Abstract
The impact of nutrition on brain development in preterm infants has been increasingly appreciated. Early postnatal growth and nutrient intake have been demonstrated to influence brain growth and maturation with subsequent effects on neurodevelopment that persist into childhood and adolescence. Nutrition could also potentially protect against injury. Inflammation and perinatal infection play a crucial role in the pathogenesis of white matter injury, the most common pattern of brain injury in preterm infants. Therefore, nutritional components with immunomodulatory and/or anti-inflammatory effects may serve as neuroprotective agents. Moreover, growing evidence supports the existence of a microbiome-gut-brain axis. The microbiome is thought to interact with the brain through immunological, endocrine, and neural pathways. Consequently, nutritional components that may influence gut microbiota may also exert beneficial effects on the developing brain. Based on these properties, probiotics, prebiotic oligosaccharides, and certain amino acids are potential candidates for neuroprotection. In addition, the amino acid glutamine has been associated with a decrease in infectious morbidity in preterm infants. In conclusion, early postnatal nutrition is of major importance for brain growth and maturation. Additionally, certain nutritional components might play a neuroprotective role against white matter injury, through modulation of inflammation and infection, and may influence the microbiome-gut-brain axis.
The importance of optimal early nutrition, that provides adequate energy and protein intake to preterm infants, has been stressed for years. Historically, emphasis has been placed on the impact of early nutrition on growth and little attention has been drawn to its implications for brain development. In recent years, there has been a growing literature supporting the latter postulate. The aim of this review is to summarize the literature on the influence of early postnatal nutrition on brain development following extremely and very preterm birth. First, we will discuss normal brain development in the preterm period and the most important patterns of brain injury. We will explore pathways through which nutrition may modulate brain development and how nutritional strategies may exert neuroprotective effects. Furthermore, we will discuss nutritional interventions that may serve as neuroprotective agents in the preterm brain, either based on clinical evidence or on theoretical grounds.
Brain Development and Patterns of Injury Following Preterm Birth
During the late second and third trimester of pregnancy, important processes of brain growth and maturation take place. Both white and gray matter structures undergo a dramatic increase in volume, with the cerebellum and cortical gray matter exhibiting the highest growth rates (1,2). As the brain matures, cortical folding progresses and gyrification becomes increasingly more complex with advancing gestational age (3). Moreover, this phase is characterized by an abundance of rapidly developing axons, glial cells, oligodendrocytes, and neurons in the white matter. Between 24–40 wk of gestation, pre-oligodendroglial progenitors differentiate to mature myelin-producing oligodendrocytes, axons develop and form connections, and neurons proliferate and migrate to the cerebral cortex and deep nuclear grey matter structures (4). Extremely preterm infants are thus exposed to extra-uterine life in a period of critical brain development, especially of white matter structures, that render them particularly susceptible to injury. Consequently, white matter injury (WMI) is the most common pattern of brain injury following preterm birth (4,5). WMI can either result from periventricular leucomalacia (PVL) or from intraventricular hemorrhage (IVH) and subsequent periventricular hemorrhagic infarction (PVHI), although the latter two only account for a small proportion of white matter lesions in modern neonatal medicine (4,5). The incidence of cystic PVL, the most severe type of WMI, has also substantially declined over the past decades (6). Today, the occurrence of more diffuse WMI remains a major problem for preterm infants (5). Diffuse WMI is nowadays considered a dynamic disease process rather than a non-progressive lesion, that is characterized by primary injury leading to secondary maturational disturbances, in line with the concept of “encephalopathy of prematurity” as suggested by Volpe (4). WMI is associated with disruptions of cortico-thalamic connections and volume changes in the overlying cortex and underlying deep gray matter structures, reflecting axonal deficits and myelination failure (4,7). Cerebellar injury is the final common pattern of brain injury of prematurity, albeit less prevalent and merely restricted to the most immature infants (8). Cerebellar hemorrhage often coincides with IVH and PVHI. In addition, the cerebellum is known to be affected by supratentorial lesions, especially WMI and IVH, which has been postulated to be the result of impaired trophic support and exposure to noxious stimuli in the cerebrospinal fluid (9).
Brain injury is an important cause of neurodevelopmental impairments that manifest following preterm birth. Cystic PVL and PVHI are associated with cerebral palsy, epilepsy, major cognitive disability, and visual impairments later in life (5,10), whereas milder motor deficits, cognitive and behavioral problems are the dominant sequelae of IVH and cerebellar injury (11,12). Yet, most preterm children display a range of mild to moderate cognitive, attentional, behavioral, and social-emotional problems that have been attributed to diffuse WMI with consecutive maturational disturbances in brain development (4,5). Hence, there is an urgent need for neuroprotective strategies to improve outcomes in these children. Several pharmacological agents, such as melatonin, N-acetylcysteine, erythropoietin (EPO), and topiramate, have been proposed as potential candidates for neuroprotection, but medicinal products fall beyond the scope of this review (13). In this review, we will focus on possible nutritional interventions.
Early Nutrition and Brain Development in Preterm Infants
In animal models, malnutrition during a vulnerable period of brain development leads to a reduction in brain cells, myelin production, and number of synapses, in addition to alterations in neurotransmitter systems. The cerebellum and hippocampus have demonstrated a particular vulnerability to the effects of early postnatal undernutrition (14). Although some effects on brain structure and metabolism are reversible by nutritional rehabilitation, others persist, with subsequent effects on behavior and cognitive functioning (14,15). These findings can at least in part be extrapolated to human development, as research on fetal malnutrition has demonstrated long-lasting consequences for mental development and psychiatric health (16,17). Prenatal exposure to undernutrition has been associated with cognitive impairments, learning disabilities, and schizophrenia. Yet, biological effects are dependent on timing and duration of malnourishment (17). Early postnatal nutritional deficits may impede brain growth and maturation. Postnatal growth impairment in preterm infants has been related to decreased microstructural development of the cerebral cortex as measured by fractional anisotropy (FA) using diffusion tensor imaging (DTI). When the cortical gray matter matures with increasing postnatal age, radial glia disappear and the complexity of connections increases. This results in a decrease in FA, reflecting microstructural maturation of the cortex. Delayed cortical maturation associated with postnatal growth restriction could, at least in part, be the result of inadequate nutritional support (18).
Several papers have reported on the impact of early nutrition on postnatal head growth and later neurodevelopment in preterm infants (19,20,21,22,23,24,25,26). Optimizing protein and energy intake and balance in the neonatal period primarily influences cognition, with effects persisting until adolescence (22,23,27). Only a few studies have evaluated the influence of nutrition on brain volumes and neurodevelopmental outcome, and yielded inconsistent results (26,28,29,30). In a large British randomized controlled trial (RCT), preterm boys that had received a high nutrient preterm formula (containing larger amounts of macronutrients, vitamins, and trace elements, such as zinc, iodine, and calcium) in the first 4 wk of life, showed significantly larger caudate nucleus volumes at 16 y of age, compared with preterm boys that had been on a standard term formula diet (30). Both at 5–8 y and at 16 y of life, preterm children in the high nutrient group demonstrated a significantly higher verbal intelligence quotient (VIQ). Again, the highest impact of nutrition was seen in preterm males, with a 12 points higher VIQ at 7.5–8 y of age in boys that had been fed the high nutrient diet (23). Another RCT failed to demonstrate any beneficial effect of a nutritionally enriched feeding regimen, which consisted of parenteral and/or enteral nutrition containing 20% more macronutrients than a standard preterm diet, on brain volumes at term equivalent age (TEA) and neurodevelopmental outcome at 3 and 9 mo of age. Yet, when data from both study arms were pooled, energy deficiency was significantly related to smaller total brain volume and lower mental and psychomotor development scores (26). In contrast, a Swedish prospective cohort study did not find any correlation between protein- and energy intake and brain volumes at TEA or neurodevelopmental outcome at 2 y corrected age. However, in this study, a positive correlation was found between insulin-like growth factor-1 (IGF-1) and each of cerebellar, gray matter, unmyelinated white matter volume, and total brain volume as well as mental development. The authors reasoned that nutritional intake alone might not be sufficient to alter postnatal growth restriction associated with impaired brain growth (28,29). Thus far, no other papers have been published on the impact of nutrition on brain volumes during the neonatal period, and most studies have focused on the relationship between postnatal nutrition and head growth as measured by occipitofrontal circumference (OFC). Head growth is a surrogate measure of brain growth and their correlation can be quantified using magnetic resonance imaging (MRI) (31). Nevertheless, OFC does not provide any information on the potential vulnerability of specific brain tissues to inadequate nutrition. Hence, to date it is unclear whether improved head growth because of optimized feeding regimens reflects global brain growth or whether it may be attributed to a selective increase in volume and maturation of certain brain structures that undergo more rapid changes in growth and development in the preterm period and may therefore be more sensitive to the effects of early nutrition.
In addition to nutrition as a composite, several clinical trials have evaluated the effect of supplementation with specific nutritional components on brain development and/or neurodevelopmental outcome in preterm infants. Examples are long-chain polyunsaturated fatty acids (LCPUFA), vitamin A, iron, and iodine and although a few studies have demonstrated some benefits, meta-analyses of trial data have not provided convincing evidence for supplementation with specific nutrients to improve developmental outcomes (32,33,34,35). Nevertheless, results from a large iodine supplementation trial are yet to be received (36). In all these studies, nutritional components were supplemented to serve as building blocks for growth and development, because preterm infants are at increased risk of deficiencies of specific nutrients. Nutrition may also provide intrinsic benefits to the developing brain. The pathways through which nutrition may modulate brain development will be discussed in the next section.
White Matter Injury and Nutrition
In their study, of preterm infants with white matter disease and term infants with neonatal encephalopathy, Dabydeen et al. revealed a dramatic impact of a high energy and protein diet during the first year after birth. Infants in the intervention group had significantly improved head growth, weight gain and increased axonal diameters in their corticospinal tracts. Because of these benefits, the trial was terminated early and, unfortunately, no neurodevelopmental outcome parameters were evaluated (37). This study illustrates how nutrition can favorably modify brain development following serious injury. If a nutritional intervention could inhibit the pathways leading to injury, it may be able to attenuate brain damage. This is particularly interesting for WMI. Here, we will briefly discuss the pathogenesis of WMI in order to offer a better understanding of how nutrition may modulate brain development.
The main pathogenetic mechanisms of WMI are considered to be inflammation and ischemia. They frequently coincide and potentiate each other (4,13). Both inflammation and ischemia initiate the three leading events in the causative chain of WMI, i.e., activation of microglia, free radical attack and excitotoxicity. The primary insult leads to degeneration of pre-oligodendrocytes (pre-OLs), the most abundant cell population in the white matter during the preterm period. Subsequently, the depletion in the OL precursor pool is counteracted by a significant increase in the progenitor OL lineage cells. These pre-OLs however fail to differentiate into mature myelinating OLs and, as a consequence, hypomyelination occurs. Moreover, pre-OLs are particularly vulnerable to recurrent ischemic injury (4,13).
Perinatal infection has been recognized as an important risk factor for WMI and disturbances in brain development in preterm infants (38,39). Recently, infection has been related to abnormal early white matter maturation as measured by FA (38,40). Neonatal infection leads to systemic inflammation and is often associated with hemodynamic instability, resulting in reduced cerebral blood flow due to impaired cerebrovascular auto regulation. This subsequently potentiates the two major components of the pathophysiology of WMI, i.e., inflammation and ischemia. Importantly, bacterial sepsis has been demonstrated to activate toll-like receptors that are present on the surface of microglia in the white matter. Activation of microglia leads to a release of free radicals and pro-inflammatory cytokines, that ultimately results in injury to the developing pre-OLs, axons, and neurons in the white matter (13). Thus, nutritional supplements that would reduce systemic infections and attenuate the inflammatory response may be able to alleviate WMI and thereby promote brain development. Immunomodulation may also offer benefits to the developing brain through the microbiome-gut-brain axis, which will be discussed into more detail below.
Microbiome-Gut-Brain Axis
The reciprocal interaction between the gut and the brain has long been recognized. In recent years, accumulating evidence has suggested the importance of the gut microbiome in this bidirectional communication system and as a result, the concept of the microbiome-gut-brain axis has emerged. The term “gut microbiome” is used to describe the complex ecosystem of bacteria that colonize the gut, including their genes, proteins, and metabolites (41). The exact mechanisms by which the gut microbiome communicates with the brain are not yet clear, but include immunological, endocrine, and neural pathways. It has long been known that the interaction between intestinal microbes and the immune system are necessary for development and regulation of immune function, but it was not until recently that research has established the importance of the gut microbiota for normal brain function (42). Animal studies have demonstrated reduced anxiety-like behavior in germ-free mice compared with controls. These altered behavioral responses were accompanied by alterations in concentrations of neurotransmitters and expression of neurotrophic factors in the brain (43,44). An exciting finding was, that reconstitution of normal gut microbiota early in life normalized behavioral patterns and neuroregulationin mice, whereas such an effect could not be established in adulthood (43). These results suggest the ability of the gut microbiome to modulate brain development and behavior and propose a critical window for intestinal microbes to influence developmental programming of long-lasting brain function.
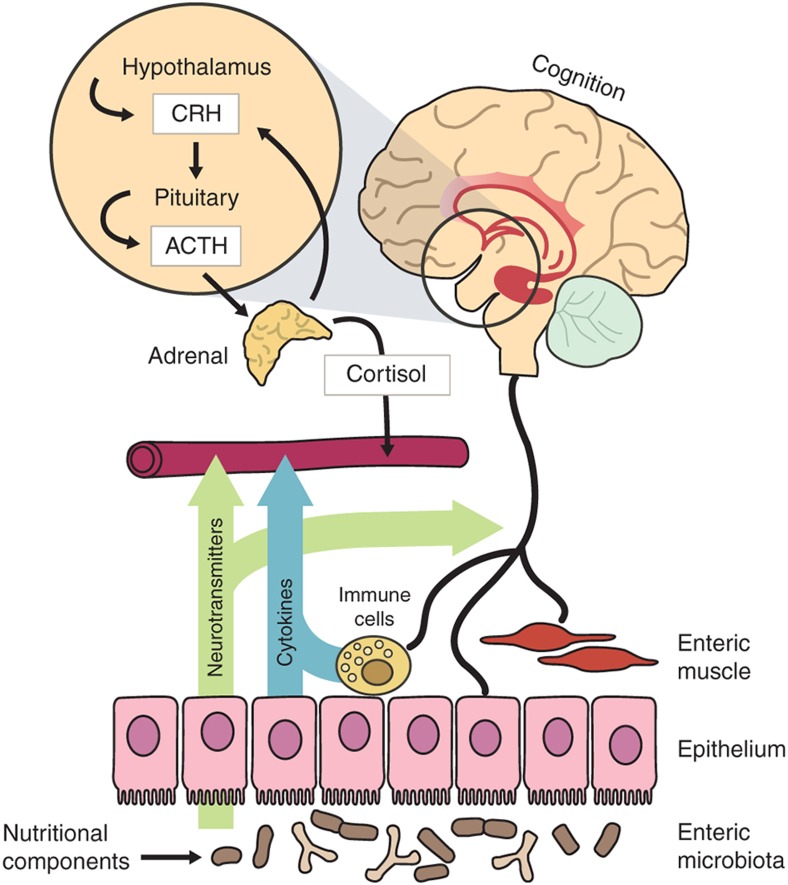
Although research has not yet addressed how the gut microbiome may modulate brain development, immune signaling is likely to play a key role. This hypothesis is supported by a mounting body of evidence showing that the immune system has an important effect on brain development (45,46). Immune cells, cytokines, and chemokines have been postulated to mediate the mechanisms through which the gut microbiome may interact with the brain. Cytokine receptors have been revealed on neurons and glial cells in the brain (46). In addition, many immune-related signaling molecules have been demonstrated to regulate processes in the brain and vice versa (45). Hence, the close interrelation between these complex organ systems is increasingly appreciated. The microbiome-gut-brain axis is shown in Figure 1.
Figure 1.
The reciprocal interaction between gut microbiota and the brain. Gut microbiota may modulate brain function and development through immune signaling (e.g., pro- and anti-inflammatory cytokines, chemokines, and immune cells), endocrine, and neural pathways. Conversely, the brain may influence the gut through neurotransmitters that impact on immune function, and through alterations in cortisol levels, intestinal motility, and permeability. Nutritional components may exert effects on each of these communication pathways. ACTH, adrenocorticotropic hormone; CRH, corticotropin-releasing hormone.
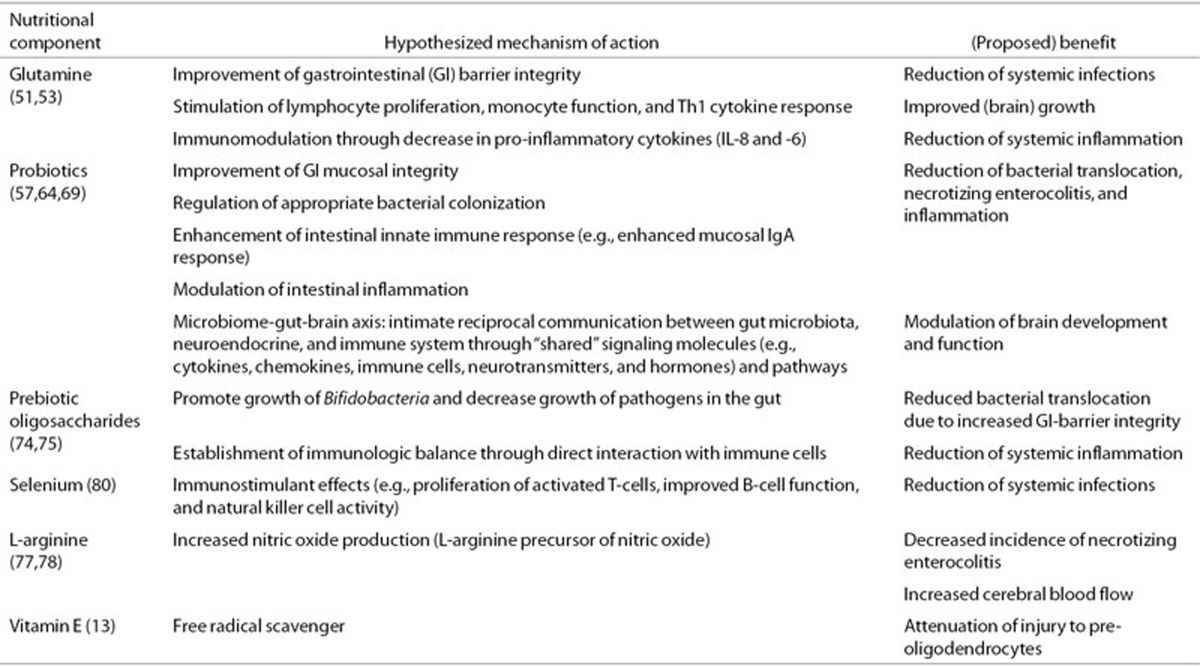
In light of the interesting concept of the microbiome-gut-brain axis, the gut microbiome now constitutes an interesting target for potential neuroprotective strategies. In the next section, we will explore nutritional supplements that may serve as neuroprotective agents. Their postulated mechanisms and benefits are outlined in Table 1.
Table 1. Nutritional components and their postulated benefits and mechanisms of action.
Nutrition as a Potential Neuroprotective Agent
Glutamine
To our knowledge, only one study has previously evaluated the impact of a nutritional intervention on microstructural brain development in preterm infants. In a randomized controlled trial (GEEF study), very preterm infants with a gestational age <32 wk or birth weight<1,500 g received either enteral glutamine supplementation from day 3 after birth until postnatal day 30, or an isonitrogenous placebo supplement (alanine). During long-term follow-up, the investigators found a tendency towards higher FA values in the cingulum bundles projecting into the hippocampus in the glutamine group compared to controls at 8 y of age. Higher FA of these white matter bundles indicates greater microstructural integrity, because of increased water diffusion in the direction of the tract. In addition, children in the glutamine group manifested larger white matter, hippocampus, and brain stem volumes than controls. All differences were either strongly associated with or completely mediated by a lower incidence of serious neonatal infections (47). However, the improvements in brain development observed in this study did not translate into better functional outcomes at 24 mo corrected age (48). Similarly, at 8 y of age, cognitive functioning, motor performance and behavioral outcomes did not significantly differ between preterm children that had been supplemented with glutamine and children that had received a control supplement, although an 8-point difference in IQ was found in favor of the glutamine group (49). The sample size in both follow-up studies was small and may have been underpowered to yield significant results. Hence, the potential benefits of early enteral glutamine supplementation on brain development and subsequent neurodevelopmental outcome remain to be further elucidated. In addition, the mechanism through which enteral glutamine supplementation reduces the risk of serious neonatal infections in preterm infants is yet to be unraveled.
One of the pathways may be that glutamine improves gut integrity and attenuates bacterial translocation, which may result in less systemic infections, thereby leading to a reduction in white matter injury (WMI) (50). A meta-analysis of five randomized controlled trials showed a significantly lower incidence of invasive infections in preterm infants who had received glutamine-supplemented enteral nutrition compared to controls (51). In addition, glutamine may offer direct benefits to the developing white matter. In experimental studies, glutamine has been shown to reduce systemic inflammation and the production of pro-inflammatory cytokines, thereby putatively exerting a direct neuroprotective effect (52,53). Furthermore, glutamine may improve the infant's nutritional status by improving gut integrity, which may lead to better growth and may consequently promote white matter development and brain growth. Some clinical trials have indeed demonstrated increased weight gain, length and head growth in glutamine-supplemented preterm infants, although others were not able to confirm these findings (51).
Future research investigating the effects of glutamine supplementation on brain development and neurodevelopmental outcomes in preterm infants needs to be considered and should particularly focus on the incidence of WMI. Yet, caution should be taken when designing such studies. Glutamate is the key excitatory neurotransmitter in the brain, but can be lethal to neurons and oligodendrocytes in case of excessive excitation, which is known as “excitotoxicity” (54). Unlike glutamate, glutamine is not toxic to the brain, but in in vitro models of hypoxia-ischemia, injured neurons have been described to release glutaminase, the enzyme that converts glutamine to glutamate, thereby leading to secondary elevations of glutamate concentrations (55). The clinical relevance of these findings for the preterm population is however unclear, as relevant experimental or human autopsy data are lacking. Importantly, in the GEEF study, amino acid concentrations were measured at different time points, and both glutamine and glutamate concentrations were never elevated in the glutamine group compared with the control group (56). Moreover, none of the clinical studies on glutamine supplementation in preterm infants have reported an increase in PVL in the intervention group, although neonatal MRI/DTI (for accurate assessment of more subtle WMI) was not included in any of these studies (51).
Probiotics
Another group of nutritional supplements that may be of interest as potential neuroprotective agents for preterm infants are probiotics. Probiotics are micro-organisms that colonize the gut and provide health benefits to the host through improved gut mucosal barrier integrity, regulation of appropriate bacterial colonization, enhanced mucosal IgA response, and immunomodulation, leading to an increase in anti-inflammatory cytokines and a decrease in pro-inflammatory cytokines (57). In the past decade, probiotic supplementation in preterm infants has been extensively studied and has proved to reduce the risk of necrotizing enterocolitis (NEC) (relative risk (RR) 0.35; 95% confidence interval (CI) = 0.24.52; and all-cause mortality (RR = 0.40; 95% CI = 0.27–0.60). There is no evidence of a reduction in the incidence of postnatal infections. Based on these results, the Cochrane Neonatal Review Group (CNRG) suggests a change in clinical practice towards routine use of probiotics in preterm infants <1,500 g. An exception is reserved for ELBW infants, because more studies are needed to assess the specific efficacy and safety in this high-risk population (58). Supplementation with probiotics has been adopted in routine clinical practice in many level III neonatal intensive care units (NICUs) across the globe, including Finland, Japan, Columbia, Denmark, Italy, Germany, New Zealand, and Australia. Despite widespread routine use, serious adverse events such as probiotic-induced sepsis have only sporadically been reported (59,60,61,62), indicating the safety of probiotic supplementation (63).
Probiotics may be of benefit to the developing preterm brain, because of a favorable alteration of the immune response, resulting in less inflammation, which may subsequently attenuate WMI. In addition, they may be able to exert beneficial effects through the microbiome-gut-brain axis (64). Probiotic administration modifies gut microbiota composition and may subsequently induce changes in signaling pathways from the gut to the brain, which may ultimately modulate brain development (64). A probiotic mixture of Lactobacillus helveticus and Bifidobacterium longum induced beneficial psychological effects and decreased serum cortisol levels in healthy adult volunteers, while the same combination of probiotics resulted in reduced anxiety-like behavior in rodents (65). In mice experiments, several behavioral effects have been ascribed to certain probiotic strains, as well as alterations in neurotransmitters, hormones, cytokines, and neurotrophic factors (66,67). The effects of some strains could not be replicated after vagotomy, indicating a crucial role for the vagus nerve in probiotic microbiome-gut-brain signaling (68). The ability of probiotics to modulate the microbiome-gut-brain axis has been demonstrated to be strain-specific, and care should be taken when translating results from one strain to another (69). Frequently investigated strains in preterm infants are Bifidobacterium bifidus, Bifidobacterium lactis, Bifidobacterium breve, Lactobacillus acidophilus, and Lactobacillus GG (58). Yet, studies addressing the question of whether administration of probiotics may improve brain development are lacking and reports on the impact of probiotics on neurodevelopment are scarce (70,71). To date, no beneficial effects on neurodevelopmental performance or reductions in major impairments, such as hearing loss, cerebral palsy, visual impairment, and mental retardation have been reported. The postulated benefits of probiotics for brain development in preterm infants deserve further investigation.
Prebiotic Oligosaccharides
Prebiotic oligosaccharides are another group of nutritional constituents that may provide benefits to the developing preterm brain. These indigestible food components naturally occur in breast milk (human milk oligosaccharides) and have been assigned antimicrobial, immunomodulatory, and anti-inflammatory functions (72). Prebiotic oligosaccharides have the potential to improve the infant's intestinal microbiota by promoting growth of Bifidobacteria, which may in turn reduce the burden of potentially pathogenic micro-organisms in the gut (73). The bifidogenic effect on the gut microbiota may support the immature immune system by establishing an immunologic balance (74). The immune-modulating capacity of prebiotic oligosaccharides might also be microbiota-independent through a direct interaction with immune cells (74). Despite these advantages, prebiotic oligosaccharide supplementation has not been demonstrated to reduce postnatal infections or NEC in preterm infants, although most studies were underpowered to yield statistically significant results (75). So far, no studies have been undertaken to evaluate the effect of prebiotic oligosaccharides on brain development. A mixture of pro- and prebiotics (often referred to as synbiotics) may be considered, as the combination is known to be synergistic, with prebiotics enhancing the survival of probiotic organisms in the host.
Other Nutritional Components
Other nutritional components that may be considered for neuroprotection are selenium, L-arginine, and vitamin E. Selenium supplementation has been demonstrated to reduce the incidence of sepsis in preterm infants in a meta-analysis of RCTs. However, results were mainly attributed to a large trial conducted in a selenium-deficient country and may therefore not be readily extrapolated to other populations. No studies have evaluated the impact of selenium on neurodevelopment (76). One trial was undertaken to investigate the effects of L-arginine and reported a reduction in NEC (77). However, no benefits for neurodevelopmental outcome were observed (78). Vitamin E has been shown to be an effective free radical scavenger in experimental studies and may thereby attenuate pre-OL injury (13). Yet, evidence from clinical studies is limited and some studies have shown an increase in serious neonatal infections (79). The clinical implications of vitamin E supplementation therefore remain unclear.
Conclusion
It is now generally accepted that adequate nutrition is crucial for brain growth and development of very preterm infants. In addition, nutritional supplements have been hypothesized to provide neuroprotective effects. Although nutrition may not be able to overcome all major deleterious effects of extreme prematurity and its consequences on brain development, nutritional therapies may offer benefits to the developing brain. Specific nutritional supplements have been shown to reduce the incidence of postnatal infections and NEC and have been assigned immunomodulatory properties. Improved immunological balance and subsequent decreased inflammation may attenuate WMI and may also exert beneficial effects on the developing brain through the gut-immune-brain axis. Nutritional interventions are of particular interest as neuroprotective strategies because they are considered safe, inexpensive, cause few side effects, and can be implemented rather easily. Moreover, nutritional supplements can be added to mother's milk and therefore combined with breastfeeding. Clinical research into the postulated benefits of nutritional supplements on brain development is urgently needed and should include MRI studies and long-term neurodevelopmental follow-up. Furthermore, future research should try to unravel the underlying mechanisms by which the gut and the gut microbiome communicate with the brain, with a particular focus on immunological pathways.
Disclosure
We disclose that one of the authors, R.M.v.E. has two affiliations. He is employed by the VU University Medical Center in Amsterdam as Associate Professor and by Danone Nutricia Research as Chief Scientific Officer. In addition, we disclose that the PhD position of the first author, K.K. is fully funded by a grant from the Dutch government (Ministry of Economic Affairs; the Province and Municipality of Utrecht, Utrecht University, and the University Medical Center Utrecht). This grant provides financial funding for a randomized controlled trial in which the authors will investigate the impact of a nutritional supplement.
Acknowledgments
We thank Liandre van der Merwe for English language editing.
References
- Clouchoux C, Guizard N, Evans AC, du Plessis AJ, Limperopoulos C. Normative fetal brain growth by quantitative in vivo magnetic resonance imaging. Am J Obstet Gynecol. 2012;206:173.e1–8. doi: 10.1016/j.ajog.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Hüppi PS, Warfield S, Kikinis R, et al. Quantitative magnetic resonance imaging of brain development in premature and mature newborns. Ann Neurol. 1998;43:224–35. doi: 10.1002/ana.410430213. [DOI] [PubMed] [Google Scholar]
- Dubois J, Benders M, Cachia A, et al. Mapping the early cortical folding process in the preterm newborn brain. Cereb Cortex. 2008;18:1444–54. doi: 10.1093/cercor/bhm180. [DOI] [PubMed] [Google Scholar]
- Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8:110–24. doi: 10.1016/S1474-4422(08)70294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpe JJ.Neurology of the Newborn5th ed. Philadelphia, PA; Elsevier; 2008 [Google Scholar]
- van Haastert IC, Groenendaal F, Uiterwaal CS, et al. Decreasing incidence and severity of cerebral palsy in prematurely born children. J Pediatr. 2011;159:86–91.e1. doi: 10.1016/j.jpeds.2010.12.053. [DOI] [PubMed] [Google Scholar]
- Ball G, Boardman JP, Aljabar P, et al. The influence of preterm birth on the developing thalamocortical connectome. Cortex. 2013;49:1711–21. doi: 10.1016/j.cortex.2012.07.006. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Benson CB, Bassan H, et al. Cerebellar hemorrhage in the preterm infant: ultrasonographic findings and risk factors. Pediatrics. 2005;116:717–24. doi: 10.1542/peds.2005-0556. [DOI] [PubMed] [Google Scholar]
- Volpe JJ. Cerebellum of the premature infant: rapidly developing, vulnerable, clinically important. J Child Neurol. 2009;24:1085–104. doi: 10.1177/0883073809338067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltirovska Salamon A, Groenendaal F, van Haastert IC, et al. Neuroimaging and neurodevelopmental outcome of preterm infants with a periventricular haemorrhagic infarction located in the temporal or frontal lobe. Dev Med Child Neurol. 2014;56:547–55. doi: 10.1111/dmcn.12393. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Bassan H, Gauvreau K, et al. Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors. Pediatrics. 2007;120:584–93. doi: 10.1542/peds.2007-1041. [DOI] [PubMed] [Google Scholar]
- Patra K, Wilson-Costello D, Taylor HG, Mercuri-Minich N, Hack M. Grades I-II intraventricular hemorrhage in extremely low birth weight infants: effects on neurodevelopment. J Pediatr. 2006;149:169–73. doi: 10.1016/j.jpeds.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Volpe JJ, Kinney HC, Jensen FE, Rosenberg PA. The developing oligodendrocyte: key cellular target in brain injury in the premature infant. Int J Dev Neurosci. 2011;29:423–40. doi: 10.1016/j.ijdevneu.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitsky DA, Strupp BJ. Malnutrition and the brain: changing concepts, changing concerns. J Nutr. 1995;125:Suppl 8:2212S–20S. doi: 10.1093/jn/125.suppl_8.2212S. [DOI] [PubMed] [Google Scholar]
- Penido AB, Rezende GH, Abreu RV, et al. Malnutrition during central nervous system growth and development impairs permanently the subcortical auditory pathway. Nutr Neurosci. 2012;15:31–6. doi: 10.1179/1476830511Y.0000000022. [DOI] [PubMed] [Google Scholar]
- Kerac M, Postels DG, Mallewa M, et al. The interaction of malnutrition and neurologic disability in Africa. Semin Pediatr Neurol. 2014;21:42–9. doi: 10.1016/j.spen.2014.01.003. [DOI] [PubMed] [Google Scholar]
- Roseboom TJ, Painter RC, van Abeelen AF, Veenendaal MV, de Rooij SR. Hungry in the womb: what are the consequences? Lessons from the Dutch famine. Maturitas. 2011;70:141–5. doi: 10.1016/j.maturitas.2011.06.017. [DOI] [PubMed] [Google Scholar]
- Vinall J, Grunau RE, Brant R, et al. Slower postnatal growth is associated with delayed cerebral cortical maturation in preterm newborns. Sci Transl Med. 2013;5:168ra8. doi: 10.1126/scitranslmed.3004666. [DOI] [PubMed] [Google Scholar]
- Cormack BE, Bloomfield FH. Increased protein intake decreases postnatal growth faltering in ELBW babies. Arch Dis Child Fetal Neonatal Ed. 2013;98:F399–404. doi: 10.1136/archdischild-2012-302868. [DOI] [PubMed] [Google Scholar]
- Dinerstein A, Nieto RM, Solana CL, Perez GP, Otheguy LE, Larguia AM. Early and aggressive nutritional strategy (parenteral and enteral) decreases postnatal growth failure in very low birth weight infants. J Perinatol. 2006;26:436–42. doi: 10.1038/sj.jp.7211539. [DOI] [PubMed] [Google Scholar]
- Ehrenkranz RA, Das A, Wrage LA, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network Early nutrition mediates the influence of severity of illness on extremely LBW infants. Pediatr Res. 2011;69:522–9. doi: 10.1203/PDR.0b013e318217f4f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz AR, Pohlandt F, Bode H, et al. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics. 2009;123:e101–9. doi: 10.1542/peds.2008-1352. [DOI] [PubMed] [Google Scholar]
- Lucas A, Morley R, Cole TJ. Randomised trial of early diet in preterm babies and later intelligence quotient. BMJ. 1998;317:1481–7. doi: 10.1136/bmj.317.7171.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan C, McGowan P, Herwitker S, Hart AE, Turner MA. Postnatal head growth in preterm infants: a randomized controlled parenteral nutrition study. Pediatrics. 2014;133:e120–8. doi: 10.1542/peds.2013-2207. [DOI] [PubMed] [Google Scholar]
- Stephens BE, Walden RV, Gargus RA, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009;123:1337–43. doi: 10.1542/peds.2008-0211. [DOI] [PubMed] [Google Scholar]
- Tan M, Abernethy L, Cooke R. Improving head growth in preterm infants–a randomised controlled trial II: MRI and developmental outcomes in the first year. Arch Dis Child Fetal Neonatal Ed. 2008;93:F342–6. doi: 10.1136/adc.2007.124255. [DOI] [PubMed] [Google Scholar]
- Isaacs EB, Morley R, Lucas A. Early diet and general cognitive outcome at adolescence in children born at or below 30 weeks gestation. J Pediatr. 2009;155:229–34. doi: 10.1016/j.jpeds.2009.02.030. [DOI] [PubMed] [Google Scholar]
- Hansen-Pupp I, Hövel H, Hellström A, et al. Postnatal decrease in circulating insulin-like growth factor-I and low brain volumes in very preterm infants. J Clin Endocrinol Metab. 2011;96:1129–35. doi: 10.1210/jc.2010-2440. [DOI] [PubMed] [Google Scholar]
- Hansen-Pupp I, Hövel H, Löfqvist C, et al. Circulatory insulin-like growth factor-I and brain volumes in relation to neurodevelopmental outcome in very preterm infants. Pediatr Res. 2013;74:564–9. doi: 10.1038/pr.2013.135. [DOI] [PubMed] [Google Scholar]
- Isaacs EB, Gadian DG, Sabatini S, et al. The effect of early human diet on caudate volumes and IQ. Pediatr Res. 2008;63:308–14. doi: 10.1203/PDR.0b013e318163a271. [DOI] [PubMed] [Google Scholar]
- Cheong JL, Hunt RW, Anderson PJ, et al. Head growth in preterm infants: correlation with magnetic resonance imaging and neurodevelopmental outcome. Pediatrics. 2008;121:e1534–40. doi: 10.1542/peds.2007-2671. [DOI] [PubMed] [Google Scholar]
- Darlow BA, Graham PJ. Vitamin A supplementation to prevent mortality and short- and long-term morbidity in very low birthweight infants. Cochrane Database Syst Rev. 2011;10:CD000501. doi: 10.1002/14651858.CD000501.pub3. [DOI] [PubMed] [Google Scholar]
- Ibrahim M, Sinn J, McGuire W. Iodine supplementation for the prevention of mortality and adverse neurodevelopmental outcomes in preterm infants. Cochrane Database Syst Rev. 2006;2:CD005253. doi: 10.1002/14651858.CD005253.pub2. [DOI] [PubMed] [Google Scholar]
- Mills RJ, Davies MW. Enteral iron supplementation in preterm and low birth weight infants. Cochrane Database Syst Rev. 2012;3:CD005095. doi: 10.1002/14651858.CD005095.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulzke SM, Patole SK, Simmer K. Long-chain polyunsaturated fatty acid supplementation in preterm infants. Cochrane Database Syst Rev. 2011;2:CD000375. doi: 10.1002/14651858.CD000375.pub4. [DOI] [PubMed] [Google Scholar]
- Williams F, Hume R, Ogston S, Brocklehurst P, Morgan K, Juszczak E. I2S2 team A summary of the iodine supplementation study protocol (I2S2): a UK multicentre randomised controlled trial in preterm infants. Neonatology. 2014;105:282–9. doi: 10.1159/000358247. [DOI] [PubMed] [Google Scholar]
- Dabydeen L, Thomas JE, Aston TJ, Hartley H, Sinha SK, Eyre JA. High-energy and -protein diet increases brain and corticospinal tract growth in term and preterm infants after perinatal brain injury. Pediatrics. 2008;121:148–56. doi: 10.1542/peds.2007-1267. [DOI] [PubMed] [Google Scholar]
- Chau V, Brant R, Poskitt KJ, Tam EW, Synnes A, Miller SP. Postnatal infection is associated with widespread abnormalities of brain development in premature newborns. Pediatr Res. 2012;71:274–9. doi: 10.1038/pr.2011.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah DK, Doyle LW, Anderson PJ, et al. Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J Pediatr. 2008;153:170–5, 175.e1. doi: 10.1016/j.jpeds.2008.02.033. [DOI] [PubMed] [Google Scholar]
- Adams E, Chau V, Poskitt KJ, Grunau RE, Synnes A, Miller SP. Tractography-based quantitation of corticospinal tract development in premature newborns. J Pediatr. 2010;156:882–8, 888.e1. doi: 10.1016/j.jpeds.2009.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korecka A, Arulampalam V. The gut microbiome: scourge, sentinel or spectator. J Oral Microbiol. 2012;4:9367–81. doi: 10.3402/jom.v4i0.9367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov II, Littman DR. Modulation of immune homeostasis by commensal bacteria. Curr Opin Microbiol. 2011;14:106–14. doi: 10.1016/j.mib.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz Heijtz R, Wang S, Anuar F, et al. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci USA. 2011;108:3047–52. doi: 10.1073/pnas.1010529108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neufeld KM, Kang N, Bienenstock J, Foster JA. Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol Motil. 2011;23:255–64, e119. doi: 10.1111/j.1365-2982.2010.01620.x. [DOI] [PubMed] [Google Scholar]
- Boulanger LM. Immune proteins in brain development and synaptic plasticity. Neuron. 2009;64:93–109. doi: 10.1016/j.neuron.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Deverman BE, Patterson PH. Cytokines and CNS development. Neuron. 2009;64:61–78. doi: 10.1016/j.neuron.2009.09.002. [DOI] [PubMed] [Google Scholar]
- de Kieviet JF, Oosterlaan J, Vermeulen RJ, Pouwels PJ, Lafeber HN, van Elburg RM. Effects of glutamine on brain development in very preterm children at school age. Pediatrics. 2012;130:e1121–7. doi: 10.1542/peds.2012-0928. [DOI] [PubMed] [Google Scholar]
- van Zwol A, van den Berg A, Huisman J, et al. Neurodevelopmental outcomes of very low-birth-weight infants after enteral glutamine supplementation in the neonatal period. Acta Paediatr. 2008;97:562–7. doi: 10.1111/j.1651-2227.2008.00719.x. [DOI] [PubMed] [Google Scholar]
- de Kieviet JF, Oosterlaan J, van Zwol A, Boehm G, Lafeber HN, van Elburg RM. Effects of neonatal enteral glutamine supplementation on cognitive, motor and behavioural outcomes in very preterm and/or very low birth weight children at school age. Br J Nutr. 2012;108:2215–20. doi: 10.1017/S0007114512000293. [DOI] [PubMed] [Google Scholar]
- Wang WW, Qiao SY, Li DF. Amino acids and gut function. Amino Acids. 2009;37:105–10. doi: 10.1007/s00726-008-0152-4. [DOI] [PubMed] [Google Scholar]
- Moe-Byrne T, Wagner JV, McGuire W. Glutamine supplementation to prevent morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2012;3:CD001457. doi: 10.1002/14651858.CD001457.pub4. [DOI] [PubMed] [Google Scholar]
- Arndt H, Kullmann F, Reuss F, Schölmerich J, Palitzsch KD. Glutamine attenuates leukocyte-endothelial cell adhesion in indomethacin-induced intestinal inflammation in the rat. JPEN J Parenter Enteral Nutr. 1999;23:12–8. doi: 10.1177/014860719902300112. [DOI] [PubMed] [Google Scholar]
- Coëffier M, Marion R, Leplingard A, Lerebours E, Ducrotté P, Déchelotte P. Glutamine decreases interleukin-8 and interleukin-6 but not nitric oxide and prostaglandins e(2) production by human gut in-vitro. Cytokine. 2002;18:92–7. doi: 10.1006/cyto.2002.1027. [DOI] [PubMed] [Google Scholar]
- Bakiri Y, Burzomato V, Frugier G, Hamilton NB, Káradóttir R, Attwell D. Glutamatergic signaling in the brain's white matter. Neuroscience. 2009;158:266–74. doi: 10.1016/j.neuroscience.2008.01.015. [DOI] [PubMed] [Google Scholar]
- Newcomb R, Sun X, Taylor L, Curthoys N, Giffard RG. Increased production of extracellular glutamate by the mitochondrial glutaminase following neuronal death. J Biol Chem. 1997;272:11276–82. doi: 10.1074/jbc.272.17.11276. [DOI] [PubMed] [Google Scholar]
- van den Berg A, van Elburg RM, Teerlink T, Lafeber HN, Twisk JW, Fetter WP. A randomized controlled trial of enteral glutamine supplementation in very low birth weight infants: plasma amino acid concentrations. J Pediatr Gastroenterol Nutr. 2005;41:66–71. doi: 10.1097/01.mpg.0000167497.55321.65. [DOI] [PubMed] [Google Scholar]
- Martin CR, Walker WA. Probiotics: role in pathophysiology and prevention in necrotizing enterocolitis. Semin Perinatol. 2008;32:127–37. doi: 10.1053/j.semperi.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Alfaleh K, Anabrees J, Bassler D, Al-Kharfi T. Probiotics for prevention of necrotizing enterocolitis in preterm infants. Cochrane Database Syst Rev. 2011;3:CD005496. doi: 10.1002/14651858.CD005496.pub3. [DOI] [PubMed] [Google Scholar]
- Jenke A, Ruf EM, Hoppe T, Heldmann M, Wirth S. Bifidobacterium septicaemia in an extremely low-birthweight infant under probiotic therapy. Arch Dis Child Fetal Neonatal Ed. 2012;97:F217–8. doi: 10.1136/archdischild-2011-300838. [DOI] [PubMed] [Google Scholar]
- Kunz AN, Noel JM, Fairchok MP. Two cases of Lactobacillus bacteremia during probiotic treatment of short gut syndrome. J Pediatr Gastroenterol Nutr. 2004;38:457–8. doi: 10.1097/00005176-200404000-00017. [DOI] [PubMed] [Google Scholar]
- Ohishi A, Takahashi S, Ito Y, et al. Bifidobacterium septicemia associated with postoperative probiotic therapy in a neonate with omphalocele. J Pediatr. 2010;156:679–81. doi: 10.1016/j.jpeds.2009.11.041. [DOI] [PubMed] [Google Scholar]
- Thompson C, McCarter YS, Krause PJ, Herson VC. Lactobacillus acidophilus sepsis in a neonate. J Perinatol. 2001;21:258–60. doi: 10.1038/sj.jp.7200509. [DOI] [PubMed] [Google Scholar]
- Luoto R, Isolauri E, Lehtonen L. Safety of Lactobacillus GG probiotic in infants with very low birth weight: twelve years of experience. Clin Infect Dis. 2010;50:1327–8. doi: 10.1086/651694. [DOI] [PubMed] [Google Scholar]
- Al-Asmakh M, Anuar F, Zadjali F, Rafter J, Pettersson S. Gut microbial communities modulating brain development and function. Gut Microbes. 2012;3:366–73. doi: 10.4161/gmic.21287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messaoudi M, Lalonde R, Violle N, et al. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br J Nutr. 2011;105:755–64. doi: 10.1017/S0007114510004319. [DOI] [PubMed] [Google Scholar]
- Bercik P, Denou E, Collins J, et al. The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology. 2011;141:599–609, 609.e1–3. doi: 10.1053/j.gastro.2011.04.052. [DOI] [PubMed] [Google Scholar]
- Desbonnet L, Garrett L, Clarke G, Kiely B, Cryan JF, Dinan TG. Effects of the probiotic Bifidobacterium infantis in the maternal separation model of depression. Neuroscience. 2010;170:1179–88. doi: 10.1016/j.neuroscience.2010.08.005. [DOI] [PubMed] [Google Scholar]
- Bercik P, Park AJ, Sinclair D, et al. The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut-brain communication. Neurogastroenterol Motil. 2011;23:1132–9. doi: 10.1111/j.1365-2982.2011.01796.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cryan JF, O'Mahony SM. The microbiome-gut-brain axis: from bowel to behavior. Neurogastroenterol Motil. 2011;23:187–92. doi: 10.1111/j.1365-2982.2010.01664.x. [DOI] [PubMed] [Google Scholar]
- Chou IC, Kuo HT, Chang JS, et al. Lack of effects of oral probiotics on growth and neurodevelopmental outcomes in preterm very low birth weight infants. J Pediatr. 2010;156:393–6. doi: 10.1016/j.jpeds.2009.09.051. [DOI] [PubMed] [Google Scholar]
- Romeo MG, Romeo DM, Trovato L, et al. Role of probiotics in the prevention of the enteric colonization by Candida in preterm newborns: incidence of late-onset sepsis and neurological outcome. J Perinatol. 2011;31:63–9. doi: 10.1038/jp.2010.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bode L. Recent advances on structure, metabolism, and function of human milk oligosaccharides. J Nutr. 2006;136:2127–30. doi: 10.1093/jn/136.8.2127. [DOI] [PubMed] [Google Scholar]
- Kapiki A, Costalos C, Oikonomidou C, Triantafyllidou A, Loukatou E, Pertrohilou V. The effect of a fructo-oligosaccharide supplemented formula on gut flora of preterm infants. Early Hum Dev. 2007;83:335–9. doi: 10.1016/j.earlhumdev.2006.07.003. [DOI] [PubMed] [Google Scholar]
- Jeurink PV, van Esch BC, Rijnierse A, Garssen J, Knippels LM. Mechanisms underlying immune effects of dietary oligosaccharides. Am J Clin Nutr. 2013;98:572S–7S. doi: 10.3945/ajcn.112.038596. [DOI] [PubMed] [Google Scholar]
- Srinivasjois R, Rao S, Patole S. Prebiotic supplementation in preterm neonates: updated systematic review and meta-analysis of randomised controlled trials. Clin Nutr. 2013;32:958–65. doi: 10.1016/j.clnu.2013.05.009. [DOI] [PubMed] [Google Scholar]
- Darlow BA, Austin NC. Selenium supplementation to prevent short-term morbidity in preterm neonates. Cochrane Database Syst Rev. 2003. p. CD003312. [DOI] [PMC free article] [PubMed]
- Amin HJ, Zamora SA, McMillan DD, et al. Arginine supplementation prevents necrotizing enterocolitis in the premature infant. J Pediatr. 2002;140:425–31. doi: 10.1067/mpd.2002.123289. [DOI] [PubMed] [Google Scholar]
- Amin HJ, Soraisham AS, Sauve RS. Neurodevelopmental outcomes of premature infants treated with l-arginine for prevention of necrotising enterocolitis. J Paediatr Child Health. 2009;45:219–23. doi: 10.1111/j.1440-1754.2008.01458.x. [DOI] [PubMed] [Google Scholar]
- Johnson L, Bowen FW, Jr, Abbasi S, et al. Relationship of prolonged pharmacologic serum levels of vitamin E to incidence of sepsis and necrotizing enterocolitis in infants with birth weight 1,500 grams or less. Pediatrics. 1985;75:619–38. [PubMed] [Google Scholar]
- Rayman MP. Selenium and human health. Lancet. 2012;379:1256–68. doi: 10.1016/S0140-6736(11)61452-9. [DOI] [PubMed] [Google Scholar]