Abstract
Immunoprecipitin detection (IPD) is the current reference confirmatory technique for anti-Aspergillus antibody detection; however, the lack of standardization is a critical drawback of this assay. In this study, we evaluated the performance of the Aspergillus Western blot (Asp-WB) IgG kit (LDBio Diagnostics, Lyon, France), a recently commercialized immunoblot assay for the diagnosis of various clinical presentations of chronic aspergillosis. Three hundred eight serum samples from 158 patients with aspergillosis sensu lato (s.l.) were analyzed. More specifically, 267 serum samples were derived from patients with Aspergillus disease, including 89 cases of chronic pulmonary aspergillosis, 10 of aspergilloma, and 32 of allergic bronchopulmonary aspergillosis, while 41 samples were from patients with Aspergillus colonization, including 15 cystic fibrosis (CF) and 12 non-CF patients. For blood donor controls, the Asp-WB specificity was 94%, while the kit displayed a sensitivity for the aspergillosis s.l. diagnosis of 88.6%, with a diagnostic odds ratio (DOR) of 119 (95% confidence interval [CI], 57 to 251). The DOR values were 185.22 (95% CI,78.79 to 435.45) and 43.74 (95% CI, 15.65 to 122.20) for the diagnosis of Aspergillus disease and Aspergillus colonization, respectively. Among the patients, the sensitivities of the Asp-WB in the diagnosis of Aspergillus colonization were 100% and 41.7% in CF and non-CF patients, respectively. The Asp-WB yielded fewer false-negative results than did IPD. In conclusion, the Asp-WB kit performed well for the diagnosis of various clinical presentations of aspergillosis in nonimmunocompromised patients, with an enhanced standardization and a higher sensitivity than with IPD, which is the current reference method.
INTRODUCTION
The various clinical presentations of aspergillosis primarily depend on host immune system efficiency (1, 2). One of the most frequent presentations is chronic pulmonary aspergillosis (CPA). This disease affects approximately 3 million, mostly immunocompetent, individuals worldwide, with a 20% to 33% mortality rate during the initial treatment and a 50% 5-year mortality rate (3, 4). It has been estimated that CPA causes approximately 450,000 deaths per year (see http://www.life-worldwide.org/fungal-diseases/chronic-pulmonary-aspergillosis/). However, the aspergillosis diagnosis relies on a body of evidence, including nonspecific clinical signs, radiological findings, and biological diagnostic test results. Therefore, the accurate diagnosis of aspergillosis currently remains a challenging issue in clinical mycology (1, 2, 5, 6). Among the diagnostic tests, serological assays that aim to detect antibodies directed against the infecting fungus in host serum are particularly relevant for the diagnosis of CPA in immunocompetent patients (5, 7). Although enzyme-linked immunosorbent assays (ELISAs) are widely used to detect specific anti-Aspergillus antibodies, immunoprecipitin detection (IPD) is currently considered the reference assay (5, 6, 8, 9). However, several drawbacks associated with IPD have also been described, including protracted results, extended turnaround times, and poor standardization, thereby limiting the possibility of result comparison (6, 8). The interlaboratory reproducibility, as IPD procedures differ between laboratories, and intralaboratory interreader reproducibility of IPD results are relatively poor (6, 8). Therefore, the disparity between the limited performance of reference diagnostic assays in the clinic and the severity of CPA is striking.
A new assay for aspergillosis diagnosis based on immunoblotting technology, the Aspergillus Western blot IgG kit (Asp-WB), has recently been commercialized (LDBio Diagnostics, Lyon, France). Commercial Western blot tests are commonly used for the diagnosis of infectious diseases, such as toxoplasmosis and HIV (10, 11); however, such tests for aspergillosis diagnosis were unavailable until recently. In contrast to IPD, Western blot assays are convenient, standardized, automatable, and easy to use and interpret. In this study, we evaluated the performance of the Asp-WB kit regarding the diagnosis of different presentations of pulmonary aspergillosis in nonimmunocompromised patients.
(This study's results were presented in part at the 23rd European Congress of Clinical Microbiology and Infectious Diseases [ECCMID], 27 to 30 April 2010, Berlin, Germany.)
MATERIALS AND METHODS
Patients and sera.
Sera were collected from a random sample of independent randomly selected blood donors (considered healthy controls) and patients complying with the inclusion criteria of the various clinical presentations of aspergillosis, as detailed in Table 1. Patient sera included in the study were stored at −20°C in the mycology laboratories at four French university hospitals, located in St. Etienne (St. E), Grenoble (G), Marseille (M), and Saint Antoine, Paris (St. A). The patients who matched with the case definition criteria were included (as detailed in Table 1).
TABLE 1.
Details of the diagnostic criteria for various clinical presentations of aspergillosis included in the study
| Groupa | Criteria |
|---|---|
| Aspergillus disease | |
| CPA | (i) Abnormal radiological/CT scan images |
| (ii) Alteration of the patient's general state | |
| (iii) Aspergillus sp.-positive culture (±3 mo) from respiratory sample or biopsy specimen and/or Aspergillus fumigatus precipitin IgG | |
| Aspergilloma | (i) Radiological/CT scan Monad's sign |
| (ii) No deterioration of the patient's general state | |
| (iii) Aspergillus sp.-positive culture (±3 mo) from respiratory sample or biopsy specimen and/or Aspergillus fumigatus precipitin IgG | |
| ABPAb | (i) Degradation of respiratory functions |
| (ii) Global IgE level of ≥1,000 kIU/liter | |
| (iii) Aspergillus-specific IgE level of ≥0.7 kIU/liter | |
| (iv) Global IgE level of ≥500 kIU/liter | |
| (v) Aspergillus sp.-positive culture (±3 mo) and/or Aspergillus fumigatus precipitin IgG and/or an abnormal radiological status | |
| Colonization | |
| Aspergillus colonization | (i) Two Aspergillus sp.-positive cultures from respiratory samples collected between ≥10 days apart and ≤6 mo apart |
| (ii) No Aspergillus disease criterion | |
| Control | |
| Blood donors | Randomly selected blood donor sera |
The Aspergillus disease and Aspergillus colonization groups are included in the aspergillosis sensu lato group. CPA, chronic pulmonary aspergillosis; ABPA, allergic bronchopulmonary aspergillosis; CT, computed tomography.
Criteria i, ii, and iii or i, iii, iv, and v are mandatory.
Case definitions.
Patient classification served to assess the test diagnostic indices for each clinically relevant subpopulation. Therefore, aspergillosis sensu lato (s.l.) patients were divided into one of two groups, the Aspergillus disease or Aspergillus colonization group, based on clinical, radiological, mycological, and serological criteria (Table 1). These criteria are a combination of those used in each of the participating centers (12–14) and those described in the literature (1, 2, 15). The first group, referred to as the Aspergillus disease group, was further subdivided into the CPA, uncomplicated aspergilloma, or allergic bronchopulmonary aspergillosis (ABPA) group. The second group, referred to as Aspergillus colonization, was further subdivided according to the cystic fibrosis (CF) status of the patient.
Serological analyses. (i) Immunoprecipitin detection test.
IPD was performed on samples from aspergillosis s.l. patients according to the routine procedures in each participating center; the immunoelectrophoresis assays were performed using Aspergillus fumigatus antigen, with either an in-house antigen (16) for G or a commercialized antigen by Bio-Rad (France) for M and St. E or Microgen bioproduct (United Kingdom) for St. A.
(ii) Aspergillus Western blot IgG kit.
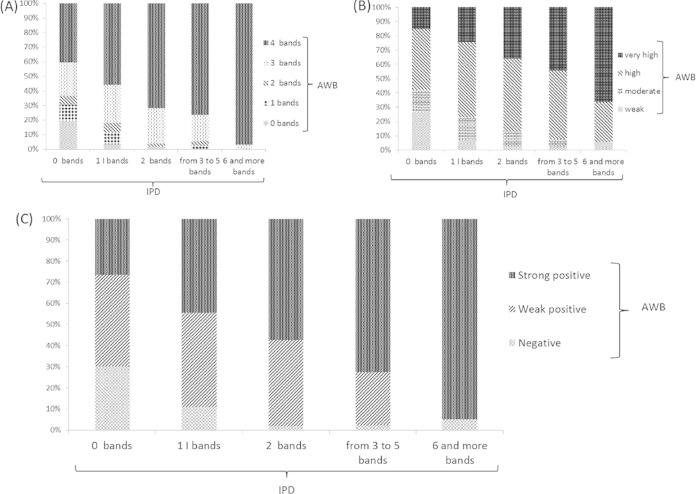
Each serum was tested using the Asp-WB IgG kit (LDBio Diagnostics, Lyon, France) according to the manufacturer's instructions. Briefly, 1.2 ml of sample buffer was dispensed into each channel of an incubation tray. Strips were placed into the incubation tray, and 10 μl of serum was dispensed following the distribution plan and incubated for 90 min under agitation. For each test, a positive control supplied by the manufacturer was used. After 3 washes with the wash buffer diluted 1/10, 1.2 ml of IgG conjugate was distributed into each channel, and the strips were incubated for 60 min. After another wash step, 1.2 ml of substrate was dispensed and incubated for 60 min, depending on the strip coloration. Each strip was left to dry at ambient temperature for at least 15 min. The result was then compared with the positive control and interpreted as either positive or negative according to the manufacturer's recommendations. Four protein bands at 16, 18 to 20, 22, and 30 kDa have been shown to be specific for Aspergillus sensitization. The Asp-WB assay was considered positive when at least two of these bands were present (Fig. 1A). The Asp-WB global intensity was also quantified by summing the intensity results of each specific band, which was scored from 1 to 4 (Fig. 1B). Asp-WB intensity was then categorized as weak (<2), moderate (2 to 4), high (5 to 10), and very high (>10). Each Asp-WB test was performed in duplicate and read by two experts. A panel of eight quality-control serum samples (highly positive human serum sample diluted in buffer with preservative), showing different specific profiles, was tested to control inter- and intralot reproducibility.
FIG 1.
Asp-WB results. (A) C+, positive control; values on next to the arrows indicate the mass (in kDa) of the specific bands. NC, negative control. (B) Quantification of Asp-WB band intensity in a positive assay. The intensities of four specific bands were 2, 4, 3, and 3, respectively, yielding a total intensity of 12.
Statistical analyses. (i) Asp-WB diagnostic indices.
Blood donor sera were used to determine Asp-WB specificity. As some patients provided multiple serum samples, Asp-WB sensitivity and other diagnostic indices were calculated considering either the result for a patient or a serum sample, for all aspergillosis s.l. patients, and for each group of patients. In the patient-based analysis, the test was considered positive if at least one of the patient's sera yielded a positive result; the denominator was the number of patients included. The serum-based analysis did not allow for intrapatient correlation, and the result of each serum was considered independent; the denominator was the number of samples included. The complementary diagnostic indices, including the diagnostic odds ratio (DOR) and the Yule Q coefficient (interpreted as null [0], negligible [0.01 to 0.09], light [0.10 to 0.29], moderate [0.30 to 0.49], strong [0.50 to 0.69], and very strong [0.70 to 1]) were calculated for aspergillosis s.l., Aspergillus disease, and Aspergillus colonization.
(ii) Asp-WB and IPD agreement.
Asp-WB result patterns were analyzed, and concordance with IPD was evaluated. The concordance between the Asp-WB and IPD results was assessed via global agreement, and Cohen's kappa coefficient was used to estimate the strength of agreement. Cohen's kappa coefficient was interpreted as slight (0 to 0.20), fair (0.21 to 0.40), moderate (0.41 to 0.60), substantial (0.61 to 0.80), and almost perfect (0.81 to 1) agreement. The proportions of Asp-WB band detection and intensity were determined for each IPD band profile. To produce semiquantitative WB results, the Asp-WB results were categorized as negative, weak positive, or strong positive (Table 2), by combining both the number and intensity data of the specific bands. The correlation between the semiquantitative Asp-WB results and the number of IPD bands was measured using Spearman's rank correlation coefficient.
TABLE 2.
Details of semiquantification of the Asp-WB results
| No. of bands | Resultsa |
||
|---|---|---|---|
| Negative | Weak positive | Strong positive | |
| 0–1 | NA | NA | NA |
| 2 | NA | 2 ≤ I ≤ 4 | 4 < I |
| 3 | NA | 3 ≤ I ≤ 6 | 6 < I |
| 4 | NA | 4 ≤ I ≤ 8 | 8 < I |
Results are from the combination of the number of 16-, 18- to 20-, 22-, and 30-kDa Aspergillus-specific bands detected and the sum of each detected band's intensity (I) relative to the positive control, as illustrated in Fig. 1B. NA, not available.
RESULTS
Patients and sera.
A panel of 212 independent blood donor serum samples and 308 serum samples from 158 patients (as defined in Table 1) was analyzed. The mean number of samples per patient was 1.95 (ranging from 1 to 4). Depending on their clinical characteristics, each patient was categorized into one of the various clinical presentations of aspergillosis defined in Table 1. Accordingly, 267 serum samples were derived from 131 patients with Aspergillus disease, including 197 from 89 patients with CPA, 13 from 10 patients with aspergilloma, and 57 from 32 patients with ABPA. The 41 serum samples from patients with Aspergillus colonization included 18 from 15 CF patients and 23 from 12 non-CF patients.
Asp-WB diagnostic indices.
Thirteen of the 212 blood donor control serum samples tested positive (8 and 5 were classified as weak and strong positive, respectively); therefore, the specificity of the Asp-WB assay was 93.9% (95% confidence interval [CI],89.7% to 96.7%) for this group. The other Asp-WB diagnostic indices were calculated for the patient- and serum-based analyses.
Patient-based analysis.
The Asp-WB diagnostic indices considering patient diagnosis are shown in Table 3. The sensitivity of the Asp-WB aspergillosis s.l. diagnosis was 88.6%. The Asp-WB sensitivity was 91.6% and 74.1% in the CPA and Aspergillus colonization groups, respectively. Asp-WB sensitivity in the diagnosis of patients with Aspergillus disease reached 90.0%, 91.0%, and 93.8% for the diagnoses aspergilloma, CPA, and ABPA, respectively. For patients with Aspergillus colonization, the sensitivity of Asp-WB was 41.7% and 100% in non-CF and CF patients, respectively. The Yule Q coefficient ranged from 0.96 to 0.99, and the DOR ranged from 43.7 (95% CI, 15.7 to 122.2 ) to 185.2 (95% CI, 79.8 to 435.5), thereby indicating that the Asp-WB kit exhibited good diagnostic performance (Table 3).
TABLE 3.
Patient- and serum-based Asp-WB kit diagnostic indices according to the various clinical presentations of aspergillosis
| Group | n |
Asp-WB diagnostic indices |
Asp-WB versus IPD* |
||||
|---|---|---|---|---|---|---|---|
| Sensitivity (% [95% CI]) | Yule Q (95% CI) | DOR (95% CI) | IPDb sensitivity (% [95% CI]) | Agreement (% [95% CI]) | Cohen's kappa (95% CI) | ||
| Patient-based analysis | |||||||
| Aspergillus disease | 131 | 91.6 (0.89–0.94) | 0.99 (0.98–0.99) | 185.22 (78.79–435.45) | 86.3 (0.83–0.89) | 84.0 (0.81–0.87) | 0.192 (0.027–0.357) |
| CPA | 89 | 91.0 | 87.6 | 87.6 | |||
| Aspergilloma | 10 | 90.0 | 100.0 | 90.0 | |||
| ABPA | 32 | 93.8 | 78.1 | 71.9 | |||
| Aspergillus colonization | 27 | 74.1 (0.66–0.82) | 0.96 (0.94–0.97) | 43.74 (15.65–122.20) | 59.3 (0.50–0.69) | 77.8 (0.70–0.86) | 0.512 (0.155–0.869) |
| Cystic fibrosis positive | 15 | 100.0 | 73.3 | 73.3 | |||
| Cystic fibrosis negative | 12 | 41.7 | 41.7 | 83.3 | |||
| Aspergillosis sensu latoa | 158 | 88.6 (0.86–0.91) | 0.98 (0.98–0.99) | 119.06 (56.50–250.90) | 81.6 (0.79–0.85) | 82.9 (0.80–0.86) | 0.332 (0.182–0.482) |
| Serum-based analysis | |||||||
| Aspergillus disease | 267 | 94.0 (0.93–0.95) | 0.99 (0.99–1.00) | 299.09 (135.62–659.57) | 87.6 (0.86–0.90) | 86.1 (0.84–0.88) | 0.21 (0.10–0.31) |
| CPA | 197 | 93.4 | 87.3 | 82.5 | |||
| Aspergilloma | 13 | 92.3 | 100.0 | 92.3 | |||
| ABPA | 57 | 96.5 | 86.0 | 86.8 | |||
| Aspergillus colonization | 41 | 73.2 (0.66–0.80) | 0.95 (0.94–0.97) | 41.75 (17.14–101.66) | 53.7 (0.46–0.61) | 75.6 (0.69–0.82) | 0.50 (0.22–0.78) |
| Cystic fibrosis positive | 18 | 100.0 | 72.2 | 72.2 | |||
| Cystic fibrosis negative | 23 | 52.2 | 39.1 | 78.3 | |||
| Aspergillosis sensu latoa | 308 | 91.2 (0.90–0.93) | 0.99 (0.98–0.99) | 159.31 (80.22–316.40) | 83.1 (0.81–0.85) | 84.7 (0.83–0.87) | 0.35 (0.25–0.45) |
The Aspergillus disease and Aspergillus colonization groups are included in the aspergillosis sensu lato group.
IPD, immunoprecipitin detection assay.
Serum-based analysis.
The results of the serum-based analysis are given in Table 3. Overall, they were similar to those of the patient-based analysis, although the Asp-WB diagnostic indices were higher in the serum-based analysis than in the patient-based analysis.
Asp-WB and IPD agreement.
Importantly, IPD results were available for the patients but not for the healthy controls. Furthermore, although IPD results were included in the patient diagnostic criteria, it is worth noting that, in both patient- and serum-based analyses, the true-positive rate was higher for Asp-WB than for IPD for the diagnosis of aspergillosis s.l., Aspergillus disease, and Aspergillus colonization (Table 3). The agreement between Asp-WB and IPD ranged from 76% to 86%, and the Cohen's kappa coefficient indicated a slight to moderate concordance between the two assays depending on the patient diagnosis in both the patient- and the serum-based analyses (Table 3).
Asp-WB banding pattern analysis.
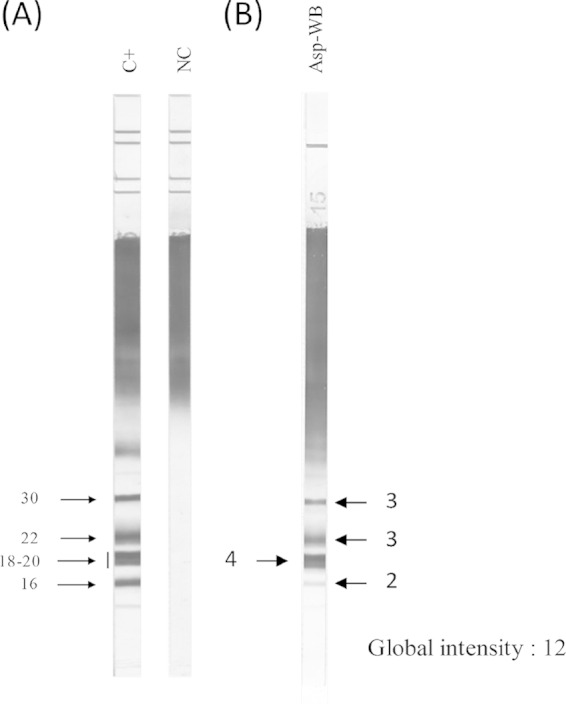
At least three specific Asp-WB bands were observed in 84% of the aspergillosis s.l. serum WB profiles. Compared with IPD (Fig. 2A), the number of bands increased with the number of IPD bands so that 100% of the sera with at least 6 precipitin lines displayed at least 3 Asp-WB bands. The same trend was observed when considering the global Asp-WB band intensity (Fig. 2B); 94% of the sera with at least 3 precipitin lines had high or very high Asp-WB banding pattern intensities. To interpret the Asp-WB results in a semiquantitative manner, the Asp-WB results were classified into three categories, depending on intensity and band number, as described in Materials and Methods. Among the aspergillosis s.l. serum samples, 28 were classified as negative, 96 were classified as weak positive, and 176 were classified as strong positive. In agreement with the findings described above, the Asp-WB semiquantitative results correlated (r = 0.77) with the IPD banding pattern, as depicted in Fig. 2C.
FIG 2.
(A) Repartition of Asp-WB banding profile according to immunoprecipitin (IPD) band number. (B) Repartition of Asp-WB global intensity according to IPD banding profile. (C) Repartition of Asp-WB categories (combining band numbers and intensities) according to IPD banding profile.
DISCUSSION
The main findings of the study were the relatively high sensitivity of the detection of specific bands with the evaluated Aspergillus-specific IgG Western blot detection kit for the diagnosis of aspergillosis in nonimmunocompromised patients and the lack of correlation between any particular banding feature and clinical presentations of aspergillosis. A major advantage of using a commercialized kit is the uniformity of reagents. Indeed, the standardization of diagnostic tests is critical when epidemiological studies and therapeutic trials evaluating diagnostic or therapeutic strategies for aspergillosis treatment require multicenter enrollment. Furthermore, the turnaround time for results is shorter with Asp-WB assays (∼4 h) than with IPD assays (∼24 to 36 h). The sensitivity and diagnostic performance of the Asp-WB assay was highlighted in both the serum- and the patient-based analyses, as evaluated by the DOR and Yule Q coefficient values. The slight concordance between the Asp-WB and IPD results (Table 3) may be at least partly explained by the heterogeneity of the IPD assays used in each of the four centers. Our objective was to evaluate the diagnostic indices of this WB test for the diagnosis of various presentations of aspergillosis and not to compare the WB with the immunoprecipitin test. Yet, in patients with various clinical presentations of aspergillosis, it was noticeable that, although IPD results were included in the case definition criteria, there were fewer false-negative results with the Asp-WB assay than with the IPD assay. One exception concerned the diagnosis of aspergilloma (Table 3), in which all patients had a positive IPD result and one had a false-negative Asp-WB result with only one intense (grade 3 on an intensity scale of 4) specific 18- to 20-kDa Asp-WB band (data not shown).
The comparison of the present findings with those of other clinical studies was limited due to the novelty of this Western blot-based test. However, some limitations of the current study are outlined. (i) Controlling for misclassification bias was hampered by the composite diagnostic criteria of aspergillosis that we used (Table 1), as no efficient gold standard is currently available. Therefore, sera from some patients infected by a microorganism other than Aspergillus might have been included in the study, which may explain at least some of the negative Asp-WB results obtained for patients diagnosed with aspergillosis. (ii) The retrospective study design did not allow us to calculate the predictive values of the Asp-WB assay. (iii) Blood donors were considered healthy, although no data were available concerning their potential exposure to Aspergillus fungi. Therefore, the underlying reason behind positive Asp-WB results obtained for some controls remains unclear. The choice to use blood donors as controls was based on the difficulty in ruling out the diagnosis of aspergillosis in at-risk patients due to the relatively poor sensitivity of the current diagnostic criteria. (iv) Cross-reactions of the Asp-WB assay were not evaluated because, according to the study design, all included patients were infected or colonized by an Aspergillus sp. alone or in combination with other fungi. (v) Specific banding patterns according to Aspergillus species were not evaluated, as A. fumigatus was isolated in all patients, either alone or in combination with another Aspergillus species (data not shown).
Assessments of band numbers and intensities in the semiquantitative interpretation of WB results have been used for the diagnosis of various infectious diseases, including HIV (17), Lyme borreliosis (18), and Helicobacter pylori carriage (19). While neither a particular Asp-WB banding pattern nor a semiquantitative Asp-WB result was significantly associated with any of the aspergillosis clinical presentations (data not shown), we found a significant correlation between semiquantitative Asp-WB results and the IPD band number. Using a semiquantitative interpretation might therefore facilitate the transition from semiquantitative IPD analysis to Asp-WB assay in the clinical practice.
As Aspergillus colonization is considered a pathway to infection, the management of clinically asymptomatic patients with Aspergillus sp. colonization remains a matter of debate. In line with this hypothesis, it has been demonstrated that persistent colonization can induce an antibody response, and according to some authors, this seroconversion should prompt the reinforcement of patient monitoring and/or the start of antifungal therapy (20–22). The primary interest of including colonized patients in this evaluation is that they are typically those in whom Aspergillus serology is performed. In contrast to effect in CF patients (21, 23–25), little is known concerning the impact of Aspergillus colonization in non-CF patients. Despite the relatively small sample size, we observed a striking difference in Asp-WB sensitivity, with 100% and 42% in CF and non-CF patients, respectively. The specificity of Asp-WB to detect Aspergillus colonization in CF patients was not determined because we did not study noncolonized CF patients. Our data show that in CF patients, the Asp-WB assay is positive in Aspergillus disease and in Aspergillus colonization. Further research is required to determine whether Aspergillus-specific IgG apparition is an early marker of aspergillosis onset.
In conclusion, this novel Western blot assay designed to detect anti-Aspergillus antibodies may be useful for the diagnosis of aspergillosis in immunocompetent patients. Its sensitivity was higher than that of the IPD assay (the current reference in anti-Aspergillus antibody detection assays), as highlighted by nonoverlapping 95% CI (Table 3). Further prospective studies are required to gain further insight into the clinical significance of Asp-WB results in diagnosing the various aspergillosis clinical presentations and monitoring patients.
ACKNOWLEDGMENTS
We are grateful to B. Michel, A. Forticaux, and D. Petkova for English language editing and the LDBio Diagnostics team for technical assistance.
A.O. is a Ph.D. student employee at LDBio Diagnostics. A.C. is a technician employee in part at LDBio Diagnostics.
This study was sponsored by LDBio Diagnostics. LDBio Diagnostics participated in the study design but did not interfere with the analyses or conclusions reported herein.
Aspergillus fumigatus antigen and diverse parasite antigens that are sold to LDBio Diagnostics are produced at the institution where P.F. is currently employed. Toxoplasma gondii antigen that is sold to LDBio Diagnostics is produced at the institution where S.R. and R.P. are currently employed.
C.H. received a research grant from Bio-Rad.
REFERENCES
- 1.Sherif R, Segal BH. 2010. Pulmonary aspergillosis: clinical presentation, diagnostic tests, management and complications. Curr Opin Pulm Med 16:242–250. doi: 10.1097/MCP.0b013e328337d6de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zmeili OS, Soubani AO. 2007. Pulmonary aspergillosis: a clinical update. QJM 100:317–334. doi: 10.1093/qjmed/hcm035. [DOI] [PubMed] [Google Scholar]
- 3.Nam H-S, Jeon K, Um S-W, Suh GY, Chung MP, Kim H, Kwon OJ, Koh W-J. 2010. Clinical characteristics and treatment outcomes of chronic necrotizing pulmonary aspergillosis: a review of 43 cases. Int J Infect Dis 14:e479–e482. doi: 10.1016/j.ijid.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 4.Jewkes J, Kay PH, Paneth M, Citron KM. 1983. Pulmonary aspergilloma: analysis of prognosis in relation to haemoptysis and survey of treatment. Thorax 38:572–578. doi: 10.1136/thx.38.8.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurup VP. 2005. Aspergillus antigens: which are important? Med Mycol 43(Suppl 1):S189–S196. doi: 10.1080/13693780500064763. [DOI] [PubMed] [Google Scholar]
- 6.Persat F. 2012. Aspergillus serology, from yesterday to today for tomorrow. J Mycol Med 22:72–82. (In French.) doi: 10.1016/j.mycmed.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 7.Van Toorenenbergen AW. 2012. Between-laboratory quality control of automated analysis of IgG antibodies against Aspergillus fumigatus. Diagn Microbiol Infect Dis 74:278–281. doi: 10.1016/j.diagmicrobio.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Kauffmann HF, De Vries K. 1980. Antibodies against Aspergillus fumigatus II: identification and quantification by means of crossed immunoelectrophoresis. Int Arch Allergy Appl Immunol 62:265–275. doi: 10.1159/000232522. [DOI] [PubMed] [Google Scholar]
- 9.Baxter CG, Denning DW, Jones AM, Todd A, Moore CB, Richardson MD. 2013. Performance of two Aspergillus IgG EIA assays compared with the precipitin test in chronic and allergic aspergillosis. Clin Microbiol Infect 19:E197–E204. doi: 10.1111/1469-0691.12133. [DOI] [PubMed] [Google Scholar]
- 10.Franck J, Garin YJ-F, Dumon H. 2008. LDBio-Toxo II immunoglobulin G Western blot confirmatory test for anti-toxoplasma antibody detection. J Clin Microbiol 46:2334–2338. doi: 10.1128/JCM.00182-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guan M. 2007. Frequency, causes, and new challenges of indeterminate results in Western blot confirmatory testing for antibodies to human immunodeficiency virus. Clin Vaccine Immunol 14:649–659. doi: 10.1128/CVI.00393-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fourneret-Vivier A, Lebeau B, Mallaret MR, Brenier-Pinchart MP, Brion JP, Pinel C, Garban F, Pison C, Hamidfar R, Plantaz D, Pelloux H, Grillot R. 2006. Hospital-wide prospective mandatory surveillance of invasive aspergillosis in a French teaching hospital (2000–2002). J Hosp Infect 62:22–28. doi: 10.1016/j.jhin.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 13.Jubin V, Ranque S, Stremler Le Bel N, Sarles J, Dubus J-C. 2010. Risk factors for Aspergillus colonization and allergic bronchopulmonary aspergillosis in children with cystic fibrosis. Pediatr Pulmonol 45:764–771. doi: 10.1002/ppul.21240. [DOI] [PubMed] [Google Scholar]
- 14.Garnaud C, Brenier-Pinchart M-P, Thiebaut-Bertrand A, Hamidfar R, Quesada J-L, Bosseray A, Lebeau B, Mallaret M-R, Maubon D, Saint-Raymond C, Pinel C, Hincky V, Plantaz D, Cornet M, Pelloux H. 2012. Seven-year surveillance of nosocomial invasive aspergillosis in a French University Hospital. J Infect 65:559–567. doi: 10.1016/j.jinf.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Izumikawa K, Tashiro T, Tashiro M, Takazono T, Kosai K, Morinaga Y, Kurihara S, Nakamura S, Imamura Y, Miyazaki T, Tsukamoto M, Kakeya H, Hayashi T, Yanagihara K, Nagayasu T, Kohno S. 2014. Pathogenesis and clinical features of chronic pulmonary aspergillosis: is it possible to distinguish CNPA and CCPA clinically? J Infect Chemother 20:208–212. doi: 10.1016/j.jiac.2013.10.016. [DOI] [PubMed] [Google Scholar]
- 16.Fricker-Hidalgo H, Coltey B, Llerena C, Renversez J-C, Grillot R, Pin I, Pelloux H, Pinel C. 2010. Recombinant allergens combined with biological markers in the diagnosis of allergic bronchopulmonary aspergillosis in cystic fibrosis patients. Clin Vaccine Immunol 17:1330–1336. doi: 10.1128/CVI.00200-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burke DS, Redfield RR, Putman P, Alexander SS. 1987. Variations in Western blot banding patterns of human T-cell lymphotropic virus type III/lymphadenopathy-associated virus. J Clin Microbiol 25:81–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zoller L, Burkard S, Schafer H. 1991. Validity of Western immunoblot band patterns in the serodiagnosis of Lyme borreliosis. J Clin Microbiol 29:174–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simán JH, Engstrand L, Berglund G, Florén C-H, Forsgren A. 2005. Evaluation of Western blot CagA seropositivity in Helicobacter pylori-seropositive and -seronegative subjects. Clin Diagn Lab Immunol 12:304–309. doi: 10.1128/CDLI.12.2.304-309.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barberan J, Alcazar B, Malmierca E, Garcia de la Llana F, Dorca J, Del Castillo D, Villena V, Hernandez-Febles M, Garcia-Perez F-J, Granizo J-J, Gimenez M-J, Aguilar L, ASP Investigator Group . 2012. Repeated Aspergillus isolation in respiratory samples from non-immunocompromised patients not selected based on clinical diagnoses: colonisation or infection? BMC Infect Dis 12:295. doi: 10.1186/1471-2334-12-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bardana EJ Jr, Sobti KL, Cianciulli FD, Noonan MJ. 1975. Aspergillus antibody in patients with cystic fibrosis. Am J Dis Child 129:1164–1167. [DOI] [PubMed] [Google Scholar]
- 22.Tashiro T, Izumikawa K, Tashiro M, Takazono T, Morinaga Y, Yamamoto K, Imamura Y, Miyazaki T, Seki M, Kakeya H, Yamamoto Y, Yanagihara K, Yasuoka A, Kohno S. 2011. Diagnostic significance of Aspergillus species isolated from respiratory samples in an adult pneumology ward. Med Mycol 49:581–587. doi: 10.3109/13693786.2010.548084. [DOI] [PubMed] [Google Scholar]
- 23.Fillaux J, Brémont F, Murris M, Cassaing S, Tétu L, Segonds C, Pipy B, Magnaval JF. 2014. Aspergillus sensitization or carriage in cystic fibrosis patients. Pediatr Infect Dis J 33:680–686. doi: 10.1097/INF.0000000000000231. [DOI] [PubMed] [Google Scholar]
- 24.Speirs JJ, Van der Ent CK, Beekman JM. 2012. Effects of Aspergillus fumigatus colonization on lung function in cystic fibrosis. Curr Opin Pulm Med 18:632–638. doi: 10.1097/MCP.0b013e328358d50b. [DOI] [PubMed] [Google Scholar]
- 25.De Vrankrijker AMM, Van der Ent CK, Van Berkhout FT, Stellato RK, Willems RJL, Bonten MJM, Wolfs TFW. 2011. Aspergillus fumigatus colonization in cystic fibrosis: implications for lung function? Clin Microbiol Infect 17:1381–1386. doi: 10.1111/j.1469-0691.2010.03429.x. [DOI] [PubMed] [Google Scholar]