Abstract
Tigecycline (TIG) is approved for use for the treatment of complicated intra-abdominal infections, skin and skin structure infections, as well as pneumonia. Acquired resistance or reduced susceptibility to TIG has been observed in Gram-negative rods, has seldom been reported in Gram-positive organisms, and has not yet been reported in Enterococcus faecium. Using the serial passage method, in vitro mutant AusTig and in vitro mutants HMtig1 and HMtig2 with decreased TIG susceptibility (MICs, 0.25 μg/ml) were obtained from strains E. faecium Aus0004 and HM1070 (MICs, 0.03 μg/ml), respectively. In addition, two vancomycin-resistant E. faecium clinical isolates (EF16 and EF22) with reduced susceptibility to TIG (MICs, 0.5 and 0.25 μg/ml, respectively) were studied. Compared to the wild-type strains, the in vitro mutants also showed an increase in the MICs of other tetracyclines. An efflux mechanism did not seem to be involved in the reduced TIG susceptibility, since the presence of efflux pump inhibitors (reserpine or pantoprazole) did not affect the MICs of TIG. Whole-genome sequencing of AusTig was carried out, and genomic comparison with the Aus0004 genome was performed. Four modifications leading to an amino acid substitution were found. These mutations affected the rpsJ gene (efau004_00094, coding for the S10 protein of the 30S ribosomal subunit), efau004_01228 (encoding a cation transporter), efau004_01636 (coding for a hypothetical protein), and efau004_02455 (encoding the l-lactate oxidase). The four other strains exhibiting reduced TIG susceptibility were screened for the candidate mutations. This analysis revealed that three of them showed an amino acid substitution in the same region of the RpsJ protein. In this study, we characterized for the first time genetic determinants linked to reduced TIG susceptibility in enterococci.
INTRODUCTION
Enterococcus faecium is a Gram-positive bacterium and is part of the human intestinal microbiota. Beside Staphylococcus aureus and Enterococcus faecalis, Enterococcus faecium is among the leading causes of hospital-acquired infections (1). Usually considered a microorganism with a limited clinical relevance, E. faecium has become a major opportunistic pathogen responsible for numerous infections, such as bacteremia, endocarditis, and urinary tract and intra-abdominal infections. This increased prevalence mainly results from the worldwide spread of hospital-adapted strains belonging to clonal complex 17 (CC17) (2). Because of its high genome plasticity, E. faecium may acquire numerous determinants of antimicrobial resistance, and most CC17 isolates are highly resistant to ampicillin and fluoroquinolones, while a significant proportion of them are resistant to glycopeptides (the so-called vancomycin-resistant enterococci [VRE]) (3). Thus, only a few alternative options (i.e., linezolid, daptomycin, or tigecycline [TIG]) remain available for the treatment of infections caused by these resistant microorganisms. Even if resistance to these compounds is still uncommon, some E. faecium clinical isolates with reduced susceptibility or resistance to antibiotics (but not to TIG) have already been reported (3), and a better understanding of the resistance mechanisms is needed for limiting their dissemination.
TIG is the only representative of the glycylcyclines, a new group of tetracyclines (4). This compound is actually the 9-tert-butylglycylamido derivative of minocycline (5). It exhibits bacteriostatic activity against a large panel of Gram-positive and Gram-negative bacteria, except Pseudomonas aeruginosa and Proteus mirabilis (4). Like classical tetracyclines, TIG inhibits bacterial protein synthesis by interacting reversibly with the 30S ribosomal subunit. This prevents the binding of the tRNA acceptor site on the ribosome and thus blocks the elongation step (4). Interestingly, TIG interacts with the ribosomal target with a 5-fold higher affinity, overcoming the main mechanisms of resistance to classical tetracyclines (i.e., ribosomal protection and active efflux) (6). In Escherichia coli, decreased susceptibility to TIG is due to MarA-mediated overexpression of the AcrAB-TolC efflux pump system (7). Similarly, TIG resistance in members of the Enterobacteriaceae other than E. coli and Acinetobacter baumannii also results from increased expression of operons encoding resistance-nodulation-cell division (RND) efflux pumps (8, 9). In Gram-positive organisms, previous experiments have shown that in vitro TIG resistance in S. aureus could be obtained by serial passage in increasing antibiotic concentrations (up to an MIC of 16 μg/ml). This resistance is also correlated with overexpression of an efflux pump gene, mepA, coding for a transporter belonging to the multidrug and toxin extrusion (MATE) family (10). In enterococci, clinical isolates with reduced TIG susceptibility (MIC > 0.25 μg/ml) seem to be exceptionally selected in vivo, and only a few strains have been reported so far (11, 12). However, the genetic basis of resistance has not yet been evidenced, while no resistant strains (selected in vitro or in vivo) have been described in E. faecium.
The aim of this study was to identify potential genes associated with reduced TIG susceptibility in E. faecium. Comparative genome analysis of one mutant obtained in vitro and its parental strain allowed detection of a mutation within the rpsJ gene, coding for the ribosomal S10 protein. The role of RpsJ changes in reduced TIG susceptibility was confirmed by demonstrating the absence of efflux and by using additional in vitro mutants and clinical isolates.
(A preliminary report of this work was presented at the 54th Interscience Conference on Antimicrobial Agents and Chemotherapy, Washington, DC, USA, 2014 [13].)
MATERIALS AND METHODS
Bacterial isolates and growth conditions.
The bacterial strains used in this study are listed in Table 1. In vitro mutants with decreased TIG susceptibility were obtained from strains E. faecium Aus0004 (14) and HM1070 (15) after serial passage on Mueller-Hinton (MH) medium containing increased concentrations of TIG (from 0.03 to 0.25 μg/ml). Briefly, three petri dishes of MH medium with 2-fold-increasing concentrations of TIG were inoculated with approximately 5 × 105 CFU of the E. faecium strains. After overnight incubation at 37°C, bacterial cells grown in the presence of the highest drug concentration were used to prepare the inoculum for a series of three MH medium plates containing 2-fold-increasing concentrations of TIG. This process was repeated for 25 days (ca. 700 generations), and the MICs of TIG were checked at each round. HMtig1 and HMtig2 were obtained by two experiments performed in parallel and therefore correspond to technical replicates. To test the stability of the reduced susceptibility to TIG, mutants were grown for 15 days (ca. 400 generations) on brain heart infusion (BHI) medium in the absence of any selective pressure.
TABLE 1.
Bacterial strains and plasmids used in the study
| Strain or plasmid | Relevant properties | Reference or source |
|---|---|---|
| Strains | ||
| E. faecium | ||
| Aus0004 | Reference strain | 14 |
| HM1070 | Reference strain | 15 |
| AusTig | In vitro mutant from Aus0004 with reduced susceptibility to TIG | This study |
| HMtig1 | In vitro mutant from HM1070 with reduced susceptibility to TIG | This study |
| HMtig2 | In vitro mutant from HM1070 with reduced susceptibility to TIG | This study |
| EF16 | Clinical isolate with reduced susceptibility to TIG | This study |
| EF22 | Clinical isolate with reduced susceptibility to TIG | This study |
| AusΔ1228 | Knockout mutant for efau004_1228 from Aus0004 | This study |
| E. coli EC1000 | E. coli cloning host | 16 |
| Plasmids | ||
| pWS3 | 20 | |
| pWS3-rpsJ | ΔrpsJ allele cloned into pWS3 | This study |
| pWS3-1228 | Δefau004_1228 allele cloned into pWS3 | This study |
Two vancomycin-resistant clinical isolates of E. faecium (EF16 and EF22) with reduced susceptibility to TIG were obtained from the collection of the National Reference Center for enterococci (CHU, Caen, France). EF16 was obtained in 2010 from a patient hospitalized in the north of France, while EF22 was isolated in 2013 from a patient hospitalized in the French southeast region. Both were isolated from rectal swabs.
E. faecium bacterial cells were routinely incubated in BHI broth at 37°C without agitation, whereas the E. coli EC1000 strain (16) was cultured under vigorous shaking (250 rpm) at 37°C in Luria-Bertani (LB) medium.
Antimicrobial susceptibility testing.
The MICs of TIG, tetracycline, minocycline, doxycycline, quinupristin-dalfopristin, vancomycin, teicoplanin, chloramphenicol, ampicillin, linezolid, ciprofloxacin, and gentamicin were determined by the broth microdilution method according to Clinical and Laboratory Standards Institute (CLSI) guidelines (17). The dilution series of antibiotics were from 32 to 0.003 μg/ml for all antibiotics except ampicillin and gentamicin, for which concentrations from 1,024 to 1 μg/ml were used. The MH medium used (BD, Spark, MD, USA) is adjusted to provide 20 to 25 mg per liter of calcium and 10 to 12.5 mg per liter of magnesium, and TIG was prepared extemporaneously. The MICs of TIG were also evaluated using Etest strips (bioMérieux, Marcy l'Etoile, France). The agar dilution method was used to determine the MICs of TIG in the presence of the efflux pump inhibitor (EPI) reserpine (10 or 50 μg/ml), a very well-known EPI in Gram-positive bacteria (18), or the proton pump inhibitor pantoprazole (10 μg/ml). From 1 to 0.01 μg/ml of TIG was added to MH agar plates, and a spot of 10 μl of the cell suspensions (0.5 McFarland standards) was inoculated onto the surface. Plates containing 500 μl dimethyl sulfoxide (which was used to dissolve reserpine) were used as controls. Incubations were performed at 37°C for 18 h.
Whole-genome sequencing and comparative genomic analysis.
The complete genome sequence of the AusTig mutant was obtained by high-throughput sequencing, using an Illumina MiSeq benchtop sequencer (ProfileXpert-LCMT, Lyon, France), from libraries constructed from genomic DNA purified with a NucleoSpin tissue kit (Macherey-Nagel, Düren, Germany). Thus, about 5 million reads (each of which was 61 bp long), corresponding to a 100-fold coverage of the E. faecium Aus0004 genome, were obtained. To identify single nucleotide polymorphisms (SNPs), comparative genomic analysis was performed, using CLC Genomics WorkBench software (Qiagen, Valencia, CA), by comparison of the sequences with the annotated sequence of the E. faecium Aus0004 wild-type strain (GenBank accession no. NC_017022) (14). The nucleotide and deduced amino acid sequences were analyzed using the BLASTN and BLASTX programs, available over the Internet at the National Center for Biotechnology Information website (http://blast.ncbi.nlm.nih.gov/Blast.cgi).
General DNA manipulations.
The primers used for this work are listed in Table 2. PCR products and plasmids were purified using a QIAquick PCR purification kit (Qiagen) and a NucleoSpin plasmid kit (Macherey-Nagel), respectively. Restriction endonucleases and T4 DNA ligase were purchased from Promega (Madison, WI, USA) and used according to the manufacturer's instructions. For the detection of the different tet genes (M, K, L, O, S, T, U, and X), genomic DNA was extracted with an InstaGene kit (Bio-Rad, Hercules, CA) and PCR was performed using GoTaq DNA polymerase (Promega), as recommended by the supplier. PCR products were sequenced in both directions (GATC Biotech, Constance, Germany).
TABLE 2.
Primers used in this study
| Primer name | Sequence (5′–3′)a |
Function | |
|---|---|---|---|
| Forward | Reverse | ||
| 1228_Seq | TGAGGAAGGTGTGGATCTGA | GCAATGGGTTGAAGGGATAA | Sequencing |
| RpsJ_Seq | AGAGGTTGCGACACGCCCGG | TCTACAACAGTTACTGGAAT | Sequencing |
| 1636_Seq | GTGGAACATAGCGAAAGTATT | TCATGCGGTGGCGCACCTCC | Sequencing |
| 2455_Seq | GATGAAAGAAGGATCTACTATG | ACTGACAGCTTCCAAGGAGC | Sequencing |
| RpsJ_U | AAAGGATCCTACGCTGAAGCTGGAGACAACATTGG | AATGGTACCGTTTTGCCATCTTGTTCCCTCCTTC | Cloning in pWS3 |
| RpsJ_D | TAAGGTACCAACTAAAACAAAAATAATGGAGGTG | AAAACTAGTACGATTGCATCGTAAACAACACTTTC | Cloning in pWS3 |
| 1228_U | CCGGGGATCCGAATTCAAAATCATGGATTACATTTTCTC | TCGTCGTTACTGCTACAGACAAATCCCAATACCAA | Cloning in pWS3 |
| 1228_D | TAGCAGTAACGACGATCGT | GCAGGTCGACGAATTCAAATCTGCTTGTCTTCTGCA | Cloning in pWS3 |
| pWS3 | TTTCCCAGTCACGACGTTGT | ACTGACAGCTTCCAAGGAGC | Cloning verification |
| Tet(S) | GACTGTGAATCTAAATTTGAAACC | GCACAATTTCGTGAGTTACTGT | PCR detection |
| Tet(T) | TAGCACATGTTGATGCAGGT | TATCATCCCTTACATTTGTC | PCR detection |
| Tet(U) | CAAAAGAAATCGATACGTGG | CGTCTGCAGATTCCTTAAAAGTC | PCR detection |
| Tet(L) | CATTTGGTCTTATTGGATCG | ATTACACTTCCGATTTCGG | PCR detection |
| Tet(M) | ACAGAAAGCTTATTATATAAC | TGGCGTGTCTATGATGTTCAC | PCR detection |
| Tet(K) | TATTTTGGCTTTGTATTCTTTCAT | GCTATACCTGTTCCCTCTGATAA | PCR detection |
| Tet(O) | GATGGCATACAGGCACAGAC | CAATATCACCAGAGCAGGCT | PCR detection |
| Tet(X) | CAATAATTGGTGGTGGACCC | TTCTTACCTTGGACATCCCG | PCR detection |
The underlined sequences correspond to restriction enzyme recognition sites (BamHI, GGATCC; KpnI, GGTACC; EcoRI, GAATTC).
Construction of deletion mutants.
For the construction of the Δefau004_01228 strain and in an attempt to delete the efau004_00094 gene, allelic replacements were carried out as previously described (19). Briefly, DNA fragments (obtained by PCR with the chromosomal DNA of E. faecium Aus0004 as the template) containing ligated upstream and downstream sequences of the desired deletion fragment were cloned into the thermosensitive replication plasmid pWS3 (20) (Table 1), and 1 μg of recombinant plasmid was used to transform E. faecium Aus0004 competent cells by electroporation. Single-crossover transformants (spectinomycin-resistant colonies) were used for temperature shifts in order to release the plasmid. Candidate clones resulting from a double-crossover event were isolated on BHI agar with or without spectinomycin (300 μg/ml). In antibiotic-susceptible clones, the loss of the plasmid and the deletion were verified by PCR and sequencing.
RESULTS
Antibiotic susceptibility profiles.
Three mutants, mutant AusTig and mutants HMtig1 and HMtig2, with reduced TIG susceptibility were obtained in vitro from the Aus0004 and HM1070 E. faecium wild-type strains, respectively. The MICs of TIG against derivative mutants (0.25 μg/ml) were 8-fold higher than those against the corresponding parental strains (0.03 μg/ml) (Table 3). Interestingly, the diminished susceptibility appeared to be stable since the MICs of TIG remained at 0.25 μg/ml for the three mutants over 2 weeks without selective pressure. The derivative mutants also appeared to be significantly less susceptible to the classical tetracyclines than wild-type strains Aus0004 and HM1070, with 4- to 8-fold increases in the MICs of doxycycline, minocycline, and tetracycline being detected (Table 3). No changes in the MICs for any other antimicrobial agents tested, including gentamicin, which also targets the 30S subunit of the ribosome, were observed (Table 3). Finally, no decrease of TIG MICs was observed in the presence of an EPI (reserpine or pantoprazole), whatever the strain tested (data not shown), suggesting that the MIC increase was probably not associated with an efflux mechanism. Of note, the growth kinetic rates of the in vitro mutants were similar to those of the corresponding parental strains under standard growth conditions in BHI medium at 37°C (data not shown).
TABLE 3.
MICs of antimicrobial agents against E. faecium strains
| Antibiotica | MICb (μg/ml) |
||||||
|---|---|---|---|---|---|---|---|
| Aus0004 vanB tet(M)c | AusTig vanB tet(M) | HM1070 | HMtig1 | HMtig2 | EF16 vanA tet(M) | EF22 vanA tet(M) tet(L) | |
| CHL | 16c | 16 | 4 | 2 | 2 | 16 | 16 |
| VAN | 16 | 16 | 0.5 | 0.5 | 1 | >32 | >32 |
| TEC | 2 | 2 | 0.5 | 1 | 1 | >32 | >32 |
| LZD | 4 | 4 | 2 | 4 | 4 | 4 | 4 |
| Q-D | 1 | 1 | 0.25 | 0.5 | 0.5 | 2 | 1 |
| AMP | 256 | 256 | <1 | <1 | <1 | 1,024 | 1,024 |
| CIP | 2 | 4 | 2 | 2 | 2 | >32 | >32 |
| GEN | 8 | 8 | 2 | 2 | 2 | 512 | 4 |
| TET | 0.25 | 1d | 0.25 | 1 | 2 | >32 | 16 |
| DOX | 0.25 | 1 | 0.25 | 1 | 2 | 8 | 4 |
| MIN | 0.06 | 0.25 | 0.12 | 0.5 | 0.5 | 32 | 0.5 |
| TIGc | 0.03 | 0.25 | 0.03 | 0.25 | 0.25 | 0.5 | 0.25 |
CHL, chloramphenicol; VAN, vancomycin; TEC, teicoplanin; LZD, linezolid; Q-D, quinupristin-dalfopristin; AMP, ampicillin; CIP, ciprofloxacin; GEN, gentamicin; TET, tetracycline; DOX, doxycycline; MIN, minocycline; TIG, tigecycline.
MICs were determined both by microdilution and by Etest (similar results). Values underlined and in boldface are at least 4-fold higher than those for the corresponding parental strain.
The tet genes were detected by PCR (see Materials and Methods).
In addition, two vanA-positive VRE clinical isolates (EF16 and EF22) were found to have reduced susceptibility to TIG (MICs, 0.5 μg/ml and 0.25 μg/ml, respectively) and were resistant to the majority of antibiotics tested (Table 3). Note that EF16 is the first E. faecium clinical isolate not susceptible to TIG (EUCAST susceptibility breakpoint, ≤0.25 μg/ml [http://www.eucast.org/clinical_breakpoints/]).
Detection of tet genes.
Tetracycline resistance is usually caused by the acquisition of resistance determinants encoded by the tet genes, which mediate either active efflux or ribosomal protection (21). Among them, seven genes have been retrieved in enterococci so far: tet(K) and tet(L), which are involved in efflux, and tet(M), tet(O), tet(S), tet(T), and tet(U), which encode ribosomal protection proteins (22). We also tested for the presence of the tet(X) gene, which encodes an oxygen-dependent monooxygenase conferring tetracycline resistance in Bacteroides fragilis, as previously described (11). By PCR, the presence of the tet(M) gene was found in the genome of Aus0004 (and its corresponding mutant, AusTig) and EF16, whereas both tet(L) and tet(M) were detected in that of EF22 (Table 3). Surprisingly, despite the presence of these two tet genes, the MIC of minocycline against EF22 appeared to be low (0.5 μg/ml), while the MICs of other tetracyclines were lower than the MIC for strain EF16, which harbors only tet(M) (Table 3). Of note, Aus0004 and its derived mutant, AusTig, remained susceptible to tetracyclines, despite the presence of tet(M). This could be due to the insertion of a group of three genes (efau004_00064, efau004_00065, and efau004_00066) that likely inactivate the locus (14).
Genomic analysis of reduced TIG susceptibility.
By comparative genomic analysis of the sequence of mutant AusTig with that of the parental strain (Aus0004), four different nucleotide substitutions were identified and verified by resequencing (Table 4). The mutation localized at position 97,523 affected the rpsJ gene (efau004_00094), coding for the S10 protein of the 30S ribosomal subunit, by creating an Asp60Tyr substitution. The second mutation was observed in the efau004_01228 gene, leading to an Asn80Ile substitution in the amino acid sequence of the protein annotated as a cation transporter (an E1-E2 family ATPase). Because efau004_01228 encodes an ATP-driven pump involved in the transmembrane transport of charged substrates, it was tempting to speculate that it could play a role in the efflux of TIG (even if the findings of phenotypic tests with reserpine or pantoprazole went against this speculation). We then constructed the corresponding deletion mutant and tested its susceptibility to TIG, but no difference in the MIC compared to that of the parental strain was observed. Our genomic analysis also revealed a Val54Leu substitution in the hypothetical protein EFAU004_01636 without putative conserved domains as well as an Ala100Thr substitution in the sequence of the l-lactate oxidase (EFAU004_02455), which is an enzyme that participates in pyruvate metabolism in the presence of oxygen.
TABLE 4.
Sequence changes in the AusTig mutant compared to the sequence of wild-type strain E. faecium Aus0004a
| Gene | Product | Nucleotide change (position) | Predicted amino acid change |
|---|---|---|---|
| efau004_00094 | S10 protein of the 30S ribosomal subunit | G → T (97,523) | Asp60 → Tyr |
| efau004_01228 | Cation transporter | T → A (1,257,670) | Asn80 → Ile |
| efau004_01636 | Hypothetical protein | G → T (1,651,985) | Val54 → Leu |
| efau004_02455 | l-Lactate oxidase | G → A (2,474,071) | Ala100 → Thr |
In order to determine the role of one or more of these mutations, additional E. faecium strains (in vitro mutants HMtig1 and HMtig2 from HM1070, clinical isolates EF16 and EF22) were tested by PCR amplification and sequencing. It appeared that efau004_01636 was present only in strain Aus0004 (and in its derivative, AusTig). Indeed, no PCR amplification of this gene was detected for the other E. faecium strains tested, suggesting that it is likely part of the accessory genome. Note that a BLAST search did not find efau004_01636 in any enterococcal genome except that of Aus0004 strain. For all the additional strains tested, the amino acid sequences of the proteins encoded by efau004_01228 (cation transporter) or efau004_02425 (l-lactate oxidase) were identical to those of the proteins from the Aus0004 wild-type strain. On the other hand, compared to the sequences of the two TIG-susceptible strains (Aus0004 and HM1070), four of the five strains exhibiting reduced TIG susceptibility possessed an amino acid substitution in the RpsJ sequence (Fig. 1). As was observed for the AusTig mutant, the HMtig1 and HMtig2 in vitro mutants showed an Asp60Tyr modification, whereas the EF16 clinical isolate had a Lys57Glu substitution. This strongly suggests that alteration of RpsJ could be (at least partially) responsible for TIG resistance in E. faecium. Thus, we sought to evaluate the role of these loci in TIG-susceptible wild-type E. faecium. We tried several times to construct an rpsJ deletion mutant, but all attempts failed, suggesting that rpsJ is likely essential for E. faecium.
FIG 1.
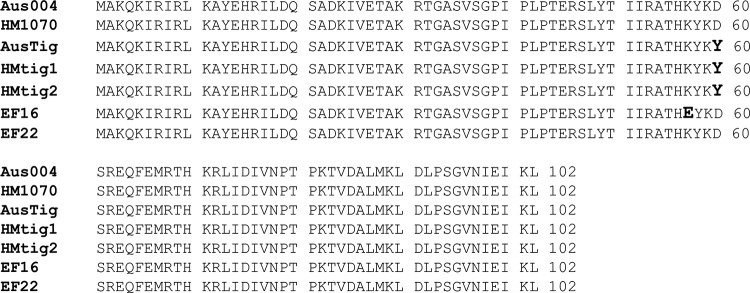
Alignment of RpsJ sequences from E. faecium strains. Mutant AusTig and mutants HMtig1 and HMtig2 are in vitro mutants from the E. faecium Aus0004 and HM1070 wild-type strains, respectively. EF16 and EF22 are vanA-positive E. faecium clinical isolates. Amino acid substitutions (compared to the sequences of the wild-type strains) are indicated in bold.
DISCUSSION
Since 2005, TIG has been approved for use for the treatment of complicated intra-abdominal infections, skin and skin structure infections, and pneumonia. Because TIG overcomes ribosomal protection and active efflux mechanisms that confer resistance to classical tetracyclines, it has attracted particular interest for the treatment of infections caused by multidrug-resistant (MDR) strains. However, reports of clinical resistance to TIG have recently increased, especially among isolates of A. baumannii and the Enterobacteriaceae (8). In contrast, TIG resistance remains seldom reported in Gram-positive bacteria, even if some intermediate or resistant strains have been described in Staphylococcus spp. and Enterococcus spp., but it has never been detected in E. faecium (8, 10–12, 23). The first clinical isolate of E. faecalis resistant to TIG (MIC, 1 μg/ml) was found in 2008 (11). Moreover, among 208 Gram-positive strains isolated from patients with secondary peritonitis, 18.9% of E. faecalis isolates were categorized as intermediate or resistant (MICs, 0.25 to 1 μg/ml), whereas no nonsusceptible E. faecium isolates were found (24). In a recent Portuguese study, several nonsusceptible enterococcal strains (MIC range, 0.5 to 1 μg/ml) were detected from hospitalized patients (2 E. faecalis strains), healthy humans (2 E. faecalis strains), and food products (3 E. faecalis strains, 1 Enterococcus hirae strain, 1 Enterococcus gallinarum strain, and 1 other strain) (12). A recent study from the Tigecycline Evaluation and Surveillance Trial (TEST) revealed that all E. faecium strains isolated in the Middle East and Africa recovered between 2004 and 2011 remained susceptible to TIG and linezolid, including VRE isolates (25). The lack of E. faecium clinical isolates intermediate or resistant to TIG correlates well with the fact that it was tedious to select nonsusceptible mutants (with a maximum MIC of 0.25 μg/ml) in vitro. Note that higher MICs may arise clinically since EF16 showed a MIC of 0.5 μg/ml. It is likely that the ability to acquire better resistance to TIG is strain dependent. This has also been observed for S. aureus, where attempts to select mutants of strain 8325-4 were unsuccessful, whereas in vitro Mu3 and N315 mutants with MICs of 16 μg/ml and 4 μg/ml, respectively, were obtained (10).
As opposed to Gram-negative organisms and S. aureus, for which resistance is mainly related to overexpression of efflux pump systems (8, 10), this mechanism did not seem to occur in E. faecium, since the presence of an EPI did not affect TIG susceptibility. Similar results were observed with a TIG-resistant strain of E. faecalis (11).
By whole-genome analysis, we were able to characterize for the first time genetic determinants associated with reduced TIG susceptibility in enterococci. Only four mutations leading to amino acid substitutions (in efau004_00094, efau004_01228, efau004_01636, and efau004_02425) were identified in the genome of an in vitro mutant with reduced TIG susceptibility (AusTig) and were considered good candidates. Because the efau004_01228 mutant showed the same TIG MIC as the wild-type strain, efau004_01636 was found only in Aus004 and its derivative strains, and efau004_02425, which encodes lactate oxidase, is a metabolic enzyme without a link with the translation pathway, the mutation in efau004_00094, coding for RpsJ (S10 ribosomal protein), could have an important influence on decreased susceptibility to TIG. In order to support this hypothesis, we analyzed the sequences of these four genes in different strains less susceptible to TIG. Only modifications in RpsJ were identified in four of the five strains with reduced susceptibility to TIG. The small S10 protein is a component of the 30S subunit that is the target of the antibiotic, which thus impedes protein synthesis. Interestingly, in E. coli, protein S10 also participates (together with the NusB protein) in processive transcription antitermination of rRNA operons and thus plays a role in the feedback control of ribosome biogenesis (26). In this context, it is suspected that the only function of NusB in antitermination is that of an adaptor facilitating the interaction between S10 and the transcription elongation complex. S10 qualifies as a moonlight protein, since its transcriptional activity is independent of ribosome binding (near the aminoacyl-tRNA site in the structure of the 30S subunit) (27). For both activities, the S10 loop (residues 46 to 67) is of architectural importance (26). The rpsJ gene is present in a single copy in the genome of E. faecium and is probably essential for the bacteria. Therefore, as expected, no corresponding mutant could be obtained. In K. pneumoniae, it seems that the inactivation of the ramR gene (coding for an indirect negative regulator of the acrAB operon) is the most common mechanism conferring resistance to TIG (28). Nevertheless, it has recently been demonstrated that the resistance to TIG of the KPC-producing K. pneumoniae KP4-R strain was due to a Val57Leu substitution in the RpsJ protein sequence (28). Moreover, as for the strains used in this study, the efflux did not appear to be involved in TIG resistance, pointing out that structural alteration of the ribosomal protein S10 in the drug target site may be a potential novel mechanism. However, since such a substitution was not present in the EF22 strain, some other mechanism(s) should be involved in the reduced susceptibility to TIG in E. faecium and remains to be elucidated.
In Neisseria gonorrhoeae, in combination with the mtrR and penB resistance determinants, the mutation that maps to the vertex of a loop in S10 was also shown to be associated with tetracycline resistance (29). In addition, in Bacillus subtilis bearing mutations in tet(A) and tet(B), the Lys46Glu substitution in the S10 protein sequence confers high-level resistance to tetracyclines (30). It was therefore tempting to speculate that the reduced susceptibility to TIG can affect the MICs of other tetracyclines. Interestingly, we observed that in vitro mutant strains also became more resistant to doxycycline, minocycline, and tetracycline independently of the presence of the tet gene. It therefore appears that altered RpsJ may be one of the determinants of resistance to tetracyclines, acting by reducing the affinity of the antibiotic for its ribosomal target. The analysis of the rpsJ sequence, in addition to the screening of tet genes, should therefore be undertaken for clinical isolates exhibiting resistance to tetracyclines. This point seems to be relevant, since classical tetracyclines (but not TIG), which are extensively used in veterinary medicine, might constitute a selective pressure for the emergence of TIG-nonsusceptible strains (12).
ACKNOWLEDGMENTS
This work was supported by a grant from the Ministère de l'Enseignement Supérieur et de la Recherche (EA4655) and the 7th Framework European Program TROCAR.
The expert technical assistance of Michel Auzou was greatly appreciated.
We all read and approved the manuscript, and we declare no conflicts of interest.
REFERENCES
- 1.Arias CA, Murray BE. 2012. The rise of the Enterococcus: beyond vancomycin resistance. Nat Rev Microbiol 10:266–278. doi: 10.1038/nrmicro2761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Top J, Willems R, Bonten M. 2008. Emergence of CC17 Enterococcus faecium from commensal to hospital-adapted pathogen. FEMS Immunol Med Microbiol 52:297–308. doi: 10.1111/j.1574-695X.2008.00383.x. [DOI] [PubMed] [Google Scholar]
- 3.Cattoir V, Giard JC. 2014. Antibiotic resistance in Enterococcus faecium clinical isolates. Expert Rev Anti Infect Ther 12:239–248. doi: 10.1586/14787210.2014.870886. [DOI] [PubMed] [Google Scholar]
- 4.Noskin GA. 2005. Tigecycline: a new glycylcycline for treatment of serious infections. Clin Infect Dis 41:S303–S314. doi: 10.1086/431672. [DOI] [PubMed] [Google Scholar]
- 5.Wenzel R, Bate G, Kirkpatrick P. 2005. Tigecycline. Nat Rev Drug Discov 4:809–810. doi: 10.1038/nrd1857. [DOI] [PubMed] [Google Scholar]
- 6.Bauer G, Berens C, Projan SJ, Hillen W. 2004. Comparison of tetracycline and tigecycline binding to ribosomes mapped by dimethylsulphate and drug-directed Fe2+ cleavage of 16S rRNA. J Antimicrob. Chemother 53:592–599. doi: 10.1093/jac/dkh125. [DOI] [PubMed] [Google Scholar]
- 7.Keeney D, Ruzin A, McAleese F, Murphy E, Bradford PA. 2008. MarA-mediated overexpression of the AcrAB efflux pump results in decreased susceptibility to tigecycline in Escherichia coli. J Antimicrob Chemother 61:46–53. doi: 10.1093/jac/dkm397. [DOI] [PubMed] [Google Scholar]
- 8.Sun Y, Cai Y, Liu X, Bai N, Liang B, Wang R. 2013. The emergence of clinical resistance to tigecycline. Int J Antimicrob Agents 41:110–116. doi: 10.1016/j.ijantimicag.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Veleba M, Higgins PG, Gonzalez G, Seifert H, Schneiders T. 2012. Characterization of RarA, a novel AraC family multidrug resistance regulator in Klebsiella pneumoniae. Antimicrob Agents Chemother 56:4450–4458. doi: 10.1128/AAC.00456-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McAleese F, Petersen P, Ruzin A, Dunman PM, Murphy E, Projan SJ, Bradford PA. 2005. A novel MATE family efflux pump contributes to the reduced susceptibility of laboratory-derived Staphylococcus aureus mutants to tigecycline. Antimicrob Agents Chemother 49:1865–1871. doi: 10.1128/AAC.49.5.1865-1871.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Werner G, Gfrörer S, Fleige C, Witte W, Klare I. 2008. Tigecycline-resistant Enterococcus faecalis strain isolated from a German intensive care unit patient. J Antimicrob Chemother 61:1182–1183. doi: 10.1093/jac/dkn065. [DOI] [PubMed] [Google Scholar]
- 12.Freitas AR, Novais C, Correia R, Monteiro M, Coque TM, Peixe L. 2011. Non-susceptibility to tigecycline in enterococci from hospitalised patients, food products and community sources. Int J Antimicrob Agents 38:174–176. doi: 10.1016/j.ijantimicag.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Cattoir V, Bucquet F, Giard J-C. 2014. Genomic analysis of reduced susceptibility to tigecycline in Enterococcus faecium, abstr. C-843 Abstr 54th Intersci Conf Antimicrob Agents Chemother American Society for Microbiology, Washington, DC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lam MM, Seemann T, Bulach DM, Gladman SL, Chen H, Haring V, Moore RJ, Ballard S, Grayson ML, Johnson PD, Howden BP, Stinear TP. 2012. Comparative analysis of the first complete Enterococcus faecium genome. J Bacteriol 194:2334–2341. doi: 10.1128/JB.00259-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bozdogan B, Leclercq R. 1999. Effects of genes encoding resistance to streptogramins A and B on the activity of quinupristin-dalfopristin against Enterococcus faecium. Antimicrob Agents Chemother 43:2720–2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leenhouts K, Buist G, Bolhuis A, ten Berge A, Kiel J, Mierau I, Dabrowska M, Venema G, Kok J. 1996. A general system for generating unlabelled gene replacements in bacterial chromosomes. Mol Gen Genet 253:217–224. doi: 10.1007/s004380050315. [DOI] [PubMed] [Google Scholar]
- 17.Clinical and Laboratory Standards Institute. 2013. Performance standards for antimicrobial susceptibility testing; approved standard, 23rd ed, M100-S23 Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 18.Ahmed M, Borsch CM, Neyfakh AA, Schuldiner S. 1993. Mutants of the Bacillus subtilis multidrug transporter Bmr with altered sensitivity to the antihypertensive alkaloid reserpine. J Biol Chem 268:11086–11089. [PubMed] [Google Scholar]
- 19.Lebreton F, van Schaik W, Sanguinetti M, Posteraro B, Torelli R, Le Bras F, Verneuil N, Zhang X, Giard JC, Dhalluin A, Willems RJ, Leclercq R, Cattoir V. 2012. AsrR is an oxidative stress sensing regulator modulating Enterococcus faecium opportunistic traits, antimicrobial resistance, and pathogenicity. PLoS Pathog 8:e1002834. doi: 10.1371/journal.ppat.1002834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang X, Vrijenhoek JE, Bonten MJ, Willems RJ, van Schaik W. 2011. A genetic element present on megaplasmids allows Enterococcus faecium to use raffinose as carbon source. Environ Microbiol 13:518–528. doi: 10.1111/j.1462-2920.2010.02355.x. [DOI] [PubMed] [Google Scholar]
- 21.Poyart C. 2010. Tetracyclines, p 327–337. In Courvalin P, Leclercq R, Rice LB (ed), Antibiogram. ASM Press, Washington, DC. [Google Scholar]
- 22.Nishimoto Y, Kobayashi N, Alam MM, Ishino M, Uehara N, Watanabe N. 2005. Analysis of the prevalence of tetracycline resistance genes in clinical isolates of Enterococcus faecalis and Enterococcus faecium in a Japanese hospital. Microb Drug Resist 11:146–153. doi: 10.1089/mdr.2005.11.146. [DOI] [PubMed] [Google Scholar]
- 23.Stein GE, Babinchak T. 2013. Tigecycline: an update. Diagn Microbiol Infect Dis 75:331–336. doi: 10.1016/j.diagmicrobio.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Tubau F, Liñares J, Rodríguez MD, Cercenado E, Aldea MJ, González-Romo F, Torroba L, Berdonces P, Plazas J, Aguilar L, Delgado A, García-Escribano N, Study Group . 2010. Susceptibility to tigecycline of isolates from samples collected in hospitalized patients with secondary peritonitis undergoing surgery. Diagn Microbiol Infect Dis 66:308–313. doi: 10.1016/j.diagmicrobio.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 25.Kanj SS, Whitelaw A, Dowzicky MJ. 2014. In vitro activity of tigecycline and comparators against Gram-positive and Gram-negative isolates collected from the Middle East and Africa between 2004 and 2011. Int J Antimicrob Agents 43:170–178. doi: 10.1016/j.ijantimicag.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 26.Luo X, Hsiao HH, Bubunenko M, Weber G, Court DL, Gottesman ME, Urlaub H, Wahl MC. 2008. Structural and functional analysis of the E. coli NusB-S10 transcription antitermination complex. Mol Cell 32:791–802. doi: 10.1016/j.molcel.2008.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weisberg RA. 2008. Transcription by moonlight: structural basis of an extraribosomal activity of ribosomal protein S10. Mol Cell 32:747–748. doi: 10.1016/j.molcel.2008.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Villa L, Feudi C, Fortini D, García-Fernández A, Carattoli A. 2014. Genomics of KPC-producing Klebsiella pneumoniae sequence type 512 clone highlights the role of RamR and ribosomal S10 protein mutations in conferring tigecycline resistance. Antimicrob Agents Chemother 58:1707–1712. doi: 10.1128/AAC.01803-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu M, Nandi S, Davies C, Nicholas RA. 2005. High-level chromosomally mediated tetracycline resistance in Neisseria gonorrhoeae results from a point mutation in the rpsJ gene encoding ribosomal protein S10 in combination with the mtrR and penB resistance determinants. Antimicrob Agents Chemother 49:4327–4334. doi: 10.1128/AAC.49.10.4327-4334.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams G, Smith I. 1979. Chromosomal mutations causing resistance to tetracycline in Bacillus subtilis. Mol Gen Genet 177:23–29. doi: 10.1007/BF00267249. [DOI] [PubMed] [Google Scholar]


