Abstract
Human exposure to Bartonella clarridgeiae has been reported only on the basis of antibody detection. We report for the first time an asymptomatic human blood donor infected with B. clarridgeiae, as documented by enrichment blood culture, PCR, and DNA sequencing.
CASE REPORT
During a study designed to determine the prevalence of Bartonella bacteremia in samples from 500 blood donors from the Blood Bank of State University of Campinas (UNICAMP—HEMOCENTRO), Sao Paulo State, Brazil (L. H. U. Pitassi, P. P. V. de Paiva Diniz, D. G. Scorpio, M. R. Drummond, B. G. Lania, M. L. Barjas-Castro, S. Colombo, S. Sowy, E. B. Breithschwerdt, W. L. Nicholson, and P. E. N. F. Velho, submitted for publication), we identified a blood donor infected with Bartonella clarridgeiae on the basis of specific PCR amplification and DNA sequencing of an amplicon obtained from the 14-day liquid enrichment blood culture.
The donor was a 39-year-old male from Santo Antonio de Posse (22°36′22″S, 46°55′10″W), a city with approximately 20,000 inhabitants located 88 miles north of Sao Paulo City, the capital of Sao Paulo state, southeastern Brazil. The man self-reported donating blood from 6 to 10 times previously. For more than 10 years, the man shared his home with a cat, and he had sustained a bite 2 years earlier. At that time, he had no symptoms. In addition, the man had domiciliary contact with two pet dogs for 4 years. He reported that these animals occasionally had flea and tick infestation. He had no tattoos and had never traveled outside Sao Paulo state, Brazil.
Immediately after the collection of a blood unit, 5 ml of blood was collected into an EDTA tube, with other 5 ml collected into a serum separator tube via accessory port. After serum centrifugation, samples were stored at −20°C until analysis. Two milliliters of the donor's whole EDTA blood was thawed and added into 8 ml of liquid Bartonella Alpha-Proteobacteria Growth (BAPGM) medium (1), and the reaction mixture was incubated at 37°C in 5% CO2, in a water-saturated atmosphere. The flask was maintained with a constant shaking motion for 14 days. A negative-control flask containing only BAPGM medium was added to each batch of samples tested and subjected to the same laboratory procedures and culture conditions. After a 14-day incubation period, a 1-ml aliquot of liquid culture medium was used for DNA extraction and another 1-ml aliquot was plated onto a blood agar plate and incubated for an additional 42 days. Blood agar plates were prepared with 30% of sheep blood confirmed to be free of Bartonella DNA by PCR (2). The liquid culture negative-control blood-agar plate was incubated under the same conditions. All culture methods were carried out in a class 2 biosafety cabinet in order to minimize the risk of specimen DNA or bacterial contamination and to protect laboratory personnel.
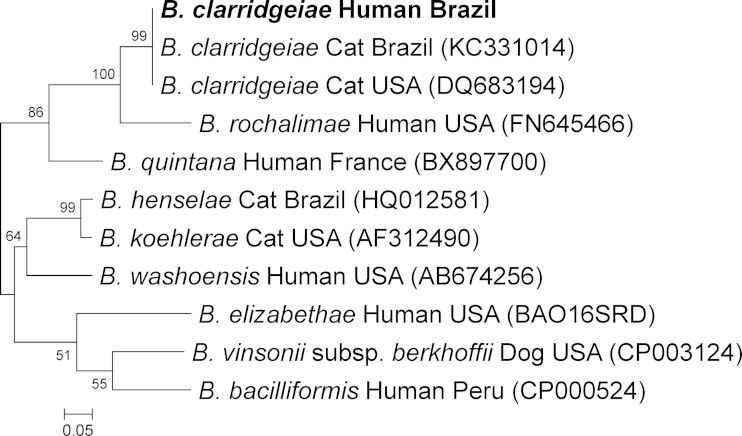
The liquid culture sample used for molecular analysis was centrifuged, and the pellet was tested for the presence of Bartonella DNA. Genomic DNA from the liquid culture was extracted using a QIAamp DNA minikit (Qiagen Inc., Valencia, CA, USA) following the manufacturer's instructions and tested by a real-time PCR using primers manually designed to amplify a fragment of the 16S-23S rRNA intergenic transcribed spacer (ITS) region of all Bartonella species. The 25-μl reaction mixture contained 1× PCR mix (SYBR Premix Ex Taq; TaKaRa Bio Inc., Shiga, Japan), 7.5 pmol of primer 314A-s (5′-CGTTTCTCTTTCTTCMGATGATGATCCC-3′), 7.5 pmol of primer 314B-s (5′-CGTTTCTCTTTCTTCRGATGATGATCCC-3′), 10.5 pmol of primer 382-as (5′-ACTTSAACCTCCGACCTCACGCTTAT-3′), 1× ROX reference dye, and 5 μl of DNA template. Amplifications were performed under the following conditions: one hot-start cycle at 95°C for 1 min followed by 50 cycles of denaturing at 94°C for 10 s, annealing at 58°C for 20 s, and extension at 72°C for 20 s. Amplification was detected by SYBR green I fluorescence with emission at 522 nm. The expected melting curves were obtained. Serial dilutions of B. henselae DNA from 109 genome equivalents (GE) per microliter to 1 GE/μl were used as a positive control, for the determination of the limit of detection of this assay (5 copies per reaction). A Mastermix reagent negative control was included in each batch of samples tested. The amplicons generated were purified (MiniElute kit; Qiagen, Valencia, CA, USA) according to the manufacturer's instructions and sequenced with a fluorescence-based automated sequencing system (Eurofins MWG Operon, Huntsville, AL, USA). Chromatogram evaluation, primer deletion, and sequence alignment were performed using Contig Express software and AlignX software (Vector NTI Suite 10.1; Invitrogen Corp., Carlsbad, CA, USA). The bacterial species was defined by comparing similarities with other sequences deposited in the GenBank database using the Basic Local Alignment Search Tool (3). A phylogenetic tree (Fig. 1) was generated based on 136-bp sequences of the ITS of B. clarridgeiae from the blood donor and closely related organisms by using the maximum-likelihood method on the basis of the Kimura 2-parameter model, with bootstrap support based on 1,000 replicates (Molecular Evolutionary Genetics Analysis [MEGA] software, version 5.2).
FIG 1.
Phylogenetic tree based on 136 bp from the 16S-23S rRNA intergenic transcribed spacer (ITS) sequences of Bartonella clarridgeiae obtained from a blood donor (in boldface) and closely related organisms constructed by using the maximum-likelihood method on the basis of the Kimura 2-parameter model. Each bacterial name is followed by isolation source and geographic-origin data, and the GenBank accession number is provided in parentheses. The numbers at the nodes indicate percentages of bootstrap support based on 1,000 replicates. Percentages corresponding to partitions reproduced in fewer than 50% of bootstrap replicates are collapsed. The scale bar indicates 0.05 substitutions per nucleotide position.
The donor serum sample was analyzed for the presence of IgG antibodies to B. henselae and B. quintana antigens grown in Vero cell cultures by an indirect immunofluorescence assay (IFA) according to a previously described procedure (4). The bacterial antigens were supplied by the Centers for Disease Control and Prevention (CDC, Atlanta, GA, USA). The serum sample was diluted 1/64 in phosphate-buffered saline (PBS), and 25 μl was applied to Bartonella-infected cells fixed to a glass slide and incubated for 30 min at 37°C. The slides were washed three times (for 5 min each time) in PBS, overlaid with fluorescein isothiocyanate-conjugated goat anti-human immunoglobulin IgG (Sigma, St. Louis, MO, USA) at a dilution of 1/150, incubated at 37°C for 30 min, washed, and dried. Slides were examined on a Labophot fluorescence microscope (Nikon, Melville, NY, USA). The cutoff titer of the IFA was 1/64. Endpoint titers were not determined. A positive test was warranted if brightly stained bacteria could be detected by fluorescence microscopy at ×400 magnification. Previously IFA-negative serum samples were used as negative controls.
By real-time PCR, amplicons of 190 bp in size were obtained from the liquid culture aliquot. After primer deletion, the remaining 136-bp sequence was 100% similar to B. clarridgeiae DNA sequences from samples collected from cats in the United States and Brazil (Fig. 1). Following subculture, no isolate was obtained from this subject and he was not seroreactive to B. henselae and B. quintana antigens.
This report describes the molecular documentation of B. clarridgeiae DNA in human blood. The subject was an asymptomatic blood donor who had previously donated blood multiple times. Bartonella spp. are the only known Gram-negative bacilli that can live inside erythrocytes while often causing persistent infections in the host (5). To date, 15 species, subspecies, or Candidatus species of Bartonella have been known to infect humans (Table 1). Asymptomatic infection with Bartonella bacilliformis in humans is well established (6), and numerous outwardly healthy animals support persistent Bartonella sp. bacteremia (5). However, a spectrum of disease manifestations associated with Bartonella spp. has gained importance within the last decades. The genus Bartonella comprises a group of reemerging and neglected zoonotic pathogens that have been associated with a broad range of serious human diseases (Table 1).
TABLE 1.
Species, subspecies, or Candidatus species of Bartonella confirmed by molecular methods to infect humans
| Species | Clinical outcome(s) | Reference(s) or source |
|---|---|---|
| B. bacilliformis | Oroya fever, verruga peruana | 6 |
| B. quintana | Bacillary angiomatosis, trench fever, bacteremia | 34 |
| B. henselae | Cat scratch disease, endocarditis, bacillary angiomatosis, peliosis hepatis, bacteremia | 7–9 |
| B. elizabethae | Fever, endocarditis | 35 |
| B. grahamii | Cat scratch disease (lymphadenopathy, reddish papule, abscess) | 36 |
| B. vinsonii subsp. berkhoffii | Endocarditis, arthritis, neurological disease, and epithelioid hemangioendothelioma | 33 |
| B. koehlerae | Anxiety, severe headaches, muscle spasms, decreased peripheral vision, and hallucinations | 37 |
| B. alsatica | Fever, lymphadenitis, and endocarditis | 38 |
| B. vinsonii subsp. arupensis | Fatigue, headache, and myalgias | 39 |
| B. washoensis | Meningitis | 40 |
| B. rochalimae | Bacteremia, fever, and splenomegaly | 24 |
| B. tamiae | Fever, headache, myalgia, maculopapular rash, petechial rash in arms and legs, abnormalities in liver function | 41 |
| B. melophagia | Dry cough, fatigue, muscle pain, and severe chills | 42 |
| B. mayotimonensisa | Endocarditis | 43 |
| B. volans (including volans-like) | Symptoms uncertain | 44 |
| B. clarridgeiae | Asymptomatic | This report |
Candidate species in the genus Bartonella.
Worldwide, Bartonella henselae is a causative agent of cat scratch disease (CSD), bacillary angiomatosis, peliosis hepatis, bacteremia, endocarditis, chronic lymphadenopathy, and neurological disorders (7–9). B. clarridgeiae has also been suggested to cause fever, headaches, malaise, lymphadenopathy (10, 11), and thoracopulmonary manifestations (12) in humans; endocarditis (13) and hepatic diseases (14) in dogs; and blindness (15) and neuritis (16) in cats. The diversity of the clinical manifestations associated with bartonellosis depends mainly on the virulence of the Bartonella sp. or strain, the level of evolutionary host adaptation of the bacterium, and the immune response of the host, which is a critical determinant of disease expression (5). In some patients, and especially in immunocompromised subjects, the disease can be fatal (17). The long-term consequence of chronic subclinical infection with Bartonella spp. in immunocompetent humans is currently unknown.
Previously, serological evidence of anti-B. clarridgeiae antibodies supported hypotheses of exposure in humans (10, 12). However, to our knowledge, B. clarridgeiae was never isolated or documented by molecular techniques in blood or tissue samples from a human. B. clarridgeiae DNA was detected from fleas (18), and bacteremic infection has been reported in sick dogs (13, 14) and in the healthy pet cat of a sick veterinarian with CSD (11). Experimentally, B. clarridgeiae can be transmitted by blood transfusion and be detected by PCR from blood, brain, lymph node, myocardium, liver, and kidney tissues not only from blood culture-positive cats but also from blood culture-negative cats (19). Furthermore, natural concomitant infection with B. clarridgeiae and B. henselae has been reported in domestic cats (20), because both Bartonella spp. are considered adapted to this host and are likely transmitted by the common cat flea (Ctenocephalides felis). In vitro, both of these Bartonella species can infect feline erythrocytes (21) and are capable of entering human endothelial cells (22).
The DNA fragment of B. clarridgeiae sequenced from this blood donor was 100% similar to DNA sequences obtained from samples collected from cats in Brazil (23) and from a cat from the United States (24). Cats are considered the natural reservoir of B. clarridgeiae, being capable of sustaining high levels of bacteremia (25). The blood donor infected with B. clarridgeiae reported long-term daily contact with two dogs and a cat for years, and he reported a cat bite 2 years earlier. Despite the fact that these animals were not tested for Bartonella sp. bacteremia, the fleas and ticks that occasionally infested his cat and dogs may have transmitted the pathogen to the owner. In a previous study of 14 immunocompetent people infected with Bartonella henselae or B. vinsonii subsp. berkhoffii, all participants reported frequent exposure to fleas and ticks from domestic cats and dogs (26).
Annually, about 15 million units of red cells are transfused in the United States and about 85 million worldwide (27). The overall rate of any bacterial contamination of red blood cells (RBCs) in blood units reportedly ranges from 0.03% to 0.3% (28). Bacterial contamination is the third most common cause of death from transfusion in the United States (29). Bartonella transmission by blood transfusion has not yet been described; however, in light of our findings, this possibility should be considered. We previously described the presence of B. henselae in a RBC unit from an asymptomatic donor (30) and noted that B. henselae is also able to survive in stored red blood cell units for 35 days (31). Additionally, suspected iatrogenic transmission by needle pricking of B. vinsonii subsp. berkhoffii and B. henselae to two veterinarians who subsequently developed different clinical manifestations (32, 33) further supports the hypothesis that Bartonella transmission by blood transfusion or blood products is feasible.
Our findings demonstrate that B. clarridgeiae can be present in healthy blood donors, and may pose a risk to blood recipients, in particular immunocompromised patients receiving blood transfusions. The relevance of the genus Bartonella to transfusion medicine in Brazil and other countries should be further investigated.
ACKNOWLEDGMENTS
This work was partially supported by a Faculty Grant in Global Health to D.G.S. from the Johns Hopkins Center for Global Health; a grant from FAEPEX—UNICAMP (Fundo de Apoio ao Ensino, à Pesquisa e à Extensão—UNICAMP); and a summer research scholarship to Stanley Sowy from the Office of the Vice President for Research and Biotechnology, Western University, Western University of Health Sciences, Pomona, CA.
We thank the study patients and Steven Henriksen and Dominique Griffon for providing the research infrastructure and support needed at Western University of Health Sciences and Hannah Mirrashed, John Greenwood, and Marizete Salvadego for technical assistance.
E.B.B. has a patent (US patent 7,115,385) for media and methods for cultivation of microorganisms (issued to E.B.B., S. Sontakke, and North Carolina State University.) E.B.B. is the chief scientific officer for Galaxy Diagnostics, a company that provides diagnostic testing for the detection of Bartonella species infection in animals and human patient samples. All other authors have no conflict of interest to declare.
REFERENCES
- 1.Maggi RG, Duncan AW, Breitschwerdt EB. 2005. Novel chemically modified liquid medium that will support the growth of seven Bartonella species. J Clin Microbiol 43:2651–2655. doi: 10.1128/JCM.43.6.2651-2655.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drummond MR, Pitassi LH, Lania BG, Dos Santos SR, Gilioli R, Velho PE. 2011. Detection of Bartonella henselae in defibrinated sheep blood used for culture media supplementation. Braz J Microbiol 42:430–432. doi: 10.1590/S1517-83822011000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. 1990. Basic local alignment search tool. J Mol Biol 215:403–410. [DOI] [PubMed] [Google Scholar]
- 4.Dalton MJ, Robinson LE, Cooper J, Regnery RL, Olson JG, Childs JE. 1995. Use of Bartonella antigens for serologic diagnosis of cat-scratch disease at a national referral center. Arch Intern Med 155:1670–1676. [PubMed] [Google Scholar]
- 5.Breitschwerdt EB, Maggi RG, Chomel BB, Lappin MR. 2010. Bartonellosis: an emerging infectious disease of zoonotic importance to animals and human beings. J Vet Emerg Crit Care (San Antonio) 20:8–30. doi: 10.1111/j.1476-4431.2009.00496.x. [DOI] [PubMed] [Google Scholar]
- 6.Chamberlin J, Laughlin LW, Romero S, Solorzano N, Gordon S, Andre RG, Pachas P, Friedman H, Ponce C, Watts D. 2002. Epidemiology of endemic Bartonella bacilliformis: a prospective cohort study in a Peruvian mountain valley community. J Infect Dis 186:983–990. doi: 10.1086/344054. [DOI] [PubMed] [Google Scholar]
- 7.Maggi RG, Ericson M, Mascarelli PE, Bradley JM, Breitschwerdt EB. 2013. Bartonella henselae bacteremia in a mother and son potentially associated with tick exposure. Parasit Vectors 6:101. doi: 10.1186/1756-3305-6-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott MA, McCurley TL, Vnencak-Jones CL, Hager C, McCoy JA, Anderson B, Collins RD, Edwards KM. 1996. Cat scratch disease: detection of Bartonella henselae DNA in archival biopsies from patients with clinically, serologically, and histologically defined disease. Am J Pathol 149:2161–2167. [PMC free article] [PubMed] [Google Scholar]
- 9.Slater LN, Welch DF, Min KW. 1992. Rochalimaea henselae causes bacillary angiomatosis and peliosis hepatis. Arch Intern Med 152:602–606. [PubMed] [Google Scholar]
- 10.Sander A, Zagrosek A, Bredt W, Schiltz E, Piemont Y, Lanz C, Dehio C. 2000. Characterization of Bartonella clarridgeiae flagellin (FlaA) and detection of antiflagellin antibodies in patients with lymphadenopathy. J Clin Microbiol 38:2943–2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kordick DL, Hilyard EJ, Hadfield TL, Wilson KH, Steigerwalt AG, Brenner DJ, Breitschwerdt EB. 1997. Bartonella clarridgeiae, a newly recognized zoonotic pathogen causing inoculation papules, fever, and lymphadenopathy (cat scratch disease). J Clin Microbiol 35:1813–1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Margileth AM, Baehren DF. 1998. Chest-wall abscess due to cat-scratch disease (CSD) in an adult with antibodies to Bartonella clarridgeiae: case report and review of the thoracopulmonary manifestations of CSD. Clin Infect Dis 27:353–357. doi: 10.1086/514671. [DOI] [PubMed] [Google Scholar]
- 13.Chomel BB, Mac Donald KA, Kasten RW, Chang CC, Wey AC, Foley JE, Thomas WP, Kittleson MD. 2001. Aortic valve endocarditis in a dog due to Bartonella clarridgeiae. J Clin Microbiol 39:3548–3554. doi: 10.1128/JCM.39.10.3548-3554.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gillespie TN, Washabau RJ, Goldschmidt MH, Cullen JM, Rogala AR, Breitschwerdt EB. 2003. Detection of Bartonella henselae and Bartonella clarridgeiae DNA in hepatic specimens from two dogs with hepatic disease. J Am Vet Med Assoc 222:47–51, 35. doi: 10.2460/javma.2003.222.47. [DOI] [PubMed] [Google Scholar]
- 15.Robinson MT, Hillman T, Langton DA, Shaw SE. 2009. Bartonella clarridgeiae in a cat in the UK. Vet Rec 164:58–59. doi: 10.1136/vr.164.2.58. [DOI] [PubMed] [Google Scholar]
- 16.Sykes JE, Westropp JL, Kasten RW, Chomel BB. 2010. Association between Bartonella species infection and disease in pet cats as determined using serology and culture. J Feline Med Surg 12:631–636. doi: 10.1016/j.jfms.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fouch B, Coventry S. 2007. A case of fatal disseminated Bartonella henselae infection (cat-scratch disease) with encephalitis. Arch Pathol Lab Med 131:1591–1594. [DOI] [PubMed] [Google Scholar]
- 18.Boudebouch N, Sarih M, Beaucournu JC, Amarouch H, Hassar M, Raoult D, Parola P. 2011. Bartonella clarridgeiae, B. henselae, and Rickettsia felis in fleas from Morocco. Ann Trop Med Parasitol 105:493–498. doi: 10.1179/1364859411Y.0000000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kordick DL, Brown TT, Shin K, Breitschwerdt EB. 1999. Clinical and pathologic evaluation of chronic Bartonella henselae or Bartonella clarridgeiae infection in cats. J Clin Microbiol 37:1536–1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chomel BB, Carlos ET, Kasten RW, Yamamoto K, Chang CC, Carlos RS, Abenes MV, Pajares CM. 1999. Bartonella henselae and Bartonella clarridgeiae infection in domestic cats from The Philippines. Am J Trop Med Hyg 60:593–597. [DOI] [PubMed] [Google Scholar]
- 21.Dehio C. 2001. Bartonella interactions with endothelial cells and erythrocytes. Trends Microbiol 9:279–285. doi: 10.1016/S0966-842X(01)02047-9. [DOI] [PubMed] [Google Scholar]
- 22.Dehio C, Meyer M, Berger J, Schwarz H, Lanz C. 1997. Interaction of Bartonella henselae with endothelial cells results in bacterial aggregation on the cell surface and the subsequent engulfment and internalisation of the bacterial aggregate by a unique structure, the invasome. J Cell Sci 110(Pt 18):2141–2154. [DOI] [PubMed] [Google Scholar]
- 23.Braga Mdo S, Diniz PP, André MR, Bortoli CP, Machado RZ. 2012. Molecular characterisation of Bartonella species in cats from São Luís, state of Maranhão, north-eastern Brazil. Mem Inst Oswaldo Cruz 107:772–777. doi: 10.1590/S0074-02762012000600011. [DOI] [PubMed] [Google Scholar]
- 24.Eremeeva ME, Gerns HL, Lydy SL, Goo JS, Ryan ET, Mathew SS, Ferraro MJ, Holden JM, Nicholson WL, Dasch GA, Koehler JE. 2007. Bacteremia, fever, and splenomegaly caused by a newly recognized Bartonella species. N Engl J Med 356:2381–2387. doi: 10.1056/NEJMoa065987. [DOI] [PubMed] [Google Scholar]
- 25.Chomel BB, Boulouis HJ, Breitschwerdt EB, Kasten RW, Vayssier-Taussat M, Birtles RJ, Koehler JE, Dehio C. 2009. Ecological fitness and strategies of adaptation of Bartonella species to their hosts and vectors. Vet Res 40:29. doi: 10.1051/vetres/2009011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Breitschwerdt EB, Maggi RG, Duncan AW, Nicholson WL, Hegarty BC, Woods CW. 2007. Bartonella species in blood of immunocompetent persons with animal and arthropod contact. Emerg Infect Dis 13:938–941. doi: 10.3201/eid1306.061337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, Holcomb JB, Illoh O, Kaplan LJ, Katz LM, Rao SV, Roback JD, Shander A, Tobian AA, Weinstein R, Swinton McLaughlin LG, Djulbegovic B; Clinical Transfusion Medicine Committee of the AABB . 2012. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med 157:49–58. doi: 10.7326/0003-4819-157-1-201206190-00429. [DOI] [PubMed] [Google Scholar]
- 28.Ramirez-Arcos S, Goldman M, Blajchman M. 2012. Bacterial contamination, p 153–189. In Popovsky MA. (ed), Transfusion reaction, vol 4–American Association of Blood Banks, Bethesda, MD. [Google Scholar]
- 29.Vamvakas EC, Blajchman MA. 2009. Transfusion-related mortality: the ongoing risks of allogeneic blood transfusion and the available strategies for their prevention. Blood 113:3406–3417. doi: 10.1182/blood-2008-10-167643. [DOI] [PubMed] [Google Scholar]
- 30.Magalhães RF, Cintra ML, Barjas-Castro ML, Del Negro GM, Okay TS, Velho PE. 2010. Blood donor infected with Bartonella henselae. Transfus Med 20:280–282. doi: 10.1111/j.1365-3148.2010.01001.x. [DOI] [PubMed] [Google Scholar]
- 31.Magalhães RF, Pitassi LH, Salvadego M, de Moraes AM, Barjas-Castro ML, Velho PE. 2008. Bartonella henselae survives after the storage period of red blood cell units: is it transmissible by transfusion? Transfus Med 18:287–291. doi: 10.1111/j.1365-3148.2008.00871.x. [DOI] [PubMed] [Google Scholar]
- 32.Lin JW, Chen CM, Chang CC. 2011. Unknown fever and back pain caused by Bartonella henselae in a veterinarian after a needle puncture: a case report and literature review. Vector Borne Zoonotic Dis 11:589–591. doi: 10.1089/vbz.2009.0217. [DOI] [PubMed] [Google Scholar]
- 33.Oliveira AM, Maggi RG, Woods CW, Breitschwerdt EB. 2010. Suspected needle stick transmission of Bartonella vinsonii subspecies berkhoffii to a veterinarian. J Vet Intern Med 24:1229–1232. doi: 10.1111/j.1939-1676.2010.0563.x. [DOI] [PubMed] [Google Scholar]
- 34.Ohl ME, Spach DH. 2000. Bartonella quintana and urban trench fever. Clin Infect Dis 31:131–135. doi: 10.1086/313890. [DOI] [PubMed] [Google Scholar]
- 35.Daly JS, Worthington MG, Brenner DJ, Moss CW, Hollis DG, Weyant RS, Steigerwalt AG, Weaver RE, Daneshvar MI, O'Connor SP. 1993. Rochalimaea elizabethae sp. nov. isolated from a patient with endocarditis. J Clin Microbiol 31:872–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oksi J, Rantala S, Kilpinen S, Silvennoinen R, Vornanen M, Veikkolainen V, Eerola E, Pulliainen AT. 2013. Cat scratch disease caused by Bartonella grahamii in an immunocompromised patient. J Clin Microbiol 51:2781–2784. doi: 10.1128/JCM.00910-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Breitschwerdt EB, Mascarelli PE, Schweickert LA, Maggi RG, Hegarty BC, Bradley JM, Woods CW. 2011. Hallucinations, sensory neuropathy, and peripheral visual deficits in a young woman infected with Bartonella koehlerae. J Clin Microbiol 49:3415–3417. doi: 10.1128/JCM.00833-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raoult D, Roblot F, Rolain JM, Besnier JM, Loulergue J, Bastides F, Choutet P. 2006. First isolation of Bartonella alsatica from a valve of a patient with endocarditis. J Clin Microbiol 44:278–279. doi: 10.1128/JCM.44.1.278-279.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Welch DF, Carroll KC, Hofmeister EK, Persing DH, Robison DA, Steigerwalt AG, Brenner DJ. 1999. Isolation of a new subspecies, Bartonella vinsonii subsp. arupensis, from a cattle rancher: identity with isolates found in conjunction with Borrelia burgdorferi and Babesia microti among naturally infected mice. J Clin Microbiol 37:2598–2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Probert W, Louie JK, Tucker JR, Longoria R, Hogue R, Moler S, Graves M, Palmer HJ, Cassady J, Fritz CL. 2009. Meningitis due to a “Bartonella washoensis”-like human pathogen. J Clin Microbiol 47:2332–2335. doi: 10.1128/JCM.00511-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kosoy M, Morway C, Sheff KW, Bai Y, Colborn J, Chalcraft L, Dowell SF, Peruski LF, Maloney SA, Baggett H, Sutthirattana S, Sidhirat A, Maruyama S, Kabeya H, Chomel BB, Kasten R, Popov V, Robinson J, Kruglov A, Petersen LR. 2008. Bartonella tamiae sp. nov., a newly recognized pathogen isolated from three human patients from Thailand. J Clin Microbiol 46:772–775. doi: 10.1128/JCM.02120-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maggi RG, Kosoy M, Mintzer M, Breitschwerdt EB. 2009. Isolation of Candidatus Bartonella melophagi from human blood. Emerg Infect Dis 15:66–68. doi: 10.3201/eid1501.081080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin EY, Tsigrelis C, Baddour LM, Lepidi H, Rolain JM, Patel R, Raoult D. 2010. Candidatus Bartonella mayotimonensis and endocarditis. Emerg Infect Dis 16:500–503. doi: 10.3201/eid1603.081673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Breitschwerdt EB, Maggi RG, Cadenas MB, de Paiva Diniz PP. 2009. A groundhog, a novel Bartonella sequence, and my father's death. Emerg Infect Dis 15:2080–2086. doi: 10.3201/eid1512.AD1512. [DOI] [PMC free article] [PubMed] [Google Scholar]