Abstract
Social relationships are generally thought of as beneficial. However, the present study set out to test the hypothesis that for individuals who perceive others to judge their appearance negatively, daily social interactions can also be a source of stress. Indeed when assessing 38 young adults, we found that both more incidences of negative exchanges reported during the past month as well as perceived negative appearance judgments by others were associated with more self-reported stress. Interestingly, however, for individuals with low attribution body esteem, higher numbers of positive social exchanges during the past month were related to health-relevant changes in biological markers of chronic stress as well. The same was true for individuals with high attribution body esteem who reported to experience only very few positive exchanges. As such, these findings go beyond the initial focus on low body esteem and negative social exchanges and introduce high body esteem as well as daily positive exchanges as potential health risk factors.
Keywords: body esteem, attribution body esteem, social exchanges, chronic stress, diurnal cortisol
Although social relationships are generally thought of as beneficial, negative social interactions have been associated with psychological distress (Newsom, Rook, Nishishiba, Sorkin, & Mahan, 2005). However, all social interactions can be sources of daily stress (Bolger, DeLongis, Kessler, & Schilling, 1989), particularly those involving social evaluation (Dickerson, Mycek, & Zaldivar, 2008). Social evaluation, in turn, may be especially relevant for individuals who are worried about being judged on their appearance (McClintock & Evans, 2001). Importantly, chronic stress due to concerns about perceived appearance judgments and social exchanges may result in physiological wear and tear and subsequently, health consequences (Goldstein & McEwen, 2002; Tsigos & Chrousos, 2002). Thus, concerns about appearance judgments may be an important moderator of the link between social exchanges and psychological and biological stress markers. To date, no study has examined the role of daily positive and negative social exchanges for self-reported chronic stress or daily functioning of physiological stress-related systems, or whether these associations vary based on attribution body esteem.
Daily social exchanges as stressors
Stress from social relationships has been associated with a host of negative mental and physical health outcomes (e.g., Newsom, Mahan, Rook, & Krause, 2008). Interestingly, a number of studies have found that simply the numbers of day-to-day positive and negative social exchanges are associated with psychological well-being as well as physical health (Finch, Okun, Pool, & Ruelman, 1999; Newsom, Nishishiba, Morgan, & Rook, 2003; Newsom et al., 2008; Okun & Keith, 1998). Using both retrospective (i.e., during the past month) and daily assessments of the frequency of exchanges, previous studies have shown links between more frequent positive social interactions and better health-related outcomes and correspondingly, more negative interactions and poorer health. In general however, all social exchanges may have the capacity to be stressful. Prior research has found that expectations about social evaluation play a vital role in whether a social interaction is stress inducing or stress buffering (Kors, Linden, & Gerin, 1997; Dickerson et al., 2008). In other words, when someone expects to be evaluated by another person, be it a stranger, friend, or romantic partner, they are more likely to experience stress related to that interaction. Thus, despite previous literature describing the health risks associated with negative exchanges (e.g., Newsom et al., 2008), this framework suggests that positive social exchanges characterized by social evaluation can be just as stressful as negative social exchanges.
Body esteem as a moderator
If associations between social exchanges and stress are less dependent on the valence of the social exchanges, the question arises which other factors may help explain potential inter-individual differences. One important moderator contributing to whether social exchanges are perceived as stressful may be body esteem. More specifically, the social-self preservation theory has described how stress is most often induced in contexts in which one’s performance is evaluated by other people (Dickerson et al., 2008). Interestingly, body image and gender theorists have suggested that the way one’s body is presented can be considered a form of performance as well (Bordo, 2003; Fredrickson & Roberts, 1997). This idea has important implications. Constant exposure to images of unattainable ideals of appearance can lead to adoption of unrealistic standards for one’s own looks. Once the societal standards for appearance are internalized, this can lead to frequent unfavorable comparisons of one’s own body against the ideal (Wertheim, Paxton, & Blaney, 2004). This discrepancy can lead to low body esteem, i.e., negative feelings about one’s body and appearance independent of one’s actual body size (Mendelson, B., Mendelson, M., & White, 2001).
As such, appearance may be a particularly relevant source of evaluation-related stress experiences in social interactions. Indeed, low body esteem has been associated with increased fear of negative evaluation as well as social phobia behaviors (McClintock & Evans, 2001). Furthermore, daily social exchanges can be frequent and occur not only with people one knows, like friends and family, but with strangers as well. Having internalized an unrealistic standard of appearance, expectations to be evaluated negatively in said social interactions may contribute to those interactions being stressful.
One facet of body esteem that captures specifically how individuals feel about their appearance in social situations is attribution body esteem (Mendelson et al., 2001). Someone with high attribution body esteem feels that others frequently make positive judgments about their appearance whereas those with low attribution body esteem perceive that others rarely make positive judgments (Mendelson et al., 2001). Because individuals with low attribution body esteem already expect that others do not evaluate their looks positively, they may carry this attitude into their social interactions thereby increasing the risk for experiencing stress association with social exchanges.
Self-verification theory offers an interesting extension to this idea. This theory posits that individuals prefer and seek out feedback that confirms their own self-view, even if their self-view is negative (Giesler, Josephs, & Swann, 1996). Thus, those with low attribution body esteem may be more likely to perceive negative evaluation and thus stress as a result of both, negative and positive social exchange; either due to social exchanges reinforcing their own negative self-view or due to positive exchanges conflicting with their negative perception of themselves.
Pathways to health outcomes
Given that social exchanges are almost impossible to avoid, such repeated and often uncontrollable interactions may result in repeated physiological stress responses. Wear and tear resulting from these repeated stress responses will eventually lead to dysfunctions in stress systems, which in turn pose a health risk (Goldstein & McEwen, 2002; Tsigos & Chrousos, 2002).
A key factor involved in physiological stress responses is the hypothalamic pituitary adrenal (HPA) axis with its hormonal end product, cortisol. Repeated chronic HPA axis activation has been found to result in dysregulation of the basal state of this system, specifically, dysfunctions in the circadian cortisol rhythm. Cortisol in a healthy individual shows a strong increase in response to awakening followed by a gradual decline over the course of the day with very low levels late at night, whereas dysregulations include patterns characterized by a flattened cortisol decrease across the day as well as hypercortisolism (ie. elevated cortisol levels throughout the day) (Chrousos & Gold, 1992). Dysregulated daily cortisol rhythms have subsequently been associated with a variety of negative physical and mental health outcomes (e.g., Kumari, Shipley, Stafford, & Kivimaki, 2011; Stetler & Miller, 2005; Matthews, Schwartz, Cohen, & Seeman, 2006). Taken together, alterations in basal stress systems may be an important pathway by which social factors can influence health (Adam & Kumari, 2009; Seltzer et al., 2009).
Study Aims
The current study aims to examine whether attribution body esteem affects health by turning daily social interactions into a source of chronic stress. Because previous literature has linked negative social exchanges to psychological well-being but not yet to chronic stress, the present study will first test (1) whether higher numbers of negative exchanges reported during the past month are associated with (a) elevated chronic psychological stress and (b) alterations in basal daily cortisol patterns. Further, since low attribution body esteem indicates that individuals feel evaluated in social situations and thus more vulnerable to stress from social exchanges, we will next examine to what extent (2) attribution body esteem will moderate the association between numbers of negative social exchanges and (a) psychological stress, as well as (b) health-relevant basal cortisol indices.
Little is known about the potential detrimental effects of positive social exchanges. As suggested above, individuals with low attribution body esteem may be more likely to perceive negative judgment in all types of social situations, making even positive exchanges potentially stressful. Thus, the third hypothesis examines (3) for individuals with lower attribution body esteem, whether higher numbers of positive exchanges during the past month will be associated with (a) increased chronic psychological stress as well as the (b) respective changes in diurnal cortisol patterns.
Method
Participants
A total of 44 Brandeis University undergraduates were recruited through the Psychology subject pool as well as advertisements in lower-division Psychology classes. This sample size (40 plus 10% to account for attrition) was based on previous findings with similar variables (social interactions and diurnal cortisol), particularly, a study reporting a large effect size (R2 = .51) with 36 healthy participants (Stetler & Miller, 2005). One participant was excluded due to missing cortisol data, two participants for missing data on the social support measure, and three for incomplete data on the social exchanges measure. Thus complete datasets were available for 38 participants (age = 20.5 ± 2.45, 15 males and 23 females, overall BMI mean = 23.4, SD = 3.72). All participants were over 18 years old and free from chronic disease. Women taking oral contraceptives were excluded from participation as this medication interferes with cortisol levels. Upon study completion, participants received credit for their Psychology class or $15. The study protocol was approved the Brandeis University Institutional Review Board.
Procedures
Participants came to the Health Psychology laboratory on a weekday and were seated in a quiet testing room. After consenting to participation, they first answered a package of questionnaires described in detail below. Next, they were given instructions on how to collect saliva samples at home. All participants collected saliva samples on two consecutive weekdays following their laboratory visit. For example, if a participant came to the laboratory on a Thursday, they were asked to collect samples the following Monday and Tuesday. Participants were asked to collect a total of 12 samples at six specific time points: immediately upon awakening, 30 minutes, 60 minutes, 4 hours, 9 hours, and 13 hours after wake-up. In addition, participants were asked to fill out a diary with scheduled times for each sample as well as the actual time each sample was taken (details on compliance described in more detail in “Home Sampling” section below). Samples were collected using the Salivette collection system (Sarstedt, Rommelsdorf, Germany) consisting of a plastic container with an inner plastic tube housing a sterile cotton roll. Participants were instructed to move the cotton roll around in their mouth for one minute, then place it back into the plastic container. They were told not to eat, drink, or brush their teeth for at least 20 minutes before collecting a sample. Samples were returned to the experimenters on a convenient day within a week of collection. At this point, participants who did not meet the minimum compliance requirements (see below) were asked to collect an additional day of samples. All saliva samples were stored at −30° C until analysis.
Measures
Questionnaires
Attribution body esteem
Attribution body esteem was assessed using the attribution subscale of the Body Esteem Scale for Adults and Adolescents (BESAA) (Mendelson et al., 2001). Attribution body esteem is conceptualized as a distinct aspect of body esteem that is closely related to feelings about one’s body in a social context. Examples of items include, “Other people consider me good looking” and “People my own age like my looks.” Questions focused on how often various feelings are experienced with responses ranging from ‘never’ to ‘always’ (0 to 4) on a 5-point Likert scale. For example, if a person answers ‘never’ to “Other people consider me good looking,” they feel that people never think they are good looking. The attribution body esteem subscale includes five items with overall average scores ranging from 0 to 4 with higher mean scores representing higher attribution body esteem, i.e., perceiving that others frequently evaluate one’s body and appearance positively. The subscale has good reliability (α = .81) (Medelson et al., 2001).
Social exchanges
Participants completed the Positive and Negative Social Exchanges (PNSE) scale to assess the frequency and impact of positive and negative social exchanges (Newsom et al., 2005). Positive social exchanges included four subtypes: informational support, instrumental support, emotional support, companionship. Negative social exchanges also included four subtypes: unwanted advice or intrusion, failure to provide help, unsympathetic or insensitive behavior, and rejection or neglect. Participants were first asked to report how often they had experienced each type of exchange within the past month and then how satisfied (for the positive exchanges) or how bothered (for the negative exchanges) they were by the exchanges they experienced on a four-point scale. The total numbers of positive and negative exchanges are each summed across the four subtypes to calculate a score for total positive and total negative exchanges. Additionally, the ratings of satisfaction and bothersomeness are each summed with higher numbers representing higher satisfaction with positive exchanges and more feelings of being bothered by negative exchanges, respectively. Satisfaction and bothersomeness scores range from 0 to 24. To be able to differentiate effects from the sheer number of positive or negative exchanges from relative effects, an additional variable was calculated called percentage of negative exchanges. This variable assessed the ratio of negative exchanges experienced relative to positive by dividing the total negative exchanges by the total positive exchanges.
Perceived chronic stress
Participants completed the 10-item Perceived Stress Scale (PSS) to assess self-reported perceived chronic stress (Cohen, Kamarck, & Mermelstein, 1983). Responses were given on a Likert rating scale ranging from ‘never’ to ‘very often’ (0 to 4). For example, “In the last month, how often have you felt that you were unable to control the important things in your life?” Answers were summed to calculate a perceived stress score with higher numbers representing more perceived stress with possible scores ranging from 0 to 40. The instrument has good reliability (α = .78) (Cohen & Hoberman, 1983).
Social support
The Interpersonal Support Evaluation List (ISEL) was used to assess perceived social support (Cohen & Hoberman, 1983). This 40-item scale captures the availability of four different types of social support: appraisal support, tangible support, self-esteem, and belonging. For example, “When I feel lonely, there are several people I can talk to.” Items are counterbalanced for positive and negative valence and rated on a 1 to 4 scale ranging from “definitely true” to “definitely false.” An overall social support sum score is calculated such that higher scores represent more perceived social support. Possible scores range from 40 to 160.
Home sampling
As mentioned above, participants collected six saliva samples at specific time-points on each of two consecutive weekdays. To assess compliance with the actual sampling protocol, participants were asked to record not only the theoretical sampling time-points computed relative to the time they woke up, they also recorded the actual time a sample was taken. These actual times relative to the intended times were used to assess compliance with sampling protocol. Furthermore, participants were asked to collect an additional day of samples if they did not return the minimum amount of completed samples, defined as four consecutive samples per day, with none of the missing samples being from the first three time points. No participants were excluded for non-compliance with the saliva sampling protocol.
Biological analysis
Saliva samples were stored at −30C until completion of the study. Samples were then thawed, centrifuged, and cortisol measured in duplicates using a commercially available chemiluminescence assay kit. Inter and intra-assay correlations were below 8%. Each of the six cortisol values from day 1 was averaged with the corresponding value from day 2 to compute one aggregated daily cortisol rhythm described by six values. Using the averaged daily rhythm, two indices of daily cortisol rhythm were computed for each participant: cortisol awakening response (CAR) increases (individual peak value minus wake-up value) and cortisol slope (individual peak value minus +13 hours value). Individual peak value was sample 2 (+30 minutes) or sample 3 (+60), whichever was higher. The CAR increase index measures the maximum magnitude of the awakening response whereas the cortisol slope index captures the maximum variability in an individual’s basal cortisol rhythm. Notably, for female participants, menstrual cycle phase was not controlled as previous studies have indicated that cycle phase does not affect cortisol awakening responses or diurnal variation in cortisol (Fries, 2009; Kirschbaum, Kudielka, Gaab, Schommer, & Hellhammer, 1999; Kudielka & Kirschbaum, 2003).
Data Analysis
Before testing the study hypotheses, descriptive analyses were ran on all study variables. BMI was controlled for in all subsequent analyses in order to focus on participants’ feelings about their appearance independent of their actual body size. Gender was controlled for as well, as previous research has consistently documented gender differences in perceived stress (e.g., Cohen & Janicki-Deverts, 2012) and body esteem (e.g., Mendelson et al., 2001).
Next, a series of partial correlations were computed to determine interrelationships among the main variables of interest as well as to test the first study hypothesis predicting that higher numbers of negative social exchanges would be associated with increased perceived stress as well as altered daily cortisol patterns. To test the hypothesis that attribution body esteem would moderate the relationship between social exchanges and stress, several sets of hierarchical regression analyses were computed. Moderation analyses were conducted according to recommended procedures for testing interaction effects in multiple regression models (Aiken & West, 1991). More specifically, predictor variables (i.e., attribution body esteem, total negative social exchanges, total positive exchanges) were z-standardized and the respective interaction terms were computed (i.e., attribution body esteem-by-negative exchanges, attribution body esteem-by-positive exchanges). Separate sets of regression analyses were computed for each of the three stress-related outcome measures (PSS, CAR increase, slope).
Results
Preliminary Analyses
Means and standard deviations of self-report variables are documented in Table 1. Consistent with previous research, participants reported experiencing more positive exchanges than negative exchanges (see Table 1). Means for perceived stress (PSS) were within the expected range based on previous studies of probability samples (Cohen & Janicki-Deverts, 2012). Interestingly, attribution body esteem was not significantly different between males and females (male M = 2.49, SD = .79; female M = 2.07, SD = .78; t = −1.63, p = .11; Cohen’s d = .54) and not associated with BMI (r = −.21, p = .22). Based on the large effect size and for conceptual reasons, gender and BMI were controlled in subsequent analyses.
Table 1.
Means (M) and standard deviations (SD) of main study variables.
| Variable | M | SD |
|---|---|---|
| Perceived chronic stress | 16.26 | 6.39 |
| Attribution body esteem | 2.24 | .80 |
| Negative exchanges | 33.45 | 27.03 |
| Positive exchanges | 154.79 | 95.10 |
| Bothersomeness | 5.55 | 2.82 |
| Satisfaction | 9.82 | 2.14 |
| % Negative exchanges | 19% | 12% |
| ISEL | 135.13 | 16.65 |
Note. Positive exchanges = Total number of positive exchanges from PNSE (Positive and Negative Social Exchanges); Negative exchanges = Total number of negative exchanges from PNSE; Bothersomeness = Total bothersomeness ratings for negative exchanges from PNSE; Satisfaction = Total satisfaction rating for positive exchanges from PNSE; % Negative Exchanges = Total Negative Exchanges from PNSE divided by Total Positive Exchanges from PNSE; ISEL = Interpersonal Support Evaluation List.
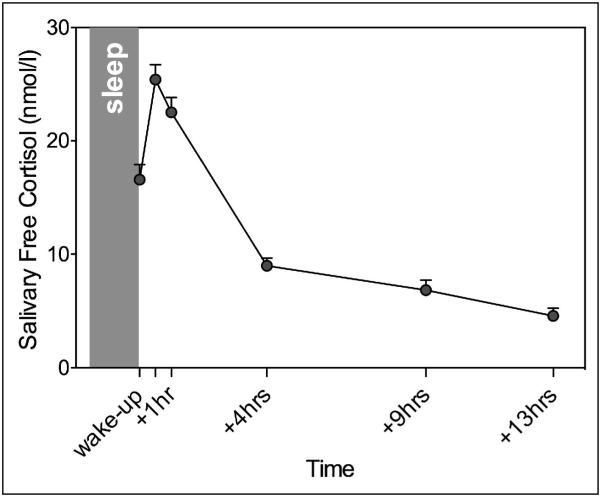
Repeated measures ANOVA of averaged cortisol concentrations revealed significant changes in cortisol levels over time, such that values increased early in the morning with subsequent decreases thereafter (F(5, 170) = 75.83, p = .066) (see Figure 1). Based on the averaged daily profile, maximum cortisol increases and cortisol slopes were computed as described earlier with maximum cortisol increase averaging 10.66 nmol/l (± 9.99 nmol/l) and decrease in slope averaging 24.48 nmol/l (± 7.62 nmol/l).
Figure 1.
Daily cortisol rhythm from six time points across the day starting upon awakening. Values average over two days.
Next, associations were examined within the various predictor variables and within the three stress-related outcome variables. Partial correlation analyses revealed that individuals who felt others were viewing their bodies more negatively reported fewer positive social exchanges (r = .32, p = .06). Contrary to the study’s hypothesis, however, such attributions were not associated with total number of negative exchanges (r = −.09, p = .59). Furthermore, although blunted CARs were associated with flatter cortisol slopes (r = .39, p = .02), self-reported perceived stress was not associated with either cortisol index (CAR: r = .14, p = .41; slope: r = .18, p = .29). For all other relationships between the main study variables, see Table 2.
Table 2.
Summary of correlations between main study variables (controlling for BMI and gender).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | PSS | - | .14 | .18 | −.48** | .33* | −.18 | .53*** | −.32^ | .45** | −.48** |
| 2. | CAR increase | .14 | - | .39* | −.11 | −.29^ | −.24 | .09 | −.17 | −.15 | −.19 |
| 3. | Cortisol slope | .18 | .39* | - | −..09 | −.29^ | .10 | .42* | −.11 | −.27 | −.13 |
| 4. |
Attribution body
esteem |
−.48** | −.11 | −.09 | - | −.09 | .32^ | −.45** | .26 | −.28 | .62*** |
| 5. | Negative Exchanges | .33* | − .29^ |
− .29^ |
−.09 | - | .32^ | .16 | .003 | .68*** | −.16 |
| 6. | Positive Exchanges | −.18 | −.24 | .10 | .32^ | .32^ | - | −.13 | .56*** | −.32^ | .52*** |
| 7. | Bothersomeness | .53*** | .09 | .42* | −.45** | −.16 | .13 | - | −.37* | .31^ | −.43** |
| 8. | Satisfaction | −.32^ | −.17 | −.11 | .26 | .003 | .56*** | −.37* | - | − .58*** |
.70*** |
| 9. | % Negative Exchanges | .45** | −.15 | −.27 | −.28 | − .68*** |
−.32^ | .31^ | − .58*** |
- | − .54*** |
| 10. | ISEL | −.48** | −.19 | −.13 | .62*** | −.16 | .52*** | −.43** | .70*** | − .54*** |
- |
Note. PSS = Perceived Stress Scale; CAR increase = wake-up value minus peak cortisol value; cortisol slope = peak value minus last evening value; Attribution body esteem = Attribution subscale of Body Esteem Scale for Adolescents and Adults; Positive exchanges = Total number of positive exchanges from PNSE (Positive and Negative Social Exchanges); Negative exchanges = Total number of negative exchanges from PNSE; Bothersomeness = Total bothersomeness ratings for negative exchanges from PNSE; Satisfaction = Total satisfaction rating for positive exchanges from PNSE; % Neg Exchanges = Total Negative Exchanges from PNSE divided by Total Positive Exchanges from PNSE; ISEL = Interpersonal Support Evaluation List – Global score.
p < .05;
p < .01;
p ≤ .001;
p < .10
Next sets of hierarchical regression analyses were computed to determine whether, depending on attribution body esteem, the number of negative social exchanges or the number of positive social exchanges differentially predicted self-reported stress and biological stress marker variables. Results of regression analyses are presented in Table 3.
Table 3.
Regressions results for attribution body esteem and negative (A) and positive (B) social exchanges predicting perceived stress and Cortisol indices.
| (A) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DV: Perceived Stress (PSS) | DV: CAR increase | DV: Cortisol slope | ||||||||||
|
| ||||||||||||
| Variable | β | SE | B | p | β | SE | B | p | β | SE | B | p |
|
| ||||||||||||
| BMI | −.19 | .26 | −32 | .23 | .08 | .50 | .23 | .65 | .22 | .37 | .44 | .24 |
| Gender | −.17 | 1.88 | −2.13 | .27 | .08 | 3.60 | 1.56 | .67 | −.10 | 2.66 | −1.48 | .58 |
| ABE | −.49 | .93 | −3.11 | .002* | −.15 | 1.78 | −1.50 | .41 | −.10 | 1.32 | −.73 | .58 |
| Negative exchanges | .24 | .93 | 1.56 | .10 | −.31 | 1.77 | −3.09 | .09 | −.27 | 1.31 | −2.04 | .13 |
| ABE × Negative exchanges | −.21 | 1.00 | −1.36 | .18 | −.01 | 1.91 | −.14 | .94 | .18 | 1.41 | 1.45 | .31 |
| R2 | .40 | .103 | .16 | |||||||||
|
| ||||||||||||
| (B) | ||||||||||||
|
| ||||||||||||
| DV: Perceived Stress (PSS) | DV: CAR increase | DV: Cortisol slope | ||||||||||
|
| ||||||||||||
| Variable | β | SE | B | p | β | SE | B | p | β | SE | B | p |
|
| ||||||||||||
| BMI | −.06 | .27 | −.10 | .71 | .02 | .45 | .05 | .91 | .06 | .33 | .12 | .72 |
| Gender | −.15 | 2.05 | −1.91 | .36 | −.03 | 3.45 | −.62 | .86 | −.18 | 2.54 | −2.83 | .27 |
| ABE | −.47 | 1.06 | −3.02 | .007* | −.07 | 1.78 | −.74 | .68 | −.17 | 1.31 | −1.32 | .32 |
| Positive exchanges | −.04 | 1.01 | −.26 | .80 | −.18 | 1.71 | −1.78 | .31 | .20 | 1.26 | 1.53 | .23 |
| ABE × Positive exchanges | −.06 | 1.06 | −.40 | .71 | .35 | 1.79 | 3.80 | .04* | .43 | 1.31 | 3.54 | .01* |
| R2 | .29 | .18 | .23 | |||||||||
|
| ||||||||||||
Note. ABE = Attribution body esteem.
Body esteem dependent effects of social exchanges on perceived chronic stress
Although a partial correlation indicated a significant positive association between negative exchanges and perceived stress (r = .33 p = .05; see Table 2), combining negative exchanges with attribution body esteem in one regression model abolished this effect, such that when controlling for attribution body esteem, higher numbers of negative exchanges no longer predicted perceived stress (see Table 3). Similarly, the number of positive social exchanges in itself did not predict perceived stress, nor did it interact with attribution body esteem to predict perceived stress. Nevertheless, how individuals felt others were judging their bodies was a significant predictor of perceived stress in both models, such that more negative attributions were associated with higher perceived stress levels, independent of numbers of positive or negative exchanges.
Body esteem dependent effects of social exchanges on daily cortisol rhythm
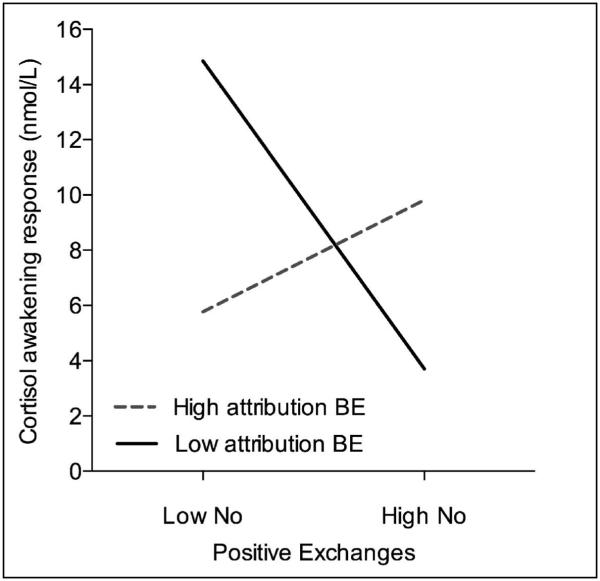
In regression analyses assessing cortisol indices, a trend was revealed for higher numbers of negative exchanges to be associated with blunted CAR increases, independent of attribution body esteem. On the contrary, neither attribution body esteem nor number of positive exchanges predicted CAR increases. However, number of positive exchanges did interact with attribution body esteem to predict CAR increase (see Figure 2). Simple slopes analyses were computed to probe the significant interaction using values one standard deviation above and one standard deviation below the mean for attribution body esteem (Holmbeck, 2002). These analyses revealed that individuals who felt others were viewing their bodies less positively while at the same time experiencing higher numbers of positive exchanges exhibited a blunted CAR (B = −5.57, β = −.56, SE = 2.29, p = .02) whereas individuals with higher attribution body esteem showed no differences in the magnitude of CAR based on the number of positive exchanges (B = 2.02, β = .20, SE = 2.63, p = .45).
Figure 2.
Higher numbers of positive exchanges are related to smaller cortisol maximum increases for individuals with low attribution body esteem, but not for individuals with high attribution body esteem.
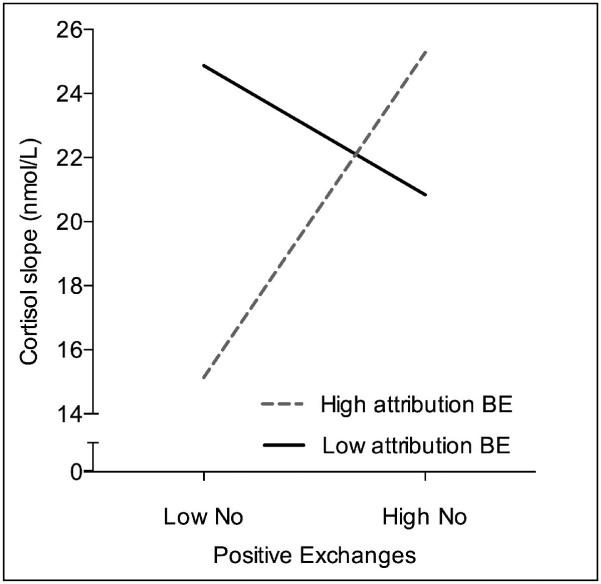
Similar to CAR increases, cortisol slopes were not predicted by total number of negative exchanges or by total number of positive social exchanges. Furthermore, attribution body esteem neither predicted cortisol slopes independently of number of negative or positive exchanges nor dependent on number of negative exchanges. However, again an interaction effect was found between number of positive exchanges and attribution body esteem. More specifically, individuals who felt others were judging their bodies more positively while experiencing fewer positive exchanges demonstrated significantly blunted cortisol slope (B = 5.07, β = .67, SE = 1.94, p = .01) whereas individuals with lower attribution body esteem appeared to be unaffected by the number of positive exchanges (B = −2.02, β = −.27, SE = 1.69, p = .24; see Figure 3).
Figure 3.
Higher numbers of positive social exchanges are related to flatter cortisol slopes for individuals with high body esteem, but not for individuals with low body esteem.
The above analyses were repeated with total exchanges (sum of negative exchanges and positive exchanges) and revealed the same interaction effects with attribution body esteem predicting CAR increase and cortisol slope. Notably, all significant main and interaction effects described remained significant when considering menstrual cycle phase as a covariate or with gender and/or BMI uncontrolled.
Discriminatory Analyses
To further investigate the role of social exchanges and determine whether the actual numbers of exchanges are the strongest predictors of stress-related variables, the above analyses were repeated with the percentage of negative exchanges, the relevance of social exchanges (bothersomeness and satisfaction), and social support as predictor variables.
Although a higher number of negative exchanges relative to positive exchanges was associated with higher perceived chronic stress as well as a trend for flatter cortisol slopes (β = .31, p = .04, β = −.33, p = .07, respectively, CAR increases: β = −.24, p = .20), these effects did not differ for individuals with higher and lower attribution body esteem (all p > .30). When assessing relevance of social exchanges instead of number of exchanges, bothersomeness of negative social exchanges was found to be associated with increased perceived stress (β = .47 p = .007) and steeper cortisol slopes (β = .44, p = .03) but not CAR increases (β = .14, p = .43). These effects were independent of attribution body esteem (all p > .14). Satisfaction with positive social exchanges was not associated with any of the stress-related variables nor did it interact with attribution body esteem to predict stress indices (all p > .13).
Lastly, to test whether the effects of social exchanges are secondary to variations in perceived social support, social support was examined as a predictor variable. Social support did not predict perceived stress or diurnal cortisol variables independently or dependent on attribution body esteem (all p > .10).
Discussion
In summary, the present study found that both the number of negative exchanges a person reports as well as how positively a person feels others judge his/her body are linked to perceived chronic stress and related changes in biological stress systems. Interestingly, those physiological changes were influenced specifically by positive social exchanges with differing relationships depending on attribution body esteem. More specifically, a blunted rise in morning cortisol was associated with higher numbers of positive social exchanges only for individuals perceiving their bodies to be judged negatively. Cortisol slopes, on the other hand, were flatter in individuals perceiving their bodies to be judged positively and experiencing fewer positive social exchanges.
Independent effects of body esteem and social exchanges on perceived chronic stress
The current study revealed that lower attribution body esteem was associated with higher self-reported chronic stress independent of the number or type of social exchanges participants experienced during the past month. This is consistent with previous findings (Croghan et al., 2006). However, the present study is the first to demonstrate this relationship for perceived negative appearance judgments by others, extending the literature and emphasizing the importance of a specific subtype of body esteem closely related to feelings about one’s body in a social context.
The study further replicated earlier findings (Bolger et al., 1989) linking negative social exchanges and perceived chronic stress. Closer examination suggests that how one perceives his/her body to be judged by others is more stress-relevant than how many negative exchanges one experiences. Additionally, negative exchanges were reported infrequently in general, which questions the usefulness of this measure when aiming to evaluate stress effects of social interactions. It may also explain why negative exchanges were only linked to self-reported chronic stress, not to biological stress markers. Perhaps participants’ memory of stress linked to the past months’ infrequent negative exchanges is sufficient to impact their psychological stress report, but not sufficient to detect the cumulative effect of acute physiological stress responses. However, the association between bothersomeness and diurnal cortisol slope was not in the expected direction. Previous literature would suggest something potentially chronically stressful like bothersomeness associated with negative exchanges to predict a flatter cortisol slope. It is notable that the bothersomeness scale had limited variability and overall, participants reported few negative exchanges. Thus, because it is not clear how generalizable it is, this finding should be interpreted with caution.
Role of positive exchanges in body esteem-related stress
Though the total number of positive social exchanges participants reported was not associated with any stress measures itself, differential effects were observed dependent on attribution body esteem. Specifically, higher numbers of positive social exchanges were related to blunted morning rises in cortisol only for individuals with lower attribution body esteem. As previously suggested based on self-verification theory, those with lower attribution body esteem may actually prefer negative feedback that is consistent with their own negative self-view (Giesler et al., 1996). As such, frequent positive exchanges may in fact be stressful specifically for this group.
On the other hand, for individuals with low body esteem, every social exchange may carry the potential for negative judgment of their appearance. The anticipation of the day’s upcoming potentially negative social exchanges may be more stressful for these individuals. Hence, even when social exchanges turn out to be positive, higher numbers of exchanges may constitute “repeated hits” of stress for individuals with lower attribution body esteem (McEwen, 1998). Given the inevitability and uncontrollability of social interactions, feeling anticipatory stress on a daily basis would then sum up to the observed chronic stress-related biological dysfunctions consistently linked to negative health outcomes (Chrousos & Gold, 1992). This idea could also explain why perceived chronic stress is not linked to positive exchanges. Anticipatory stress takes its toll regardless of whether the subsequent experience turns out to be positive or negative, whereas both positive and negative experiences weigh into reporting perceived chronic stress. In summary, these findings emphasize the importance of considering perceived appearance judgment by others not only in current stress theories, but also as a health risk factor.
For individuals with high attribution body esteem, no associations were observed between negative or positive exchanges and the magnitude of cortisol awakening responses. This suggests that these individuals may not be as susceptible to anticipatory stress related to upcoming exchanges, maybe because they approach the day believing that others will judge them positively. On the other hand, individuals with higher attribution body esteem exhibited flatter cortisol slopes across the day only when they also reported lower numbers of positive exchanges. In other words, positive body-related attributions are not necessarily stress-protective in all contexts. It could be speculated that despite generally feeling good about the way their appearance is judged, these individuals may still be internalizing an unattainable societal ideal for appearance, such that lack of validation through positive social exchanges makes them susceptible to stress and its biological consequences. Importantly, further probing of this relationship revealed that only a subset of participants who reported high attribution body esteem also reported low numbers of positive exchanges. Although this association should thus be interpreted cautiously, it does provide preliminary evidence that even those with who perceive others judge their appearance positively may be at risk for chronic stress. Additional research is needed to further investigate for whom and in what contexts this is most likely to occur.
Taken together, although research on body esteem consistently addresses and discusses the negative health consequences of low body esteem, the current findings put individuals with high body esteem into the spotlight by uncovering for the first time potential health consequences of stress associated with maintaining a high body esteem. Furthermore, these findings point to differential health-relevant pathways by which social interactions can be associated with physiological stress depending upon an individual’s expectations about how others will judge their appearance.
Limitations
It is important to note that this study’s measure of social exchanges did not allow for distinguishing between actual negative interactions, interpretation of neutral or positive interactions as negative, and anticipation of negative interactions. The study did assess how bothered or satisfied participants were with the reported social exchanges and neither revealed attribution body esteem-dependent links to stress measures. As previously described, participants reported few negative exchanges. Because of this, positive exchanges drive the results of analyses examining total numbers of social exchanges making it difficult to determine the role of overall exchanges. Additionally, daily social exchanges during the past month were assessed retrospectively as opposed to every day. Future studies would benefit from utilizing designs with ecological momentary assessment to determine whether the associations in the present study persist on a daily basis. Furthermore, daily assessment of social exchanges with corresponding longer-term measurement of diurnal cortisol, may reveal links between daily variation in numbers social exchanges and cortisol that the present study was unable to detect. In addition, information on appearance investment was not collected to consider along with ratings of attribution body esteem. It could be argued that the personal importance put on one’s appearance plays a role in how attribution body esteem affects social exchanges. Furthermore, assessing self-esteem in future studies would help to determine the differential effects of attribution body esteem on stress-related outcome measures over and above overall feelings of self-esteem. Finally, the design of the study does not allow for establishing directionality or causality.
It should be noted that although post-hoc power analyses confirm adequate power to detect medium to large effects, the relatively small sample size limits the ability to examine additional covariates and detect weaker relationships. In other words, it is possible that other potentially important relationships cannot be detected in the current sample.
Implications and Outlook
In summary, despite a substantial body of literature describing the relationships between social interactions, stress, and health, the current study is among the first to link specifically daily social exchanges to both psychological and biological stress. Thus, these findings extend the literature on the health relevance of the frequency of social interactions themselves without regard to social support or strain associated with those interactions. Furthermore, the study highlight a factor that affects the interpretation of social exchanges and thereby moderates its associations with stress: attribution body esteem or feelings about how others are judging one’s appearance. The present findings thus (1) identify a specific part of the way an individual feels about his/her body that is stressful, namely, how one perceives others are judging one’s looks, and (2) suggest underlying mechanisms, i.e., changes in basal cortisol rhythm, linking low body esteem to negative health outcomes. It can be speculated that individuals with low attribution body esteem may feel more anticipatory stress associated with the day’s upcoming social interactions putting them at higher risk for negative health outcomes. On the other hand, high attribution body esteem may not necessarily be stress protective without a specific social context that includes adequate positive feedback from social interactions. As such, these findings caution against stress reduction programs aiming only at reducing negative exchanges or only focusing on individuals with low attribution body esteem.
Based on the study’s findings, several directions for future studies are particularly promising. First, examining the role of attribution body esteem in acute psychosocial stress responses may help uncover early health-relevant warning signs. Furthermore, assessing different age groups would investigate potential changes in the relevance of perceived appearance judgments by others. Strategies individuals use to minimize stress from social interactions may depend on their attribution body esteem. Considering these strategies may help understand inter-individual differences in health impacts of attribution body esteem. Finally, examining the relative contribution of other inter-individual factors such as personality and self-esteem will help to elucidate the specific role of body esteem in connection with social interactions and stress.
Highlights.
Daily social exchanges are associated with both psychological and biological stress.
Perceived appearance judgments moderate this relationship.
Not only low but also high body esteem is associated with biological stress effects.
Acknowledgments
This work was supported by NIGMS Brain-Body-Behavior Interface in Learning and Development Across the Lifespan training grant T32GM084907 (A.M.G. & S.B.L) and NIA training grant T32AG000204 (N.J.S.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adam EK, Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009;34(10):1423–1436. doi: 10.1016/j.psyneuen.2009.06.011. doi:10.1016/j.psyneuen.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Aiken L, West S. Multiple Regression: Testing and Interpreting Interaction Effects. Sage; Thousand Oaks, CA: 1991. [Google Scholar]
- Bolger N, DeLongis A, Kessler RC, Schilling EA. Effects of daily stress on negative mood. Journal Of Personality And Social Psychology. 1989;57(5):808–818. doi: 10.1037//0022-3514.57.5.808. doi:10.1037/0022-3514.57.5.808. [DOI] [PubMed] [Google Scholar]
- Bordo S. Unbearable weight: Feminism, Western culture, and the body. University of California Press; 2003. [Google Scholar]
- Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cohen S, Janicki-Deverts D. Who's stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006 and 2009. Journal of Applied Social Psychology. 2012 [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Croghan IT, Bronars C, Patten CA, Schroeder DR, Nirelli LM, Thomas JL, Hurt RD. Is Smoking related to body image satisfaction, stress, and self-esteem in young adults? American Journal of Health Behavior. 2006;30(3):322–333. doi: 10.5555/ajhb.2006.30.3.322. doi: 10.5993/AJHB.30.3.10. [DOI] [PubMed] [Google Scholar]
- Chrousos GP, Gold PW. The concepts of stress and stress system disorders: overview of physical and behavioral homeostasis. Journal of the American Medical Association. 1992;267(9):1244–1252. doi:10.1001/jama.1992.03480090092034. [PubMed] [Google Scholar]
- Dickerson SS, Mycek PJ, Zaldivar F. Negative social evaluation, but not mere social presence, elicits cortisol responses to a laboratory stressor task. Health Psychology. 2008;27(1):116–121. doi: 10.1037/0278-6133.27.1.116. doi:10.1037/0278-6133.27.1.116. [DOI] [PubMed] [Google Scholar]
- Finch JF, Okun MA, Pool GJ, Ruehlman LS. A comparison of the influence of conflictual and supportive social interactions on psychological distress. Journal of Personality. 1999;67:581–621. doi: 10.1111/1467-6494.00066. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Roberts T-A. Objectification theory: Toward understanding women's lived experiences and mental health risks. Psychology of Women Quarterly. 1997;21(2):173–206. doi: 10.1111/j.1471-6402.1997.tb00108.x. [Google Scholar]
- Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): Facts and future directions. International Journal Of Psychophysiology. 2009;72(1):67–73. doi: 10.1016/j.ijpsycho.2008.03.014. doi:10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Giesler R, Josephs RA, Swann WR. Self-verification in clinical depression: The desire for negative evaluation. Journal Of Abnormal Psychology. 1996;105(3):358–368. doi: 10.1037//0021-843x.105.3.358. doi:10.1037/0021-843X.105.3.358. [DOI] [PubMed] [Google Scholar]
- Goldstein DS, McEwen B. Allostasis, homeostats, and the nature of stress. Stress: The International Journal On The Biology Of Stress. 2002;5(1):55–58. doi: 10.1080/102538902900012345. doi:10.1080/102538902900012345. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal Of Pediatric Psychology. 2002;27(1):87–96. doi: 10.1093/jpepsy/27.1.87. doi:10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus–pituitary–adrenal axis. Psychosomatic Medicine. 1999;61:154–162. doi: 10.1097/00006842-199903000-00006. [DOI] [PubMed] [Google Scholar]
- Kors DJ, Linden W, Gerin W. Evaluation interferes with social support: Effects on cardiovascular stress reactivity in women. Journal Of Social And Clinical Psychology. 1997;16(1):1–23. doi:10.1521/jscp.1997.16.1.1. [Google Scholar]
- Kudielka BM, Kirschbaum CC. Awakening cortisol responses are influenced by health status and awakening time but not by menstrual cycle phase. Psychoneuroendocrinology. 2003;28(1):35–47. doi: 10.1016/s0306-4530(02)00008-2. doi:10.1016/S0306-4530(02)00008-2. [DOI] [PubMed] [Google Scholar]
- Kumari M, Shipley M, Stafford M, Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II study. Journal of Clinical Endocrinological Metabolism. 2011;96(5):1478–85. doi: 10.1210/jc.2010-2137. doi: 10.1210/jc.2010-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews K, Schwartz J, Cohen S, Seeman T. Diurnal cortisol decline is related to coronary calcification: CARDIA study. Psychosomatic Medicine. 2006;68(5):657–661. doi: 10.1097/01.psy.0000244071.42939.0e. doi:10.1097/01.psy.0000244071.42939.0e. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. In: McCann SM, Lipton JM, Sternberg EM, Chrousos GP, Gold PW, Smith CC, editors. Annals of the New York Academy of Sciences. Vol. 840. New York Academy of Sciences; New York, NY US: 1998. pp. 33–44. S. M. Neuroimmunomodulation: Molecular aspects, integrative systems, and clinical advances. [DOI] [PubMed] [Google Scholar]
- McClintock JM, Evans IM. The underlying psychopathology of eating disorders and social phobia: A structural equation analysis. Eating Behaviors. 2001;2(3):247–261. doi: 10.1016/s1471-0153(01)00032-0. doi:10.1016/S1471-0153(01)00032-0. [DOI] [PubMed] [Google Scholar]
- Mendelson BK, Mendelson MJ, White DR. Body-esteem scale for adolescents and adults. Journal of Personality Assessment. 2001;76:90–106. doi: 10.1207/S15327752JPA7601_6. [DOI] [PubMed] [Google Scholar]
- Newsom JT, Rook KS, Nishishiba M, Sorkin DH, Mahan TL. Understanding the relative importance of positive and negative social exchanges: examining specific domains and appraisals. Journal of Gerontology: Psychological Sciences. 2005;60B:304–312. doi: 10.1093/geronb/60.6.p304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newsom JT, Mahan TL, Rook KS, Krause N. Stable negative social exchanges and health. Health Psychology. 2008;27(1):78–86. doi: 10.1037/0278-6133.27.1.78. doi:10.1037/0278-6133.27.1.78. [DOI] [PubMed] [Google Scholar]
- Newsom JT, Nishishiba M, Morgan DL, Rook KS. The relative importance of three domains of positive and negative social exchanges: A longitudinal model with comparable measures. Psychology and Aging. 2003;18:746–754. doi: 10.1037/0882-7974.18.4.746. [DOI] [PubMed] [Google Scholar]
- Okun MA, Keith VM. Effects of positive and negative social exchanges with various sources on depressive symptoms in younger and older adults. The Journals Of Gerontology: Series B: Psychological Sciences And Social Sciences. 1998;53B(1):P4–P20. doi: 10.1093/geronb/53b.1.p4. doi:10.1093/geronb/53B.1.P4. [DOI] [PubMed] [Google Scholar]
- Seltzer M, Almeida DM, Greenberg JS, Savla J, Stawski RS, Hong J, Taylor J. Psychological and biological markers of daily lives of midlife parents of children with disabilities. Journal Of Health And Social Behavior. 2009;50(1):1–15. doi: 10.1177/002214650905000101. doi:10.1177/002214650905000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stetler C, Miller GE. Blunted cortisol response to awakening in mild to moderate depression: regulatory influences of sleep patterns and social contacts. Journal Of Abnormal Psychology. 2005;114(4):697–705. doi: 10.1037/0021-843X.114.4.697. doi:10.1037/0021-843X.114.4.697. [DOI] [PubMed] [Google Scholar]
- Tsigos C, Chrousos GP. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. Journal of Psychosomatic Research. 2002;53:865–871. doi: 10.1016/s0022-3999(02)00429-4. [DOI] [PubMed] [Google Scholar]
- Wertheim E, Paxton S, Blaney SM. Risk factors for the development of body image disturbances. In: Thompson JK, editor. Handbook of eating disorders and obesity. John Wiley & Sons; Hoboken, NJ: 2004. pp. 463–494. 2004-00177-023. [Google Scholar]