Abstract
The treatment of erectile dysfunction (ED) has been a fascination involving multiple medical specialities over the past century with urologic, cardiac and surgical experts all contributing knowledge toward this multifactorial disease. With the well-described association between ED and cardiovascular disease, angiography has been utilized to identify vasculogenic impotence. Given the success of endovascular drug-eluting stent (DES) placement for the treatment of coronary artery disease, there has been interest in using this same technology for the treatment of vasculogenic ED. For men with inflow stenosis, DES placement to bypass arterial lesions has recently been reported with a high technical success rate. Comparatively, endovascular embolization as an approach to correct veno-occlusive dysfunction has produced astonishing procedural success rates as well. However, after a thorough literature review, arterial intervention is only recommended for younger patients with isolated vascular injuries, typically from previous traumatic experiences. Short-term functional outcomes are less than optimal with long-term results yet to be determined. In conclusion, the hope for a minimally invasive approach to ED persists but additional investigation is required prior to universal endorsement.
Keywords: erectile dysfunction, impotence, penile erection, vasculogenic
INTRODUCTION
From Leriche's description of aortoiliac insufficiency in 19321 to Michal's seminal studies in phalloarteriography,2 our appreciation of the significance of penile arterial insufficiency (PAI) as an etiologic factor for erectile dysfunction (ED) is the culmination of work over the last century.3,4 While the hope has been that penile revascularization procedures can treat broad populations of men with ED, the evidence indicates that these procedures are only suited for men with focal arterial lesions.5,6
The advent of drug-eluting stents (DES) and their proven benefit in coronary applications brought renewed interest with regards to the interventional treatment of ED. Endovascular techniques, while novel and academically interesting, are practically limited by a lack of a noninvasive, anatomic method for documenting PAI before and after the intervention. Currently, the role of endovascular treatment of ED is unclear except for cases of proximal iliac disease secondary to peripheral arterial disease.7 In light of the recent ZEN trial8 and reports of successful embolization techniques for veno-occlusive dysfunction,9 we examine the potential benefits and limiting factors with novel endovascular treatments for vasculogenic ED.
VASCULOGENIC ERECTILE DYSFUNCTION
Normal erectile function depends on adequate arterial inflow as well as venous outflow occlusion. Filling of the corporal sinusoids results in a suprasystolic intracaversonal pressure, up to several 100 mmHg. In the presence of either impaired caversonal smooth muscle relaxation or arterial inflow stenosis, filling of the corporeal bodies is compromised. In the case of corporeal veno-occlusive dysfunction (CVOD), the required intracavernosal pressure is unsustainable.10 Either point of failure – compromised arterial inflow or venous leakage – may result in vasculogenic ED.10
The major source of arterial inflow to the penis comes from the internal pudendal artery (IPA), a branch of the internal iliac artery (IIA). The IPA eventually subdivides into the cavernosal arteries, which in turn give rise to the helicine arteries that empty into the lacunar spaces within the corpora cavernosa (Figure 1).11 The tunica albuginea surrounds the paired corpora cavernosa, compressing the subtunical and emissary veins, limiting venous return from the penis through the deep dorsal vein when erect. Atherosclerotic disease of the IIA or IPA may limit the increase in blood flow required to fill the corpora cavernosa and achieve an erection.
Figure 1.
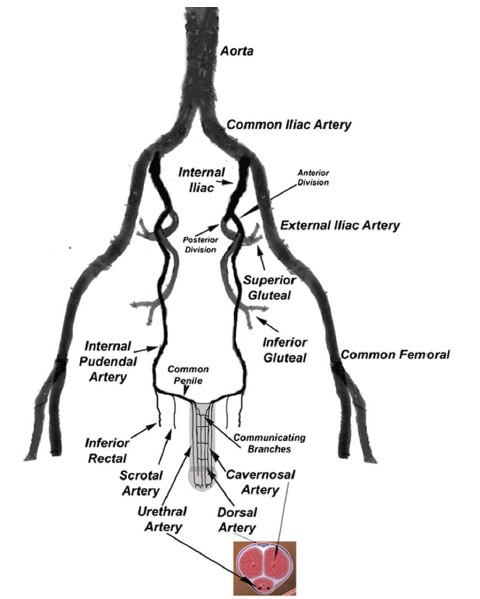
Arterial blood supply to the penis. This figure is reproduced with permission from Rogers et al.11
Currently, the first-line therapy for ED is oral phosphodiesterase-5 inhibitors (PDE5i).12 However, when oral ED therapy fails, subsequent therapies are progressively invasive and include intracavernosal injections, intraurethral suppositories, vacuum erection devices, and penile prostheses.12 In the presence of a proximal fixed obstruction to arterial flow, corpora cavernosa filling may be limited despite endothelial, smooth muscle relaxation and such scenarios may result in sub-optimal response to PDE5i. Interventional treatment of atherosclerotic disease in the IIA and IPA may, therefore, offer another approach to ED refractory to current first-line therapies.
ZEN TRIAL
The Zotarolimus-Eluting Peripheral Stent System (Medtronic, Minneapolis MN, USA) for the treatment of ED in males with sub-optimal response to PDE5 inhibitors (ZEN) trial, published in 2012,8 was the first trial of DES for the treatment of ED. While recruitment methods were not reported, 383 subjects were screened, and those with an International Index of Erectile Function 6 (IIEF-6) baseline of < 22 proceeded to a 4 week run-in phase. The authors describe the use of the IIEF-6 score, which is a modified IIEF, that takes six questions from the IIEF that have the highest discriminating power to diagnose ED.13 The run-in phase consisted of a 4 weeks trial of PDE5i and a required minimum of four sexual encounters. At the end of the run-in phase, patients with IIEF-6 scores remaining < 22 who reported ED for 50% or more of their sexual encounters were screened by penile Doppler ultrasound and those with adequate systolic velocity as well as those with venous leak were excluded from the trial. Invasive penile angiography criteria were designed to include patients with unilateral or moderate to severe bilateral stenosis of the IPA. Patients with ≥ 70% stenosis of non-IPA erectile-related arteries were excluded. Ultimately 30 out of 383 screened subjects (7.8%) were enrolled in the trial (Figure 2)14 – procedural success was 100%, and no adverse events were reported at 30 days.
Figure 2.
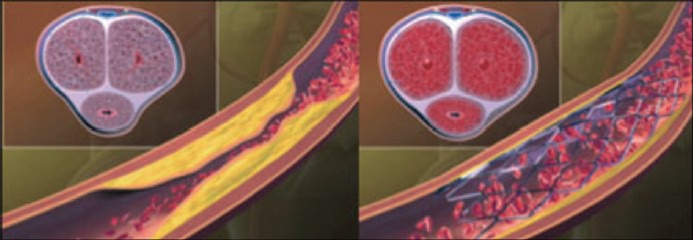
Left panel: Atherosclerotic narrowing in the internal pudendal artery resulting in poor arterial inflow and ED with suboptimal filling of penile cavernosal tissue. Right panel: Improved arterial inflow after implantation of a zotarolimus-eluting peripheral stent system. This figure is reproduced with permission from Rogers et al.14
Mean IIEF-6 domain scores were 15.5 ± 4.2 preprocedure, 22.4 ± 6.3 at 3 months, and 21.8 ± 6.5 at 6 months. The feasibility endpoint was defined as an IIEF domain score increase of at least 4 in over half of subjects at 3 months. Despite a positive trend, increases in total IIEF-6 scores and peak systolic velocity at 3 and 6 months, follow-up was limited by a small sample size, accompanied by large standard deviations and a lack statistical significance. Such variance in the ZEN data makes definitive conclusions with regards to treatment efficacy difficult to establish.
While the ZEN trial defined PDE5i nonresponders as those patients demonstrating IIEF-6 scores < 22 at the end of the 4 week run-in phase, much remains unclear regarding each patient's experience with these drugs before the trial and during the period following intervention. It is unknown whether the patients had been taking PDE5i with insufficient response prior to beginning the run-in phase, or if the run-in phase was the initial attempt at first-line pharmacotherapy. The authors note that PDE5i therapy was continued in patients after intervention as was “clinically indicated.” Given the variety of protocols for PDE5i treatment for ED, it would be valuable to know the specific details concerning the drugs, dosage and dosing regimens for study patients both during the run-in phase and following stent placement.
One significant limitation of the ZEN trial was its exclusion of patients taking nitrates. Nitrates are frequently used to treat anginal symptoms in cardiac patients, and with growing data supporting nitrate/hydralazine combination therapy in select patients with symptomatic congestive heart failure (CHF),15 their use for this indication is likely to increase. Given the increased prevalence of ED among patients with coronary artery disease (CAD) or CHF,16,17 the exclusion of these patients in examining the benefits of endovascular treatment for ED overlooks a significant population of patients who may benefit.
Zotarolimus is an mTOR inhibitor, an immunosuppressive agent indicated for use in coronary DES. DES, such as the zotarolimus-eluting stent used in the ZEN trial, are designed to provide controlled local release of immunosuppressive agents thereby slowing the rate of stent neointimalization and reducing the rate of restenosis. This benefit is not without cost, as patients receiving coronary DES require a minimum of 12 months of dual antiplatelet therapy with aspirin and a P2Y12 inhibitor such as clopidogrel to offset the increased risk of stent thrombosis.18 Neither the authors of the ZEN trial nor subsequent review authors have addressed the risks inherent to long-term dual-agent antiplatelet therapy.
While the combination of aspirin and clopidogrel or other P2Y12 inhibitors represents the mainstay of pharmacotherapy after endovascular stent placement, this treatment regimen is not without significant risk. In a meta-analysis of patients on daily P2Y12 inhibitor therapy, patients taking clopidogrel had a 3.88% risk of major bleeding events and a 5.87% risk of major or minor bleeding events as defined by the Thrombolysis in Myocardial Infarction trial.19,20 Although these risks are widely regarded as acceptable when balanced against the risk of coronary stent thrombosis and subsequent myocardial ischemia, there are likely a number of patients for whom the restoration of erectile function does not outweigh the increased bleeding risk. On the other hand, given the correlation between CAD and concomitant ED, there is likely a population of patients with ED already on dual antiplatelet therapy for which the placement of a DES would confer no additional pharmacotherapeutic risk. By excluding patients on nitrates for the purpose of demonstrating PDE5i nonresponse via a run-in phase, the protocol of the ZEN trial overlooks this potential patient population.
The choice to use DES in the ZEN trial was made partially on the assumption that smaller arteries are more prone to restenosis, and thus the effects of zotarolimus would be particularly beneficial in this case. However, the observed restenosis of 11 out of 32 lesions (34.4%) represents a significantly increased rate of restenosis compared to 9.2% for DES placed in the coronary vasculature.21 This finding suggests that the zotarolimus, for unknown reasons, may have less of an effect in the small pelvic vasculature than direct extrapolation from cardiac data would predict.
Given the risks associated with dual antiplatelet therapy and the relatively high rate of restenosis despite the elution of zotarolimus from the stent, it is reasonable to consider the use of bare metal stents (BMS). BMS require a shorter duration of dual antiplatelet therapy (minimum 1 month)18 compared to DES and thus reduce the bleeding risks in patients not taking antiplatelet agents for another indication.
LIMITATIONS
There is a lack of radiographic data correlating pelvic arterial disease with ED. The Incidence of Male Pudendal Artery Stenosis in Sub-optimal Erections Study (IMPASSE) was designed by the ZEN investigators to define normal pelvic vascular anatomy and examine the relationship between pelvic arterial disease and ED.7 However, this study was terminated and results were never published due to similar difficulties in patient selection that limited the scope of the ZEN trial. The acquisition of this information is critical for predicting an optimal population for future trials. An attempt for a trial similar to IMPASSE is needed, as utility of pudendal stenting hinges upon general population analysis of IPA stenosis.
YOUNG MEN WITH BLUNT PELVIC TRAUMA-AN IDEAL PATIENT POPULATION?
It has been demonstrated that blunt pelvic trauma can initiate a cascade of events resulting in endothelial dysfunction and ultimately a reactive atherosclerotic process resulting in focal stenosis.22 The distal IPA passing through Alcock's canal is especially susceptible to blunt mechanical trauma and compression against the ischio-pubic ramus.22 While penile revascularization has been occasionally attempted in such cases, these procedures are technically complex and should only be performed by surgeons experienced with this procedure.11 Given the feasibility of IPA stenting with DES, as demonstrated by the ZEN trial, we propose that such endovascular interventions may ultimately be ideally suited for rare and difficult to treat cases of ED in young men with focal atherosclerotic disease secondary to blunt pelvic trauma.
In contrast to these young patients with focal disease are older subjects who have diffuse atherosclerotic disease. ED in this population is secondary to potential plaque formation in all vasculature involved with penile tumescence.14 Whereas stenting men with focal lesions causing ED has provided successful outcomes, percutaneous intervention in men with widespread atherosclerosis has not proven beneficial and therefore excludes a large population of men with ED who have diffuse vascular disease.
VENO-OCCLUSIVE DYSFUNCTION
Surgical options for ED secondary to venous leak have historically been limited to open surgical ligation of the deep dorsal vein and its collaterals with a reported success rate of 25%.23,24 Aschenbach et al.9 reported an 88.8% clinical success rate after endovascular venous embolization therapy with histoacryl-lipiodol. In this trial of 29 patients, the diagnosis of CVOD was confirmed with pharmacocavernosometry and cavernosography. This procedure had a high technical success rate and was performed on an outpatient basis under local anesthesia. Furthermore, no complications were experienced throughout the trial. Given the paucity of reliable options for the treatment of CVOD, Aschenbach's minimally invasive percutaneous venous embolization technique with histoacryl-lipiodol is an important and encouraging advancement that merits further study.
However, isolated and focal venous leaks are a rare cause of ED. Rather corporal CVOD has been recognized as the true underlying cause for most cases of venous leak. CVOD may occur as a result of age or injury related changes to the tunica albuginea, cavernosal smooth muscle dysfunction from structural alterations, excessive adrenergic input or from shunts created during priapism episodes and subsequent repair.10 Although poor venous occlusion may be the underlying mechanical defect, other factors play a role in the etiology of CVOD negating single vessel occlusion from endovascular techniques as a viable solution for the majority of the effected population. Therefore, the long-term results of venous embolization therapy need to be substantiated as durability was not shown with venous ligation surgery.
DISCUSSION
The etiology of vasculogenic ED is complex and multifactorial. Most patients with long-standing atherosclerotic disease will likely not be good candidates for IPA stenting due to the diffuse nature of atherosclerotic disease. Appropriate patient selection will be paramount for success and depend on clinicians’ abilities to interpret imaging data and correlate degrees of atherosclerotic burden with severity of ED. More accurate and noninvasive methods for the diagnosis of focal stenotic lesions that are likely amenable to endovascular revascularization techniques will provide added benefit in patient selection. Moreover, techniques such as computed tomographic angiography (CTA) to evaluate pelvic arterial lesions are currently being studied by Wang et al.25 for planned percutaneous angioplasty of distal penile vasculogenic lesions in the PERFECT-1 study.26 Results indicate a positive correlation between obstructive lesions identified at the time of intervention and those previously discovered on CTA. Such noninvasive imaging has the potential to identify a larger subset of men with ED secondary to isolated obstructive lesions.
Microsurgical arterial reconstruction with various conduits was attempted from the 1970s until the early 2000s, but such procedures are technically complex and only a few surgeons have routinely attempted to utilize this technique in select patient populations – typically young men with pelvic trauma.22 Only four studies describing microsurgical penile artery bypass for focal stenosis secondary to blunt pelvic trauma are considered good quality. Also, revascularization surgery is considered “experimental” by the American Urological Association.27 In the 1980s and 1990s transluminal angioplasty without stenting was attempted with varying results in a short clinical follow-up period.7 Collectively, studies report a total of 65 patients with an average success rate of 55%28,29,30,31,32,33 The vast majority of these interventions were directed at the larger iliac arteries, with only three interventions at the IPA.7 It has been postulated that failure of these techniques may have been due to high rates of restenosis.8
Montorsi's artery size hypothesis34 and theories linking ED to CAD are based on the fact that the small diameter helicine arteries become damaged early in the atherosclerotic process. If this were true then, these patients would not benefit from endovascular treatment as endovascular access and stenting of these extremely small vessels is not possible. While the artery-size hypothesis partially explains the complex relationship between ED and CAD, evidence exists to suggest that vasculogenic ED is not entirely due to atherosclerosis of the erectile related arteries. Rather, microscopic endothelial and various autonomic factors likely play a major role in the pathogenesis.16 Thus, it remains unclear whether relief of the macroscopic inflow stenosis is a viable and efficient means of treating complex vasculogenic ED.
In summary, endovascular intervention with angioplasty and DES placement offers hope for men with ED from focal arterial lesions resulting from blunt trauma. However, long-term data will be required to evaluate its efficacy fully. Although hemodynamically feasible, the pathophysiology of ED is commonly multifactorial, even in such isolated lesions. Whereas coronary and peripheral vasculature are often amenable to luminal diameter increases that result in long-term patency, the penile anatomy is co-dependent on surrounding anatomy for successful tumescence. Furthermore, when endothelial dysfunction, microvascular changes or structural defects that result in CVOD accompany arterial inflow stenosis, isolated therapy with endovascular stent placement becomes less effective. The hope for a less invasive method to treat ED in select populations may be possible in the future, but its time is not right now.
AUTHOR CONTRIBUTIONS
EDK participated in creative design, manuscript review and revision, project supervisor; RCO conducted literature review, creative design, assist with manuscript drafting, revision and review; GSW participated in creative design and manuscript review; CDR conducted literature review, creative design, drafted manuscript, review and revision. OOE participated creative design.
COMPETING INTERESTS
The authors declare no competing interests.
REFERENCES
- 1.Leriche R, Morel A. The syndrome of thrombotic obliteration of the aortic bifurcation. Ann Surg. 1948;127:193–206. doi: 10.1097/00000658-194802000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michal V, Pospichal J. Phalloarteriography in the diagnosis of erectile dysfunciton. World J Surg. 1978;2:239–48. doi: 10.1007/BF01553563. [DOI] [PubMed] [Google Scholar]
- 3.Rosen MP, Greenfield AJ, Walker TG, Grant P, Guben JK, et al. Arteriogenic impotence: findings in 195 impotent men examined with selective internal pudendal angiography. Young Investigator's Award. Radiology. 1990;174:1043–8. doi: 10.1148/radiology.174.3.174-3-1043. [DOI] [PubMed] [Google Scholar]
- 4.Vlachopoulos C, Rokkas K, Ioakeimidis N, Aggeli C, Michaelides A, et al. Prevalence of asymptomatic coronary artery disease in men with vasculogenic erectile dysfunction: a prospective angiographic study. Eur Urol. 2005;48:996–1002. doi: 10.1016/j.eururo.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Wespes E, Wildschutz T, Roumeguere T, Schulman CC. The place of surgery for vascular impotence in the third millennium. J Urol. 2003;170:1284–6. doi: 10.1097/01.ju.0000086160.63566.11. [DOI] [PubMed] [Google Scholar]
- 6.Sohn M, Hatzinger M, Goldstein I, Krishnamurti S. Standard operating procedures for vascular surgery in erectile dysfunction: revascularization and venous procedures. J Sex Med. 2013;10:172–9. doi: 10.1111/j.1743-6109.2012.02997.x. [DOI] [PubMed] [Google Scholar]
- 7.Shishehbor MH, Philip F. Endovascular treatment for erectile dysfunction: an old paradigm revisited. J Am Coll Cardiol. 2012;60:2628–30. doi: 10.1016/j.jacc.2012.09.032. [DOI] [PubMed] [Google Scholar]
- 8.Rogers JH, Goldstein I, Kandzari DE, Köhler TS, Stinis CT, et al. Zotarolimus-eluting peripheral stents for the treatment of erectile dysfunction in subjects with suboptimal response to phosphodiesterase-5 inhibitors. J Am Coll Cardiol. 2012;60:2618–27. doi: 10.1016/j.jacc.2012.08.1016. [DOI] [PubMed] [Google Scholar]
- 9.Aschenbach R, Steiner T, Kerl MJ, Zangos S, Basche S, et al. Endovascular embolisation therapy in men with erectile impotence due to veno-occlusive dysfunction. Eur J Radiol. 2013;82:504–7. doi: 10.1016/j.ejrad.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 10.Lue TF. Erectile dysfunction. N Engl J Med. 2000;342:1802–13. doi: 10.1056/NEJM200006153422407. [DOI] [PubMed] [Google Scholar]
- 11.Rogers JH, Rocha-Singh KJ. Endovascular therapy for vasculogenic erectile dysfunction. Curr Treat Options Cardiovasc Med. 2012;14:193–202. doi: 10.1007/s11936-012-0171-z. [DOI] [PubMed] [Google Scholar]
- 12.Hatzimouratidis K, Eardley I, Giuliano F, Hatzichristou D, Moncada I, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Assoc Urol. 2014:17–27. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 13.Ramanathan R, Mulhall J, Rao S, Leung R, Martinez Salamanca JI, et al. Predictive correlation between the International Index of Erectile Function (IIEF) and Sexual Health Inventory for Men (SHIM): implications for calculating a derived SHIM for clinical use. J Sex Med. 2007;4:1336–44. doi: 10.1111/j.1743-6109.2007.00576.x. [DOI] [PubMed] [Google Scholar]
- 14.Rogers JH, Karimi H, Kao J, Link D, Javidan J, et al. Internal pudendal artery stenoses and erectile dysfunction: correlation with angiographic coronary artery disease. Catheter Cardiovasc Interv. 2010;76:882–7. doi: 10.1002/ccd.22646. [DOI] [PubMed] [Google Scholar]
- 15.Taylor AL. The African American heart failure trial: a clinical trial update. Am J Cardiol. 2005;96:44–8. doi: 10.1016/j.amjcard.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 16.Gandaglia G, Briganti A, Graham J, Kloner R, Montorsi F, et al. A systematic review of the association between erectile dysfunction and cardiovascular disease. Eur Urol. 2013 doi: 10.1016/j.eururo.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 17.Schwarz E, Rastogi S, Kapur V, Sulemanjee N, Rodriguez J. Erectile dysfunction in heart failure patients. J Am Coll Cardiol. 2006;48:1111–9. doi: 10.1016/j.jacc.2006.05.052. [DOI] [PubMed] [Google Scholar]
- 18.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2012;79:453–95. doi: 10.1002/ccd.23438. [DOI] [PubMed] [Google Scholar]
- 19.Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987;76:142–54. doi: 10.1161/01.cir.76.1.142. [DOI] [PubMed] [Google Scholar]
- 20.Tang XF, Fan JY, Meng J, Jin C, Yuan JQ, et al. Impact of new oral or intravenous P2Y12 inhibitors and clopidogrel on major ischemic and bleeding events in patients with coronary artery disease: a meta-analysis of randomized trials. Atherosclerosis. 2014;233:568–78. doi: 10.1016/j.atherosclerosis.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 21.Yeung AC, Leon MB, Jain A, Tolleson TR, Spriggs DJ, et al. Clinical evaluation of the Resolute zotarolimus-eluting coronary stent system in the treatment of de novo lesions in native coronary arteries: the RESOLUTE US clinical trial. J Am Coll Cardiol. 2011;57:1778–83. doi: 10.1016/j.jacc.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Dicks B, Bastuba M, Goldstein I. Penile revascularization – contemporary update. Asian J Androl. 2013;15:5–9. doi: 10.1038/aja.2012.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katzenwadel A, Popken G, Wetterauer U. Penile venous surgery for cavernosal venous leakage: long-term results and retrospective studies. Urol Int. 1993;50:71–6. doi: 10.1159/000282455. [DOI] [PubMed] [Google Scholar]
- 24.Lewis R. Venous surgery in the patient with erectile dysfunction. Urol Clin North Am. 1993;1:21. [Google Scholar]
- 25.Wang T, Lee W, Chen W, Chen M. Comprehensive assessment of prevalence and distribution of obstuctive pelvic arterial lesions by computed tomographic angiography in patients with erectile dysfunction. J Am Coll Cardiol. 2013;62:B160. [Google Scholar]
- 26.Wang TD, Lee WJ, Yang SC, Lin PC, Tai HC, et al. Safety and six-month durability of angioplasty for isolated penile artery stenoses in patients with erectile dysfunction: a first-in-man study. EuroIntervention. 2014;10:147–56. doi: 10.4244/EIJV10I1A23. [DOI] [PubMed] [Google Scholar]
- 27.Montague D, Jarrow J, Broderick G, Dmochowski R, Heaton J, et al. American Urological Association Education and Research, Inc; 2005. The Management of Erectile Dysfunction: an Update; pp. 1–24. Available from: http://www.auanet.org/common/pdf/education/clinical-guidance/Erectile-Dysfunction.pdf . [Google Scholar]
- 28.Castaneda-Zuniga WR, Gomes A, Weens C, Ketchum D, Amplatz K. Transluminal angioplasty in the management of mesenteric angina. Rofo. 1982;137:330–2. doi: 10.1055/s-2008-1056211. [DOI] [PubMed] [Google Scholar]
- 29.Van Unnik JG, Marsman JW. Impotence due to the external iliac steal syndrome treated by percutaneous transluminal angioplasty. J Urol. 1984;131:544–5. doi: 10.1016/s0022-5347(17)50490-5. [DOI] [PubMed] [Google Scholar]
- 30.Goldwasser B, Carson CC, 3rd, Braun SD, McCann RL. Impotence due to the pelvic steal syndrome: treatment by iliac transluminal angioplasty. J Urol. 1985;133:860–1. doi: 10.1016/s0022-5347(17)49258-5. [DOI] [PubMed] [Google Scholar]
- 31.Dewar ML, Blundell PE, Lidstone D, Herba MJ, Chiu RC. Effects of abdominal aneurysmectomy, aortoiliac bypass grafting and angioplasty on male sexual potency: a prospective study. Can J Surg. 1985;28:154–6. 9. [PubMed] [Google Scholar]
- 32.Angelini G, Pezzini F, Mucci P. Arteriosclerosis and impotence. Minerva Psichiatr. 1985;26:353–17. [PubMed] [Google Scholar]
- 33.Urigo F, Pischedda A, Maiore M, Salis A, Picciau M, et al. Role of arteriography and percutaneous transluminal angioplasty in the diagnosis and treatment of arterial vasculogenic impotence. Radiol Med. 1994;88:86–92. [PubMed] [Google Scholar]
- 34.Montorsi P, Ravagnani P, Galli S, Rotatori F, Briganti A, et al. The artery size hypothesis: a macrovascular link between erectile dysfunction and coronary artery disease. Am J Cardiol. 2005;96:19M–23M. doi: 10.1016/j.amjcard.2005.07.006. [DOI] [PubMed] [Google Scholar]


