Abstract
Picky eating is a common cause of concern for parents of young children. Paediatricians and family physicians are in a key position to help parents learn ways to feed their children effectively. Despite the high prevalence of picky eating, the growth of the majority of picky eaters does not suffer adversely. In the absence of worrying signs and symptoms, reassurance of the child’s normal growth would help allay parental anxieties. Reinforcement of basic feeding principles and providing healthy dietary advice are important strategies to help parents manage children who are picky eaters.
Keywords: feeding guidelines, feeding principles, paediatrics, picky eater, picky eating
Josh, a three-year-old boy, was brought to see you by his mother for being very picky with his food. His mother was worried that Josh has not been putting on enough weight over the past 12 months because he had only achieved a quarter of his ‘expected weight’, according to the child’s health booklet. According to his mother, Josh preferred ‘adult food’ over the nutritious meals prepared just for him. Mealtime has now become a nightmare for his mother, with Josh running around while his mother tries to ‘stuff’ him with food. He was not interested in trying new foods, and preferred drinking milk and juices throughout the day.
HOW COMMON IS THIS IN MY PRACTICE?
Picky or fussy eating in an otherwise healthy toddler or preschooler is a common problem worldwide. Parental perception of their children’s pickiness with food ranges from 20% to 50%, based on studies in the United States, Australia, the United Kingdom, and China.(1,2) In Singapore, nearly half of surveyed parents (including caregivers) perceived their child as a picky eater, and a third of them would consult a doctor about their child’s eating behaviour.(3) Despite the high prevalence of picky eating, the growth of the majority of these children does not suffer adversely.(1,4,5) Paediatricians and general practitioners commonly encounter in their practice patients who are picky eaters. Picky eating is the cause of considerable parental concern, and superficially assuring parents with a mere ‘there is nothing wrong with your child’ may leave many feeling frustrated, and risk compounding parental anxieties. Physicians need to have a systematic approach to evaluating a child with feeding difficulties; this approach should include the identification of red flags suggestive of serious organic pathology. In the absence of worrying signs or symptoms, the reassurance of normal growth can often help to allay parental concerns. Guidance on good feeding practices and the provision of healthy diet advice are useful strategies to help parents feed their child effectively, thus avoiding the transformation of mealtimes into a constant battleground.
WHAT IS PICKY EATING?
The term ‘picky eating’ has no clear clinical definition. It has, however, been described as the consumption of an inadequate variety of food.(1) The 10th revision of the International Classification of Diseases describes ‘feeding disorder of infancy and childhood’, which encompasses ‘difficulty (in) feeding’, as generally involving food refusal, and extreme faddiness in the presence of an adequate food supply and a reasonably competent caregiver, and in the absence of organic disease.(6)
Common characteristics of picky eaters include eating a limited amount of food, refusing food (particularly fruits and vegetables), being unwilling to try new foods, accepting only a few types of food, preferring drinks over food, and having strong food preferences.(1,5) Goh and Jacob(3) reported additional picky behaviours in local children aged 1–10 years, such as eating sweets and fatty foods instead of healthy foods, and eating snacks instead of having proper meals.
WHAT IS THE EXPECTED NORMAL GROWTH?
A major concern of parents of picky eaters is the effect picky eating has on the child’s physical and mental development.(3) A basic explanation of normal growth will help to provide reassurance. During the first year of life, an average infant triples his/her birth weight and increases his/her birth length by 50%.(7) In the second year of life, the expected growth is an average increase in height and weight of 12 cm and 2–3 kg, respectively. From two years of age until the growth spurt at puberty, the average growth of a child continues at a rate of approximately 6–8 cm per year, and 2 kg per year.(8)
All children in Singapore are given a child health booklet at birth. Parents often misinterpret the 50th percentile on the growth charts of the health booklet as the expected normal weight for every child. Parents should be reassured that only children with growth parameters that are two standard deviations or more from the mean, i.e. ≤ 3rd percentile and ≥ 97th percentile, are considered to be significantly deviated from the normal and require in-depth evaluation. It is also important to note that the most effective way to use growth charts is through serial growth measurements. Serially obtained growth measurements that are shown to rise above or drop below two major percentile lines indicate either an accelerated or a faltering growth, respectively. Both observations may require further evaluation.(9)
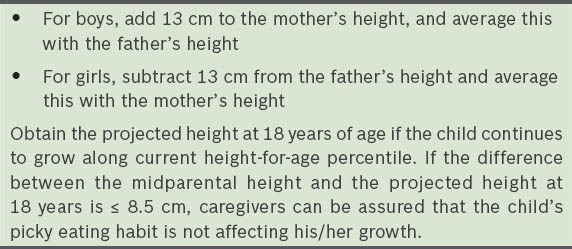
A picky eater who is growing along the 3rd percentile line, but whose parents are of short stature, may not necessarily be suffering from poor growth. In such a case, midparental height adjusted for the child’s gender (Table I) will help to determine whether the child is thriving appropriately, according to his or her genetic potential.(10)
Table I.
Calculation of midparental height.(10)
AETIOLOGY
Exposure to food tastes starts from conception and continues with infant feeding experiences.(11,12) It has been shown that breastfeeding exposes infants to a wider range of food tastes than formula feeding.(13) Such taste variations conferred by breastfeeding help children with earlier acceptance of new foods later on.(14) However, even with good nutrition during pregnancy and breastfeeding, a child’s acceptance of a new food may require repeated exposure of up to 10 times.(15,16) Parental acceptance, in particular maternal acceptance, of new foods trains a child to accept or reject a food.(17)
An interesting theory explains that some children eat fruits and vegetables due to their taste preferences; there is a genetic predisposition for bitter-taste sensitivity – children with low taste sensitivity are likely to eat more vegetables than children with higher taste sensitivity.(18) The preference for salty and sweet taste is also likely to be biologically influenced and enhanced by repeated exposure.(19) Apart from biological factors, the parent-child relationship, family dynamics and the child’s temperament play an important role in influencing a child’s eating behaviour. Pressurising or enticing the child to eat more may not always have the desired effect. Sometimes, caregivers may have unrealistic expectations of growth, as they do not appreciate the physiological decrease in appetite that occurs between one and five years of age. Young children can have considerably varied appetites at mealtimes, but their total daily energy intake usually remains constant.(20) Parents who perceive that their child is not growing enough are more likely to overreact when there are variations in the child’s food intake.
As young children develop their sense of autonomy, they may prefer to feed themselves and start choosing the food they eat.(21) Young children also tend to be neophobic with regard to food.(15,17) Most parents would perceive such children as picky. However, studies have shown that despite children’s initial aversion to new food, most eventually learn to accept them upon repeated exposure.(17)
Food refusal may sometimes be a way to seek attention and affirmation from adults.(22) This behaviour may stem from difficulties present in the parent-child relationship. An inverse association has been shown between a dysfunctional familial environment and a child’s dietary intake.(23)
WHAT ARE THE RED FLAGS?
In order to determine whether the child’s feed refusal is the result of a physiological decrease in appetite or an organic cause, it is vital that a detailed medical and dietary history is taken. A careful physical examination is important to ascertain whether there are any signs of organic disease or malnutrition. Some red flags suggestive of potential organic conditions are listed in Table II.(24) Children with any red flag signs and symptoms may require further evaluation or referral to relevant specialists.
Table II.
Red flag signs and symptoms in children with feed refusal.(24)
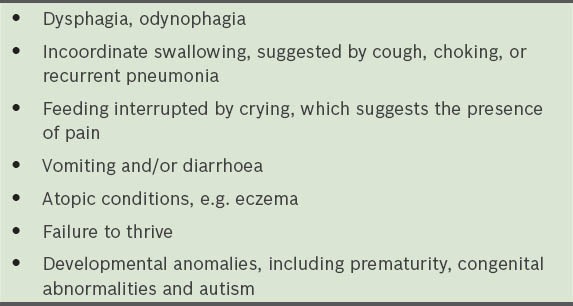
In the absence of any red flags and if physical examination is unremarkable, the management of picky eaters should target the identification of behavioural or environmental factors, and involve an accordingly tailored therapy. In recalcitrant cases, it may be necessary to refer the child to a multidisciplinary feeding clinic that comprises an oromotor specialist, a dietician and a paediatric gastroenterologist.
HOW MUCH IS ENOUGH?
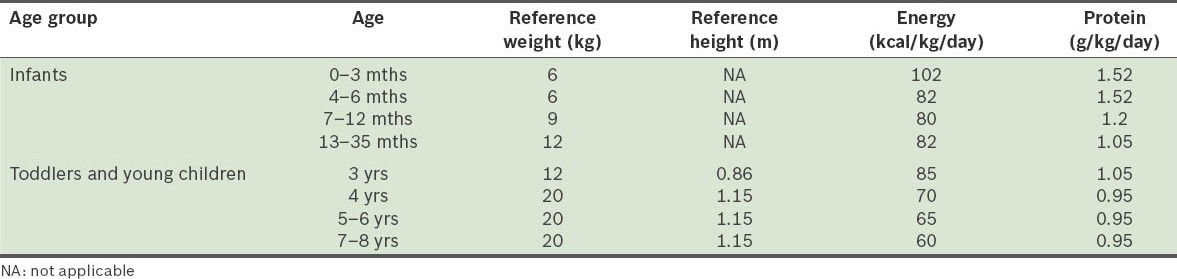
Due to caregivers’ and parents’ personal perceptions of the food portion that children must finish, they often raise concerns of children consuming too little food. Table III can be used to estimate young children’s daily energy and protein requirements.(25) If it is deemed necessary for a child to consume more energy than that estimated in the dietary reference index (DRI) to catch up with growth, an intake of 1.5–2 times of the normal DRI for the respective age range may be prescribed.(25)
Table III.
Dietary reference index for energy and protein requirements for infants, toddlers and young children.(25)
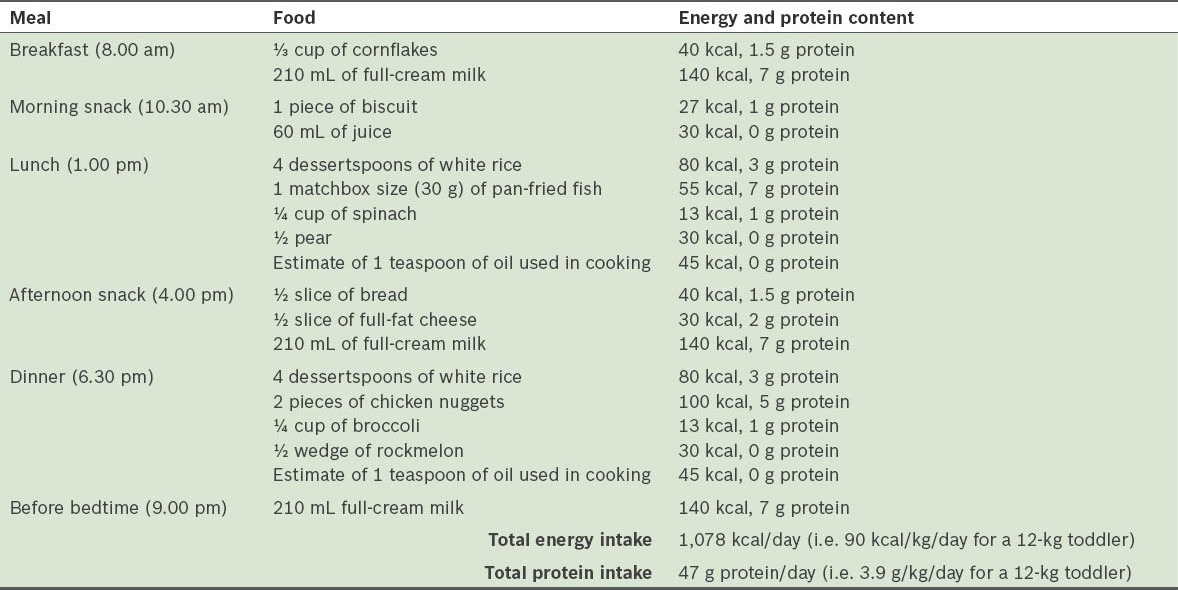
In a busy clinical setting, food exchange lists such as that shown in Table IV can assist practitioners in quickly estimating whether the amount of food consumed (as reported by caregivers) provides adequate energy to meet the child’s growth requirement. Food exchange lists group foods according to similarities in energy, carbohydrate, protein and fat content, so as to ease calculation of macronutrients intake. Table V illustrates how a day’s menu made up of what parents may perceive to be a small amount of food can provide sufficient energy and protein for young children (calculated using the food exchange list).
Table IV.
Food exchange list for macronutrients estimation and meal planning.
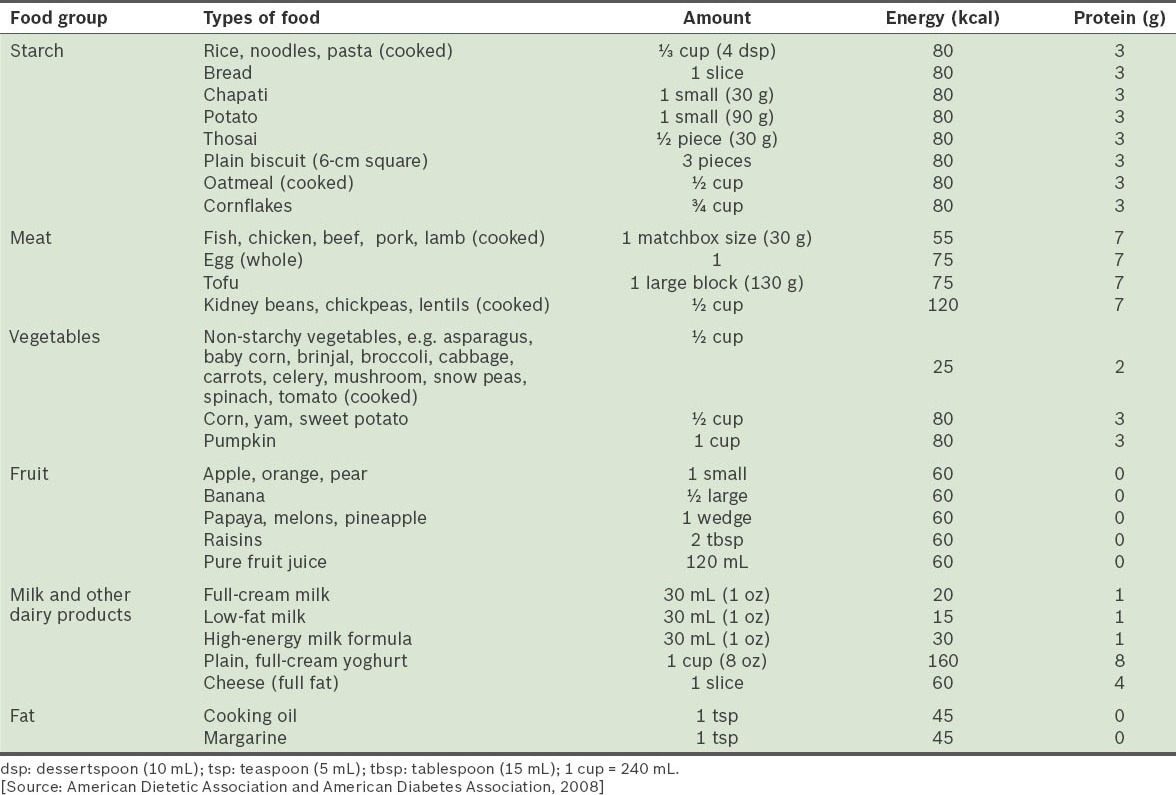
Table V.
Sample menu for a two-year-old toddler.
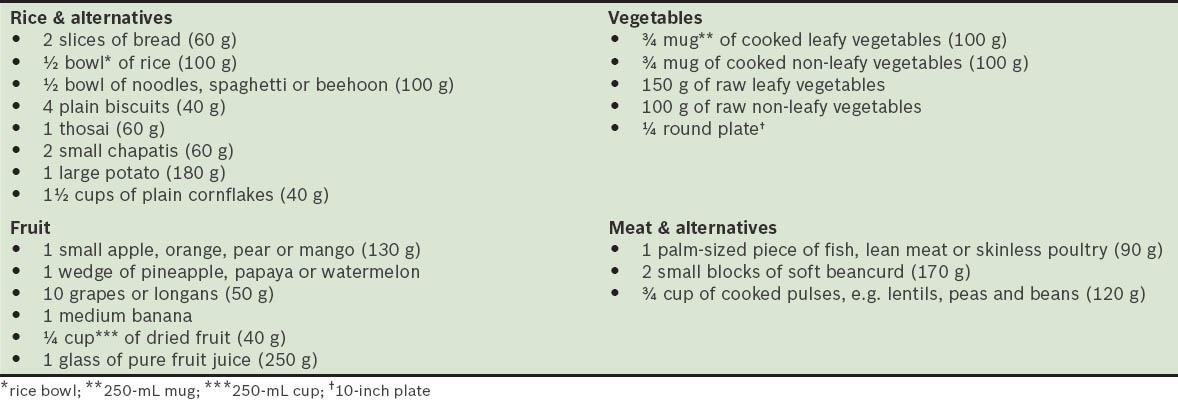
It is important to emphasise to parents to consistently serve children a variety of foods from the major food groups – rice and alternatives, fruits and vegetables, meat and alternatives – as illustrated in the food pyramid from the Health Promotion Board (HPB), Singapore (Fig. 1). HPB has also developed local dietary guidelines to help parents plan nutritious meals with age-appropriate servings for children, as shown in Tables VI and VII.(26)
Fig. 1.
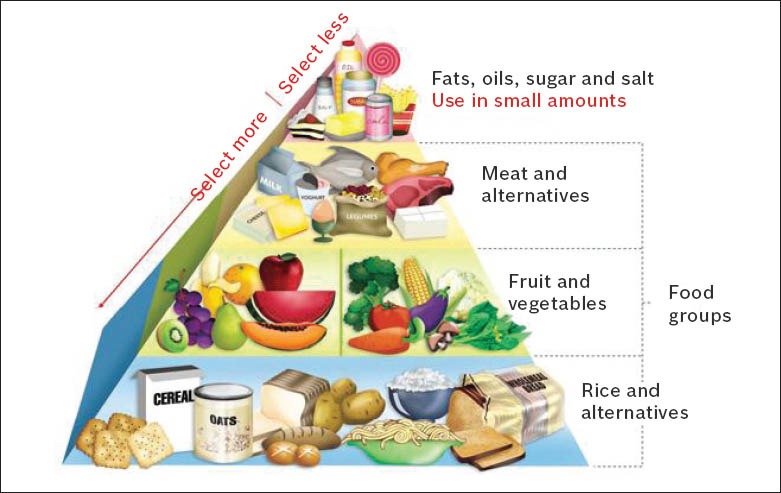
Diagram shows a healthy diet pyramid. [Source: HPB (26)]
Table VI.
Recommended number of servings for children and adolescents [adapted from HPB (26)].
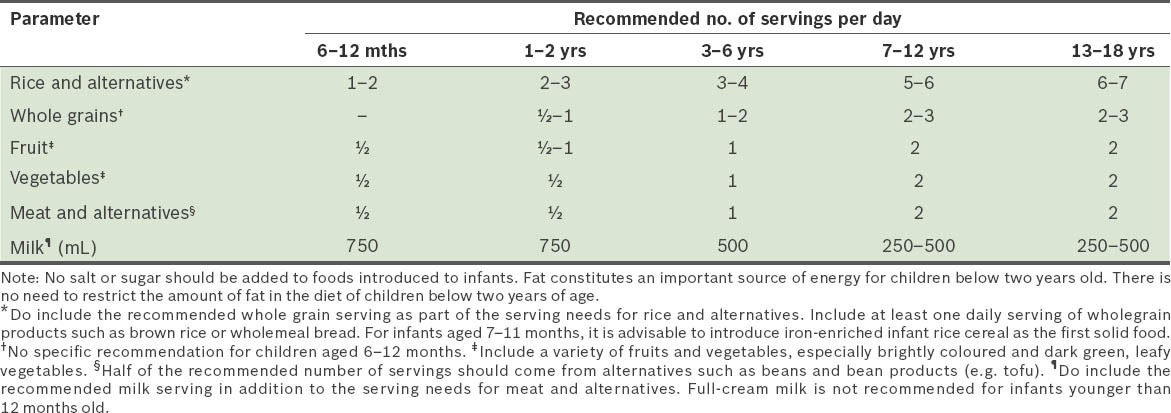
Table VII.
Examples of one serving of food, classified according to the different food groups [adapted from HPB (26)].
FEEDING TIPS FOR PARENTS
Satter(22) provides practical advice on how to best cultivate good eating behaviour in a child, recommending division of responsibility between the parents and the child – parents take responsibility for preparing the right amount and mix of food, and deciding on the venue and time to serve the meal; the child is responsible for how much food to eat, or even to not eat. Parents should also be responsible for providing a pleasant, distraction-free and safe environment for meals and snacks. In a clinic setting, the physician can advise concerned parents on basic feeding principles and underscore the importance of consistent adherence to such principles.(24) The following list outlines some basic feeding principles:(22,24)
Feed to encourage appetite – (a) serve small meals and snacks at consistent times of the day, with 2–3 hours between each meal and snack time, allowing the child to become hungry before the next meal. Young children feel most comfortable with scheduled mealtimes; (b) offer milk, nutritional beverages, juice, soup or water at the end of the meal or snack, and not before, in order to prevent filling their stomachs.
Avoid distraction – (a) seat children at a table for meals and snacks. A comfortable position for eating is one in which the table is at the stomach level of the child. Therefore, use a highchair or booster if necessary; (b) avoid allowing television, tablets, toys, electronics or books at mealtimes, as this takes away the experience of eating. Instead, engage children using food or by allowing children to self-feed.
Families should eat together – (a) eat together as a family to allow interaction and bonding; (b) use family mealtimes as an opportunity to teach healthy eating habits and good table manners to children.
Encourage independent feeding – allow for food spillage and age-appropriate mess during mealtimes; cover the floor if it makes cleaning up after meals easier.
Systematically introduce new food – (a) provide some of the child’s favourite foods together with a small amount of new food; (b) if the child refuses a new food, offer just one bite of the new food without tricking, hiding, bribing or forcing. If the child continues to refuse after three attempts, do not force the child. The caregiver can attempt to reintroduce the new food after a few days or weeks. A child’s preference often changes, although it can take up to ten exposures before the child accepts the food.(15,16)
Limit duration – (a) eating should begin within 15 mins of the start of the meal; (b) meals should last no longer than 20–30 mins; (c) when the meal is over, all food should be removed and only be offered again at the next planned meal. Caregivers should not become a short order cook.
Serve age-appropriate food – (a) offer food appropriate for the child’s oral motor development; (b) use reasonably small helpings (e.g. size of the child’s fist). A general rule of thumb is to offer one tablespoon of each food per year of the child’s age. A bigger serving can be offered, according to the child’s appetite.(25)
Maintain a neutral attitude during feeding time – (a) do not get overly excited or animated such as the use of ‘flying airplanes’ into the child’s mouth; (b) never become or even appear angry; (c) bribes, threats or punishments have no role in healthy eating.
Vitamin and mineral supplementation may be considered if the child’s diet is deemed nutritionally inadequate. Appetite stimulants should not be routinely recommended in a child who is thriving well.
Josh was noted to be an active and cheerful child. His height and weight were thriving along the 25th percentile and physical examination was normal. There were no red flags noted in his history or physical examination, and there were no notable developmental delays. Josh’s mother was relieved after understanding how to refer to the growth charts, and after realising that Josh was still growing. Although she was surprised to hear that Josh could be extending his autonomy to his choice of food, she was able to relate this to Josh’s assertion with his toys and play activities. You shared some parental tips on basic feeding principles and the introduction of new food, and agreed on a plan to review Josh’s well-being in three months.
TAKE HOME MESSAGES
Picky eating behaviour is very common among young children and causes considerable parental anxiety.
Most children who are labelled ‘picky eaters’ have appropriate growth.
It is important to identify red flags suggestive of serious organic pathology, and to offer appropriate treatment or referral to specialists.
Simple healthy dietary advice with an emphasis on serving food from the major food groups helps parents to plan nutritious meals.
Tips with respect to basic feeding principles can help parents learn how to feed their ‘picky eaters’ effectively.
REFERENCES
- 1.Wright CM, Parkinson KN, Shipton D, Drewett RF. How do toddler eating problems relate to their eating behavior, food preferences and growth? Pediatrics. 2007;120:e1069–75. doi: 10.1542/peds.2006-2961. [DOI] [PubMed] [Google Scholar]
- 2.Jin XM, Shi R, Jin ZJ. Epidemiological investigation on the eating problems of children aged 1 to 6 years in Shanghai, China. Chinese J Child Health Care. 2009;17:387–9. 392. [Google Scholar]
- 3.Goh DY, Jacob A. Perception of picky eating among children in Singapore and its impact on caregivers: a questionnaire survey. Asia Pac Fam Med. 2012;11:5. doi: 10.1186/1447-056X-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reau NR, Senturia YD, Lebailly SA, Christoffel KK. Infant and toddler feeding patterns and problems: Normative data and a new direction. Pediatric Practice Research Group. J Dev Behav Pediatr. 1996;17:149–53. [PubMed] [Google Scholar]
- 5.Mascola AJ, Bryson SW, Agras WS. Picky eating during childhood: a longitudinal study to age 11 years. Eat Behav. 2010;11:253–7. doi: 10.1016/j.eatbeh.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World health Organization. International classification of diseases (ICD). ICD-10 Version: 2010 [online] [Accessed April 28 2014]. Available at: http://apps.who.int/classifications/icd10/browse/2010/en#/F98.2.
- 7.Lucas BL, Feucht SA. Nutrition in childhood. In: Mahan KL, Escott-Stump S, editors. Krause’s Food & Nutrition Therapy. 12th ed. St Louis: Saunders; 2008. p. 222. [Google Scholar]
- 8.Shaw V, Lawson M. Nutritional assessment, dietary requirements, feed supplementation. In: Shaw V, Lawson M, editors. Clinical Paediatric Dietetics. 3rd ed. Oxford: Blackwell Publishing; 2008. p. 10. [Google Scholar]
- 9.Sentongo T. Growth assessment and monitoring. In: Corkins MR, Balint J, Bobo E, Plogsted S, Yaworski JA, editors. The A.S.P.E.N Pediatric Nutrition Support Core Curriculum. United States of America: Silver Spring; 2010. p. 146. [Google Scholar]
- 10.Tanner JM, Goldstein H, Whitehouse RH. Standards for children’s height at ages 2-9 years allowing for heights of parents. Arch Dis Child. 1970;45:755–62. doi: 10.1136/adc.45.244.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skinner JD, Carruth BR, Bounds W, Ziegler P, Reidy K. Do food-related experiences in the first 2 years of life predict dietary variety in school-aged children? J Nutr Educ Behav. 2002;34:310–5. doi: 10.1016/s1499-4046(06)60113-9. [DOI] [PubMed] [Google Scholar]
- 12.Mennella JA, Pepino MY, Reed DR. Genetic and environmental determinants of bitter perception and sweet preferences. Pediatrics. 2005;115:e216–22. doi: 10.1542/peds.2004-1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooke LJ, Wardle J, Gibson EL, et al. Demographic, familial and trait predictors of fruit and vegetable consumption by pre-school children. Public Health Nutr. 2004;7:295–302. doi: 10.1079/PHN2003527. [DOI] [PubMed] [Google Scholar]
- 14.Maier AS, Chabanet C, Schaal B, Leathwood PD, Issanchou SN. Breastfeeding and experience with variety early in weaning increase infants’ acceptance of new foods for up to two months. Clin Nutr. 2008;27:849–57. doi: 10.1016/j.clnu.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan SA, Birch LL. Infant dietary experience and acceptance of solid foods. Pediatrics. 1994;93:271–7. [PubMed] [Google Scholar]
- 16.Forestell CA, Mennella JA. Early determinants of fruit and vegetable acceptance. Pediatrics. 2007;120:1247–54. doi: 10.1542/peds.2007-0858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galloway AT, Lee Y, Birch LL. Predictors and consequences of food neophobia and pickiness in young girls. J Am Diet Assoc. 2003;103:692–8. doi: 10.1053/jada.2003.50134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bell KI, Tepper BJ. Short-term vegetable intake by young children classified by 6-n-propylthoiuracil bitter-taste phenotype. Am J Clin Nutr. 2006;84:245–51. doi: 10.1093/ajcn/84.1.245. [DOI] [PubMed] [Google Scholar]
- 19.Liem DG, de Graaf C. Sweet and sour preferences in young children and adults: role of repeated exposure. Physiol Behav. 2004;83:421–9. doi: 10.1016/j.physbeh.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 20.Birch LL, Johnson SL, Andresen G, Peters JC, Schulte MC. The variability of young children’s energy intake. N Eng J Med. 1991;324:232–5. doi: 10.1056/NEJM199101243240405. [DOI] [PubMed] [Google Scholar]
- 21.Cerro N, Zeunert S, Simmer KN, Daniels LA. Eating behaviour of children 1.5-3.5 years born preterm: parents’ perceptions. J Paediatr Child Health. 2002;38:72–8. doi: 10.1046/j.1440-1754.2002.00728.x. [DOI] [PubMed] [Google Scholar]
- 22.Satter E. Feeding dynamics: helping children to eat well. J Pediatr Health Care. 1995;9:178–84. doi: 10.1016/s0891-5245(05)80033-1. [DOI] [PubMed] [Google Scholar]
- 23.Kintner M, Boss PG, Johnson N. The relationship between dysfunctional family environments and family member food intake. J Marriage Fam. 1981;43:633–41. [Google Scholar]
- 24.Kerzner B. Clinical investigation of feeding difficulties in young children: a practical approach. Clin Pediatr. 2009;48:960–5. doi: 10.1177/0009922809336074. [DOI] [PubMed] [Google Scholar]
- 25.Otten JJ, Hellwig JP, Meyers LD. Washingtong: National Academies Press; 2006. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. [Google Scholar]
- 26.Health Promotion Board [online]; [Accessed March 24 2014]. Health Promotion Board Singapore. Build a Healthy Food Foundation. Available at: http://www.hpb.gov.sg/HOPPortal/health-article/2638. [Google Scholar]


