Abstract
Patients with cardiovascular disease and their partners expect health care providers to provide sexual counseling to assist them in maintaining sexual quality of life. Evidence suggests however, that there is a gap in integrating evidence into practice and that relatively few cardiac patients receive sexual counseling. This can result in negative psychological, physical, and quality of life outcomes for couples who may needlessly decide sexual activity is too risky and cease all sexual activity. Two scientific statements now exist that provide ample guidance to health care providers in discussing this important topic. Using a team approach that includes physicians, nurses, physical therapists, rehabilitation staff, and others is important to ensure that sexual counseling occurs throughout recovery. In addition, several trials using interventional approaches for sexual counseling provide insight into successful approaches for sexual counseling in practice. This article provides practical strategies and evidence-based approaches for assessment and sexual counseling for all cardiac patients and their partners, and specific counseling for those with ischemic conditions, heart failure, and implanted devices.
Keywords: cardiovascular diseases, health care providers, rehabilitation, sexual behavior, sexual counseling, sexual dysfunction, physiological, sexual dysfunction, psychological, sexual partners
WHY SEXUAL COUNSELING?
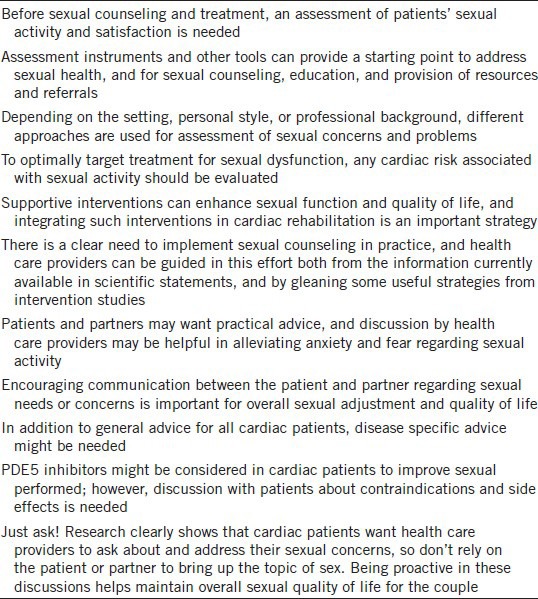
Sexual counseling is an activity that health care providers may be hesitant to address; but, it is important in maintaining both overall and sexual quality of life for many couples. There is ample research that illustrates that patients and their partners are in need of sexual counseling and expect health care providers to both initiate the topic and provide counseling about sexual activity and cardiovascular disease (CVD).1,2,3 The responsibility for counseling includes physicians, nurses, physical therapists, rehabilitation staff and others; thus, health care providers must be informed regarding how to address sexual issues and the content to be discussed. Two recent scientific statements provide guidance to address common questions of when to resume sexual activity, the safety of sexual activity, assessment, and specific counseling by cardiac diagnosis.1,4,5,6,7 This article will provide essential information for health care providers to initiate sexual counseling in practice, and is applicable to both men and women with CVD (Table 1).
Table 1.
Key points
What is sexual counseling?
Sexual counseling is recognized as an important aspect of care by the World Health Organization and efforts are in progress to better understand the elements, implementation, and outcomes for sexual counseling as delivered by health care providers.8 Most recently, it has been defined as “an interaction with patients that includes information on sexual concerns and safe return to sexual activity, as well as assessment, support, and specific advice related to psychological and sexual problems, also referred to as psychosexual counseling” (p. 2).1 This definition underscores the importance of health care providers taking an active role in sexual assessment and counseling. In addition, such interactions are not a one-time event, and sexual assessment and counseling should be ongoing and in a variety of settings. Using a multidisciplinary approach can ensure that sexual counseling is fully integrated into care.
SEXUAL ASSESSMENT
Before beginning treatment and counseling, an assessment of patients’ sexual activity and satisfaction is needed.1,9,10,11
How to assess sexual concerns/problems
With sexual assessment in cardiac patients, it is important to get a complete description of the nature of the problem, underlying causes, and perceptions, such as thoughts, beliefs and misconceptions that patients and partners have about the problem or the underlying course. In addition to cardiac specific causes and possible adverse effects of cardiac medication, other underlying conditions that contribute to sexual dysfunction should be assessed, as well as adverse effects of cardiovascular and noncardiovascular medications.1,12 Other questions can be posed to gain insight of underlying reasons or consequences of sexual problems such as, any medical comorbidities that may be contributing to sexual dysfunction, complicating factors such as on-going ischemia or active nitrate use, whether the patient is a candidate for treatment of erectile dysfunction (ED), and/or should this patient be referred to a specialist.12,13
When conducting a sexual assessment, it is important to consider the needs and concerns of the couple as a dyad, as partners may have heightened concerns about triggering a myocardial infarction (MI) or adverse event with sexual activity. Partners may exhibit higher level of concern than the patient. In addition, the need for support and information might vary between the patient and partner, perhaps necessitating different approaches to address sexual concerns.1 Few studies have examined the needs of partners; however, some literature suggests that those patients who have experienced MI or/and implanted cardioverter defibrillator (ICD) results in considerable concerns by partners.11
General assessment questions
An open discussion during a clinic or office visit regarding the patient and partner's sexual concerns can help determine the direction of treatment and counseling.13 There may be a need for information concerning sexuality in several domains, for example in relation to the relationship and symptoms.14,15,16 Some patients might want to know more about medications and psychological factors. Open-ended questions tend to facilitate discussion, for example, “What concerns do you have about resuming sexual activity with your heart failure (HF)” or “Many people have concerns about resuming sexual activity after a heart attack. What concerns do you have?”11,17 The response to such an open-ended question may allow the health care provider to get a sense of which sexual counseling topics might need to be discussed and how open patients are to such discussions.
Strategies for assessment
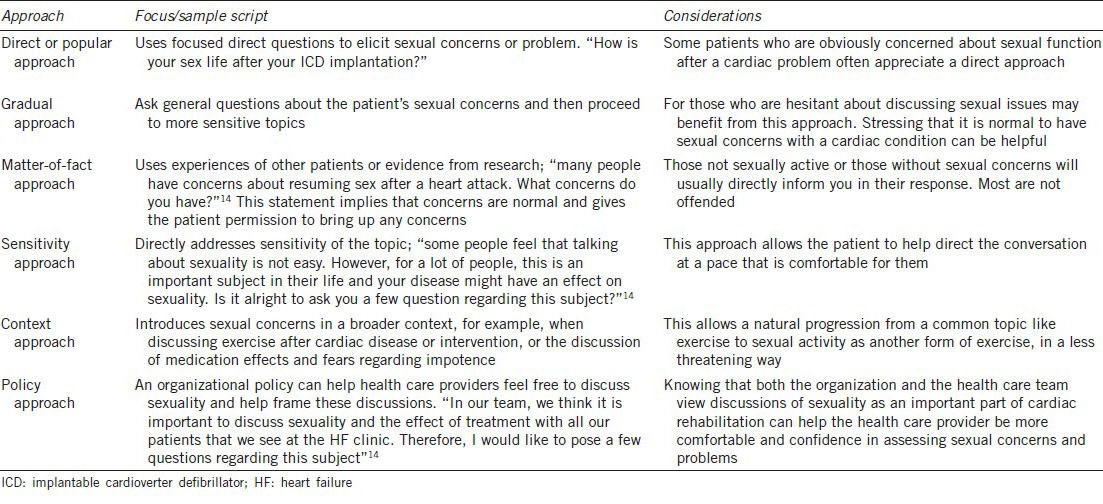
Depending on the setting, personal style, or professional background, different approaches are used for assessment of sexual concerns and problems.14 There is no evidence on the most effective approach of assessment; however, it is important that the health care provider feels comfortable with the subject. There are several approaches for sexual assessment that can be practically applied (Table 2).14 These allow the health care provider to tailor the discussion to the needs and concerns of the patient based on the initial assessment. For example, some patients who have been wondering if sexual activity is safe often appreciate a more direct approach in order to get their questions answered, while such an approach might be too confronting for other patients.14 In a recent study of 296 cardiac patients in The Netherlands, none of the respondents stated that it would annoy them if the cardiologist would ask about sexual function. Only one patient said this question would offend him, but most respondents considered a question about sexual health as something positive.2 At the same time; however, one should realize that cultural and personal differences need to be considered in discussing sex with patients and their partners. Often, people might regard sex as private and talking about sex can be viewed as taboo or unnecessary in some cultures.2,18 Similarly, cultures within organizations may influence the health care provider's comfort in bringing up sexual topics. Although there is often a lack of organizational policy for discussing sexual health with patients, it might be considered in the assessment.19 A good policy can help professionals to address the subject.14
Table 2.
Approaches for sexual assessment14
Practical tools for assessment
Assessment instruments and other tools can provide a starting point to address sexual health, and for sexual counseling, education, and provision of resources and referrals.1,14 These tools may consist of questionnaires, diaries, or event logs. Some questionnaires are specially developed to measure ED, such as the International Index of Erectile Function-5,20 which is a frequently used 5 items self-report questionnaire. Another questionnaire aimed to measure male sexual function is for example the Brief Male Sexual Function Inventory,21 a 10 items self-report scale that measures drive, erection, ejaculation, problem with sexual function, and sexual satisfaction.
There are also questionnaires that assess female sexual health. The Female Sexual Function Index, is a 19 items questionnaire measuring a woman's desire, arousal lubrication, orgasm, and satisfaction.22 The Brief Index of Sexual Functioning for Women23 consists of 22 items that measure sexual desire, sexual activity, and sexual satisfaction. These instruments might also be used with female partners of men with CVD when assessing the couple as a dyad.
Some questionnaires are suitable to use in both genders or have specific gender specific versions, such as derogatis interview for sexual functioning (DISF) and DISF – self-report.24
Evaluating risk of sex before treatment
To optimally target treatment for men, any cardiac risk associated with sexual activity should be evaluated. The recommendations from the third Princeton Consensus Conference, similar to prior reports, emphasized evaluation and management of men with ED who are at risk for CVD, focusing efforts on risk reduction, and addressing any risk associated with sexual activity individually.7 Exercise ability can be used to guide estimates of cardiovascular risk with sexual activity, although in some cases, stress testing may be needed to evaluate each man's cardiovascular health as related to the physical demands of sexual activity.25 Furthermore, exercise tolerance should be established before the initiation of ED therapy in all men regardless of cardiovascular risk.
Patients determined to be at low-risk, generally can perform moderate intensity exercise without symptoms, and sexual activity is generally safe. Low-risk patients are those successfully revascularized, or with asymptomatic and controlled hypertension, mild valvular disease, and left ventricular dysfunction (New York Heart Association [NYHA] Classes I and II HF).7 Low-risk patients are often good candidates for ED therapy.
High-risk patients are those with severe CVD, unstable, and/or moderate to severe symptoms for which sexual activity may pose significant risk, thus sexual activity should be avoided. For patients deemed to be at high-risk, sexual activity should be deferred until their condition is optimally managed and stabilized.4 Common high-risk conditions include: unstable/refractory angina pectoris, uncontrolled hypertension, congestive HF (NYHA Class IV), a recent MI < 2 weeks without intervention, high-risk dysrhythmia such as exercise-induced ventricular tachycardia, ICD with frequent shocks and poorly controlled atrial fibrillation, obstructive hypertrophic cardiomyopathy and severely symptomatic and moderately to severe disease, such as aortic stenosis.7
Indeterminate risk patients are those requiring further evaluation with exercise stress testing before sexual activity can be recommended. Those included in this risk category are those with: mild to moderate stable angina pectoris, prior MI within the last 2–8 weeks and without intervention awaiting exercise electrocardiography, congestive HF (NYHA Class III), and noncardiac sequelae of atherosclerotic disease such as peripheral arterial disease and history of stroke or transient ischemic attack.7 Patients in the indeterminate category are reclassified into low- or high-risk based on further testing.
INTERVENTIONS FOR SEXUAL COUNSELING: WHAT WORKS?
Studies testing interventional approaches for sexual counseling are limited, although some early work began in the mid-1970 and early 1980's.1 Recent attention to this topic has provided insights regarding effective strategies for sexual counseling. Consensus document recommendations for interventional studies, based on those showing greatest effectiveness, include the use of a psychosocial framework, such as cognitive behavioral therapy and social support (Class IIa; Level of Evidence B).1 This illustrates the importance of including both psychosexual and physical aspects in counseling. In addition, it is suggested that educational approaches with repeated meetings with both patients and partners, and using a multidisciplinary approach may yield greatest effectiveness (Class IIa; Level of Evidence B).1
Several studies cited here illustrate both interventional approach and positive outcomes of sexual counseling (Table 3). Klein et al.26 studied the use of sexual therapy with a multi-faceted approach in Phase 2 cardiac rehabilitation patients. Sexual activity, sexual satisfaction, and overall sexual quality of life improved postintervention. The study findings illustrate that supportive interventions can enhance sexual function and quality of life, and integrating such interventions in cardiac rehabilitation is an important strategy.
Table 3.
Sample interventions for sexual counseling
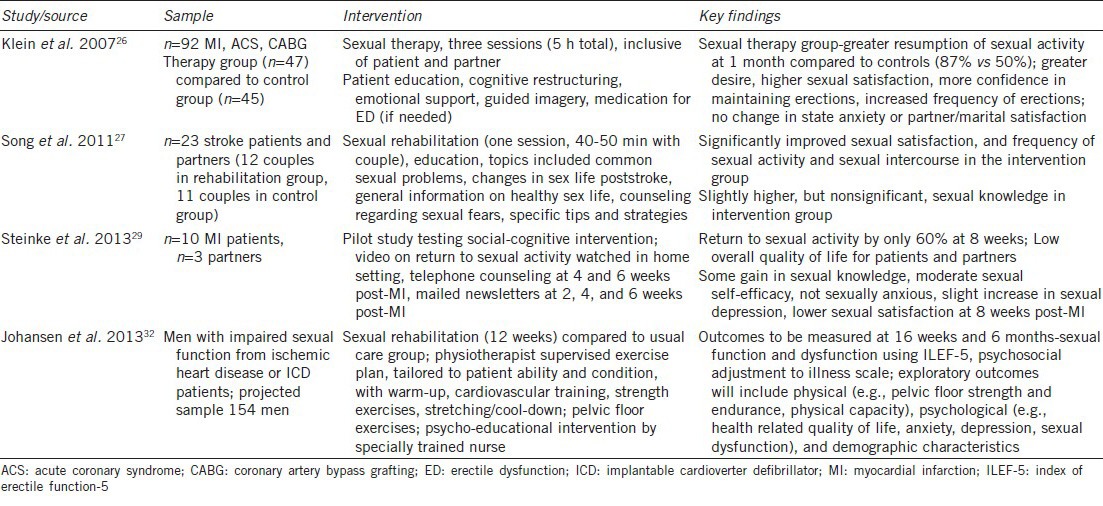
Stroke patients often face considerable challenges in resuming sexual activity, related to physical deficits from the stroke and psychological impact. Song et al.27 tested a one-session sexual rehabilitation program, primarily educational in nature, with stroke patients and partners, and implemented prior to hospital discharge, with outcomes later measured at 1 month postdischarge. While there were improvements in sexual satisfaction and the frequency of sexual activity, sexual knowledge did not improve. Gains in short-term sexual knowledge has been reported at 1 month post-MI,28 but changes in longer term knowledge may be difficult to achieve.
A small pilot study of MI patients tested a social-cognitive sexual counseling intervention, implemented with several interventional components over an 8-week period.29 This is one of few studies to use the psychosexual measure of sexual self-concept in a cardiac population.30,31 Overall, patients exhibited some improvement in sexual knowledge, had moderate sexual self-efficacy, and were not sexually anxious, but with slightly increased sexual depression at 8 weeks post-MI. Of concern is the low rate of return to sexual activity; only 60% reported return to sexual activity at 8 weeks, compared to 80% prior to the MI.29 This appeared to contribute to the finding of lower sexual satisfaction, and perhaps low quality of life scores. A strength of the study is the use of specific measures for psychosexual factors (sexual anxiety, sexual depression, sexual self-efficacy, and sexual satisfaction), areas not usually addressed. Global measures, such as for depression or anxiety does not differentiate between overall psychological distress compared to that related to sexual activity. Thus, using sexual-specific measures may provide greater understanding of sexual concerns and problems, and help guide interventions. Further testing of the intervention used in this study is clearly needed.
One promising study in progress includes a 12 weeks sexual rehabilitation program for men with an ICD or ischemic heart disease.32 This is a follow-up to a preliminary study of 196 ICD patients that elicited patient concerns related sexual function and changes in sexual behavior, but yielded no differences in the intervention and control groups.33 For the later study, more intensive exercise and training plan, as well as a psycho-educational intervention are planned components of the intervention.32 This study is important in that few studies have examined sexual function in ICD patients, and intervention studies are almost nonexistent.
The studies highlighted here are more recent, have solid designs for sexual counseling interventions, and show promising results. Additional intervention studies, 10 in all and spanning the years of 1976 to 2012 are presented with study details in the sexual counseling consensus document.1 While further intervention studies are needed, some aspects of these interventions may be readily adapted for use in clinical settings, for example, ongoing sexual counseling and support, as well as addressing psychosexual concerns. There is a clear need to implement sexual counseling in practice, and health care providers can be guided in this effort both from the information currently available in scientific statements, and by gleaning some useful strategies from these intervention studies.
SEXUAL COUNSELING – GENERAL STRATEGIES
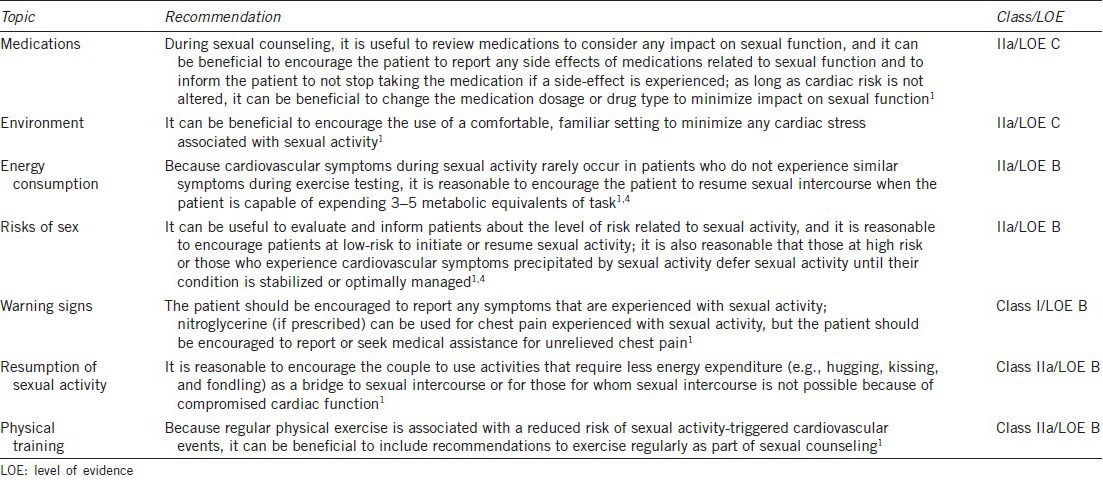
There are general sexual counseling topics that are applicable across cardiovascular diagnoses (Table 4). Health care providers may view these topics as too simplistic or not needing to be addressed. From the authors’ experience in sexual counseling, patients and partners want this practical advice, and it may be helpful in alleviating anxiety and fear regarding sexual activity. In addition, encouraging communication between the patient and partner regarding sexual needs, or concerns are important for overall sexual adjustment and quality of life.
Table 4.
General counseling strategies
Medication effects
Cardiovascular medications are well-known to cause sexual dysfunction, although newer generations of drugs appear to have less sexual side-effects. Beta blockers and thiazide diuretics in particular may impact erectile function,34 although some reports also implicate angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) in ED,35 while others note a neutral or even positive effect of ACE inhibitors and ARBs.34 It is important to advise the patient not to stop taking medications suddenly if a sexual side-effect is experienced. Often, adjusting the dosage or changing to another medication in the same or different classification may alleviate sexual dysfunction. Thorough assessment for any reported sexual side-effects is important to evaluate whether sexual dysfunction is related to underlying vascular effects or to the drug itself. It is imperative to establish a good relationship with the patient to ensure that the provider has accurate information on which to base clinical decision-making.
Decreasing stress related to sex
There is less research regarding environmental considerations, but encouraging the couple to choose a comfortable, familiar setting is reasonable, to avoid any undue stress on the heart. Research supports that sexual activity with an unfamiliar partner may increase anxiety and cardiac stress, as well as increased risk of coital MI and mortality.4,36 Patients often ask if they should change their usual sexual position or if doing so minimizes the risk. In general, most patients can assume a position of comfort or their usual position if they choose.1 If the patient has had a coronary artery bypass graft (CABG) for example, instructing patients to avoid positions that would put undue strain on incision sites would be important to note in counseling. Thus, health care providers may need to adjust instructions regarding positioning depending on the individual cardiac condition and patient status. A recent online supplement to a consensus document provides visual examples of sexual positioning, which may be helpful to share with patients and partners during sexual counseling.1
Role of physical activity
Recommendations for energy consumption and physical activity go hand in hand. It is helpful to suggest that couples engage in physical activity together, not only to increase physical activity, but to promote intimacy. If the patient is able to engage in physical activity at the level of 3–5 metabolic equivalent of task without symptoms (e.g. walking on the treadmill at 3–4 miles per hour or climbing 2 flights of stairs briskly), sexual activity can usually be resumed.1,4 Some patients may need to undergo exercise testing to verify readiness for sexual activity. It is important to note that not all patients may be able to engage in sexual activity, for example, when experiencing cardiac symptoms or an HF exacerbation. For these times, it is helpful to discuss that there are a range of sexual activities and some require low levels of energy, for example, hugging or kissing. These, along with sexual touching or masturbation, might be used as a bridge to sexual intercourse, so that couples begin with activities that require the least energy expenditure and gradually add other sexual activities until they are ready for sexual intercourse.1 Some patients may define sexual intercourse as the only type of sexual activity, so discussing a range of sexual activities can help promote intimacy for a couple. If the provider does not discuss these topics, the patient and/or partner may believe that any sexual activity is prohibited.
Warning signs
Another important area is the discussion of warning signs with sexual activity. Stressing the risk of a cardiac event during sexual activity is low can help alleviate the couple's fears, and sexual activity as the cause of acute MI is generally < 1%, and the absolute risk within 1 h of sexual activity is low (2-3 per 10 000 person-years).25,37,38 Patients should report symptoms occurring with sexual activities such as chest pain, shortness of breath, rapid or irregular heart rate, dizziness, insomnia after sexual activity, or fatigue the day after sexual activity. Nilsson et al.39 have reported that patients’ knowledge was low for several areas related to safety, including reporting warning signs such as palpitations or shortness of breath, not stopping a medication immediately for sexual side-effects, and avoiding heavy meals or alcohol prior to sexual activity. This provides further evidence that health care providers must provide specific instructions to couples.
SEXUAL COUNSELING FOR SPECIFIC CARDIAC CONDITIONS
This section focuses on the most common cardiac diagnoses encountered by health care providers and content to include in sexual counseling. Conditions that will be discussed include ischemic conditions such as angina, MI, postpercutaneous intervention, or coronary bypass surgery; HF; and implanted devices. The reader is referred to the two scientific statements for other conditions such as congenital heart disease, valvular heart disease, and stroke.1,4
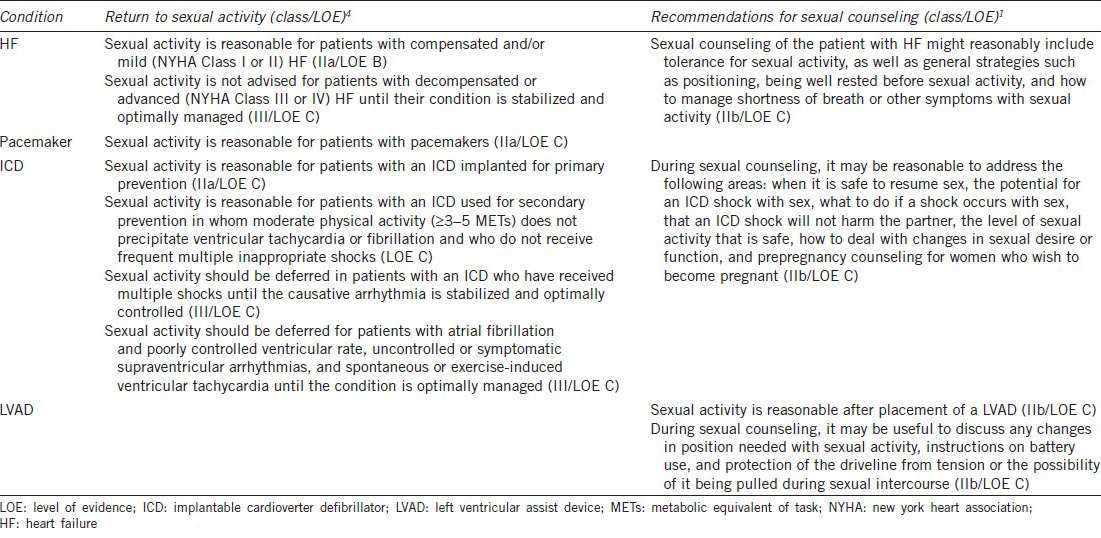
One key aspect for the conditions discussed is that the cardiac condition must be stabilized and optimally managed before recommending the patient resume sexual intercourse. As mentioned previously, other less vigorous sexual activities might be resumed in the interim. Advice on when to resume sexual activity depends on the particular cardiac condition (Tables 5 and 6), and then individualized to the patient and partner. Patients not only want to know when they can resume sexual activity, but how to go about resuming sex. In our experience during postcardiac recovery, patients and partners may be confused, scared, and unsure about resuming sex; therefore, the recommendations for sexual counseling are a guide to help health care providers address the common topics for sexual counseling. In addition, the general counseling strategies cited previously (Table 4) are important to discuss with all cardiac patients.
Table 5.
Recommendations for sexual activity and counseling for ischemic conditions
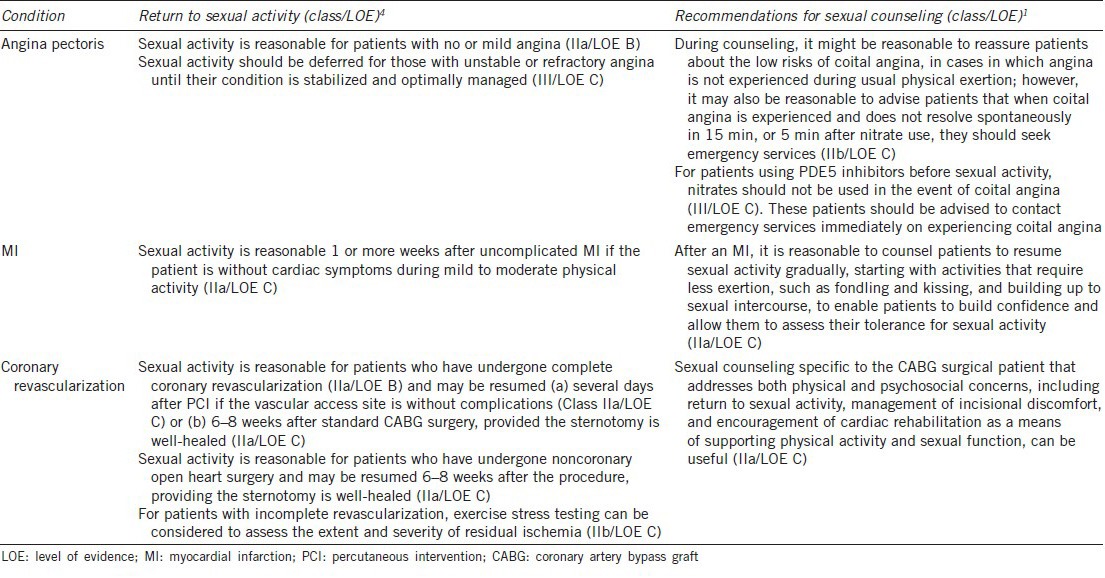
Table 6.
Recommendations for sexual activity and counseling for HF or implanted devices
Ischemic conditions
For patients with angina or MI, and once their condition is stabilized, and they are asymptomatic, sexual activity can usually be resumed within a week or more after the cardiac event (Table 5). Those who had a complicated MI, including cardiac arrest, hypotension, serious arrhythmias, or HF, may need to resume sexual activity gradually over a longer period of time and may need exercise stress testing to determine readiness for sexual activity.4,40 Patients and their partner are often fearful that sexual activity may cause another MI. Assessing sexual concerns and addressing these with education and psychological support can be quite helpful. In addition, advising patients to choose a position of comfort and one that allows unrestricted breathing is useful.40 It is important to discuss the warning signs as mentioned previously, including any coital angina. Patients should be directly told what interventions to try, such as stopping to rest or taking nitroglycerine (if prescribed), and when to seek emergency treatment. As noted in Table 5, if the patient experiences angina and has taken a phosphodiesterase-5 (PDE5) inhibitor, nitrates should not be used.25
After CABG, patients may be fearful about resuming sex, much like the MI patient, so providing reassurance and education is important. Both patients and partners are concerned that engaging in sexual activity may cause harm to the sternum if an open approach was used. Patients can be encouraged to use a position that avoids straining on the sternal incision or one that is uncomfortable (Table 5). Often, using a mild pain reliever before sexual activity can alleviate any discomfort, as well as the use of pillows strategically placed to provide support of incisional/sternal areas.40 In addition, women have described breast discomfort such as shooting pain to the breasts, numbness, tingling, and heaviness;41,42 therefore, supporting both the breasts and incisions using the strategies above are good suggestions for women post-CABG.
Heart failure
The ability to engage in sexual activity is very much dependent on the class of HF, being stabilized, and optimal medical management. Those patients with NYHA Class I or II HF can usually engage in sexual activity if well-managed and asymptomatic with sexual activity (Table 6). In patients with NYHA Class III or IV HF, being optimally managed and not in a decompensated state will help determine the safety of sexual activity.4 Some patients may not be able to safely engage in sexual intercourse; thus, other less vigorous sexual activities may be recommended. The use of sexual foreplay may help gauge tolerance for sexual activity.1
In sexual counseling, health care providers should additionally advise the HF patient to use a sexual position that allows for easier breathing, such as a semi-reclining or upright position, and avoiding positions that require less effort, such as an on-bottom position. Discussion of warning signs/symptoms during sexual activity is particularly relevant in HF, and encouraging patients to stop and rest if shortness of breath occurs. One practical suggestion is to have the patient time the use of diuretics so that frequent urination does not interfere with sexual activity.1,40
Implanted devices
Patients with a pacemaker have few restrictions on sexual activity, unless their overall cardiac condition is limiting in regards to sexual activity. It is well-known, however, that those patients with an ICD and their partners have considerable anxiety and fear about the ICD and the potential for ICD discharge during sexual activity. Thus, assessment of sexual concerns, education, and psychological support are needed. In general, ICD patients can usually resume sexual activity fairly quickly after ICD placement, particularly if asymptomatic with moderate physical activity (Table 6). The exception would be for patients who experience frequent inappropriate ICD shocks or arrhythmias.4 Sexual counseling should include avoiding pressure or strain on the implantation site, discussion of patient/partner fears of ICD firing with sexual activity, the low-risk of ICD firing with sexual activity, that the partner would not be harmed if it does fire, reporting ICD discharge with sexual activity to the health care provider as device settings may need to be adjusted, and taking medications as prescribed to prevent sinus tachycardia.1 Changes in sexual desire and sexual activity after ICD have been reported, so it is important to instruct the patient to report any sexual problems experienced.
Of the few studies available regarding a left ventricular assist device (LVAD), these indicate that the sexual function may improve after LVAD, owing to greater sexual interest, desire, and energy. In one study, patients returned to sexual activity within 1 month after returning home postimplant.43 Unique to this population are patient, and partner fears related to driveline displacement. Avoiding tension on the driveline and using sexual positions to protect the driveline from potential dislodgement would be important in sexual counseling (Table 6).1
COUNSELING REGARDING PHOSPHODIESTERASE-5 INHIBITORS
Men commonly turn to PDE5 inhibitors to assist with ED, with sildenafil, tadalafil, and vardenafil as the commonly used drugs in this class. These drugs overall effectiveness and safety have been established for most men. Vardenafil and sildenafil have a shorter duration of action, with a half-life of about 4 h, while the longer-acting tadalafil has a half-life of 17.5 h.25 PDE5 inhibitors cause modest reductions of systolic and diastolic blood pressures, which could be problematic in those cardiovascular patients with hypotension. In addition, vardenafil may cause the QTc interval to be prolonged, and should be avoided in patients with a history of torsades de pointes, those with congenital QTc prolongation, and if medications that prolong the QTc interval are being used.25 The safety and effectiveness of PDE5 inhibitors is fairly well-established, and few serious cardiac events have been reported. The most common side-effects with PDE5 inhibitors are headache, flushing, dyspepsia, visual changes, and nasal congestion.
As mentioned, the use of both short- and long-acting nitrates is contraindicated with the concomitant use of PDE5 inhibitors, as significant drops in systemic arterial pressure can result. A patient presenting with ischemic conditions should not receive short- or long-acting nitrates within 24 h of use of vardenafil or sildenafil, or within 48 h of use of tadalafil.25 It is advised that patients on chronic nitrate therapy be reevaluated if treatment with PDE5 inhibitors is sought; changing to a nonnitrate therapy might be considered.
The choice of PDE5 inhibitor is based on a comprehensive discussion between patient and provider, and taking into account, which drug might yield long-term treatment success. A thorough assessment of sexual function and patterns of dysfunction are important considerations. In counseling patients, the discussion includes the action and onset of each drug, specific dosing, and side-effects. For most patients, sildenafil or vardenafil are taken 30–60 min prior to sexual activity, while tadalafil is taken at least 2 h before anticipated sexual activity. The longer half-life of tadalafil allows for greater spontaneity of sexual activity. In some cases, daily dosing with tadalafil might be appropriate, with some studies showing improved erectile function over time.44 Important in counseling is the discussion of drugs to avoid, such as nitrates, or for which caution is advised (e.g. alpha blockers), and providing the rationale in understandable terms for the patient and partner, to increase adherence and to avoid potentially dangerous side-effects. In addition, taking sildenafil and vardenafil on an empty stomach is suggested, as high fat meals interferes with plasma concentration of the drug.45,46
SUMMARY
Providing sexual counseling of cardiac patients is an important role for health care providers. Assessment of patients and partners sexual concerns with a few select questions or using a standardized assessment instrument can determine both sexual concerns, interest in sexual activity, and level of previous sexual activity. Then, knowledge of the individual patient's medical condition and application of both general and specific sexual counseling strategies by cardiac condition can be used effectively in addressing patients’ sexual quality of life.
AUTHOR CONTRIBUTIONS
EES contributed to the parts of “Why sexual counseling, Interventions for sexual counseling, sexual counseling– general strategies, sexual counseling for specific cardiac conditions, and counseling regarding PDE5 inhibitors.” TJ contributed to the parts of “Sexual assessment and sexual counseling– HF.”
COMPETING INTERESTS
The authors declare that they have no competing interests.
REFERENCES
- 1.Steinke EE, Jaarsma T, Barnason SA, Byrne M, Doherty S, et al. Sexual counseling for individuals with cardiovascular disease and their partners: a consensus document from the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP) Circulation. 2013;128:2075–96. doi: 10.1161/CIR.0b013e31829c2e53. [DOI] [PubMed] [Google Scholar]
- 2.Nicolai MP, van Bavel J, Somsen GA, de Grooth GJ, Tulevski II, et al. Erectile dysfunction in the cardiology practice-a patients’ perspective. Am Heart J. 2014;167:178–85. doi: 10.1016/j.ahj.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 3.Byrne M, Doherty S, Murphy AW, McGee HM, Jaarsma T. Communicating about sexual concerns within cardiac health services: do service providers and service users agree? Patient Educ Couns. 2013;92:398–403. doi: 10.1016/j.pec.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Levine GN, Steinke EE, Bakaeen FG, Bozkurt B, Cheitlin MD, et al. Sexual activity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2012;125:1058–72. doi: 10.1161/CIR.0b013e3182447787. [DOI] [PubMed] [Google Scholar]
- 5.DeBusk R, Drory Y, Goldstein I, Jackson G, Kaul S, et al. Management of sexual dysfunction in patients with cardiovascular disease: recommendations of the Princeton Consensus Panel. Am J Cardiol. 2000;86:175–81. doi: 10.1016/s0002-9149(00)00896-1. [DOI] [PubMed] [Google Scholar]
- 6.Kostis JB, Jackson G, Rosen R, Barrett-Connor E, Billups K, et al. Sexual dysfunction and cardiac risk (the Second Princeton Consensus Conference) Am J Cardiol. 2005;96:313–21. doi: 10.1016/j.amjcard.2005.03.065. [DOI] [PubMed] [Google Scholar]
- 7.Nehra A, Jackson G, Miner M, Billups KL, Burnett AL, et al. The Princeton III Consensus recommendations for the management of erectile dysfunction and cardiovascular disease. Mayo Clin Proc. 2012;87:766–78. doi: 10.1016/j.mayocp.2012.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Developing sexuality counselling guidelines for health care providers. [Last accessed on 2014 Feb 28]. Available from: http://www.who.int/reproductivehealth/topics/sexual_health/counselling/en/
- 9.Giagulli VA, Moghetti P, Kaufman JM, Guastamacchia E, Iacoviello M, et al. Managing erectile dysfunction in heart failure. Endocr Metab Immune Disord Drug Targets. 2013;13:125–34. doi: 10.2174/1871530311313010015. [DOI] [PubMed] [Google Scholar]
- 10.Medina M, Walker C, Steinke EE, Wright DW, Mosack V, et al. Sexual concerns and sexual counseling in heart failure. Prog Cardiovasc Nurs. 2009;24:141–8. doi: 10.1111/j.1751-7117.2009.00052.x. [DOI] [PubMed] [Google Scholar]
- 11.Jaarsma T, Steinke EE, Gianotten WL. Sexual problems in cardiac patients: how to assess, when to refer. J Cardiovasc Nurs. 2010;25:159–64. doi: 10.1097/JCN.0b013e3181c60e7c. [DOI] [PubMed] [Google Scholar]
- 12.Mandras SA, Uber PA, Mehra MR. Sexual activity and chronic heart failure. Mayo Clin Proc. 2007;82:1203–10. doi: 10.4065/82.10.1203. [DOI] [PubMed] [Google Scholar]
- 13.Hardin SR. Cardiac disease and sexuality: implications for research and practice. Nurs Clin North Am. 2007;42:593–603. doi: 10.1016/j.cnur.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Jaarsma T. Sexual problems in heart failure patients. Eur J Cardiovasc Nurs. 2002;1:61–7. doi: 10.1016/S1474-5151(01)00009-3. [DOI] [PubMed] [Google Scholar]
- 15.Westlake C, Dracup K, Walden JA, Fonarow G. Sexuality of patients with advanced heart failure and their spouses or partners. J Heart Lung Transplant. 1999;18:1133–8. doi: 10.1016/s1053-2498(99)00084-4. [DOI] [PubMed] [Google Scholar]
- 16.Driel AG, de Hosson MJ, Gamel C. Sexuality of patients with chronic heart failure and their spouses and the need for information regarding sexuality. Eur J Cardiovasc Nurs. 2014;13:227–34. doi: 10.1177/1474515113485521. [DOI] [PubMed] [Google Scholar]
- 17.Steinke EE. Sexual counseling after myocardial infarction. Am J Nurs. 2000;100:38–43. [PubMed] [Google Scholar]
- 18.Altiok M, Yilmaz M. Opinions of individuals who have had myocardial infarction about sex. Sex Disabil. 2011;29:263–73. [Google Scholar]
- 19.Hoekstra T, Lesman-Leegte I, Couperus MF, Sanderman R, Jaarsma T. What keeps nurses from the sexual counseling of patients with heart failure? Heart Lung. 2012;41:492–9. doi: 10.1016/j.hrtlng.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 21.Mykletun A, Dahl AA, O’Leary MP, Fosså SD. Assessment of male sexual function by the brief sexual function inventory. BJU Int. 2006;97:316–23. doi: 10.1111/j.1464-410X.2005.05904.x. [DOI] [PubMed] [Google Scholar]
- 22.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 23.Taylor JF, Rosen RC, Leiblum SR. Self-report assessment of female sexual function: psychometric evaluation of the brief index of sexual functioning for women. Arch Sex Behav. 1994;23:627–43. doi: 10.1007/BF01541816. [DOI] [PubMed] [Google Scholar]
- 24.Derogatis LR. The Derogatis Interview for Sexual Functioning (DISF/DISF-SR): an introductory report. J Sex Marital Ther. 1997;23:291–304. doi: 10.1080/00926239708403933. [DOI] [PubMed] [Google Scholar]
- 25.Lange RA, Levine GN. Sexual activity and ischemic heart disease. Curr Cardiol Rep. 2014;16:445. doi: 10.1007/s11886-013-0445-4. [DOI] [PubMed] [Google Scholar]
- 26.Klein R, Bar-on E, Klein J, Benbenishty R. The impact of sexual therapy on patients after cardiac events participating in a cardiac rehabilitation program. Eur J Cardiovasc Prev Rehabil. 2007;14:672–8. doi: 10.1097/HJR.0b013e3282eea52d. [DOI] [PubMed] [Google Scholar]
- 27.Song H, Oh H, Kim H, Seo W. Effects of a sexual rehabilitation intervention program on stroke patients and their spouses. NeuroRehabilitation. 2011;28:143–50. doi: 10.3233/NRE-2011-0642. [DOI] [PubMed] [Google Scholar]
- 28.Steinke EE, Swan JH. Effectiveness of a videotape for sexual counseling after myocardial infarction. Res Nurs Health. 2004;27:269–80. doi: 10.1002/nur.20022. [DOI] [PubMed] [Google Scholar]
- 29.Steinke EE, Mosack V, Hertzog J, Wright DW. A social-cognitive sexual counseling intervention post-MI-development and pilot testing. Perspect Psychiatr Care. 2013;49:162–70. doi: 10.1111/j.1744-6163.2012.00345.x. [DOI] [PubMed] [Google Scholar]
- 30.Steinke EE, Wright DW, Chung ML, Moser DK. Sexual self-concept, anxiety, and self-efficacy predict sexual activity in heart failure and healthy elders. Heart Lung. 2008;37:323–33. doi: 10.1016/j.hrtlng.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 31.Steinke E, Mosack V, Hill T. Sexual self-perception and adjustment of cardiac patients: a psychometric analysis. J Res Nurs. 2013;18:191–201. [Google Scholar]
- 32.Johansen PP, Zwisler AD, Hastrup-Svendsen J, Frederiksen M, Lindschou J, et al. The CopenHeartSF trial – comprehensive sexual rehabilitation programme for male patients with implantable cardioverter defibrillator or ischaemic heart disease and impaired sexual function: protocol of a randomised clinical trial. BMJ Open. 2013;3:e003967. doi: 10.1136/bmjopen-2013-003967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berg SK, Elleman-Jensen L, Zwisler AD, Winkel P, Svendsen JH, et al. Sexual concerns and practices after ICD implantation: findings of the COPE-ICD rehabilitation trial. Eur J Cardiovasc Nurs. 2013;12:468–74. doi: 10.1177/1474515112473528. [DOI] [PubMed] [Google Scholar]
- 34.Baumhäkel M, Schlimmer N, Kratz M, Hackett G, Jackson G, et al. Cardiovascular risk, drugs and erectile function – a systematic analysis. Int J Clin Pract. 2011;65:289–98. doi: 10.1111/j.1742-1241.2010.02563.x. [DOI] [PubMed] [Google Scholar]
- 35.Hoekstra T, Jaarsma T, Sanderman R, van Veldhuisen DJ, Lesman-Leegte I. Perceived sexual difficulties and associated factors in patients with heart failure. Am Heart J. 2012;163:246–51. doi: 10.1016/j.ahj.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 36.Parzeller M, Bux R, Raschka C, Bratzke H. Sudden cardiovascular death associated with sexual activity. A forensic autopsy study (1972–2004) Forensic Sci Med Pathol. 2006;2:109–14. doi: 10.1385/FSMP:2:2:109. [DOI] [PubMed] [Google Scholar]
- 37.Muller JE, Mittleman MA, Maclure M, Sherwood JB, Tofler GH. Triggering myocardial infarction by sexual activity. Low absolute risk and prevention by regular physical exertion. Determinants of Myocardial Infarction Onset Study Investigators. JAMA. 1996;275:1405–9. doi: 10.1001/jama.275.18.1405. [DOI] [PubMed] [Google Scholar]
- 38.Dahabreh IJ, Paulus JK. Association of episodic physical and sexual activity with triggering of acute cardiac events: systematic review and meta-analysis. JAMA. 2011;305:1225–33. doi: 10.1001/jama.2011.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nilsson UG, Svedberg P, Fridlund B, Alm-Roijer C, Thylén I, et al. Sex knowledge in males and females recovering from a myocardial infarction: a brief communication. Clin Nurs Res. 2012;21:486–94. doi: 10.1177/1054773812437241. [DOI] [PubMed] [Google Scholar]
- 40.Steinke EE. Sexuality and chronic illness. J Gerontol Nurs. 2013;39:18–27. doi: 10.3928/00989134-20130916-01. [DOI] [PubMed] [Google Scholar]
- 41.King KM, Gortner SR. Women's short-term recovery from cardiac surgery. Prog Cardiovasc Nurs. 1996;11:5–15. [PubMed] [Google Scholar]
- 42.Moore SM. CABG discharge information: addressing women's recovery. Clin Nurs Res. 1996;5:97–104. doi: 10.1177/105477389600500108. [DOI] [PubMed] [Google Scholar]
- 43.Samuels LE, Holmes EC, Petrucci R. Psychosocial and sexual concerns of patients with implantable left ventricular assist devices: a pilot study. J Thorac Cardiovasc Surg. 2004;127:1432–5. doi: 10.1016/j.jtcvs.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 44.Smith WB, II, McCaslin IR, Gokce A, Mandava SH, Trost L, et al. PDE5 inhibitors: considerations for preference and long-term adherence. Int J Clin Pract. 2013;67:768–80. doi: 10.1111/ijcp.12074. [DOI] [PubMed] [Google Scholar]
- 45.Kloner RA. Cardiovascular effects of the 3 phosphodiesterase-5 inhibitors approved for the treatment of erectile dysfunction. Circulation. 2004;110:3149–55. doi: 10.1161/01.CIR.0000146906.42375.D3. [DOI] [PubMed] [Google Scholar]
- 46.Weeks B, Ficorelli CT. How new drugs help treat erectile dysfunction. Nursing. 2006;36:18–9. doi: 10.1097/00152193-200601000-00013. [DOI] [PubMed] [Google Scholar]


