Children with chronic health conditions (CHCs) learn how to manage their conditions through everyday life experiences with their families, peers, health providers, and others in their communities. While most studies using children’s perspectives describe disease specific management issues and tend to be more skill related, non-categorical or non-disease-specific issues are largely overlooked (Wollenhaupt, Rodgers, & Sawin, 2012). Non-categorical studies, because they may be applied to a multitude of conditions, may be of special benefit to future clinical practice, health care policy, and research (Rolland, 1994). The purpose of this qualitative descriptive study was to systematically describe the understandings of condition management from the perspectives of school-aged children (8 – 13 years) with a variety of CHCs.
School-aged children are transitioning from concrete ways of thinking to cognitive thought processes that are more complex and intellectual (Vygotsky, [1967],2004). Children’s understanding also varies according to everyday experiences. The lives of children with CHC are filled with daily reminders and potential learning experiences related to their condition (Crisp, Ungerer, & Goodnow, 1996; McMenamy & Perrin, 2008). Although the family remains the main source of information and guidance for the school-aged child, sustained encounters outside the home and family environment provide opportunities for expanded experiences (Coll & Szalacha, 2004). Thus, school-aged children with CHCs begin to learn how to navigate life and their conditions outside the home. Their families are then challenged to expand condition management from the home to include the school and the community as their children engage in these settings and rely more on adults outside the family structure (Emiliani, Bertocchi, Poti, & Palareti, 2011).
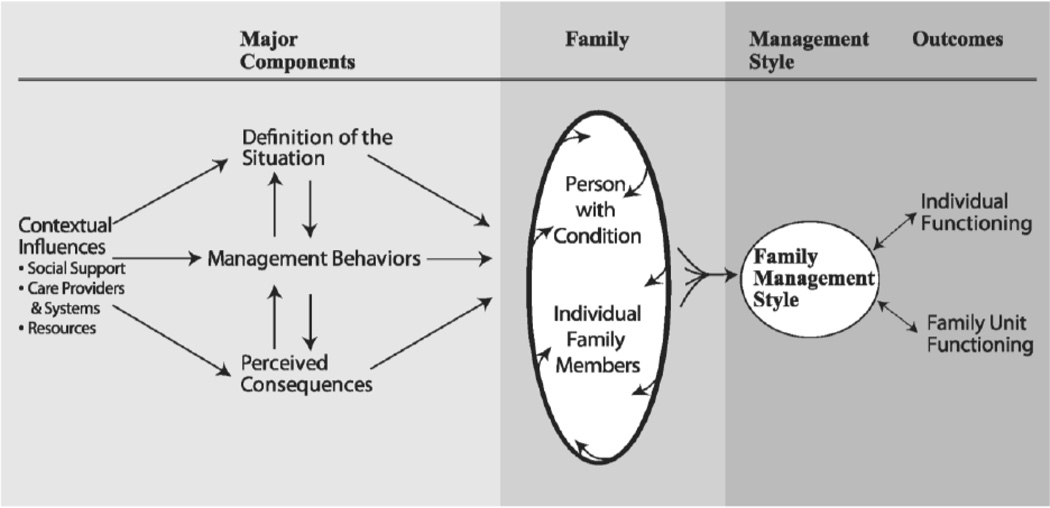
The Family Management Style Framework (FMSF) (Figure 1) was developed using symbolic interactionism (Blumer, 1969) to describe the process of family management, identifying how families define the condition, manage it, and perceive the consequences of the condition (Knafl, Deatrick, & Havill, 2012). The FMSF has been used to explore family management of a variety of conditions in a non-categorical or non-disease-specific manner and to identify the domains or categories that are common across disease entities, with findings applicable to a wide range of health conditions (Knafl, et al., 2012). The major components within the framework, including definition of the situation, management behaviors, and perceived consequences, provide us with the parents’ perspectives on non-disease specific condition management, that is, how they see the child and the condition, the amount of effort it takes to manage the condition and the disruption the condition causes the family, and the way the parents are thinking about the child’s future (Knafl, et al., 2012). The FMSF was developed predominantly from information gathered from the parents of children with CHCs, but as can be seen from the framework, differentiates family members and the person with the condition. This study adds the perspectives of school-aged children with CHCs within the context of family management and describes how these children understand their condition and incorporate it into their daily lives.
Figure 1.
Current Model of the Family Management Style Framework
Reprinted from “Knafl, K.A. and Deatrick, J.A. (February 2012). Continued development of the family management style framework. Journal of Family Nursing. 18(1), 11-35.
DOI:10.1177/1074840711430665. Copyright 2012 by Sage Publications.
Design and Methods
This qualitative, descriptive study identified the perspectives of school-aged children with CHCs using directed content analysis. Directed content analyses are based on an a priori framework that guide the creation of interview guide and analytic codes (Hsieh, H. F., & Shannon, S. E., 2005). The FMSF dimensions (defining, managing, and perceived consequences of the condition) directed the development of the interview guide as well as the analysis of the interviews. Data were collected through interviews with children who had been diagnosed with a CHC for at least six months and were between 8 and 13 years of age. A six-month lag from diagnosis ensured that the child and family had time to understand the reality of the diagnosis and develop an approach to condition management.
Setting and Sample
Thirty-two children with a variety of CHCs were recruited from three ambulatory clinics (endocrine, hematology, and pulmonary) in a large pediatric hospital located in the northeastern U.S. Both the hospital and the university with which it is affiliated granted IRB approval for the study prior to any recruitment activities. A purposeful, maximum variation sampling strategy was used to recruit a sample with a wide variety of condition experiences (Patton, 2002). A three-pronged approach to recruitment was used: 1) clinic recruitment via posters in the waiting room and referral from the health care provider; 2) mailings to families meeting the inclusion criteria; and 3) word of mouth. Interested parents contacted the study via phone or return mail inquiry, were contacted by phone, provided verbal consent, and then provided screening information regarding inclusion criteria and condition characteristics. If the screening criteria were met an appointment for the home interview was made. At the beginning of the interview, the first author who was principal investigator reviewed the study information with the parent and the child, answered any questions, and obtained informed consent/assent. It was made clear throughout the process that participation was voluntary.
Data Collection
The first author conducted the interviews between June 2012 and January 2013. Most of the interviews (n=30) were held at participants’ homes, although two families preferred to meet at an alternative setting, one at the local YMCA and the other at the University. While the qualitative interview data were collected from the child with a CHC, the parent completed demographic information and surveys about the child and the family (Table 1). For reporting purposes a primary/recruitment CHC was identified for each child; however, over half of the children in the sample had more than one CHC.
Table 1.
Characteristics of study population
| Characteristic | N (%) or mean (range) |
|---|---|
| Parent | 32 |
| Mother Informant | 30 (94%) |
| Age in years | 41 (32 to 51) |
| Household Income (US dollars) | 11 (30%) less than $30,000/year |
| 3 (9%) $30,000 – $59,000/year | |
| 4 (13%) $60,000 – $99,000/year | |
| 13 (41%) over $100,000/year | |
| 1 (3%) Not reported | |
| Educational Level | 24 (75%) graduated from college |
| Race/Ethnicity | 10 (31%) Black |
| 1 (3%) Hispanic | |
| 21 (66%) White | |
| Child | 32 |
| Age in years | 10.4 (8 to 13) |
| Male | 18 (56%) |
| Primary Diagnosis | |
| Asthma | 13 (41%) |
| Diabetes | 8 (25%) |
| Cystic Fibrosis | 4 (13%) |
| Hemophilia | 2 (6%) |
| Hereditary Spherocytosis | 1 (3%) |
| Phenylketonuria | 1 (3%) |
| Sickle Cell Disease | 1 (3%) |
| Eosinophilic Gastrointestinal Disease | 1 (3%) |
| Chronic Sinusitis | 1 (3%) |
| Interview Location | |
| Home | 30 (94%) |
| Local YMCA | 1 (3%) |
| School of Nursing | 1 (3%) |
The in-depth, semi-structured interviews were conducted using open-ended questions focused on children’s descriptions of their families, what it was like to be diagnosed with a CHC, what typical school and weekend days were like, and how they perceived their futures. The interview guide was developed with consideration for the developmental age and abilities of the children participating in the study. Initially, the interview guide was developed from the aims of the study, directly inquiring how the children perceived their condition, managed it, and understood its consequences. In consultation with researchers experienced in conducting interviews with children, the interview guide was revised to a more conversational format. The questions dealt with the child’s everyday life, an area where they realized they in fact were the experts (Table 2). The interview guide was piloted with two children, and a few very small changes were made based on the experience of the interviewer and child feedback.
Table 2.
Interview guide
| Tell me a little about yourself |
| Draw a picture of your family, tell me about it |
| Tell me when you found out you had (name of condition) |
| Take me through a typical school day |
| Describe a typical weekend day and its difference from weekdays |
| What will it be like when you’re older? What will change? |
| Tell me your advice for: a child who just found out they have (name of condition). Your family. Your friends. |
All interviews were digitally recorded and transcribed verbatim by a transcription service. Child interviews lasted between 23 and 81 minutes; although some children seemed a little shy at the beginning, none refused to be interviewed and, once they began telling their stories and realized that there were no wrong answers, they seemed much more comfortable.
Data collection stopped when saturation on major themes was reached and no new information emerged from the child interviews (Patton, 2002). The interviewer wrote field notes shortly after leaving the family homes/interviews to document impressions and reflections so as to improve the accuracy and thoroughness of the descriptions.
Data Analysis
Analyses of the children’s responses were conducted using directed content analysis methods (Elo & Kyngas, 2008; Hsieh & Shannon, 2005), which allowed for the identification of categories related to the children’s perspectives on family management of their CHCs. We attempted to remain close to the children’s own words and meanings while using our current knowledge regarding the FMSF to guide or sensitize the inquiry (Hsieh & Shannon, 2005). The initial code list was developed using the definitions of domains and categories within the FMSF, revised to reflect the likely perspective of children. Coding of the interviews began with receipt of the first verified transcript. Each subsequent transcript was read and coded for the child’s perceptions of his or her condition, management behaviors, and consequences. Codes were then modified and grouped into categories. Constant comparison was used for subsequent interviews, allowing for analysis both of the individual data and across cases (O'Connor, Netting, & Thomas, 2008). Data collection was complete when saturation of major themes was identified (Patton, 2002). Atlas-ti (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany), a qualitative data management software program, was used to maintain and sort the interviews and related data.
Several strategies to ensure trustworthiness and credibility were used. The lead author conducted a methodical review of each interview and documented the decision process throughout the study, using audit trails. An experienced qualitative researcher (JD) listened to interviews and conducted an audit of the analyses of the data, using the audit trails as a guide. In addition, the researcher participated in a weekly qualitative collective - a group engaged in the study of qualitative methodologies – that provided feedback and confirmation of analysis process throughout the study.
Results
The 32 children in the study were between 8 and 13 years old (M=10.4 years). There was a range of family incomes and diversity of race in the sample (Table 1). Although the child was the primary informant and focus of the study, the parent (mother = 30) provided all of the demographic data as well as the condition characteristic information (Table 3). Condition characteristics were described as the 1) onset of the condition (acute or gradual), 2) progression of the condition (relapsing/remitting, progressive, stable), and 3) stigma their child experienced due to the condition. These characteristics provided a way to describe the diversity of the sample across specific diagnoses (Table 3). These data show that the parent described the onset, progression, and stigma independently of the diagnosis. For example, of the eight children with diabetes, five parents described the onset as acute, whereas three thought it was gradual; two described the course as progressive, two as constant, and four as relapsing; and five identified the condition as stigmatizing whereas three did not. These data show the diversity of this sample regarding key characteristics both within and across diagnoses and support the potential of these children to provide data regarding the cross cutting issues regarding family management of their chronic health conditions.
Table 3.
Diversity Across Conditionsa
| Condition (n) | Onset | Course | Stigma | ||||
|---|---|---|---|---|---|---|---|
| Acute | Gradual | Progressive | Constant | Relapsing | Yes – Stigma | No – Stigma | |
| Asthma (13) | 5 | 8 | 1 | 4 | 8 | 3 | 10 |
| Diabetes (8) | 5 | 3 | 2 | 2 | 4 | 5 | 3 |
| Cystic Fibrosis (5) | 2 | 3 | 1 | 3 | 1 | 4 | 1 |
| Hemophilia (2) | 2 | 0 | 0 | 2 | 0 | 1 | 1 |
| Other (4) | 1 | 1 | 0 | 3 | 1 | 2 | 2 |
| TOTALS (32) 2 diagnosed at birth; no symptoms/no onset | 15 | 15 | 4 | 14 | 14 | 15 | 17 |
| Total by Category | 30a | 32 | 32 | ||||
| Genetic | 5 | 3 | 1 | 8 | 1 | 6 | 4 |
| Developed | 10 | 12 | 3 | 6 | 13 | 9 | 13 |
Adapted from Categorization of Chronic Illnesses by Psychosocial Type (Rolland, 1994)
The results of the directed content analysis presented here are organized according to the FMSF’s three dimensions: 1) definition of the situation; 2) management behaviors; and 3) perceived consequences. Within each dimension, categories are identified that explain the perspectives of the children with CHCs who participated in the study. These categories have been named using a phrase from the child interview that best represented the child perspective.
Definition of the Situation
As the children described what their CHC meant for them, important elements related to having a chronic health condition were identified and defined. Children spoke about how they felt compared to their peers and siblings, what made their day easier or harder, what they worried about in regard to the condition and what gave them feelings of confidence or control over the condition. Quotes from the children were used to identify the themes and are as follows: They want us to be like regular kids, Sometimes I get scared, And then we’re good, It’s pretty easy for us to handle/it’s hard for us cause it’s not normal, and Mom and Dad agree/disagree. The school-aged children in this study readily described what it meant to them to have a CHC.
They (parents and providers) want us to be like regular kids
The interview began with a broad question asking the children to “…tell me a little bit about yourself?” Only a few children included the CHC in their brief introductions. Instead, most gave their age and grade, and they talked about the activities they and their friends enjoyed. Most children had to be prompted to begin talking about their condition even though they had had an active role in the assent process and knew the study was focused on how their condition affected them, both at home and away from home. They also described their daily activities differently; some readily alluded to trips to the nurses’ office for treatments during their school day, whereas others who also did those activities did not mention them.
Children talked about the things they were able to do that were typical and made themselves feel typical, comparing themselves to their siblings or friends. They also spoke about the ways that the condition limited them and their ability to participate in activities and made them feel different. Children often described that management of their health condition could be hard for them, either as hard for them to learn or hard for them to follow the recommended treatments, or both. They did, however, recognize that their abilities and understanding had changed over time as they had matured and developed.
Children discussed the way they and their friends dealt with the condition and the support the friends provided and how that made them feel typical, especially friends who had the same condition. “…you have to be able to push it aside…. you can’t go ‘oh, I can’t go with my friends cause my diabetes is messed up.’ You kind of don’t have to think about it all the time” (11-year-old, Type 1 Diabetes). For some children the condition was not a big problem, but rather something they recognized made them unique and they were proud of. Other children had more difficulty incorporating the condition into everyday life and stated that it was hard, made them feel very different than those around them, and felt that people didn’t really understand what it was like.
Sometimes I get scared
Reflecting their awareness of the seriousness of their condition, the children discussed whether their parents worried about them or if they worried about themselves. They were particularly aware their parents worried about them within the context of remembering the reaction at diagnosis. Statements such as “…she wasn’t worried about it at that time cause I wasn’t like…older yet” (9-year-old, Type 1 Diabetes) showed an awareness of the potentially serious nature of the diagnosis and the likelihood that it would change in the future.
In terms of the children’s worries, as one child with asthma stated, “Basically, when I’m swimming, sometimes I get scared and I’m like ‘Oh, no, what’s going to happen?’ I get scared that I won’t be able to breathe” (13-year-old, Asthma) There were also children on the other side of the spectrum who didn’t think the condition was very serious. One boy with asthma stated, “Mine’s just really weak…. The asthma’s weak. I don’t even think I need the medication” (11-year old, Asthma).
A few of the children spoke of knowledge they had regarding the condition that made them worry. Some children with diabetes were aware of the potential for amputations and renal failure when they were older, and a child with asthma told of knowing a friend who died because his asthma wasn’t controlled. This information confirmed the seriousness of their condition, but as one young boy stated, “That kind of scares me. That pretty much convinces me to get my blood sugar down all the time” (11-year-old, Type 1 Diabetes).
And then we’re good
Children’s understanding of their condition was evident in their discussion of symptoms and symptom management. The children’s understanding regarding their diagnosis, symptoms, and treatments varied widely. All knew the name of their condition. Though some children had an intimate understanding of the condition and why treatments were given, others didn’t know how they got the condition, what medications they were taking, or what the medications did.
Children talked about doing things to decrease symptoms and manage the condition, as well as plans that were in place should something happen. Children with asthma spoke of stopping to rest and catch their breath and of drinking water, and children with diabetes would check their blood sugar if they were not feeling well and prior to strenuous activities. Many children had cell phones that enabled them to keep in contact with their parents regarding condition updates while they were away from home. Having access to parents seemed to increase the children’s confidence. One girl stated that access to her parents allowed her to handle her glucose levels when away from home and allowed participation in activities with her friends without direct adult supervision. “I have my own emergency cell phone…. I always have it … call [mother’s] cell, I'm like, ‘oh, I'm here,’ or ‘hi, I'm low’ or whatever. Then I'll go to sleep…l keep my phone right beside me… Test, tell [mother] my blood sugar, and then we're good” (11-year-old, Type 1 Diabetes).
It’s pretty easy for us to handle/it’s hard for us cause it’s not normal
The participants in the study spoke of their impression of incorporating management into daily care; what made having the condition easy or hard both within the home and during outside activities. Children identified having the family showing support and understanding, telling how the family let them be in control relative to their treatment regimen when possible, including planning for outings and activities, as things that made having the condition easier. At school, children who described relative ease of management discussed having understanding teachers and nurses, an ability to integrate care into the everyday routine (e.g., keeping an inhaler in their desk, permission to have extra snacks), and a flexible schedule that allowed the student to do what needed to be done and still participate in the important classroom activities. As one child with allergies said, “I don’t have bad allergies…no, just like I’m anaphylactic…so if I touch it, I get a hive. If I eat it, then that’s when I’ll need an Epipen” (8-year-old, Cystic Fibrosis, Allergies).
Alternatively, some children expressed difficulty managing the condition and the way it made them feel different. As another child with cystic fibrosis confided, “I didn’t really want it. It’s not good. I don’t like it and I want to get rid of it” (9-year-old with Cystic Fibrosis). Children reporting more difficulty carrying out management within the home said it was difficult for them to perform the treatment correctly and there was no one to remind them or help them problem solve. These children had trouble remembering treatments and medications. These kinds of incidents threw off the child’s day and made it difficult to get back on track. At school, teachers or staff who didn’t understand their condition and prevented them from getting the treatment they needed made management more difficult. Although this group was a minority, they spoke of the frustration of not being listened to when they believed they needed to do something.
Mom and Dad agree/disagree…
The majority of children believed their parents always agreed on the approach used in condition management. Only one child in the study identified an area where his parents did not agree on a management activity. This disagreement revolved around the child’s ability to give his own insulin injections: “…mom just doesn’t want me to do it, but I don’t know why. She thought that I did it the wrong way … My dad, he does think I can do it, but I think no” (9-year-old, Type 1 Diabetes).
The remainder of the children described agreement between the parents with regard to management and identified either one parent as their primary point person or shared responsibilities between both parents. Most often the mother was identified as the primary person, although the father was readily identified as being the backup. Other children talked about each parent having discrete activities he or she took responsibility for or the child and parent sharing management responsibilities.
Management Behaviors
Management of the condition refers to efforts directed toward caring for the condition and incorporating it into everyday life, both for children and their families. This section does not identify tasks associated with management that would be condition-specific, but rather describes the children’s perspectives on overall condition management activities and how they make sense of them.
They do it for my health and stuff
Children were able to discuss why condition management was important and connected to specific strategies for such management. As might be expected given the developmental stage of the participants, the children had only a very basic understanding of why condition management was important, but generally understood it was to keep them healthy. They talked of activities such as checking in to make sure treatments were done, reminders about schedules, and actively getting treatments and medications ready.
The children also reflected on the ways the family accepted and problem solved the diagnosis and how it helped them frame the condition for themselves. One child talked about how her parents were proactive in learning about the diagnosis and incorporating it as a normal part of their child; “…he [Dad] [looked up Olympians with diabetes] said he looked them up, ‘Just to let you know your dreams will never be crushed because of this.’ That helped” (12-year-old, Type 1 Diabetes). For this child it meant having diabetes didn’t mean she didn’t have to give up other aspirations and goals.
Children often talked about the goals they had playing games or sports, but were less likely to talk about goals in terms of condition management. One child, however, clearly identified his personal goal of remembering to take his pill every morning without being reminded. Children also had treatment preferences based upon their priorities. One child with diabetes talked about changing the type of insulin she was taking so she could have more control and worry less about whether she could eat something. Two children with cystic fibrosis talked about the time it took for treatments and giving priority to a method that did the job but took less time. These children understood the need to keep healthy balanced with their goals and desires in other areas of their lives.
I do it, they do it, and we do it
Children discussed the way routines and related strategies for management of the condition were incorporated into everyday life. Three ways of doing things were apparent from the children’s perspectives. They used “I” statements to explain management activities they did on their own (e.g., I check my blood sugar, I take my treatment, and I do it myself). Children used “they” statements to identify management activities outside of their control. Finally, children used “we” statements, talking about management as a joint venture between them and their parents.
It’s just kind of my schedule
The children also described how they developed their own routines and related strategies for condition management and incorporated them into everyday life. One child with asthma explained her strategy for participating in sports while keeping her asthma under control, assessing how her body felt, and doing things that helped her with endurance and relaxation;
When I run, I only run like two laps. I run out of breath, I walk, then I run again, I run out of breath, then I walk for another couple of laps, then I jog while I breathe really heavy, and after we stretch a little bit and there’s this one stretch called the goalie stretch where you just lay down and you stretch your whole body. That kind of relaxes me (10-year-old, Asthma).
Children in the study often talked about their view of condition management in relation to the school day: what they did before, during, and after school. Furthermore, treatments were tied to school and activity-related events, not clock time (e.g., medications or treatments were done before lunch, during the second recess, or before taking the bus home). This also carried over to after-school activities, where treatments were tied to going to practice, dance or instrument lessons, and bedtime. Children looked at their daily routines as a series of events. Children also spoke of the effort they needed to take care of their condition and how management was incorporated into the school day or disrupted school. For example, they spoke of having to leave class early to go to the nurse’s office for treatments, blood glucose testing, or other medications at prescribed times during the day. Over the weekend or on non-school days, the major differences were stated in terms of the school day.
Children also identified routines or schedules for occasional activities such as vacations or trips, and what had to happen or what planning needed to occur to ensure that the proper medications and technology were taken along. They also spoke of what needed to happen in order to sleep over at a friend’s house or at the grandparents’ home. Some children were also aware of the routines associated with appointments, describing the need to go every three months for an HbA1C check or once a year for pulmonary function tests. One student athlete with both diabetes and asthma reported that he often had to stop before, during, and after practices or games to check his blood glucose level or take inhalation treatments, and also he had to have rescue inhalers on the sideline. Parents were frequently at the games, which provided assurance that medical needs could be handled.
To tell or not to tell
Children spoke of the role that telling others played in the management strategies. Some were very clear that others needed to know in order for them to maintain their health status. This was evident across all conditions when children spoke of participating in activities outside of the home and recognizing the risk of others not knowing in case they needed help. Two children stated that it was a group effort, and one said his friends would actually ask him if he was okay sometimes: “if I’m acting like upset or angry all the time, they’ll just be like ‘Okay, are you alright? Do you need to do your thing or whatever?’ I’m like ‘Yeah, I’ll go test’ and they’re usually right” (11-year-old, Type 1 Diabetes).
Other children were more private, saying no one really needed to know. One girl said people knowing might hurt your chances of getting a job you really need, and another explained a friend had teased her so now she does not tell friends.
Children described the process that occurred within the family in order to manage their condition, and they reported varying personal control. Some of the participants had very little control beyond following the instructions they were given for condition management by the health care provider or the caregiver or passively watching the caregiver, but all were aware of condition management and the approaches and attitudes of the people around them.
If they weren’t hounding me, I wouldn’t be this free
Children described the way their family incorporated condition management into family life and what it meant to them. The children spoke of their view of family life and also of their parents’ and their own satisfaction with the management.
Many children spoke of the family’s focus outside the realm of condition management, citing activities the family did together. Whether playing golf, watching the Three Stooges, or traveling, children recognized when their family was focusing on family life and when they were too focused on their condition. One child suggested that families should have “check-ins” to recap the week in order to identify what worked well and what may need to change. This may be the child’s recognition that occasionally the family focus needs to come back to the condition for a brief period of time in order to evaluate the process.
Two children recognized that the focus was on the condition when parents were doing or assisting with treatments. Complexity was added for the caregivers when they were helping with treatments and siblings were vying for the parents’ attention. Children believed they should be the priority during that time and thought parents should control siblings.
Some children spoke of the attention or focus that was on the condition as a necessary part of family life, and that was accepted. One child recognized the family’s adjustment to her condition as putting more responsibility on everyone, but acknowledged that they were able to take on these additional challenges. Another child explained her perspective when she contrasted her family’s focus to that of another child she knew, explaining her family hounded her about the things she needed to do, but over time it allowed her to be free to do it all herself while her friend had no stability because his parents never helped him out and he was left to figure things out by himself. Other children told about the family diet that had changed for everyone, not just the child with the chronic condition, in conjunction with the diagnosis and diet restrictions.
Consequences
The consequences theme related to how children viewed the future in light of their CHC. This was a difficult area for most children to address in relation to managing their condition. The children did recognize the things they were currently doing were different from what they had done when they were younger, but had limited insight into what might be expected of them in the future. Some identified more typical life changes that they expected to occur, such as going to college, getting married, having a family. A few children were very technology oriented and described changes that might occur if scientific advancement in condition treatment were made.
I might have a totally different life when I’m older
The future was not something many of this group of children spoke of readily within the context of their CHC. Many children spoke of having more responsibilities or being more responsible in the future, although what those responsibilities would be and what being more responsible meant was largely left unsaid. Coupled with the expectation that responsibilities would increase was the implied understanding that parental responsibilities would decrease. As one child stated when reflecting on the future, “…it’s a little bit harder ‘cause you have all the responsibilities., like your parents don’t help you out with everything like when you’re my age” (11 year old, Type 1 Diabetes).
Children spoke vaguely about the implications of their condition for their future and the family’s future. Expectations centered on changes in treatment and changes in expectations for self and the family. Some of the school-aged children in the study had “techie” looks at the future, imagining time machines so they could look ahead and see the future. One child imagined “tech pads” that would test blood sugar and another child seemed to be well versed in potential technological developments that may be on the horizon, talking about the “artificial pancreas” and the FDA approval process.
Children expected change in the future, although they did not explain what form the change would take. Children expressed uncertainty concerning the future in terms of medication and treatment requirements, and they imagined a future in which their parents would not be readily assisting with their care and where they would possibly be living on their own. Several children talked about future changes related to the need to be employed, and two children talked of having their own family one day. “I might have a totally different life when I’m older. Maybe I would get a house, maybe I would get a job, and maybe I would get a life” (8-year-old, Hemophilia) was the poignant comment of one child.
Discussion
The results of this study support the applicability of the FMSF as a framework to explore the perspectives of school-aged children with a variety of CHCs. In telling their stories, the children discussed the meaning the condition had for their life, the management efforts required, and the expected consequences of the condition and management needs. Although not all areas were discussed with the same depth and description, the children provided rich descriptions of the meaning and management components, and showed the beginning development of understanding of the condition consequences and future considerations.
Definition of the Situation, the first dimension of the FMSF, examines the subjective meaning family members attribute to important elements of their situation (Knafl & Deatrick, 2003). From the adult perspective, child identity and view of condition are foundational to family management as parents beliefs about the child’s capabilities are tied closely to their understanding of the condition and the associated demands and limitations (Knafl, et al., 2012). Wollenhaupt (2013), in an analysis of adolescents with spina bifida, also noted the importance of identity for adolescence and the potential for this to influence the relationship between the adolescent and the family. This was similar to our findings with the children in our study, who were comparing themselves to siblings and classmates and talking of ways they were similar or different. Studies examining families of children with CHCs have found that the connections between families and children can have great impact with positive family relationships leading to better health outcomes (Cohen, Lumley, Naar-King, Partridge, & Cakan, 2004; DeLambo, Ievers-Landis, Drotar, & Quittner, 2004; Fiese, Wamboldt, & Anbar, 2005) and negative family relationships leading to declines in children’s health (Fiese & Everhart, 2006; Lewin et al., 2006). Children are making connections between perceptions of how their family makes meaning from the condition and how they understand their condition. Additional research is needed to understand the relationship between family management, child identity and these important health outcomes.
Management Behaviors represents the efforts directed toward caring for the condition and adapting family life to condition related demands and incorporates family beliefs about the condition in addition to the goals, priorities and values the guide the approach to management (Knafl, et al., 2012). Of special interest, the development of routines for managing the condition is an important aspect of condition management that helps families (Case-Smith, 2004). Bedell et al. (2005) and Cashin et al. (2008) also highlight the importance of having the whole family involved in these routines, and having routines both at home and for condition-related responsibilities to be done outside of the home. Family rituals, whether infrequent (e.g., birthday celebrations, holidays) or daily (mealtime, games, or reading), promote a positive family environment and health-related quality of life (Santos, Crespo, Silva, & Canavarro, 2012). Families and children with CHCs, recognizing the importance of rituals and routines as a way to integrate illness care into family life and to decrease emphasis on the illness itself, can positively influence both family and child outcomes (Knafl, et al., 2013). For instance, children with CHC in this study viewed their condition management around their daily activities, including before and after school. Therefore, communicating about condition management within the context of family routines may enable parents and children to problem solve their responsibilities and fulfill their roles.
Perceived Consequences examines the balance between condition management and other aspects of family life and the implications for the child and family’s future (Knafl, et al., 2012). When children talked about the condition itself, it was not usually oriented toward the future; rather, it was about changes over time since they had first been diagnosed or from when they were younger. Some spoke about the condition being easier to handle because they were older and understood more about the condition, whereas others spoke about how the condition may have gotten better or worse over time. Consistent with other studies in which older children demonstrated stronger language skills and higher levels of cognitive functioning (Coyle, Russel, Shields, & Tanaka, 2007), the younger group tended to be more concrete and had relatively less insight into several of the dimensions. Although these findings are typical within the developmental expectations, of importance is the degree of insight and perspective of the older group. These findings show the developmental progression and changes in cognitive understanding.
The findings also support the expectation that condition management is a two way street, with both the child and the family having perspectives and influencing the process. Knowing that family management is a phenomenon that resonates with families and also with children with CHC provides the foundation for exploration of this unique perspective and its relationship to both family and child outcomes. There are certainly other variables, including those in the contextual influences of the FMSF that are both environmental (i.e., family situations, social determinants of health) and child-specific (development, health condition) that place in context and influence these dimensions. Findings from this study about intra-family processes, however, are important for practitioners, researchers, and families to consider as we work to prepare children with chronic health conditions to become adolescents assuming more of their health care management on a daily basis.
Implications for Practice
In a report published by the World Health Organization, Michaud, Suris, and Viner (2007) acknowledged, “In clinical interactions with younger children, management decisions are made ‘adult to adult’ by health professionals in consultation with parents, and day-to-day disease management is generally undertaken directly by parents.” (p. 8). The findings here support the need for health care professionals to include children at a much younger age, realizing that children with CHC are listening and forming perspective regardless of their intentional inclusion or exclusion. The American Academy of Pediatrics supports that approach, recommending children be included in visits as early as age four in order to become comfortable speaking with the health care provider. The Academy also recognizes that some children as young as 9 or 10 may have concerns or questions about their health that they want to discuss with the provider alone, although others this age may not be ready for this (Hagan, Shaw, & Duncan, 2008). Including the school-aged child in discussions can help the child better understand and plan condition management when away from the parents and help the family create ways to support the child in this developmental endeavor (Kirk, Beatty, Callery, Milnes, & Pryjmachuk, 2012). One can imagine that a plan to develop the necessary toolbox with the child and family will help support and ease transitions from family-focused management to self-care in the adolescent and young adult.
Concern is high regarding the transition of pediatric patients to adult care (Schwartz et al., 2013); the goal is to have the transfer done in a timely and safe manner. This is especially true of specialty pediatric practices that see children and families with particular chronic health conditions. The evidence in this study focuses on the issues that concerned school-aged children, especially their self-identity, view of the condition, and management approach. Issues were not often mentioned about future responsibilities and expectations, ways to resolve conflict concerning condition management, and decision-making within the health care context. Efforts need to be placed on building upon a developmentally appropriate awareness of future management goals to accomplish preparation for transition. For instance, children were able to accomplish the tasks of care, but were not aware of anticipated changes that may occur with puberty, as they enter middle school, or as a general course of the condition. Helping to prepare children for anticipated changes and providing skills can help children manage these changes.
Though school-aged children with CHC are not ready to be the primary decision maker, they are aware of many limitations, implications, and useful strategies for management relative to their condition. If they are not included in goal setting, creating strategies to meet the goals, and evaluating the outcomes reflectively, they may not develop the appropriate skills for decision making as they enter adolescence and young adulthood. Health care providers usually have years, starting at diagnosis, to help children with CHCs and their families focus on issues key to condition management and prepare for the transition to adult care. It would be beneficial to develop the mindset that this preparation should include the child from the diagnosis forward.
Limitations
There are some limitations to this study that must be acknowledged. Although there was considerable diversity in this sample of school-aged children, the participants all were treated at the same large children’s hospital, which may have led to some homogeneity in the treatment experience, especially within clinics. Additionally, these children were typical for age related to cognitive development, and children with cognitive impairments might have presented differently. Although the characteristics of the various conditions were diverse, the conditions were predominantly physical. Considering that some of the most prevalent CHCs among children are asthma, obesity, and mental health conditions including ADHD (Perrin, Gnanasekaran, & Delahaye, 2012), only asthma was a primary diagnosis in this sample and ADHD was a co-morbidity in four children. The diversity across race was also limited and future studies should include participants with broader cultural experiences. The small sample size did not allow for comparison within and among subgroups marked by age, race, socio-economic status, or other important variables. (Table 1)
Future Research
The current study shows that the FMSF can be used to investigate the perspectives of children with CHCs. Recently, four different patterns of family management have been identified; family-focused, somewhat family-focused, somewhat condition-focused, and condition-focused (Knafl, et al., 2013). A mixed methods analysis of the qualitative child data and quantitative data from one of their parents is currently in progress. This analysis is exploring the similarities and differences between the parent and child perspectives of family management based upon the management pattern.
Future research to address the limitations of the current study is needed. The current study sample was limited with respect to conditions represented and lacked cultural diversity. As qualitative studies are often limited to a small number of participants, the next step needs to be quantitative. Development of a family management measure for children/adolescence would require a larger sample and an opportunity to obtain a more diverse sample. With the development of a child measure to complement the Family Management Measure (FaMM) we would have the ability to identify the strengths families and children have to build on and weaknesses for which interventions might help to improve outcomes.
This study fills gaps in our science about school-aged children and their understanding of their CHC, how they and their families incorporate CHC into their daily lives, and family management. The perspectives of children not only adds important contextual understandings for the FMSF, but also helps us better comprehend the family unit. In addition, the design of this study systematically considers selection of a sample based on the characteristics of the children’s conditions and not on their medical diagnoses. These data, therefore, have the potential to be used to formulate a measure that fulfills a mandate set by the United States National Guideline Clearinghouse; that is, that we design measures and metrics that are sensitive to health phenomenon across populations and that can be used to stratify subgroups in order to examine whether disparities in health exist among a diverse population of patients (National, 2014). As populations of children with CHC survive with more and more intense and complex CHC, pediatric nurses are called upon to use robust frameworks to identify those issues that not only have significance within specific settings but have the potential to be tested globally within and across potentially vulnerable and at risk children and families.
Highlights.
Children may better understand condition management within the context of routines
Children develop perspectives about their condition and its management
Children’s reports are consistent with The Family Management Framework
Children may not have insight about long-term implications of their condition
Acknowledgement
The authors acknowledge and thank Phyllis A. Dexter for her editorial assistance with this paper.
Funding – The first author received financial support from the National Institute of Nursing Research, National Institutes of Health (T32NR007066; T32NR007100; F31NR011524; R01NR011589) and Sigma Theta Tau, Xi Chapter.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest – The authors have no conflicts of interest to declare.
Contributor Information
Barbara L. Beacham, Email: bbeacham@iu.edu.
Janet A. Deatrick, Email: deatrick@nursing.upenn.edu.
References
- Bedell GM, Cohn ES, Dumas HM. Exploring parents' use of strategies to promote social participation of school-age children with acquired brain injuries. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.] The American journal of occupational therapy : official publication of the American Occupational Therapy Association. 2005;59(3):273–284. doi: 10.5014/ajot.59.3.273. [DOI] [PubMed] [Google Scholar]
- Blumer H. Symbolic interactionism; perspective and method. Englewood Cliffs, N.J.: Prentice-Hall; 1969. [Google Scholar]
- Case-Smith J. Parenting a child with a chronic medical condition. [Research Support, U.S. Gov't, P.H.S.] The American journal of occupational therapy : official publication of the American Occupational Therapy Association. 2004;58(5):551–560. doi: 10.5014/ajot.58.5.551. [DOI] [PubMed] [Google Scholar]
- Cashin GH, Small SP, Solberg SM. The Lived Experience of Fathers Who Have Children With Asthma: A Phenomenological Study. Journal of pediatric nursing. 2008;23(5):372–385. doi: 10.1016/j.pedn.2007.08.001. doi: http://dx.doi.org/10.1016/j.pedn.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Cohen DM, Lumley MA, Naar-King S, Partridge T, Cakan N. Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with type 1 diabetes: a prospective study. Journal of pediatric psychology. 2004;29(3):171–184. doi: 10.1093/jpepsy/jsh019. [DOI] [PubMed] [Google Scholar]
- Coll CG, Szalacha LA. The multiple contexts of middle childhood. Future of Children. 2004;14(2):81–97. [Google Scholar]
- Coyle KK, Russel LA, Shields JP, Tanaka BA. Summary Report: Collecting data from children ages 9–13: Lucile Packard Foundation for Children's Health. 2007 [Google Scholar]
- Crisp J, Ungerer JA, Goodnow JJ. The impact of experience on children's understanding of illness. Journal of Pediatric Psychology. 1996;21(1):57–72. doi: 10.1093/jpepsy/21.1.57. [DOI] [PubMed] [Google Scholar]
- DeLambo KE, Ievers-Landis CE, Drotar D, Quittner AL. Association of observed family relationship quality and problem-solving skills with treatment adherence in older children and adolescents with cystic fibrosis. [Research Support, U.S. Gov't, P.H.S.] Journal of pediatric psychology. 2004;29(5):343–353. doi: 10.1093/jpepsy/jsh038. [DOI] [PubMed] [Google Scholar]
- Elo S, Kyngas H. The qualitative content analysis process. Journal of Advanced Nursing. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Emiliani F, Bertocchi S, Poti S, Palareti L. Process of Normalization in Families With Children Affected by Hemophilia. Qualitative Health Research. 2011;21(12):1667–1678. doi: 10.1177/1049732311417456. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Everhart RS. Medical adherence and childhood chronic illness: family daily management skills and emotional climate as emerging contributors. [Research Support, N.I.H., Extramural Review] Current Opinion in Pediatrics. 2006;18(5):551–557. doi: 10.1097/01.mop.0000245357.68207.9b. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Wamboldt FS, Anbar RD. Family asthma management routines: connections to medical adherence and quality of life. [Research Support, Non-U.S. Gov' Research Support, U.S. Gov't, P.H.S.] The Journal of pediatrics. 2005;146(2):171–176. doi: 10.1016/j.jpeds.2004.08.083. [DOI] [PubMed] [Google Scholar]
- Hagan JF, Shaw JS, Duncan PM. Bright futures : guidelines for health supervision of infants, children, and adolescents. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Kirk S, Beatty S, Callery P, Milnes L, Pryjmachuk S. Perceptions of effective self-care support for children and young people with long-term conditions. Journal of Clinical Nursing. 2012;21(13–14):1974–1987. doi: 10.1111/j.1365-2702.2011.04027.x. [DOI] [PubMed] [Google Scholar]
- Knafl KA, Deatrick JA. Further refinement of the family management style framework. Journal of family nursing. 2003;9(3):232–256. [Google Scholar]
- Knafl KA, Deatrick JA, Havill NL. Continued development of the family management style framework. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Review] Journal of family nursing. 2012;18(1):11–34. doi: 10.1177/1074840711427294. [DOI] [PubMed] [Google Scholar]
- Knafl KA, Deatrick JA, Knafl GJ, Gallo AM, Grey M, Dixon J. Patterns of family management of childhood chronic conditions and their relationship to child and family functioning. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] Journal of pediatric nursing. 2013;28(6):523–535. doi: 10.1016/j.pedn.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin AB, Heidgerken AD, Geffken GR, Williams LB, Storch EA, Gelfand KM, Silverstein JH. The relation between family factors and metabolic control: the role of diabetes adherence. Journal of pediatric psychology. 2006;31(2):174–183. doi: 10.1093/jpepsy/jsj004. [DOI] [PubMed] [Google Scholar]
- McMenamy JM, Perrin EC. The impact of experience on children's understanding of ADHD. Journal of Developmental and Behavioral Pediatrics. 2008;29(6):483–492. doi: 10.1097/DBP.0b013e318190317c. [DOI] [PubMed] [Google Scholar]
- Michaud P-A, Suris JC, Viner R. WHO Discussion Papers on Adolescence. World Health Organization; 2007. The adolescent with a chronic condition: Epidemiology, developmental issues and health care provision. [Google Scholar]
- National Quality Measure Clearinghouse. Desirable attributes of a quality measure. 2014 May 29; Retrieved October 1, 2014, from http://www.qualitymeasures.ahrq.gov/tutorial/attributes.aspx.
- O'Connor MK, Netting FE, Thomas ML. Grounded theory - Managing the challenge for those facing Institutional Review Board oversight. Qualitative Inquiry. 2008;14(1):28–45. [Google Scholar]
- Patton MQ. Qualitative research and evaluation methods. 3rd ed. Thousand Oaks, CA: Sage Publications, Inc; 2002. [Google Scholar]
- Perrin JM, Gnanasekaran S, Delahaye J. Psychological aspects of chronic health conditions. Pediatrics in Review. 2012;33(3):99–109. doi: 10.1542/pir.33-3-99. [DOI] [PubMed] [Google Scholar]
- Rolland JS. Families, illness, & disability: An integrative treatment model. New York: Basic Books; 1994. [Google Scholar]
- Santos S, Crespo C, Silva N, Canavarro MC. Quality of Life and Adjustment in Youths with Asthma: The Contributions of Family Rituals and the Family Environment. Family Process. 2012;51(4):557–569. doi: 10.1111/j.1545-5300.2012.01416.x. [DOI] [PubMed] [Google Scholar]
- Schwartz LA, Brumley LD, Tuchman LK, Barakat LP, Hobbie WL, Ginsberg JP, Deatrick JA. Stakeholder validation of a model of readiness for transition to adult care. [Research Support, N.I.H., Extramural Validation Studies] JAMA pediatrics. 2013;167(10):939–946. doi: 10.1001/jamapediatrics.2013.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vygotsky LS. Imagination and Creativity in Childhood. [Article]. [Voobrazhenie i tvorchestvo v detskom vozraste, [1967] Journal of Russian & East European Psychology. 2004;42(1):7–97. [Google Scholar]
- Wollenhaupt J, Rodgers B, Sawin KJ. Family management of a chronic health condition: perspectives of adolescents. Journal of family nursing. 2012;18(1):65–90. doi: 10.1177/1074840711427545. [DOI] [PubMed] [Google Scholar]