Abstract
A number of circulating and imaging biomarkers are robustly associated with cardiovascular (CV) risk. The overall expectation from a biomarker in the erectile dysfunction (ED) setting is to enhance the optimal management of a man with this disorder but no clinical atherosclerosis. Evidence demonstrating that these biomarkers enhance risk prediction for individuals with ED is at this stage still limited for most of them. A better identification of the subsets of the ED population that require further risk stratification, as well as the initiation of randomized trials that will formally test the ability of biomarkers to predict CV risk, could make biomarker-guided prevention an attainable goal.
Keywords: biomarkers, erectile dysfunction, risk prediction
BIOMARKERS FOR PREDICTION OF CARDIOVASCULAR DISEASE WITHIN ERECTILE DYSFUNCTION
Although scoring systems for cardiovascular (CV) risk prediction are valuable in the assessment of asymptomatic individuals, differences between predicted and actual events do exist.1 In theory, the addition of further variables to current risk-scoring systems should improve our ability to predict CV disease (CVD) risk.2 However, candidate biomarkers, apart from proving an incremental predictive value over and above traditional risk factors, they must fulfill stringent criteria in order to be integrated into clinical practice; these include calibration, discrimination, and reclassification.3,4 Of these, reclassification is the most important. Reclassification assesses the proportion of individuals reclassified correctly (either moving to a higher or to a lower risk category) by the addition of a new biomarker.
From the pathophysiological standpoint, vasculogenic erectile dysfunction (ED) may result from impairment of endothelial dependent and/or independent smooth muscle relaxation (i.e. functional vascular ED, early stages), occlusion of the penile arteries by atherosclerosis (i.e. structural vascular ED, late stages), or a combination of these processes.5 Vasculogenic (or primarily vasculogenic) ED is increasingly being regarded as the early clinical manifestation of a generalized vascular disease and carries an independent risk for future CV events.6,7,8 However, even within ED, there are subgroups of patients with a further increased risk of future cardiac events that require further CV risk assessment.9 Thus, it is vital to determine biomarkers that can assist to identify patients at higher CV risk and predict CV events. The use of biomarkers may be particularly useful in assessing CV risk in younger ED patients whose risk may be underestimated by global risk assessments such as the European SCORE or the Framingham risk score.9 The biomarkers of generalized vascular disease discussed below are such candidates and based on their predictive ability in various populations, they are expected to be predictive of CV events in ED patients. Few, however, have proven their predictive ability within ED.
Finally, although not strictly in the sense of biomarkers, the role of unconventional risk factors should be stressed. Indeed, while we generally pertain to ED patients with organic risk factors, unconventional risk factors shown to be associated with incidence of major adverse CV events, such as depression, low education, and reported partner's hypoactive sexual desire10,11 should be part of the assessment.
Hormonal testing
Hormonal testing, as principally represented by testosterone levels, has been shown to be an independent predictor of CVD risk and primarily, CV mortality. Indeed, testosterone deficiency, which is frequent in aged males with risk factors, such as arterial hypertension or diabetes, is implicated in the common pathogenetic pathways of vasculogenic ED and CVD.12 There is a significant inverse association between low testosterone levels and CVD risk and CV mortality,13 while, seen from a different perspective, there is a protective link between higher endogenous testosterone levels and fatal and nonfatal CV events as it was reported in a prospective study in males aged 61–80 years.14 In a recent study, in hypertensive individuals without clinical atherosclerosis, we showed that this marker reclassifies correctly a considerable percentage of patients to a higher or lower risk category.15 In men with ED, total testosterone levels below 8 nmol l−1 was associated with increased chance of fatal major adverse cardiac events (MACE).16 Men with lower levels of testosterone also face a higher risk of having subclinical organ damage, such as left ventricular hypertrophy,17 increased aortic stiffness,18 carotid atherosclerosis,19 and low ankle-brachial index (ABI).20 The measurement of prolactin may be also useful for CVD prediction within ED population since it has been shown that for each 10 ng ml−1 increment of prolactin levels in men without pathological hyperprolactinemia (prolactin < 735 mU l−1 or 35 ng ml−1) the risk for MACE is decreased by 5%.21
Penile peak systolic velocity
The measurement of peak systolic velocity (PSV) using a dynamic penile Doppler ultrasound (with intracavernous injection of alprostadil) alone represents a reliable marker for detecting penile vascular damage and diagnosis of vasculogenic ED in patients with CV risk factors because it strongly correlates with functional erection.22 Interestingly, assessment of both flaccid and dynamic PSV (flaccid PSV <13 cm s−1 and dynamic PSV <25 cm s−1) in penile Doppler is a prognostic marker for incident major CV events, suggesting the possible implementation of biomarkers of penile vascular disease in prediction of CVD. It has been shown that risk of CAD increases by 5% for each decrement of 5 cm s−1 in the dynamic PSV.23 Furthermore, two recently reported Doppler parameters, such as impaired response to prostaglandin E (PGE) intracavernous injection test24 and flaccid penile acceleration25 (a parameter that reflects PSV, the systolic rise time and end diastolic velocity, measurable without using PGE injection) have been associated with adverse CV events.
Aortic stiffness
In recent years, great emphasis has been placed on the role of aortic stiffness in the development of CVD and this biomarker is increasingly used in the clinical assessment of patients. Evidence to date suggests that aortic stiffness fulfills the criteria for a marker of vascular aging.26 Measurement of carotid-femoral pulse wave velocity (PWV) provides a comprehensive noninvasive assessment of aortic stiffness. PWV is an important predictor of future CV events and all-cause mortality both in the general population and in patients with disease states.27 The ability of aortic stiffness to predict future CV events in ED patients without established CVD has been recently investigated.28 Increased aortic PWV predicts independently major adverse CV events in long-term follow-up (Figure 1). This predictive ability was independent of classic risk that is often present in such patients. Addition of PWV to a multivariate model including classical risk factors (age, smoking, diabetes, systolic blood pressure, total cholesterol, high-density lipoprotein) offered a statistically significant improvement in the resulting C-statistic indicating the ability of PWV for CV events discrimination beyond the classical risk factors. Most importantly, addition of PWV to standard risk factors model yielded correct patient reclassification to higher or lower risk category by a considerable percentage of patients (27.6%). Finally, in a previous study by Corona et al.29 peripheral pulse pressure, a crude index of arterial stiffness, was also shown to predict outcome in ED patients.
Figure 1.
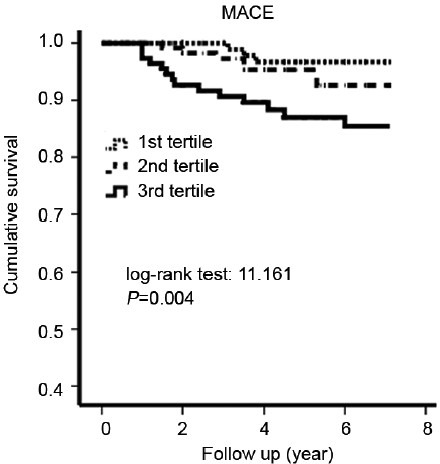
Kaplan–Meier curves for major adverse cardiovascular events by tertile group of carotid–femoral pulse wave velocity (PWV) in 344 erectile dysfunction patients (mean age 56 years) without established cardiovascular disease. Cut-offs of the tertiles for PWV were 7.6 and 8.8 m s−1. With permission from Vlachopoulos et al.28
Carotid intima media thickness and plaques
A number of longitudinal studies assessing different populations have examined the relationship between carotid intima media thickness (cIMT) and future events, most frequently the incidence of cardiac events (myocardial infarction, angina pectoris, coronary intervention) and cerebrovascular events (stroke or transient ischemic attack).30,31 Measurement of cIMT has been included in the recommendations for the evaluation of CV risk of a patient.32 However, the ability of this biomarker to improve risk prediction has been recently challenged.33,34 Nevertheless, although the predictive value of cIMT has not been at this stage evaluated in men with ED, measurement of this biomarker can be recommended for the assessment of intermediate-risk ED patients.35,36
Ankle-brachial index
Ankle-brachial index, the ratio of blood pressure in the dorsalis pedis artery to that in the brachial artery is widely used to detect peripheral artery disease (PAD).37 A low ABI, besides signaling advanced atherosclerosis, predicts future CV events. Specifically, it has been associated with approximately twice the 10 years CV mortality and major coronary event rate compared with the overall rate in each Framingham category.37 ABI is recommended in ED patients to identify individuals with PAD.35,37 While the measurement of ABI appears to be useful specifically in intermediate risk patients,36 data regarding the ability of ABI to predict CV events within ED are scarce.
Microalbuminuria
Microalbuminuria as determined by albumin/creatinine ratio 3.4–34 mg mmol−1 and albumin excretion ratio 30–300 mg day−1 is an easily measured noncirculating marker of microvascular injury. In both diabetic and nondiabetic hypertensive patients, microalbuminuria, even below the threshold values usually considered, has been shown to predict CV events.38 A study in a population of diabetic ED patients with angiographically proven CAD, in whom hypertension was highly prevalent, reported a significant association of microalbuminuria with CV events.39
Calcium score
Coronary artery calcification is a surrogate marker for atherosclerosis, with the calcium score (CACS) being proportional to atherosclerotic plaque burden and CVD risk.40 More recently, in a comparison of the ability of six risk markers (CACS, cIMT, ABI, brachial flow-mediated dilation, high-sensitivity C-reactive protein, and family history of CAD) in intermediate risk individuals (Framingham 10 years risk, 5%–20%) enrolled in the Multi-Ethnic Study of Atherosclerosis, CACS provided superior improvements in risk estimation versus the other risk markers.41 The measurement of calcified atherosclerotic plaques in coronary arteries by CACS is associated with ED presence and severity.42,43 However, there are no data within ED population to evaluate measurement of CACS for prediction of CVD.
Other circulating and noncirculating markers
A wide range of other circulating and noncirculating biomarkers has been studied for their ability to predict risk of future CV events. Although not specific for ED, it might be reasonable to measure biomarkers that have been proposed for the intermediate risk patient such as C-reactive protein, uric acid, glycated hemoglobin, and lipoprotein-associated phospholipase A2.35,36
MARKERS FOR THE ERECTILE DYSFUNCTION PATIENT - WHICH ONE?
Table 1 offers a critical evaluation of biomarkers as regards the ability to predict CVD risk within ED. Grading of biomarkers is continuously changing as studies accumulate, and hence, the title of this review points out the evolving nature of the field. Figure 2 is a suggested flow chart for the assessment and management of patients with ED and no known CVD. Patients without established CVD should be evaluated for their risk of future events according to risk scores (e.g. European SCORE or Framingham). Determination of exercise ability and stress testing is crucial to the assessment. The measurement of biomarkers should be part of the overall evaluation in low or intermediate risk ED patients. Testosterone, due to its double role as both a diagnostic tool and a biomarker, is a first line test in all men with a diagnosis of organic ED. PWV has established a potent role by fulfilling criteria of risk prediction such as reclassification.28 Despite not fulfilling all criteria, ABI and microalbuminuria are considered first line biomarkers due to their ease of use, applicability and cost. cIMT is moved to the second line group of tests due to the recent challenge of its predictive ability in intermediate risk patients. Coronary artery calcium is categorized in the same group of tests; despite its potent predictive ability, exposure to radiation should be carefully weighed.
Table 1.
Prognostic value availability, response to treatment, and cost of biomarkers in men with ED (scored from 0 to 4+)a
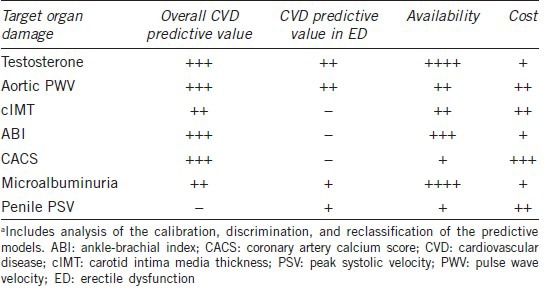
Figure 2.
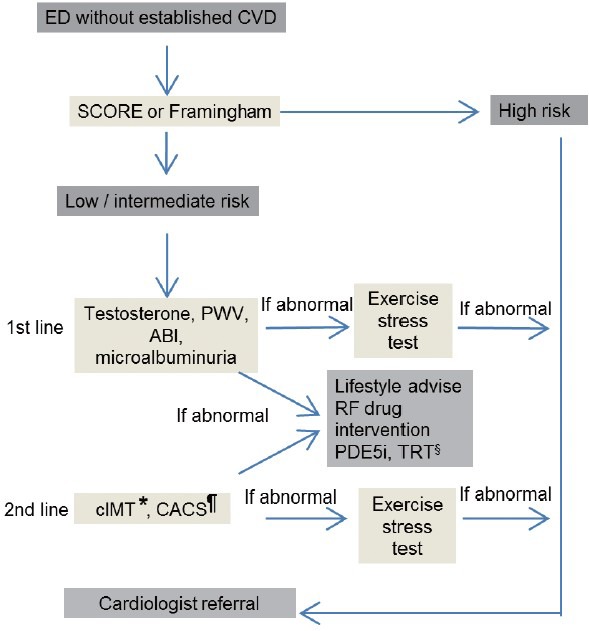
Cardiovascular risk assessment in men with vasculogenic ED and not established CVD. All patients should be evaluated for their risk of future events according to risk scores (SCORE or Framingham). Testosterone, PWV, ABI, and microalbuminuria should be used as first line tools to further characterize cardiovascular risk in men with low or intermediate risk. Additional markers such as IMT, CACS will depend on levels of first line biomarkers, availability, and institutional practice. *Although cIMT shows a significant potential to be implemented in clinical practice, further evidence is needed before such implementation can occur and further studies are needed to elaborate on the ability of this marker to reclassify, discriminate, and calibrate the risk of ED patients. ¶CACS has a potent predictive ability recently shown; however, exposure to radiation should be carefully weighed. §Where appropriate. ABI: ankle-brachial index; CACS: coronary artery calcium scoring; CAD: coronary artery disease; CCTA: coronary computed tomography angiography; cIMT: carotid intima-media thickness; CVD: cardiovascular disease; ED: erectile dysfunction; PDE5i: phosphodiesterase type 5 inhibitors; PWV: pulse wave velocity; TRT: testosterone replacement therapy.
Patients with adequate exercise ability or a negative stress test can initiate or resume sexual activity and begin treatment for ED. In patients with a positive stress test or in high-risk patients, sexual activity should be deferred until the cardiac condition has been treated and stabilized. In all cases, patient follow-up and reassessment of exercise ability and biomarkers are recommended.
CONCLUSIONS
Testosterone and biomarkers of generalized vascular disease may help to further quantify CV risk specifically in intermediate risk ED patients even though most of them do not fulfill the criteria to adequately predict CV risk in this specific population. Although the emerging status of biomarkers provides an excellent illustration of how application of basic and clinical science of vasculogenic ED can advance clinical care, we still need to do better. Nevertheless, the clinical use of biomarkers has the ability to provide the clinician with a tool to gauge residual risk and chart a course for optimal management of the ED patient. It is yet to be proven whether multiple biomarkers could be combined to improve performance for prediction of CV risk in these patients.
REFERENCES
- 1.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 2.Vasan RS. Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation. 2006;113:2335–62. doi: 10.1161/CIRCULATIONAHA.104.482570. [DOI] [PubMed] [Google Scholar]
- 3.Wang TJ. Assessing the role of circulating, genetic, and imaging biomarkers in cardiovascular risk prediction. Circulation. 2011;123:551–65. doi: 10.1161/CIRCULATIONAHA.109.912568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–16. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vlachopoulos C, Ioakeimidis N, Terentes-Printzios D, Stefanadis C. The triad: erectile dysfunction – endothelial dysfunction – cardiovascular disease. Curr Pharm Des. 2008;14:3700–14. doi: 10.2174/138161208786898716. [DOI] [PubMed] [Google Scholar]
- 6.Vlachopoulos C, Jackson G, Stefanadis C, Montorsi P. Erectile dysfunction in the cardiovascular patient. Eur Heart J. 2013;34:2034–46. doi: 10.1093/eurheartj/eht112. [DOI] [PubMed] [Google Scholar]
- 7.Jackson G, Boon N, Eardley I, Kirby M, Dean J, et al. Erectile dysfunction and coronary artery disease prediction: evidence-based guidance and consensus. Int J Clin Pract. 2010;64:848–57. doi: 10.1111/j.1742-1241.2010.02410.x. [DOI] [PubMed] [Google Scholar]
- 8.Vlachopoulos CV, Terentes-Printzios DG, Ioakeimidis NK, Aznaouridis KA, Stefanadis CI. Prediction of cardiovascular events and all-cause mortality with erectile dysfunction: a systematic review and meta-analysis of cohort studies. Circ Cardiovasc Qual Outcomes. 2013;6:99–109. doi: 10.1161/CIRCOUTCOMES.112.966903. [DOI] [PubMed] [Google Scholar]
- 9.Miner M, Seftel AD, Nehra A, Ganz P, Kloner RA, et al. Prognostic utility of erectile dysfunction for cardiovascular disease in younger men and those with diabetes. Am Heart J. 2012;164:21–8. doi: 10.1016/j.ahj.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Fisher AD, Bandini E, Rastrelli G, Corona G, Monami M, et al. Sexual and cardiovascular correlates of male unfaithfulness. J Sex Med. 2012;9:1508–18. doi: 10.1111/j.1743-6109.2012.02722.x. [DOI] [PubMed] [Google Scholar]
- 11.Rastrelli G, Corona G, Fisher AD, Silverii A, Mannucci E, et al. Two unconventional risk factors for major adverse cardiovascular events in subjects with sexual dysfunction: low education and reported partner's hypoactive sexual desire in comparison with conventional risk factors. J Sex Med. 2012;9:3227–38. doi: 10.1111/j.1743-6109.2012.02947.x. [DOI] [PubMed] [Google Scholar]
- 12.Jones TH, Saad F. The effects of testosterone on risk factors for, and the mediators of, the atherosclerotic process. Atherosclerosis. 2009;207:318–27. doi: 10.1016/j.atherosclerosis.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Corona G, Rastrelli G, Monami M, Guay A, Buvat J, et al. Hypogonadism as a risk factor for cardiovascular mortality in men: a meta-analytic study. Eur J Endocrinol. 2011;165:687–701. doi: 10.1530/EJE-11-0447. [DOI] [PubMed] [Google Scholar]
- 14.Ohlsson C, Barrett-Connor E, Bhasin S, Orwoll E, Labrie F, et al. High serum testosterone is associated with reduced risk of cardiovascular events in elderly men. The MrOS (Osteoporotic Fractures in Men) study in Sweden. J Am Coll Cardiol. 2011;58:1674–81. doi: 10.1016/j.jacc.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 15.Vlachopoulos C, Ioakeimidis N, Terentes-Printzios D, Aznaouridis K, Rokkas K, et al. Plasma total testosterone and incident cardiovascular events in hypertensive patients. Am J Hypertens. 2013;26:373–81. doi: 10.1093/ajh/hps056. [DOI] [PubMed] [Google Scholar]
- 16.Corona G, Monami M, Boddi V, Cameron-Smith M, Fisher AD, et al. Low testosterone is associated with an increased risk of MACE lethality in subjects with erectile dysfunction. J Sex Med. 2010;7:1557–64. doi: 10.1111/j.1743-6109.2009.01690.x. [DOI] [PubMed] [Google Scholar]
- 17.Svartberg J, von Mühlen D, Schirmer H, Barrett-Connor E, Sundfjord J, et al. Association of endogenous testosterone with blood pressure and left ventricular mass in men. The Tromsø Study. Eur J Endocrinol. 2004;150:65–71. doi: 10.1530/eje.0.1500065. [DOI] [PubMed] [Google Scholar]
- 18.Vlachopoulos C, Ioakeimidis N, Miner M, Aggelis A, Pietri P, et al. Testosterone deficiency: a determinant of aortic stiffness in men. Atherosclerosis. 2014;233:278–83. doi: 10.1016/j.atherosclerosis.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Muller M, van den Beld AW, Bots ML, Grobbee DE, Lamberts SW, et al. Endogenous sex hormones and progression of carotid atherosclerosis in elderly men. Circulation. 2004;109:2074–9. doi: 10.1161/01.CIR.0000125854.51637.06. [DOI] [PubMed] [Google Scholar]
- 20.Tivesten A, Mellström D, Jutberger H, Fagerberg B, Lernfelt B, et al. Low serum testosterone and high serum estradiol associate with lower extremity peripheral arterial disease in elderly men. The MrOS Study in Sweden. J Am Coll Cardiol. 2007;50:1070–6. doi: 10.1016/j.jacc.2007.04.088. [DOI] [PubMed] [Google Scholar]
- 21.Corona G, Rastrelli G, Boddi V, Monami M, Melani C, et al. Prolactin levels independently predict major cardiovascular events in patients with erectile dysfunction. Int J Androl. 2011;34:217–24. doi: 10.1111/j.1365-2605.2010.01076.x. [DOI] [PubMed] [Google Scholar]
- 22.Aversa A, Sarteschi LM. The role of penile color-duplex ultrasound for the evaluation of erectile dysfunction. J Sex Med. 2007;4:1437–47. doi: 10.1111/j.1743-6109.2007.00546.x. [DOI] [PubMed] [Google Scholar]
- 23.Corona G, Monami M, Boddi V, Cameron-Smith M, Lotti F, et al. Male sexuality and cardiovascular risk. A cohort study in patients with erectile dysfunction. J Sex Med. 2010;7:1918–27. doi: 10.1111/j.1743-6109.2010.01744.x. [DOI] [PubMed] [Google Scholar]
- 24.Rastrelli G, Corona G, Monami M, Melani C, Balzi D, et al. Poor response to alprostadil ICI test is associated with arteriogenic erectile dysfunction and higher risk of major adverse cardiovascular events. J Sex Med. 2011;8:3433–45. doi: 10.1111/j.1743-6109.2011.02474.x. [DOI] [PubMed] [Google Scholar]
- 25.Rastrelli G, Corona G, Lotti F, Aversa A, Bartolini M, et al. Flaccid penile acceleration as a marker of cardiovascular risk in men without classical risk factors. J Sex Med. 2014;11:173–86. doi: 10.1111/jsm.12342. [DOI] [PubMed] [Google Scholar]
- 26.Vlachopoulos C, Aznaouridis K, Stefanadis C. Aortic stiffness for cardiovascular risk prediction: just measure it, just do it ! J Am Coll Cardiol. 2014;63:647–9. doi: 10.1016/j.jacc.2013.10.040. [DOI] [PubMed] [Google Scholar]
- 27.Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–27. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 28.Vlachopoulos C, Ioakeimidis N, Aznaouridis K, Terentes-Printzios D, Rokkas K, et al. Prediction of cardiovascular events with aortic stiffness in patients with erectile dysfunction. Hypertension. 2014;64:672–8. doi: 10.1161/HYPERTENSIONAHA.114.03369. [DOI] [PubMed] [Google Scholar]
- 29.Corona G, Monami M, Boddi V, Rastrelli G, Melani C, et al. Pulse pressure independently predicts major cardiovascular events in younger but not in older subjects with erectile dysfunction. J Sex Med. 2011;8:247–54. doi: 10.1111/j.1743-6109.2010.01966.x. [DOI] [PubMed] [Google Scholar]
- 30.Lorenz MW, Schaefer C, Steinmetz H, Sitzer M. Is carotid intima media thickness useful for individual prediction of cardiovascular risk. Ten-year results from the Carotid Atherosclerosis Progression Study (CAPS)? Eur Heart J. 2010;31:2041–8. doi: 10.1093/eurheartj/ehq189. [DOI] [PubMed] [Google Scholar]
- 31.Nambi V, Chambless L, Folsom AR, He M, Hu Y, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk in Communities) study. J Am Coll Cardiol. 2010;55:1600–7. doi: 10.1016/j.jacc.2009.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 33.Den Ruijter HM, Peters SA, Anderson TJ, Britton AR, Dekker JM, et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA. 2012;308:796–803. doi: 10.1001/jama.2012.9630. [DOI] [PubMed] [Google Scholar]
- 34.Bots ML, Groenewegen KA, Anderson TJ, Britton AR, Dekker JM, et al. Common carotid intima-media thickness measurements do not improve cardiovascular risk prediction in individuals with elevated blood pressure: the USE-IMT collaboration. Hypertension. 2014;63:1173–81. doi: 10.1161/HYPERTENSIONAHA.113.02683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122:2748–64. doi: 10.1161/CIR.0b013e3182051bab. [DOI] [PubMed] [Google Scholar]
- 36.Nehra A, Jackson G, Miner M, Billups KL, Burnett AL, et al. The Princeton III Consensus recommendations for the management of erectile dysfunction and cardiovascular disease. Mayo Clin Proc. 2012;87:766–78. doi: 10.1016/j.mayocp.2012.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ankle Brachial Index Collaboration. Fowkes FG, Murray GD, Butcher I, Heald CL, et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perkovic V, Verdon C, Ninomiya T, Barzi F, Cass A, et al. The relationship between proteinuria and coronary risk: a systematic review and meta-analysis. PLoS Med. 2008;5:e207. doi: 10.1371/journal.pmed.0050207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gazzaruso C, Solerte SB, Pujia A, Coppola A, Vezzoli M, et al. Erectile dysfunction as a predictor of cardiovascular events and death in diabetic patients with angiographically proven asymptomatic coronary artery disease: a potential protective role for statins and 5-phosphodiesterase inhibitors. J Am Coll Cardiol. 2008;51:2040–4. doi: 10.1016/j.jacc.2007.10.069. [DOI] [PubMed] [Google Scholar]
- 40.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): the Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) Atherosclerosis. 2012;223:1–68. doi: 10.1016/j.atherosclerosis.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 41.Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–95. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chiurlia E, D’Amico R, Ratti C, Granata AR, Romagnoli R, et al. Subclinical coronary artery atherosclerosis in patients with erectile dysfunction. J Am Coll Cardiol. 2005;46:1503–6. doi: 10.1016/j.jacc.2005.06.068. [DOI] [PubMed] [Google Scholar]
- 43.Jackson G. Erectile dysfunction and asymptomatic coronary artery disease: frequently detected by computed tomography coronary angiography but not by exercise electrocardiography. Int J Clin Pract. 2013;67:1159–62. doi: 10.1111/ijcp.12275. [DOI] [PubMed] [Google Scholar]


