis confirmed quickly, and pericardial fluid was drained sooner.
In 10% patients with chest pain and suspected ACS, where ECG reading did not prove the diagnosis, FoCUS showed evidence of contractile segment changes.
This finding, in a patient with a clinical history compatible with myocardial ischemia and no history of prior coronary disease, can be used to confirm the clinical diagnosis of ACS. Furthermore, in one patient, FoCUS showed signs of pericarditis, changing the initial diagnostic hypothesis. Although the percentage of patients with chest pain, normal ECG, and changes in the contractile segments in the ultrasound was small, this population is frequently seen in emergency services and there is clear evidence that faster treatment of ACS leads to lower morbidity and mortality1. Consequently, this diagnostic tool is of great importance for these patients.
The use of FoCUS in this sample was also important in assessing LV function in patients who arrived with paroxysmal arrhythmias. Especially in atrial fibrillation, the choice of medication for controlling heart rate and pharmacological cardioversion should take into account the presence or absence of LV dysfunction10.
The possibility of quickly confirming or excluding a diagnosis in severe cases without needing to wait for more complex and more time-consuming tests that are not always immediately available in emergency departments is essential, because it allows for early treatment of serious illnesses, such as ACS, aortic dissection, acute cardiac failure, pulmonary embolism, and cardiac tamponade.
In addition, the fact that the examination can be carried out at the bedside in a timely manner, with an easily transportable device and with no need for patient transport, provides the ultra-portable equipment with a unique advantage in rapidly clarifying specific issues and streamlining care in emergency departments. Furthermore, FoCUS allowed significant numbers of patients to avoid unnecessary and, at times, potentially harmful therapy.
Despite great laboratorial and technical advances, there are still difficulties in the rapid diagnosis of acute and potentially fatal cardiovascular diseases. Approximately 2%-8% patients with ACS are discharged from emergency departments without the correct diagnosis4, resulting in increased mortality5,6.
Dyspnea is an important symptom that drives patients to seek emergency medical care, and rapid diagnosis of the cause is required11. The main causes of dyspnea in these patients are cardiac or pulmonary in origin12; however, it is difficult to distinguish between these causes, and the clinical history and physical examination are inconclusive in several cases13,14. Although a diagnosis of acute cardiac failure can be made clinically in most cases, a diagnostic doubt may remain in some cases. In this study, the FoCUS allowed for the rapid confirmation or exclusion of the heart as the cause of dyspnea, without the need for time-consuming or detailed diagnostics, such as the evaluation of brain natriuretic peptide (BNP) levels.
Recent studies with the ultra-portable device also demonstrated its usefulness for clinical diagnosis, although they included stable patients who were hospitalized.
A Norwegian study that included patients admitted to an internal medicine ward, evaluated the use of the device and noted a change in initial diagnosis in 18% patients15, a result similar to the one seen in this study; however, the studies were performed with populations with different diseases. FoCUS has also been tested as a tool for resolving clinical doubts in patients admitted to cardiology wards, where it provided good results for most patients in whom it was used, and also was consistent with conventional Doppler echocardiography16. Moreover, in the outpatient setting, FoCUS improved the diagnostic accuracy of medical histories and physical examinations in patients with various diseases17. It is important to note that, unlike in the present study, in the cited studies, the FoCUS ultrasound was performed by physicians, not ultrasound technicians, indicating that FoCUS does not need to be performed by a specialist.
In contrast with previous studies15-17, this was the first study to use ultra-portable FoCUS only in patients who were seen in the emergency department shortly after the assessment of medical history, physical examination, and ECG reading. Furthermore, this study was conducted in a clinical emergency department in a tertiary general hospital that comprised patients with acute clinical disease of various etiologies (cardiac or otherwise). This excluded the bias involved with an exclusive cardiac emergency ward, where most patients have acute cardiovascular diseases.
FoCUS ultrasound should not be considered a complete Doppler echocardiographic examination18,19, and should be used as a tool to assess heart disease in the population20 or as a complement to physical examination17,18, as a targeted examination that addresses a specific concern and improves diagnostic speed and accuracy18, exactly as shown in the results of the present study. The aim of performing FoCUS in an emergency scenario is to speed up the main diagnosis, especially when a complete echocardiogram is not immediately feasible. The majority of patients undergoing FoCUS will require a conventional echocardiogram, along with all the structural and hemodynamic measurements offered by this diagnostic, to fine-tune therapy and for medium and long term follow-up.
The ultra-portable device used in this study proved to be effective for obtaining good two-dimensional images and good-quality color flow mapping. The device allowed performing some linear measurements, but cavity measurements were not obtained in our study. The device does not allow measurements of area and volume, and also does not have continuous or pulsed Doppler; thus, it limits objective measurements, such as LV ejection fraction (Simpson method) or the quantification of valvular stenosis/insufficiency.
Consequently, this study demonstrated that the use of FoCUS in a clinical emergency department allowed for the rapid confirmation or exclusion of diagnostic hypotheses in cases where there was doubt regarding the diagnosis after the assessment of medical history, physical examination, and ECG reading.
Limitations
This was a descriptive study that did not compare FoCUS with a conventional examination. However, this comparison has already been made in previous studies, validating the use of this new diagnostic tool16,17,21-23.
The examinations in this study were performed by a single cardiologist with experience in echocardiography. However, several previous studies have shown that FoCUS performed by physicians who are not specialists in echocardiography is accurate as a complementary investigation to physical examination15-17,21-27. In addition, it has been demonstrated that nonspecialist physicians can undergo a brief training to learn how to perform FoCUS24,28.
Conclusion
Ultra-portable cardiac ultrasound used in an emergency department aided in quickly confirming or ruling out clinical diagnoses and, consequently, beginning treatment more quickly and avoiding inappropriate therapy for incorrect diagnoses. Because this is a descriptive study, it is necessary to perform comparative and randomized studies to confirm these results.
Footnotes
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conception and design of the research: Mancuso FJN, Siqueira VN, Gois AFT, Carvalho ACC, Campos O; Acquisition of data and Statistical analysis: Mancuso FJN; Analysis and interpretation of the data: Mancuso FJN, Siqueira VN, Moisés VA; Writing of the manuscript: Mancuso FJN, Siqueira VN, Moisés VA, Campos O; Critical revision of the manuscript for intellectual content: de Paola AAV, Carvalho ACC.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Piegas LS, Feitosa G, Mattos LA, Nicolau JC, Rossi JM, Neto, Timerman A, et al. Sociedade Brasileira de Cardiologia Diretriz da Sociedade Brasileira de Cardiologia sobre tratamento do infarto agudo do miocárdio com supradesnível do segmento ST. Arq Bras Cardiol. 2009;93(6) supl. 2:e179–e264. [PubMed] [Google Scholar]
- 2.Montera MW, Almeida RA, Tinoco EM, Rocha RM, Moura LZ, Réa-Neto A, et al. Sociedade Brasileira de Cardiologia II Diretriz brasileira de insuficiência cardíaca aguda. Arq Bras Cardiol. 2009;93(3) supl.3:1–65. [PubMed] [Google Scholar]
- 3.Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008;(7):1–38. [PubMed] [Google Scholar]
- 4.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics-2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. Erratum in: Erratum in: Circulation. 2010;121(12):e260. [DOI] [PubMed] [Google Scholar]
- 5.Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342(16):1163–1170. doi: 10.1056/NEJM200004203421603. [DOI] [PubMed] [Google Scholar]
- 6.Swanson N, Montalescot G, Eagle KA, Goodman SG, Huang W, Brieger D, et al. Global Registry of Acute Coronary Events Investigators Delay to angiography and outcomes following presentation with high-risk, non-ST-elevation acute coronary syndromes: results from the global registry of acute coronary events. Heart. 2009;95(3):211–215. doi: 10.1136/hrt.2008.149922. [DOI] [PubMed] [Google Scholar]
- 7.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Nicolau JC, Timerman A, Piegas LS, Marin-Neto JA, Rassi A., Jr Guidelines for Unstable Angina and Non-ST-Segment Elevation Myocardial Infarction of the Brazilian Society of Cardiology (II Edition, 2007) Arq Bras Cardiol. 2007;89(4):e89–e131. doi: 10.1590/s0066-782x2007001600015. [DOI] [PubMed] [Google Scholar]
- 9.Zimerman LI, Fenelon G, Martinelli M, Filho, Grupi C, Atié J, Lorga A, Filho, et al. Sociedade Brasileira de Cardiologia Diretrizes brasileiras de fibrilação atrial. Arq Bras Cardiol. 2009;92(6) supl.1:1–39. [Google Scholar]
- 10.Scanavacca MI, Brito FS, Maia I, Hachul D, Gizzi J, Lorga A, et al. Sociedade Brasileira de Cardiologia. Sociedade Brasileira de Cirurgia Cardiovascular. Departamento de Estimulação Cardíaca Artificial (DECA) da SBCCV Diretrizes para avaliação e tratamento de pacientes com arritmias cardíacas. Arq Bras Cardiol. 2002;79(5):1–50. [PubMed] [Google Scholar]
- 11.Wang CS, Fitzgerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294(15):1944–1956. doi: 10.1001/jama.294.15.1944. [DOI] [PubMed] [Google Scholar]
- 12.Morrison LK, Harrison A, Krishnaswamy P, Kazanegra R, Clopton P, Maisel A. Utility of a rapid B-natriuretic peptide assay in differentiating congestive heart failure from lung disease in patients presenting with dyspnea. J Am Coll Cardiol. 2002;39(2):202–209. doi: 10.1016/s0735-1097(01)01744-2. [DOI] [PubMed] [Google Scholar]
- 13.Mulrow C, Lucey C, Farnett L. Discriminating causes of dyspnea through the clinical examination. J Gen Intern Med. 1993;8(7):383–392. doi: 10.1007/BF02600079. [DOI] [PubMed] [Google Scholar]
- 14.Schmitt B, Kushner M, Wiener S. The diagnostic usefulness of history of the patient with dyspnea. J Gen Intern Med. 1986;1(6):386–393. doi: 10.1007/BF02596424. [DOI] [PubMed] [Google Scholar]
- 15.Mjolstad OC, Dalen H, Graven T, Kleinau JO, Salvesen O, Haugen BO. Routinely adding ultrasound examinations by pocket-sized ultrasound devices improves inpatient diagnostics in a medical department. Eur J Intern Med. 2012;23(2):185–191. doi: 10.1016/j.ejim.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Gianstefani S, Catibog N, Whittaker AR, Ioannidis AG, Vecchio F, Wathen PT, et al. Pocket-size imaging device: effectiveness for ward-based transthoracic studies. Eur Heart J Cardiovasc Imaging. 2013;14(12):1132–1139. doi: 10.1093/ehjci/jet091. [DOI] [PubMed] [Google Scholar]
- 17.Galderisi M, Santoro A, Versiero M, Lomoriello VS, Esposito R, Raia R, et al. Improved cardiovascular diagnostic accuracy by pocket size imaging device in non-cardiologic outpatients: the NaUSiCa (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound. 2010;8:51. doi: 10.1186/1476-7120-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sicari R, Galderisi M, Voigt JU, Habib G, Zamorano JL, Lancelotti P, et al. The use of pocket-size imaging devices: a position statement of the European Association of Echocardiography. Eur J Echocardiogr. 2011;12(2):85–87. doi: 10.1093/ejechocard/jeq184. [DOI] [PubMed] [Google Scholar]
- 19.Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the american society of echocardiography. J Am Soc Echocardiogr. 2013;26(6):567–581. doi: 10.1016/j.echo.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 20.Egan M, Ionescu A. The pocket echocardiograph: a useful new tool? . Eur J Echocardiogr. 2008;9(6):721–725. doi: 10.1093/ejechocard/jen177. [DOI] [PubMed] [Google Scholar]
- 21.Prinz C, Voigt JU. Diagnostic accuracy of a hand-held ultrasound scanner in routine patients referred for echocardiography. J Am Soc Echocardiogr. 2011;24(2):111–116. doi: 10.1016/j.echo.2010.10.017. [DOI] [PubMed] [Google Scholar]
- 22.Prinz C, Dohrmann J, van Buuren F, Bitter T, Bogunovic N, Horstkotte D, et al. The importance of training in echocardiography: a validation study using pocket echocardiography. J Cardiovasc Med (Hagerstown) 2012;13(11):700–707. doi: 10.2459/JCM.0b013e328356a55f. [DOI] [PubMed] [Google Scholar]
- 23.Prinz C, Dohrmann J, van Buuren F, Bitter T, Bogunovic N, Horstkotte D, et al. Diagnostic performance of handheld echocardiography for the assessment of basic cardiac morphology and function: a validation study in routine cardiac patients. Echocardiography. 2012;29(8):887–894. doi: 10.1111/j.1540-8175.2012.01728.x. [DOI] [PubMed] [Google Scholar]
- 24.Cardim N, Fernandes Golfin C, Ferreira D, Aubele A, Toste J, Cobos MA. Usefulness of a new miniaturized echocardiographic system in outpatient cardiology consultations as an extension of physical examination. J Am Soc Echocardiogr. 2011;24(2):117–124. doi: 10.1016/j.echo.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 25.Mayo PH. Training in critical care echocardiography. Ann Intensive Care. 2011;1:36. doi: 10.1186/2110-5820-1-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spevack DM, Tunick PA, Kronzon I. Hand carried echocardiography in the critical care setting. Echocardiography. 2003;20(5):455–461. doi: 10.1046/j.1540-8175.2003.03083.x. [DOI] [PubMed] [Google Scholar]
- 27.Spurney CF, Sable CA, Berger JT, Martin GR. Use of a hand-carried ultrasound device by critical care physicians for the diagnosis of pericardial effusions, decreased cardiac function, and left ventricular enlargement in pediatric patients. J Am Soc Echocardiogr. 2005;18(4):313–319. doi: 10.1016/j.echo.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 28.Siqueira VN, Mancuso FJ, Campos O, Carvalho AC, de Paola AA, Moises VA. Results of a 30 days training of cardiology residents to perform focused cardiac ultrasound examination with hand-carried cardiac ultrasound device. J Am Soc Echocardiogr. 2013;26(6):B62. doi: 10.1111/echo.12887. [DOI] [PubMed] [Google Scholar]