Abstract
Background
Fatal opioid overdose is a significant cause of mortality among injection drug users (IDUs).
Methods
We evaluated an overdose prevention and response training programme for IDUs implemented by a community-based organization in Los Angeles, California. During a 1-hour training session participants learned skills to prevent, recognize, and respond to opioid overdoses, including: calling for emergency services, performing rescue breathing, and administering an intramuscular injection of naloxone (an opioid antagonist). Ninety-three IDUs were trained from September 2006 to January 2008. Of those, 66 (71%) enrolled in the evaluation study. In total, 47 of 66 participants (71%) completed both a baseline interview and three-month follow-up interview.
Results
Participants were 21% female, 42% White, 29% African American, and 18% Latino. Most were homeless and reported living predominantly in the street (44%), temporary housing such as hotels or motels (15%), or shelters (14%). Significant increases were found in overdose knowledge, driven largely by increase in knowledge about the appropriate use of naloxone. Twenty-two participants witnessed and responded to 35 overdoses during the follow-up period. Twenty-six overdose victims were reported to have recovered, four died, and the outcome of five cases was unknown. The most commonly reported response techniques included: staying with the victim (85%), administering naloxone (80%), providing rescue breathing (66%), and calling emergency services (60%). The average number of appropriate response techniques used by participants increased significantly from baseline to follow-up (p<0.05). Half (53%) of programme participants reported that their drug use decreased at follow-up.
Conclusion
Results suggest that overdose prevention and response training programmes may be associated with improvements in knowledge and overdose response behaviour among IDUs, with few adverse consequences and some unforeseen benefits, such as reductions in drug use.
Keywords: opioid overdose, naloxone, evaluation, injection drug use, intervention, homeless
INTRODUCTION
Fatal opioid overdose is a significant cause of premature mortality.The U.S. Centers for Disease Control and Prevention report that in 2005, 33, 541 persons died of drug-induced causes in the United States (Kung et al., 2008). In 2003, opioids were responsible for more drug-related deaths than any other drug as reported by the U.S. Drug Abuse Warning Network (SAMHSA Office of Applied Studies, 2005). Heroin or metabolites specific to heroin were reported in more than one-third of opioid-related overdose deaths reported by DAWN, though prescription opioids such as methadone, hydrocodone, and oxycodone, also contribute significantly to opioid-related mortality in the U.S. (SAMHSA Office of Applied Studies, 2005; Zacny et al., 2003).
Administration of opioids via the intravenous route significantly elevates the risk of overdose (Sporer, 1999). Studies among IDUs in the United States and abroad have found rates of witnessed drug overdoses ranging from 54% to 92% (Galea et al., 2006; Pollini et al., 2006; Seal et al., 2003; Strang et al., 1999), and rates of non-fatal overdoses experienced by IDUs ranging from 40% to 68% (Galea et al., 2006; Kerr et al., 2007; Pollini et al., 2006; Strang et al., 1999). Opioid overdoses result in mortality by depressing respiration in the overdose victim, ultimately leading to hypoxia and death (White & Irvine, 1999). Because death resulting from opioid overdoses generally takes 1–3 hours, there is usually time for medical intervention (Sporer, 1999).
In the United States and elsewhere, IDUs have demonstrated a willingness to be trained to respond to potentially fatal opioid overdoses among their peers (Seal et al., 2003; Strang et al., 2000; Strang et al., 1999), and preliminary evaluations suggest that training programmes can produce sustained increases in knowledge and response skills, potentially saving lives (Green et al., 2008). As a result, training programmes have been implemented in some areas of the U.S., including New York (Galea et al., 2006; Piper et al., 2007), Chicago (Maxwell et al., 2006), New Mexico (New Mexico Department of Health, 2008), Baltimore (Tobin et al., 2008), and San Francisco (Seal et al., 2005). These programmes generally include training in the recognition of opioid overdose and appropriate response techniques, including rescue breathing and the administration of naloxone. Naloxone is an opioid antagonist (Julien, 2005) that is routinely used in clinical and pre-clinical settings to reverse potentially fatal opioid overdoses (Baca & Grant, 2005). Some side effects associated with naloxone administration have been reported, but are relatively rare (Sporer, 1999,2003) and have been debated (Hsu et al., 1997). Naloxone has no psychoactive properties or pharmacologic activity in the absence of opioids. In the United States, naloxone is available only by prescription and is not sold over the counter (Burris et al., 2001).
Homelessness has been associated with an elevated risk of experiencing overdose among IDUs (Kerr et al., 2007). The Skid Row area of Los Angeles, California has the highest concentration of homeless persons in the city of Los Angeles (over 5,000 individuals on any given night), 30% of whom report current drug use (Los Angeles Homeless Services Authority, 2007). While drug overdose was the 6th leading cause of premature death in all of Los Angeles County, it was the 4th leading cause of premature death in the area where Skid Row is located (Los Angeles County Department of Public Health, 2006). Homeless individuals may face additional challenges in storing prescription medications such as naloxone. Therefore, those living on the streets of Skid Row are at increased risk of experiencing fatal opioid overdoses. In this paper, we report on the evaluation of an overdose prevention and response training programme that was implemented September of 2006 for IDUs in the Skid Row area of Los Angeles, California.
METHODS
The Homeless Health Care Los Angeles Center for Harm Reduction (HHCLA-HRC) is a community-based organization that provides services to IDUs including syringe exchange, medical care, case management, and referrals to drug detoxification programmes. Eligibility criteria for the HHCLA-HRC are: 1) being a current IDU, and 2) being at least 18 years old. Clients are not required to be residents of the Skid Row area, but most live, access services, and buy and/or use drugs in the Skid Row area. In September 2006, HHCLA-HRC staff offered an overdose prevention and response training programme to all HHCLA-HRC clients. Participants were recruited via street outreach, distribution of advertising leaflets, and one-on-one recruitment within the HRC. Interested IDUs were referred to one of several HHCLA staff members who explained more about the training and enrolled participants.
The Overdose Prevention and Response Training Programme
Trainings were conducted individually or in small groups (2–6 people) by KDW and MG. Both trainers were educated in overdose prevention and response training through their participation in local overdose prevention efforts and a “Train the Trainer” seminar conducted by the Harm Reduction Coalition. Trainings were offered four days a week, depending on staff availability, on a drop-in basis. Each training consisted of a single, one-hour session that covered four primary topics: 1) mechanisms of opioid overdose, 2) strategies for the prevention of opioid overdose, 3) recognition of opioid overdose, and 4) recommended response techniques. The entire curriculum is available from the authors. Appropriate response techniques followed the S.C.A.R.E. M.E. strategy developed by the Chicago Recovery Alliance (www.anypositivechange.org): Stimulation, Call for help, Rescue breathing, Evaluation, Muscular injection of naloxone, Evaluation and support (including staying with the victim until medical help arrives and placing the victim in the recovery position).
The trainers presented the information using a set of prepared slides, and discussion was encouraged throughout. A hands-on demonstration and practice session followed the presentation. Participants were encouraged to discuss the information they learned in the training with friends, family, or using buddies, and the trainers suggested that they send those individuals in to be trained, as well, though no educational tools were provided for the purpose of training others.
Upon successfully demonstrating knowledge and skills in the four topic areas, each participant met one-on-one with the programme physician, who documented the encounter and provided two doses of naloxone in 1ml (.4 mg/ml naloxone), pre-filled, single-dose syringes. A prescription label was affixed to the box, dated, and signed by the physician. Participants also received a kit containing latex gloves, alcohol swabs, a rescue breathing mask, and a small card describing the response technique. There was no limit on the number of doses that participants could receive, nor on the number of times they could return for refills.
The Evaluation Study
Study recruitment was conducted from September 2006 to January 2008. All training participants were offered the opportunity to participate in the evaluation study. Participation in the training was not contingent upon study enrolment. The University of Southern California Institutional Review Board approved all study procedures. The study aimed to assess whether training participants: 1) increased knowledge related to naloxone and overdose risks/symptoms, 2) improved attitudes related to overdose response and summoning emergency assistance, 3) increased the frequency with which they engaged in recommended overdose response techniques, and 4) decreased the frequency with which they engaged in non-recommended overdose response techniques.
If training participants agreed to enroll in the study, they immediately provided written informed consent and completed a short baseline interview. Participants returned three months later to complete a follow-up interview. When possible, participants were contacted via email, phone, and/or letter to remind them of their follow-up visit. The Los Angeles County Sheriff's inmate locater database, which is publicly available via the Internet, was checked when a participant did not return for his/her scheduled follow-up interview. If participants were incarcerated on the date of their scheduled interview and for the majority of the one-month period thereafter, they were considered “unavailable” to conduct their follow-up interview.
Those who returned to obtain a refill of naloxone for any reason during the follow-up period also completed an incident report documenting the circumstances necessitating the refill, including loss, theft, confiscation, or use. If the naloxone was used to respond to an overdose, detailed information was collected about the response. Participants received a $5 food voucher for completing the baseline assessment, and $20 and a $5 food voucher for completing the three-month follow-up assessment.
Measures
Trained interviewers administered the surveys in private offices at the HHCLA-HRC. Demographic information including age, race, ethnicity, housing status, drug use behaviour, and enrolment in drug treatment were collected at baseline and three-month follow-up. For the most recent overdose experienced and witnessed in the past three months we asked a series of questions about the signs used to recognize the overdose, techniques used to respond, outcome (i.e., survived or not), and negative consequences associated with the overdose. Knowledge was assessed at both baseline and three-month follow-up using six questions, similar to those used by others (Tobin et al., 2008), that asked about risk factors for overdose, symptoms used to recognize an opioid overdose, and appropriate use of naloxone (Table 2). Attitudes towards responding to overdoses (i.e., likelihood of administering naloxone, calling emergency services, and teaching someone else to respond to an overdose) were assessed on a 5-point Likert-type scale with response choices ranging from “definitely not likely” to “very likely”. At follow-up, participants were asked whether they still had the naloxone they were given at the training and, if not, what happened to it.
Table 2.
Changes in knowledge, attitudes, and behaviour from baseline to three-month follow-up (n=47).
| Baseline | 3-month follow-up |
Test statistic* |
p-value | |
|---|---|---|---|---|
| Overall knowledge mean (std) | 76.5 (15.4) | 91.5 (9.6) | t=6.94 | <0.0001 |
| Overall knowledge median (IQR) | 77.8 (66.7 – 88.9) | 88.9 (88.9 – 1.0) | S=334.50 | <0.0001 |
| Knowledge items (% correct): | ||||
| Drinking alcohol when using opiates increases your risk of OD | 78.7 | 91.5 | χ2 = 3.00 | 0.15 |
| Slamming your drugs increases your risk of OD | 89.4 | 97.9 | χ2 = 2.67 | 0.22 |
| Using drugs after getting out of detox or jail/prison increases your risk of OD | 87.2 | 100.0 | -- | |
| You are at greatest risk of dying from an OD if you are alone when you inject | 100.0 | 100.0 | -- | |
| Change in the color of someone's lips/nails is a sign of heroin OD | 85.1 | 97.9 | χ2 = 4.50 | 0.07 |
| Heroin OD causes your heartbeat to speed up | 85.1 | 78.7 | χ2 = 1.29 | 0.45 |
| After a person has been revived with naloxone, they can fall back into an OD | 48.9 | 89.4 | χ2 = 19.00 | <0.0001 |
| The effect of naloxone lasts for 24 hours | 31.9 | 70.2 | χ2 = 12.46 | 0.03 |
| Naloxone works for a heroin OD (not cocaine or both) | 83.0 | 97.9 | χ2 = 5.44 | 0.04 |
| Attitude items: | ||||
| Worried about getting arrested for calling emergency services | 15 (32%) | 16 (34%) | χ2 = 0.11 | 0.99 |
| Likelihood you will give someone a shot of naloxone if they OD’d near you (median, range: 1–5) | 5 | 5 | S = 21.5 | 0.27 |
| Likelihood you will call emergency services if you are with someone who OD’d (median, range 1–5) | 5 | 5 | S = 3.5 | 0.90 |
| Likelihood of teaching someone to respond to an OD in the next three months (median, range 1–5) | 4.5 | 3.5 | S = −76.5 | 0.03 |
| Behavior items: | ||||
| Trained someone to respond to an OD since training | --- | 19 (40.4%) | ||
| Change in drug use since training | ||||
| Increased | --- | 6 (12.8%) | ||
| Decreased | --- | 25 (53.2%) | ||
| No change | --- | 16 (34.0%) | ||
| Currently enrolled in drug treatment | 10 (22.7%) | 16 (36.4%) | χ2 =4.5 | 0.07 |
t = Paired Student’s t-test; S=Wilcoxon Signed Rank test; χ2 = McNemar's test
Analysis
Univariate statistics were calculated for all variables of interest. Attrition analysis was conducted using Chi-square tests or Fischer’s Exact test when expected cell frequencies were less than five. To examine changes in knowledge and attitudes (aims 1 and 2), we included all those individuals who completed both a baseline and three-month follow-up survey. A single knowledge index was created, representing the percent of correct answers. Because the psychometric properties of this index were poor (Cronbach’s alpha = 0.39), we also report the score on each individual item. Changes in knowledge and attitudes from baseline to follow-up were calculated using paired Student's t-test for means, Wilcoxon Signed Rank test for medians, and McNemar’s test for paired proportions.
We next described the total number of overdose responses reported during the follow-up period using data from the three-month follow-up surveys and incident reports, including characteristics of the overdose, symptoms used to recognize the overdose, response behaviour, and outcome. To investigate changes in overdose response behaviour (aims 3 and 4), we restricted the follow-up data set to those who reported responding to an overdose both at baseline and at three-month follow-up. Because of the limitations introduced by the small sample size, we collapsed outcome variables into two summary measures representing the average number of recommended and non-recommended response techniques employed at each event. We compared the summary measure using paired Student's t-tests for means and Wilcoxon Signed Rank tests for medians. The proportion of witnessed overdoses to which participants responded was compared using McNemar’s test. All analyses were conducted using SAS 9.1.3.
RESULTS
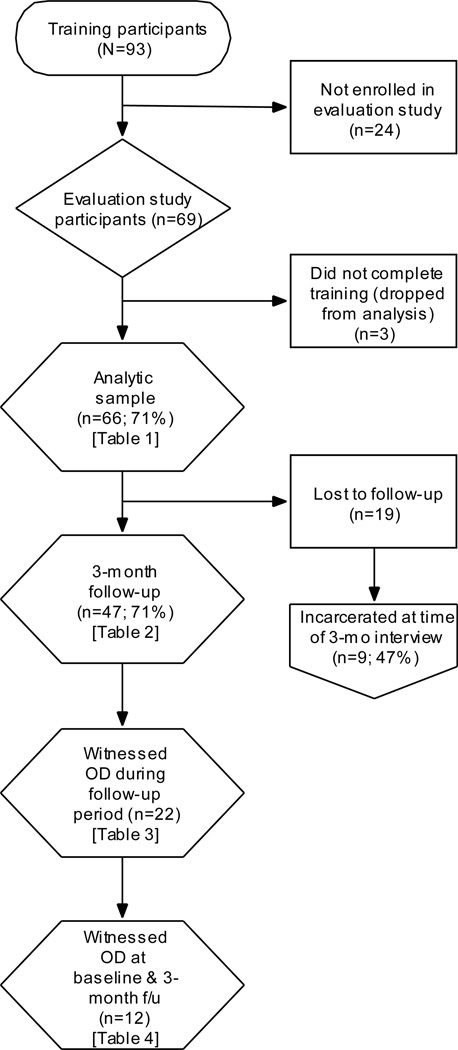
Ninety-three IDUs were trained from September 2006 to January 2008. Of those, 69 (74%) enrolled in the evaluation study. Figure 1 shows study participation rates. Though no data were collected from those who refused to enroll, anecdotal accounts suggest that the most common reasons for not enrolling were not having enough time and not wanting to return for the follow-up interview. Of those who enrolled, three did not complete the training (because they were too high or too tired) and were dropped from subsequent analysis, yielding an analytic sample of 66. Demographic characteristics are described in Table 1. Participants were 21% female, 42% White, 29% African American, and 18% Latino and 11% other or mixed. Most were homeless and reported living predominantly in the street (44%), temporary housing such as hotels or motels (15%), or shelters (14%). Ninety-seven percent reported using heroin, and of those 98% said their preferred mode of administration was injection. Use of other drugs such as crack, alcohol, benzodiazepines, and other opiates was also common. Program participants were similar to the larger population of HHCLA-HRC clients in gender and ethnicity (all p’s >0.05), but were significantly more likely to be homeless (p=0.002).
Figure 1.
Flow diagram of training and evaluation study participation.
Table 1.
Demographic characteristics of study participants and experience with drug overdoses in 3 months prior to training (N=66).
| N | % | |
|---|---|---|
| Age | ||
| Mean (std) | 45.8 (9.1) | |
| Median (IQR) | 46.5(41–52) | |
| Age of first injection | ||
| Mean (std) | 21.5 (9.1) | |
| Median (IQR) | 19.5 (15–26) | |
| Female | 14 | 21.1 |
| Ethnicity | ||
| White | 28 | 42.4 |
| African American | 19 | 28.8 |
| Latino | 12 | 18.2 |
| Mixed ethnicity | 4 | 6.1 |
| American Indian | 2 | 3.0 |
| Asian | 1 | 1.5 |
| Housing status. Living in: | ||
| The street or in a car | 29 | 43.9 |
| My own house | 12 | 18.2 |
| Hotel/motel/SRO | 10 | 15.2 |
| Shelter | 9 | 13.6 |
| Someone else’s house | 4 | 6.1 |
| Other | 2 | 3.0 |
| Drugs used (past 30 days)*: | ||
| Heroin | 58 | 96.7 |
| Crack cocaine | 23 | 38.3 |
| Alcohol | 12 | 20.0 |
| Benzodiazapines | 7 | 11.7 |
| Other opiates | 6 | 10.0 |
| Powder cocaine | 3 | 5.0 |
| Methadone (non-prescribed) | 3 | 5.0 |
| Methamphetamine | 2 | 3.3 |
| Number of participants who experienced OD in 3 months prior to training | 10 | 15.2 |
| Total number of ODs experienced | 24 | |
| Number of participants who witnessed OD in 3 months prior to training | 32 | 48.5 |
| Total number of ODs witnessed | 148 |
drug categories are not mutually exclusive
Among the 66 training participants, 10 (15%) reported experiencing an overdose in the three months prior to the training. The median number of overdoses experienced before the training was one (Interquartile Range; IQR: 1-1). While nine individuals reported overdosing only once in the previous three months, one individual reported overdosing 15 times. Thirty-two participants (49%) reported having witnessed an overdose in the three months prior to the training. In 29 cases (91%), the victim recovered or was taken to the hospital. In 3 cases (9%) the victim was already dead or died at the scene. These 32 participants reported witnessing a total of 148 overdoses; the median witnessed by an individual was two overdoses (IQR: 1–4). While most individuals reported witnessing between one and six overdoses in the previous three months, one individual reported witnessing 37 and another reported witnessing 50 overdoses. These two individuals also reported heavy drug use, and may have been exposed to multiple overdoses due to their heavy drug and street involvement.
Forty-seven participants (71%) returned to complete their three-month follow-up interview. Participants lost to follow-up were similar to those who were retained in age (p=0.99), gender (p=0.98), homelessness (p=0.12), race (white vs non-white, p=0.55), current drug treatment enrolment (p=0.09), and experiencing an overdose in the past three months (p=0.71). Of the 19 participants lost to follow-up, 9 (47%) were unavailable to conduct their interview because they were incarcerated. No other information was available regarding reasons participants were lost to follow-up.
Table 2 describes changes from baseline to follow-up among the 47 individuals who returned for their three-month follow-up. Overall, baseline knowledge was high. Still, scores on the overall knowledge index increased significantly from baseline to three-month follow-up (mean score increased from 77% to 92% and median increased from 78% to 89%, p’s <0.0001). Changes in individual knowledge items are also reported. A statistically significant increase was observed for three items that asked about the appropriate use and effects of naloxone. No significant changes were observed in the items asking about risk factors for overdose or overdose symptoms, and two items had scores of 100% at follow-up.
No significant changes were observed in attitudes about overdose response, including likelihood of administering naloxone, likelihood of calling emergency services, or worry over being arrested after calling emergency services (all p’s >0.05). At three-month follow-up, the likelihood that participants would train someone else in overdose response in the next three months decreased significantly (p=0.03). At the same time, 19 (40%) participants reported at follow-up that they had already trained someone in the interim three months. Having trained someone in overdose response was significantly associated with increased intention to train someone at follow-up, controlling for baseline intention (β = 0.42, p<0.01).
At follow-up, participants were asked whether their drug use had increased, decreased, or stayed the same since the training. A majority (53%) reported that their drug use had decreased. In support of this observation, an increased proportion reported enrolment in drug treatment, from 23% to 36% (p=0.07).
During the follow-up period, 22 individuals reported responding to a total of 35 overdoses (Table 3). Most of the overdose victims were strangers (40%), associates/acquaintances (31%), and friends (17%). One participant provided data about her own overdose, during which her friend injected her with her own naloxone. Another provided information about the use of his naloxone by a friend to rescue a third party. Nine individuals reported responding to more than one overdose. Those who responded to multiple overdoses were similar to those who responded to one or fewer in age, gender, and homelessness status (all p’s >0.10). The most overdoses responded to during the follow-up period by a single person was four. Similar to the others, multiple responders most frequently responded to overdoses experienced by strangers (64%), associates/acquaintances (27%), and friends (7%). Due to the limitations posed by small cell sizes, these proportions were not assessed for statistical significance.
Table 3.
Characteristics of 35 overdoses witnessed during follow-up period, as reported by 22 individuals.
| N | % | |
|---|---|---|
| Relationship to victim: | ||
| Stranger | 14 | 40.0 |
| Associate/acquaintance | 11 | 31.4 |
| Friend | 6 | 17.1 |
| Self | 1 | 2.9 |
| Sex partner | 1 | 2.9 |
| Dealer | 1 | 2.9 |
| Other | 1 | 2.9 |
| Signs used to recognize overdose:* | ||
| Non-responsive | 20 | 57.1 |
| Abnormal or no breathing | 19 | 54.3 |
| Lips/fingers turned blue | 18 | 51.4 |
| Collapsed | 10 | 28.5 |
| He/she was in a ‘nod’ | 5 | 14.3 |
| Other† | 17 | 48.6 |
| Response to overdose:* | ||
| Appropriate responses: | ||
| Stimulated by sternum rub | 9 | 25.7 |
| Called emergency services (n=34) | 21 | 60.0 |
| Police responded | 14 | 66.7 |
| Someone got arrested at the scene | 3 | 14.3 |
| Rescue breathing/CPR | 23 | 65.7 |
| Muscular injection of naloxone | 28 | 80.0 |
| Stayed with victim (n=34) | 29 | 85.3 |
| Inappropriate Responses: | ||
| Did nothing | 3 | 8.6 |
| Stimulated by hitting/slapping/shaking | 12 | 34.3 |
| Rubbed with ice/put in shower/bath/water | 4 | 11.4 |
| Injected with milk or salt water | 0 | -- |
| Injected with cocaine | 0 | -- |
| Other | 7 | 20.0 |
| Outcome: | ||
| Victim recovered and/or was taken to hospital | 26 | 74.3 |
| Victim died | 4 | 11.4 |
| Don’t know | 5 | 14.3 |
| Negative consequences associated with overdose: (n=34)* | ||
| Victim got angry | 5 | 14.7 |
| Someone got arrested | 3 | 8.8 |
| Victim vomited | 1 | 2.9 |
| Victim had a seizure | 0 | -- |
| Other§ | 7 | 20.6 |
Response choices were not mutually exclusive
e.g., “eyes rolled back in head”, “others told me he had overdosed”, “saw the needle in his arm”
e.g., “police harassment”
Participants reported a variety of symptoms that they observed to recognize the overdose. The most frequently symptoms were non-responsiveness (57%), abnormal or no breathing (54%), and change in the color of lips/nails (51%). Finding the victim collapsed (29%) or in a “nod” (14%) was also common. A large proportion (49%) reported other signs of the overdose (e.g., being told that the victim had overdosed by others, finding the victim with a needle in his/her arm, or seeing the victim’s eyes rolled back in his/her head).
Techniques used to respond to the witnessed overdoses were categorized into recommended and non-recommended methods, according to the S.C.A.R.E. M.E. technique taught in the training. Recommended responses included stimulation using the sternum rub (26%), calling emergency services (60%), rescue breathing (66%), administering a muscular injection of naloxone (80%), and staying with the victim until help arrives (85%). Among the 21 individuals who reported calling emergency services, 67% reported that the police responded to the call and 14% said that someone at the scene was arrested.
Non-recommended responses included doing nothing to help the overdose victim (9%), hitting, slapping, shaking the victim (33%), and using ice or cold water to try to revive him/her (11%). Twenty-percent reported some other non-recommended response technique (e.g., walking the person around, trying to stand him/her up, or shouting at him/her). No participants reported injecting the victim with cocaine or other stimulants, milk, or salt water. Approximately half reported using only recommended techniques, while half reported using both recommended and non-recommended techniques.
In 26 (74%) of cases, the victim recovered at the scene and/or was taken to the hospital. In four (11%) cases, the victim was already dead by the time the participant arrived or died at the scene, and in five cases (14%) the outcome was unknown. Negative consequences associated with the witnessed overdoses included the victim getting angry (15%), vomiting (3%), and someone getting arrested (9%). In no account did the victims experience a seizure. Other negative consequences were also reported (e.g., being harassed by police).
In addition to requests to replace used naloxone, six refills were provided to replace naloxone that was lost or stolen, four were provided to replace naloxone confiscated by the police, and four refills were provided for some other reason.
Table 4 presents changes in response behaviour reported by the 12 participants who described witnessing an overdose both at the baseline and three-month follow-up. At both time points, participants reported responding to a similar proportion of the total number of overdoses they witnessed. The average number of recommended response techniques employed increased significantly (mean increased from 2 to 3.3, p=0.01; median increased from 2.0 to 4.0, p=0.02). At three-month follow-up, more participants used the sternum rub to stimulate the victim, provided rescue breathing, administered naloxone, and stayed until help arrived. The mean number of non-recommended responses decreased from 0.9 to 0.7, though this difference was not statistically significant. At three-month follow-up, fewer participants did nothing to help, and fewer used ice or cold water to stimulate the victim.
Table 4.
Changes in behavior in response to witnessed overdoses among participants who reported witnessing overdose at both baseline and 3-month follow-up (n=12).
| Baseline | 3-month follow-up |
Test statistic* |
p- value |
|
|---|---|---|---|---|
| Proportion of witnessed overdoses responded to in past 3 months (n = 10) | 0.66 | 0.75 | S = 4 | 0.58 |
| n (%) | n (%) | |||
| Behavior in response to most recently witnessed overdose: | ||||
| Recommended Responses§ | ||||
| Mean (std) | 2.0 (1.0) | 3.3 (1.1) | t = 3.0 | 0.01 |
| Median (IQR) | 2.0 (1.0–3.0) | 4.0 (2.5–4.0) | S = 25.5 | 0.02 |
| Stimulate with sternum rub | 1 (8.3%) | 3 (25%) | ||
| Call emergency services | 8 (66.7%) | 8 (66.7%) | ||
| Rescue breathing | 6 (50.0%) | 9 (75.0%) | ||
| Naloxone injection | 0 | 8 (66.7%) | ||
| Stayed with victim | 9 (75.0%) | 11 (91.7%) | ||
| Non-recommended Responses§ | ||||
| Mean (std) | 0.9 (0.7) | 0.7 (0.8) | t = −0.9 | 0.39 |
| Median (IQR) | 1.0 (0.5–1.0) | 0.5 (0.0–1.0) | S = −6.0 | 0.56 |
| Nothing | 3 (25.0%) | 1 (8.3%) | ||
| Hit/slapped/shook | 4 (33.3%) | 5 (41.7%) | ||
| Injected with salt or milk | 0 | 0 | ||
| Injected with cocaine | 0 | 0 | ||
| Ice/cold water | 4 (33.3%) | 2 (16.7%) | ||
S = Wilcoxon Signed Rank test; t = Paired Student's t-test
Response choices were dichotomous [yes/no]
DISCUSSION
Over the course of this 16-month programme, 66 individuals were trained in techniques for responding to opioid overdoses and data were collected about 35 overdoses they witnessed after the training. Among the witnessed overdoses, participants reported that 26 (74%) of the victims recovered, while 4 did not. The proportion of victims who died at the scene was similar before (9%) and after (11%) the training. However, important changes in knowledge, attitudes, and response behaviour were observed. Baseline knowledge about overdose risks and symptoms was generally high, which has been observed in other studies (e.g., Strang et al., 2008) and may reflect ongoing risk reduction education and outreach among IDUs prior to the introduction of naloxone. Despite these high baseline levels of knowledge, participants demonstrated significant increases in knowledge at follow-up, driven largely by increases in knowledge about naloxone. Training participants also significantly increased the number of recommended techniques used in response to witnessed overdoses and slightly decreased the number of non-recommended techniques, though this decrease did not achieve statistical significance.
Importantly, 40% of the overdose victims were strangers. This high frequency of assisting strangers may be characteristic of this largely homeless population, where overdoses are more likely to be observed by others. In a sample reporting a lower prevalence of homelessness, the most frequently reported relationship was friend or drug partner (Tobin et al., 2005). Some training participants reported that they discussed their training with other IDUs in the event that an overdose occurred so that they could be summoned to the scene. This phenomenon may represent the acquisition of new forms of “street capital” (Bourdieu, 1986). IDUs trained in overdose response may integrate new response techniques into their behavioural repertoire, leading to changes in social roles. Others have observed that overdose response training may extend the natural caretaking and helping roles that some IDUs assume within their social networks (Sherman et al., 2008). This may be particularly relevant among those IDUs who reported responding to multiple overdoses, and those who trained others in overdose response.
Some have found that the frequency of calling emergency services decreases after participants have undergone this type of training (Tobin et al., 2008), while others have observed an increase (Galea et al., 2006). We found no change in the frequency of calling emergency services before and after the training. Medical follow-up is recommended for overdose victims revived with naloxone, and there is a possibility that victims may not be revived using the techniques learned in a training. However, there are very real and serious consequences that could result from police response to emergency services calls – in this study police responded to two-thirds of the calls and three people were arrested at the scene. The high prevalence of police response and arrest found in this study may reflect an increase in policing in the Skid Row area that coincided with the implementation of the programme (Blasi & others, 2007). The threat of arrest and subsequent incarceration is an important barrier to calling emergency services in the event of a drug overdose (Davidson et al., 2002), though this fear may be moderated by a history of actual contact with police (Tobin et al., 2005). To address the public health implications of the barriers to summoning medical assistance, both individual- and policy-level interventions are needed, such as “Good Samaritan” legislation that protects the individual who calls emergency services from prosecution (New Mexico Department of Health, 2007). In the meantime, it is critical that programmes emphasize the need for medical follow up and that participants are trained to observe for the possibility of relapse and to discourage the victim from using more opioids, in the event that they choose not to summon emergency medical response.
Our results differ somewhat from those of others (e.g., Tobin et al., 2008) who report no incidences of loss, theft or confiscation of participants’ naloxone. Four of our training participants reported having their naloxone confiscated by police and six reported it lost or stolen. In an environment characterized by significant amounts of homelessness, where IDUs are increasingly subject to police surveillance and arrest, the ability of IDUs to hold on to their naloxone long enough to use it is a challenge to the success of this type of programme. More effort is needed to sensitize and educate street-level law enforcement officers regarding the life-saving potential of this type of programme. The loss or theft of naloxone may have been made more likely by the high rates of homelessness observed in this sample. For homeless individuals, challenges related to safely storing naloxone – or any essential medication – need to be addressed.
Concerns that distributing naloxone provides a “safety net” that encourages continued or escalating drug use have been noted (Sporer & Kral, 2007). Our findings and others (Seal et al., 2005) suggest the opposite – 53% of participants in this study reported that their drug use decreased at follow-up, and we observed a marginally significant increase in the proportion reporting current enrolment in drug treatment. Similar to the provision of syringe exchange services, this type of programme may serve as a gateway for under-served individuals to take advantage of other services such as drug treatment. Individuals trained in overdose response and, more specifically, those involved in successful “rescues,” may also experience an increased sense of self-worth that may translate into other positive health behaviors such as reductions in drug use or increased participation in drug treatment and/or other services such as HIV/HCV testing (e.g., Maxwell et al., 2006).
Limitations of this study should be noted. The study design was observational and lacked a control condition, therefore it is impossible to attribute outcome changes soley to the programme. Furthermore, the study design is vulnerable to internal validity threats, including: 1) the effects of unique historical events that may have influenced behaviour or attitudes, 2) selection bias in program participants and/or those who chose to enroll in the evaluation study, 3) testing effects (e.g., improvement in knowledge scores due solely to the learning effect of taking multiple knowledge quizzes over time), and 4) maturation (though the short follow-up period may somewhat limit the effect of maturation). All data are based on self-report and are therefore subject to both recall bias and socially-desirable reporting. Because information about witnessed and observed overdoses were obtained only from those individuals who returned for their follow-up visits or completed an incident report, the number of overdoses witnessed and experienced by study participants is likely underestimated, and there is likely some selection bias in those who returned. Participants in this study were ethnically diverse, but were mostly homeless, somewhat limiting our ability to generalize to non-homeless populations. Given the precariousness of chronic homelessness and the high rates of incarceration during the follow-up period, the 71% follow-up rate was higher than expected and somewhat comparable to others (Strang et al., 2008), though a larger completion rate would have been desirable. However, our findings are strengthened by the fact that those lost to follow-up did not differ significantly from those who were retained. Finally, while the current study provides some preliminary evidence for changes in knowledge and behaviour over the three-month follow-up period, future experimental studies with longer follow-up periods will be required to determine whether these changes are associated with the program and are sustainable over time.
CONCLUSIONS
In this study, we have provided preliminary evidence for the feasibility and efficacy of a relatively low-threshold overdose prevention and response training programme for IDUs. Participants in this programme reported 26 successful overdose reversals, along with increases in knowledge and changes in behaviour. Several quasi-experimental studies have now evaluated overdose prevention and response training programmes to prevent fatal opioid overdoses among IDUs, and findings consistently reflect the ability of these training programmes to change behaviour and to reverse potentially fatal opioid overdoses. These programmes come at relatively low cost to the organization (i.e., staff time and naloxone) compared to the enormous benefit of the lives saved. This study contributes to a growing literature suggesting that overdose prevention and response training programmes for IDUs may be associated with changes in knowledge and overdose response behaviour, with few negative consequences and the possibility of unforeseen benefits such as reductions in drug use or increased utilisation of drug treatment.
ACKNOWLEDGEMENTS
This research was funded by foundation support and private fundraising. †Karla Wagner was contracted as a consultant to HHCLA in the design and implementation of the project. We are indebted to the individuals who participated in the training programme and evaluation study for making this report possible. In addition, we thank the staff of the HHCLA-HRC: Dyhan Cardona, Yolanda Delgado, Seamon Hill, Taviah Hopkins, Ronald McCree, and Carla Toms and the study data collectors: Carla Blieden, James Brasuell, Rachel Grana, and Janie Shelton. Finally, we thank the numerous others who provided consultation and direction on the development of the training programme, evaluation study, and manuscript, including: Josh Bamburger, Dan Bigg, Ricky Bluthenthal, Emalie Hurrieaux, Alex Kral, Sarz Maxwell, Susan Sherman, Elan Shultz, Sharon Stancliff, and Courtney Byrd-Williams.
REFERENCES
- Baca CT, Grant KJ. Take-home naloxone to reduce heroin death. Addiction. 2005;100(12):1823–1831. doi: 10.1111/j.1360-0443.2005.01259.x. [DOI] [PubMed] [Google Scholar]
- Blasi G, et al. Policing our way out of homelessness? The first year of the safer cities initiative on Skid Row. Los Angeles, CA: UCLA School of Law; 2007. [Google Scholar]
- Bourdieu P. The forms of capital. In: Richardson J, editor. Handbook of theory and research for the sociology of education. New York: Greenwood Press; 1986. [Google Scholar]
- Burris S, Norland J, Edlin BR. Legal aspects of providing naloxone to heroin users in the United States. International Journal of Drug Policy. 2001;12(3):237–248. [Google Scholar]
- Davidson PJ, Ochoa KC, Hahn JA, Evans JL, Moss AR. Witnessing heroin-related overdoses: The experiences of young injectors in San Francisco. Addiction. 2002;97(12):1511–1516. doi: 10.1046/j.1360-0443.2002.00210.x. [DOI] [PubMed] [Google Scholar]
- Galea S, Worthington N, Piper TM, Nandi VV, Curtis M, Rosenthal DM. Provision of naloxone to injection drug users as an overdose prevention strategy: Early evidence from a pilot study in New York City. Addictive Behaviors. 2006;31(5):907–912. doi: 10.1016/j.addbeh.2005.07.020. [DOI] [PubMed] [Google Scholar]
- Green TC, Heimer R, Grau LE. Distinguishing signs of opioid overdose and indication for naloxone: An evaluation of six overdose training and naloxone distribution programs in the United States. Addiction. 2008;103(6):979–989. doi: 10.1111/j.1360-0443.2008.02182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu W, Rao RB, Nelson LS. Naloxone hazards overstated. Journal of Toxicology. Clinical Toxicology, 1997. 1997;35(2):215–217. doi: 10.3109/15563659709001198. [DOI] [PubMed] [Google Scholar]
- Julien RM. A primer of drug action. 10th ed. New York: Worth Publishers; 2005. [Google Scholar]
- Kerr T, Fairbairn N, Tyndall M, Marsh D, Li K, Montaner J, et al. Predictors of non-fatal overdose among a cohort of polysubstance-using injection drug users. Drug and Alcohol Dependence. 2007;87(1):39–45. doi: 10.1016/j.drugalcdep.2006.07.009. Epub 2006 Sep 2007. [DOI] [PubMed] [Google Scholar]
- Kung HC, Hoyert DL, Xu JQ, Murphy SL. Deaths: Final data for 2005 National Vital Statistics Reports; vol. 56 no 10. Hyattsville, MD: National Center for Health Statistics; 2008. [PubMed] [Google Scholar]
- Los Angeles County Department of Public Health. Mortality in los angeles county 2003: Leading causes of death and premature death. [Retrieved May 15, 2008];2006 from http://lapublichealth.org/wwwfiles/ph/hae/dca/LA%20County%20Mortality%20Report%202003b.pdf. [Google Scholar]
- Los Angeles Homeless Services Authority. 2007 Greater Los Angeles Homeless County. Los Angeles: 2007. [Google Scholar]
- Maxwell S, Bigg D, Stanczykiewicz K, Carlberg-Racich S. Prescribing naloxone to actively injecting heroin users: A program to reduce heroin overdose deaths. Journal of Addictive Diseases. 2006;25(3):89–96. doi: 10.1300/J069v25n03_11. [DOI] [PubMed] [Google Scholar]
- New Mexico Department of Health. Department of health encourages people to seek medical help for overdose - NM first state in nation to pass 911 good samaritan law. [Retrieved May 15, 2008];2007 from http://www.health.state.nm.us/pdf/harmreduction.pdf. [Google Scholar]
- New Mexico Department of Health. State provides nasal spray to reverse drug overdoses. [Retrieved May 15, 2008];2008 from http://www.health.state.nm.us/pdf/narcan.pdf. [Google Scholar]
- Piper TM, Rudenstine S, Stancliff S, Sherman SG, Nandi VV, Clear A, et al. Overdose prevention for injection drug users: Lessons learned from naloxone training and distribution programs in New York City. Harm Reduction Journal. 2007;25(4) doi: 10.1186/1477-7517-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollini RA, McCall L, Mehta SH, Celentano DD, Vlahov D, Strathdee SA. Response to overdose among injection drug users. American Journal of Preventive Medicine. 2006;31(3):261–264. doi: 10.1016/j.amepre.2006.04.002. [DOI] [PubMed] [Google Scholar]
- SAMHSA Office of Applied Studies. Dawn series d-27. Rockville, md.: 2005. Drug Abuse Warning Network, 2003: Area profiles of drug-related mortality. DHHS publication no. (sma) 05–4023. [Google Scholar]
- Seal KH, Downing M, Kral AH, Singleton-Banks S, Hammond JP, Lorvick J, et al. Attitudes about prescribing take-home naloxone to injection drug users for the management of heroin overdose: A survey of street-recruited injectors in the san francisco bay area. Journal of Urban Health. 2003;80(2):291–301. doi: 10.1093/jurban/jtg032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Thawley R, Gee L, Bamberger J, Kral AH, Ciccarone D, et al. Naloxone distribution and cardiopulmonary resuscitation training for injection drug users to prevent heroin overdose death: A pilot intervention study. Journal of Urban Health. 2005;82(2):303–311. doi: 10.1093/jurban/jti053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman S, Gann D, Scott G, Carlberg S, Bigg D, Heimer R. A qualitative study of overdose responses among Chicago IDUs. Harm Reduction Journal. 2008;5(1):2. doi: 10.1186/1477-7517-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sporer KA. Acute heroin overdose. Annals of Internal Medicine. 1999;130(7):584–590. doi: 10.7326/0003-4819-130-7-199904060-00019. [DOI] [PubMed] [Google Scholar]
- Sporer KA. Strategies for preventing heroin overdose. BMJ: British Medical Journal. 2003;326(7386):442–444. doi: 10.1136/bmj.326.7386.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sporer KA, Kral AH. Prescription naloxone: A novel approach to heroin overdose prevention. Annals of Emergency Medicine. 2007;49(2):172–177. doi: 10.1016/j.annemergmed.2006.05.025. [DOI] [PubMed] [Google Scholar]
- Strang J, Best D, Man L, Noble A, Gossop M. Peer-initiated overdose resuscitation: Fellow drug users could be mobilised to implement resuscitation. International Journal of Drug Policy. 2000;11(6):437–445. doi: 10.1016/s0955-3959(00)00070-0. [DOI] [PubMed] [Google Scholar]
- Strang J, Manning V, Mayet S, Best D, Titherington E, Santana L, et al. Overdose training and take-home naloxone for opiate users: Prospective cohort study of impact on knowledge and attitudes and subssequent management of overdoses. Addiction. 2008;103:1648–1657. doi: 10.1111/j.1360-0443.2008.02314.x. [DOI] [PubMed] [Google Scholar]
- Strang J, Powis B, Best D, Vingoe L, Griffiths P, Taylor C, et al. Preventing opiate overdose fatalities with take-home naloxone: Pre-launch study of possible impact and acceptability. Addiction. 1999;94(2):199–204. doi: 10.1046/j.1360-0443.1999.9421993.x. [DOI] [PubMed] [Google Scholar]
- Tobin KE, Davey MA, Latkin CA. Calling emergency medical services during drug overdose: An examination of individual, social and setting correlates. Addiction. 2005;100(3):397–404. doi: 10.1111/j.1360-0443.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- Tobin KE, Sherman SG, Beilenson P, Welsh C, Latkin CA. Evaluation of the Staying Alive programme: Training injection drug users to properly administer naloxone and save lives. International Journal of Drug Policy. 2008 doi: 10.1016/j.drugpo.2008.03.002. [DOI] [PubMed] [Google Scholar]
- White JM, Irvine RJ. Mechanisms of fatal opioid overdose. Addiction. 1999;94(7):961–972. [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi MY, Sannerud C. CPDD taskforce on prescrption opioid non-medical use & abuse: Position statement. Drug & Alcohol Dependence. 2003;69(3):215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]