Abstract
The term orbital hypertelorism (ORH) implies “widely apart orbits.” This may also be associated with the abnormal vertical orientation of the orbits (dystopia). This deformity may be unilateral or bilateral, symmetric or asymmetric and may be present in a variety of craniofacial conditions. The treatment is primarily carried out for aesthetic reasons. The timing of treatment is dictated by the underlying condition and the type of procedure envisaged. The mainstay of treatment consists of moving the orbits medially to near normal position. This is accomplished by either an orbital translocation or facial bipartition technique. The choice of procedure is governed by the shape of the maxillary arch and associated occlusal conditions. We must differentiate between the telecanthus (also called pseudo-hypertelorism) and a true ORH as the management differs in these two conditions. The ORH involves extensive intracranial and extracranial operation whereas the telecanthus correction is relatively simpler surgery. The article will discuss the aetiology, classification, presentation, treatment options, timing of surgery and the choice of surgical procedures. Illustrative case reports with long-term results will be used to explain the management of these patients.
KEY WORDS: Box osteotomy, cranial bone graft, facial bipartition, intra-cranial and extra-cranial procedure, lateralization of orbit, orbital socket, telecanthus or pseudo-hypertelorism, vertical dystopia
INTRODUCTION
The term hypertelorism means an increased distance between two body parts.[1] Greg applied it for the eyes and termed it as “ocular hypertelorism” in 1924 to signify widely placed eyes.[2] He used interpupillary distance (IPD) to record its presence. However, Tessier noted that IPD could be increased because of exophoria alone without any bony abnormality of the orbit. He, therefore, proposed the term “orbital hypertelorism” (ORH), wherein there is true lateralisation of the whole of the bony orbit in a way that the distance between the lateral canthus and auditory meatus is shortened.[3]
The ORH is not a disease in itself but the manifestation of a craniofacial deformity that may be present in a variety of craniofacial conditions. The orbits are placed wide apart resulting in an abnormal appearance with ‘broad nose’. It may be present in conditions such as a craniofacial dysplasia, encephaloceles and craniosynostosis syndromes. The increased inner intercanthal distance (ICD) can also occur following trauma or tumours in the naso-orbital region; however there is no change in the position of the lateral wall of the orbit. This ‘pseudo-hypertelorism’ is now a days referred to as ‘telecanthus’.
SOME DEFINITIONS
The distance between two medial canthi measured at the level of posterior lacrimal crest is known as ICD. The outer canthal distance (OCD) is between the two lateral canthi. The distance between the two mid-pupillary regions in the front gaze is called IPD. The palpebral fissure length is the distance between the medial and lateral canthi [Figure 1]. The ICD, OCD and IPD are always increased in all cases of true hypertelorism. It may be emphasised that increased ICD alone without any increase in OCD cannot be termed as hypertelorism. Such a situation can be present in naso-orbito-ethmoid fractures or nasofrontal meningo-encephaloceles. It is better to employ the term ‘telecanthus’ in such conditions. The IPD would also be increased in all cases of hypertelorism. An increased IPD alone as seen in exophorias is not indicative of hypertelorism. Figure 2 illustrates the various measurements in a normal, hyperteloric and pseudo-hyperteloric (telecanthic) orbit.
Figure 1.
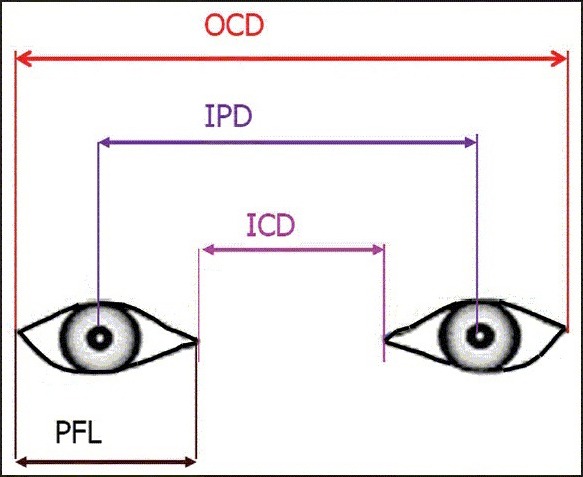
Some definitions pertaining to orbital measurements. ICD: Inner canthal distance, IPD: Inter pupillary distance, OCD: Outer canthal distance, PFL: Palpebral fissure length
Figure 2.
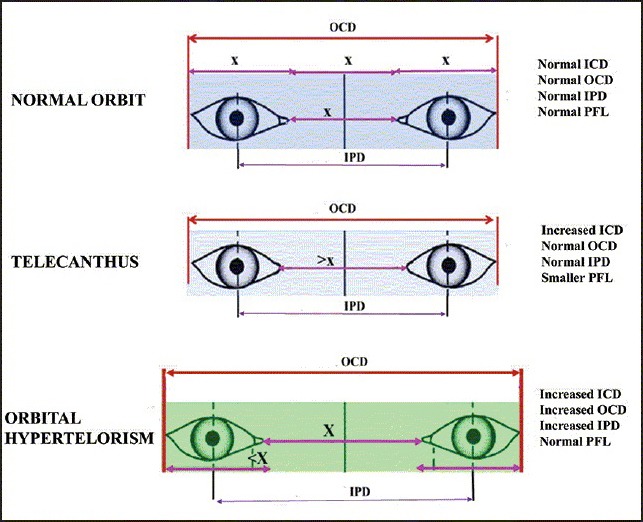
Graphic representation of various measurements as seen in normal orbit (upper row), in orbital telecanthus or pseudo-hypertelorism (middle row) and in orbital hypertelorism (lower row)
The ORH can be seen in a variety of conditions such as craniofacial clefts, craniofacial dysplasias and craniosynostosis syndromes such as Apert and Crouzan. The ORH can be bilateral or may be present only on one side. It may also be associated with orbital dystopias. Figure 3 shows illustrative examples of the ORH. The medial ICD may be increased in cases of meningo-encephaloceles, following trauma or tumors in the naso-orbito-ethmoid (NOE) region. This can give the appearance of wide set eyes, but the lateral orbital walls are normally placed, and the IPD is normal. Figure 4 shows various examples of telecanthus.
Figure 3.
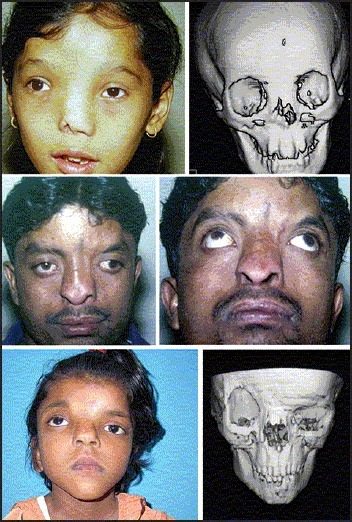
Examples of orbital hypertelorism (true lateralization of the orbit); bilateral symmetrical hypertelorism (upper row), unilateral hypertelorism (middle row) and hypertelorism associated with craniosynostosis (lower row)
Figure 4.
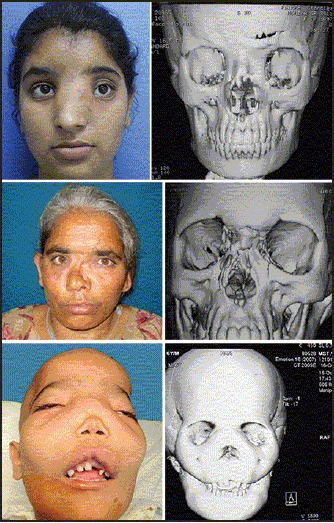
Examples of orbital telecanthus seen in nasofrontal meningo-encephaloceles (upper row), naso-orbito-ethmoid fracture (middle row) and a case of polyostotic fibrous dysplasia (lower row)
EMBRYOLOGY
The ORH probably gets established at about 28 mm embryo stage when a defective development of the nasal capsule leads to freezing of the future fronto-naso-orbito-ethmoid complex thereby preventing the movement of the orbit towards midline.[4] Another reason could be a deficient latero-medial movement of the orbit.[5] Mann feels that early ossification of the lesser wings of sphemoids leads to arrest of orbits in the foetal position.[6] If the frontonasal prominence remains in its embryonic position, the optic placodes cannot move towards the midline resulting in ORH.[7]
AIM OF TREATMENT IN HYPERTELORISM
The corrective surgery is indicated primarily for cosmetic reasons. In the majority of the patients mental and physical development is normal. The patients may have issues with the body image and find it difficult to get integrated into the peer group and the society.
It was not possible to correct the hypertelorism before the landmark work of Paul Tessier in late 60's when he developed the combined intra-cranial and extra-cranial technique for the correction of the deformity.[8,9] He challenged the surgical tenets prevalent at that time and demonstrated that it was possible to move the orbits in three dimensions without adversely affecting the vision. He suggested that this was possible because of the inherent laxity of the optic nerve in the socket. He also demonstrated that large areas of the craniofacial skeleton can be devascularised and these would still survive completely provided healthy lining and cover is present. The techniques of ORH correction have been further refined by Tessier,[3,8,9,10,11,12,13] Converse,[14] van der Meulen et al.,[15,16] Ortiz-Monasterio et al.[17] and Marchac et al.[18] These pioneers visualised the bony orbit consisting of two parts — the outer square shaped box containing the globe and the inner cone shaped part housing the optic nerve. If these parts can be separated, the outer box can be moved in three dimensions without adversely affecting the vision [Figure 5].
Figure 5.
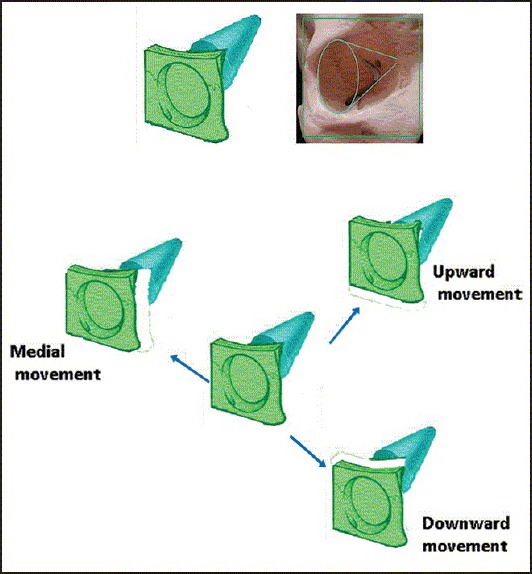
The bony orbit visualised as consisting of a four walled box and a cone. The box contains the globe and the cone contains the optic nerve (upper row). The lower rows show that the orbital box once separated from the cone can be moved in three dimensions without affecting the optic nerve
The purpose of surgery in hypertelorism is:
Bring the two orbits closer together.
Correct any orbital dystopia.
Narrow the nasal dorsum and create a normal nose with adequate projection.
Correct any soft tissue blemishes such as excess skin over the nose, and any nasal clefts or widows peak or displaced eyebrows.
TIMING OF SURGERY
One would like to operate as early as possible to avoid peer teasing and emotional sequelae of ORH. However, it is not advisable to perform this surgery in a child <5 years of age. Since, the osteotomy lines during the surgical procedures is going through the inferior orbital rim, it is likely to injure the un-erupted tooth roots with resultant maxillary growth disturbances. Moreover, the bone stock may not be very good for holding the osteotomies together with fixation, thereby predisposing to relapse of the deformity. Hence, majority of the craniofacial centres would delay the correction of ORH to about 5-7 years of age. The results of surgery performed in adults are more reliable, stable, and the operation is technically much simpler than in a child. However, waiting till the adulthood can lead to a lot of psychological and body image problems.
OPERATIVE TECHNIQUES
Box osteotomy
The surgery may be performed as a “box osteotomy” which permits a translational movement along the horizontal or vertical axes as per needs of the ORH deformity. This entails bony cuts going through the infraorbital rim. The classic orbital box osteotomy involves an en-bloc movement of the orbits medially into the space created by resection of abnormally wide nasal and ethmoidal bones. The procedure is best performed by a combined intracranial and extracranial approach. The access to orbital roof and cribriform region is gained after a frontal craniotomy has been performed, and the frontal lobes have been retracted gently. The bi-coronal incision gives a good view of the lateral and medial orbital walls. However the addition of subciliary incisions is recommended for better access to the infraorbital rim and floor of the orbit. All the soft tissue is separated from the orbital roof, lateral wall, medial wall and the floor. The proposed markings for the orbital osteotomy are shown in the Figure 6. The cuts are made in the orbital roof staying about 2 cm from the supraorbital margin, and the cut stops short of the cribriform region so as to protect the olfactory nerves. The medial wall cut is posterior the lacrimal crest so that the nasolacrimal duct and the lacrimal sac can be protected. The lateral cut can either split the orbital wall sagittal or simply go through the greater wing of sphenoid. The cut in the infraorbital region is below the infraorbital nerve exiting from the infraorbital foramen and this extends on to the floor of the orbit. The desired bony resection to be performed is marked on the dorsum of the nose and it removes the excess nasal bone, nasal septum and the enlarged ethmoid sinuses. After removal of the central excess tissue that is causing hypertelorism, the bony orbits can be moved medially into this space and held in place either with plates and screws or by wires. The orbital shift medially results in bony gaps in the lateral orbital wall that need be filled with bone graft and split cranial bone graft is a good choice. Since all the walls of the orbit are moving as one single unit, the orbital volume remains unchanged. Tessier advocated keeping a supraorbital bar to stabilize and guide the mobilized orbits.[8,11] Orbital box osteotomy procedure is generally chosen whenever the dental occlusion is normal.
Figure 6.
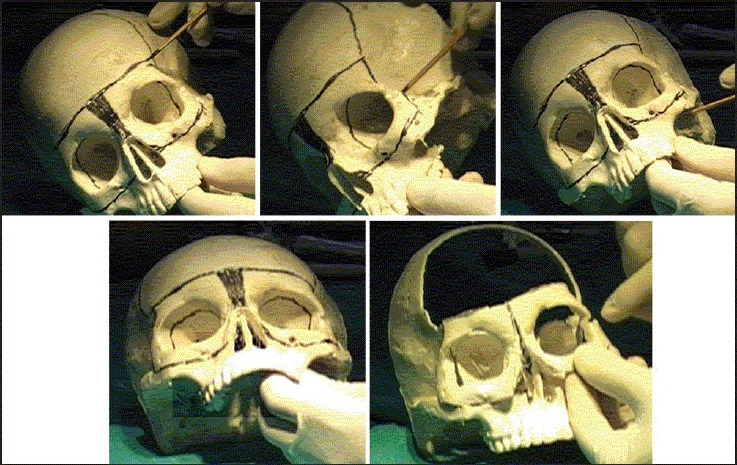
Markings for the orbital box osteotomy on a skull model. The frontal craniotomy and the various markings for the cuts in the orbital walls and roof are shown in upper row and the left picture in lower row. The picture on right in the lower row shows the moved orbits after removal of central excess tissue and completion of box osteotomy cuts (pictures courtesy Dr. Mukund Jagannathan)
Facial bipartition
If the dental occlusion is angulated as in cases of Apert's syndrome or some craniofacial clefts, “facial bipartition” is the surgery of choice. This procedure was proposed by van der Meulen et al.[15,16] and developed by Tessier.[13] It involves medialisation of the two hemi faces. Here the medial resection of the nasal dorsum is in a “V” shaped form, and the palatal bone is split in the midline. The lateral cuts go through the zygomatic arch and pterygomaxillary junction [Figure 7]. The ensuing rotation allows correction of the narrow maxillary arch and also widens the nasal fossae and improves breathing. It would also result in a change of the orbital axis. This procedure is very useful for severe deformities. Facial bipartition would also increase the orbital volume and may improve the proptotic eyes seen in many of these cases.
Figure 7.
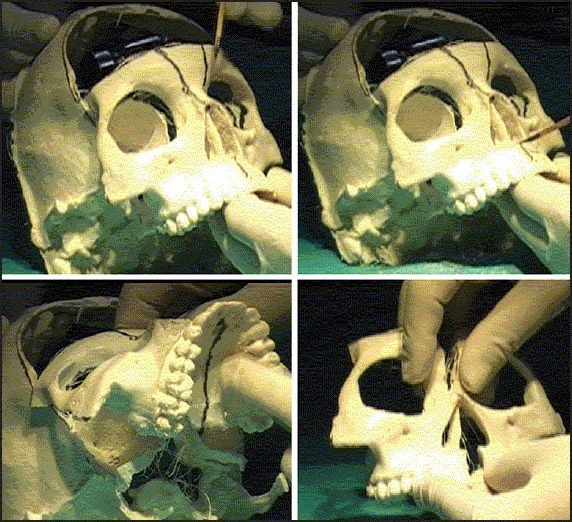
Markings for the facial bipartition. On a skull model. The upper row shows that the frontal craniotomy has been performed and the cuts in the orbital roof, lateral wall and the floor have been made. The zygomatic arch has been divided and the pterygomaxillary cut has also been completed. Upper row left shows markings for the removal of the central bony excess. The picture in upper row right and lower row left shows the markings for splitting the palate in midline. The picture in lower row on right shows completion of cuts and medialising the two halves of the facial bipartition (pictures courtesy Dr. Mukund Jagannathan)
In facial bipartition cases, no frontal bar is preserved; however in box osteotomy the frontal bar is preserved to guide the medial movement of the orbit. This prevents any inadvertent rotational deformity. In facial bipartition since facial rotation is needed, the frontal bar is not kept in order to permit unhindered facial rotation.
Canthopexy
The medial canthi need to be identified and anchored. These can be fixed using trans-nasal wires that fix both the canthi. This technique can be quite frustrating at times. The author has devised a technique wherein a two-hole titanium plate is used for this purpose.[19] The plate is secured to the thick nasal bone, and the lower hole is kept at the level of lacrimal crest. The ipsilateral canthus is securely fixed this hole using steel wires [Figure 8].
Figure 8.
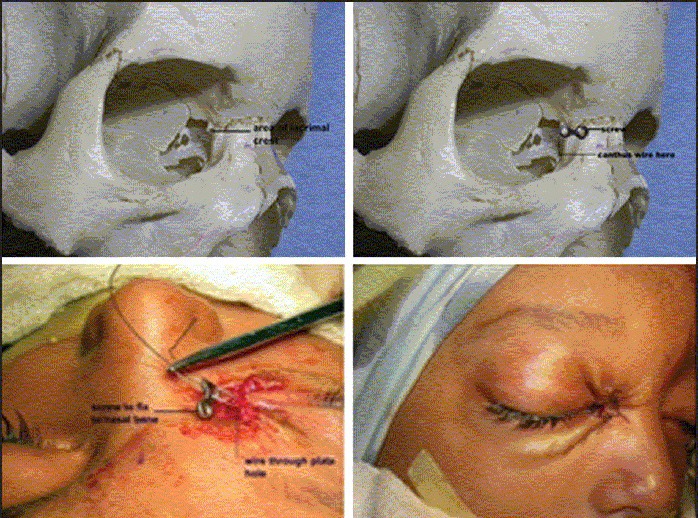
Author's technique of medial canthopexy. The upper row (left) shows the position of lacrimal crest in a skull. The picture on right shows placement of a two-hole plate with the lower hole at the level of posterior lacrimal crest. The lower row (left shows threading of the canthal wire into the lower hole prior to fixing the plate at the upper hole with a screw to the solid nasal bone
Fronto-galeal flap
The removal of ethmoids and the nasal septum exposes the extradural space to the nasal cavity and can be a source of ascending infection. A vascularized flap such as fronto-galeal flap as described by Jackson et al.[20] is interposed between the two cavities to prevent infection.
Dorsal nasal augmentation
Majority of these patients will need augmentation of the dorsum and this is best accomplished by using split cranial bone graft as a cantilever.
Management of excessive skin
In many patients, there is excessive skin present over the dorsum. The excess skin is removed primarily at the time of definitive surgery [Figure 9]. In selected patients, the excess skin and the soft tissue could be removed very early around 9 months or so for better social acceptance without any major orbital osteotomies.
Figure 9.

Management of the excess skin by excision at the time of primary surgery; the lower row shows well healed area 1-year after the surgery
Illustrative case examples
Symmetrical hypertelorism
The patient in Figure 10 has bilateral symmetrical hypertelorism. This should ideally be corrected by medial orbital shift using “box osteotomy” technique. The planning has been shown on the three-dimensional computed tomography (CT) scan image in the middle row. A “box osteotomy” has been planned, and the orbits were medialised after removing the excess bone from the midline nasal area. The defects in the lateral side were bone grafted. The supraorbital bar was kept intact for guiding the movement of the orbital box medially. A split cranial bone craft was cantilevered to augment the projection of the nose. The postoperative pictures in the lower row after 3 years show stable result. The well healed mediatised bony orbits are seen in the three-dimensional reconstruction in the lower row.
Figure 10.

A case of hypertelorism who underwent orbital translocation using bilateral box osteotomy. Upper row showing preoperative appearance. The middle row outlines the planned osteotomy and the planned removal of the widened bones in the midline. The middle figure shows the orbits after removal of the midline bony excess and execution of the box osteotomy. The picture on left shows medially mobilized orbits. Lower row shows result 3 years postoperative
Asymmetrical hypertelorism
Figure 11 shows a patient of the craniofacial cleft who has hypertelorism only on his left side. The other side bony orbit has a normal position. It was, therefore, decided to shift the bony orbit medially only on the affected side. The planning of the orbital shift and excision of the widened nasal bone is shown in the upper row in the picture on the right side. The middle row shows the unilateral orbital box osteotomy markings and the completion of the osteotomy cuts on the operation table. The patient also had nasal augmentation with split cranial bone graft. The picture on the right in the middle row shows well healed medialised orbit and nasal dorsum. The patient also underwent eyebrow correction as a secondary procedure 6 months later. The lower row shows appearance 15 years after the initial surgery.
Figure 11.

A case of craniofacial cleft where unilateral box osteotomy was performed. Upper row shows preoperative appearance and the operative plan. The middle row shows per operative view of the unilateral hypertelorism and the planned and completed osteotomy 15 years postoperative result is seen in the lower row
Facial bipartition
This 6-year-old patient presented with hypertelorism and broad nasal dorsum with ill-defined tip. She also had an angulated maxillary arch with dental malocclusion [Figure 12a, upper row]. She underwent facial bipartition procedure. She also had augmentation of the nasal dorsum with cranial bone graft. The 10 years postoperative picture in the lower row shows stable hypertelorism correction and a well-maintained nasal tip projection.
Figure 12a.

Preoperative appearance of hypertelorism in a 6-year-old child (upper row). The correction was done using facial bipartition technique. The results at 10 years postoperative follow-up (lower row).
The patient in Figure 12b had a very severe ORH (upper row). There maxillary arch was “V-shape and narrow. A facial bipartition procedure was undertaken. However, the postoperative result was not very satisfactory. He would require further refinements in the form soft tissue nasal correction and nasal dorsal augmentation at a later date.
Figure 12b.

A severe case of hypertelorism who underwent facial bipartition surgery (upper row). The 3 months postoperative result are seen in the lower row
Craniosynostosis with hypertelorism
Figure 13 shows a 6-year-old patient having plagiocephaly with hypertelorism. Marked orbital dystopia is also noted (upper row). The plagiocephaly was corrected with an onlay bone graft on the affected side. A box osteotomy was planned on both sides as shown on the CT scan picture in the lower row. The correction was planned with orbital box osteotomy technique as this would permit not only the medialisation of the orbits but would also allow appropriate shift of the orbital boxes to correct the vertical dystopia. The right orbit was shifted inferiorly by removing the bar from the inferior orbital margin, and the left orbit was elevated by keeping a bone graft under the inferior orbital wall. Postoperative appearance after 2 years is seen in the lower row pictures.
Figure 13.
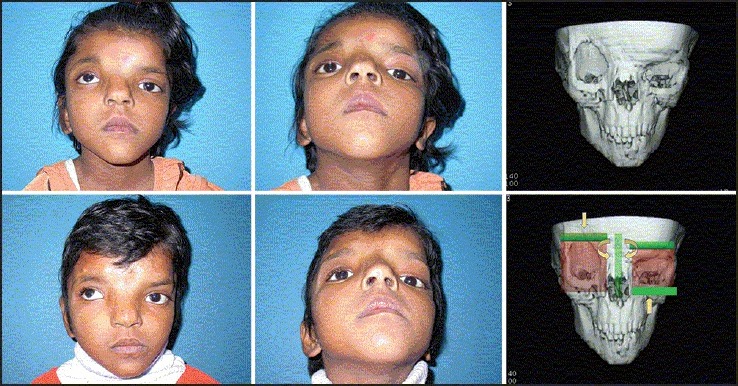
A case of plagiocephaly with hypertelorism. She also has vertical orbital dystopia (upper row) Orbital box osteotomy was done with correction of the dystopia done by using bone grafts to alter the orbital heights as shown in the plan on the CT scan in the lower row. The postoperative picture 2 years later shows stable result
Pseudo-hypertelorism (telecanthus)
Nasofrontal meningo-encephalocele
These patients have increased medial ICD but the position of the bony orbit is normal as can be seen in this patient in Figure 14 (upper row). A defect in the anterior skull base midline leads to herniation of meninges and brain causing increased medial ICD. The patient underwent correction of the meningo-encephalocele using the Chula technique. This technique employs limited access osteotomy and permits removal of the herniating neural tissue and duraplasty as comfortably as with the regular bifrontal craniotomy technique.[21] The defect in the frontal bone and anterior skull base was reconstructed with split cranial bone graft. The nasal dorsum was also augmented with the bone graft. The medial canthopexy was performed on both sides. The lower row shows result 1½ years after the surgery.
Figure 14.

A case of frontonasal meningo-encephaloceles showing telecanthus (upper row). The correction was done using Chula technique and the medial orbital wall was reconstructed along with medial canthopexy. The postoperative appearance 3 years later is shown in the lower row
Post-traumatic telecanthus
The malunited naso-orbito-ethmoid fractures can present with significant telecanthus as shown in Figure 15 (upper row). The splayed bones were contoured with high speed burr. An augmentation of the nasal dorsum was performed using split cranial bone grafts. A medial canthopexy was also done. The lower row shows postoperative results after 3 months.
Figure 15.

Posttraumatic telecanthus following naso-orbito-ethmoid fracture (upper row). She is same patient shown in Figure 4. She underwent contouring of the malunited bone cranial bone grafting of the nasal dorsum and a medial canthopexy. The postoperative picture at 3 months a is seen in the lower row
Craniofacial fibrous dysplasia masquerading as telecanthus
This patient had polyostotic craniofacial fibrous dysplasia leading to obliteration of the nasal airway, and blocking of ethmoidal sinuses and created an increased ICD [Figure 16, upper row]. Extensive contouring of the nasal passages, ethmoids and the maxillae was undertaken. The nasal dorsum was augmented with split cranial bone grafts. Medial canthopexy was also performed. The lower row shows postoperative pictures at 6 months.
Figure 16.

A case of polyostotic fibrous dysplasia giving an appearance of pseudo-hypertelorism (upper row). The excess bone was contoured, a dorsal nasal augmentation was done with cranial bone graft and medial canthopexy was performed. The lower row shows the results 6 months postoperative
COMPLICATIONS
Correction of hypertelorism would necessitate a combined intra-cranial and extra-cranial approach. The ethmoid sinuses are opened up and there is a danger of ascending infection from the nasal passages. The use of fronto-galeal flap can effectively seal this passage and prevent infection.[20] We have had no case of any serious infection in any of more than 70 cases done for correction of this deformity. There is a real danger of vision loss, but with a careful approach these problems can be avoided.
These cases may need small touch up procedures in the form of soft tissue corrections.
DISCUSSION
As can be seen from the above illustrative cases, hypertelorism could be present in a variety of situations. One, however, needs to differentiate between a true ORH and a pseudo-hypertelorism. The former necessitates a far more extensive procedure that is a combination of intra-cranial and extra-cranial approaches. The orbits can be medialised either by box osteotomy technique or by facial bipartition technique. In both technique some surgeons would always like to leave a frontal bando (also known as bar) to guide the movement of the orbits. However others feel that it is not mandatory. The facial bipartition is a better procedure when there are associated dental arch deformities that are seen in cases of Apert's syndrome or other craniofacial cleft cases. The box osteotomy is an elegant procedure and can help one to not only medialise the orbits but also permits correction of vertical orbital dystopia. This technique can be easily adapted to the unilateral ORH. Use of cranial bone grafts after relocation of the orbits adds to stability of the results achieved on the operating table. The medial canthopexy is an important part of the procedure and can bring in dramatic improvement in the result. The authors prefer use of a two-hole plate for securing the canthal tendon at the level of the posterior lacrimal crest.[19]
The surgery has become very safe these days as we are able to separate the nasal cavity from the extra-cranial space by interposition of vascularised tissue such fronto-galeal flaps.
Telecanthus is also known as pseudo-hypertelorism and can be present in cases of nasofrontal meningo-encephaloceles, after trauma or tumours in the naso-orbito-ethmoid region. We need to address only the medial orbital wall in these cases and there is no need for any orbital relocation in these cases.
The excess skin is addressed at the time of primary surgery itself. However in some cases one may need to do minor revisions at a later date.
CONCLUSION
Hypertelorism can occur in a variety of situations such as craniofacial dysplasia, craniofacial clefts and some craniosynostosis syndromes. It may or may not be associated with narrowing of the maxillary arch and dental malocclusions. The indication for surgery is for cosmetic reasons and restoration of body image. The correction can be performed using a combined intracranial and extracranial approach. The orbits can be mobilised into the medial position after removing part of the enlarged nasal and ethmoid bones by using either ‘box osteotomy’ or ‘facial bipartition’ technique. Telecanthus is also known as pseudo-hypertelorism and can be present in cases of nasofrontal meningo-encephaloceles, after trauma or tumours in the naso-orbito-ethmoid region. We need to address only the medial orbital wall in these cases and there is no need for any orbital relocation in these cases.
The morbidity and mortality in these cases is negligible if the ORH correction is carried out in dedicated large volume craniofacial centres.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1. [Last accessed on 2014 Aug 30; at 6.30 pm]. Available from: http://www.medical-dictionary.thefreedictionary.com/hypertelorism .
- 2.Greig DM. Hypertelorism: A hitherto undifferentiated congenital craniofacial deformity. Edinb Med J. 1924;31:560. [Google Scholar]
- 3.Tessier P. Orbital hypertelorism. I. Successive surgical attempts. Material and methods Causes and mechanisms. Scand J Plast Reconstr Surg. 1972;6:135–55. doi: 10.3109/02844317209036714. [DOI] [PubMed] [Google Scholar]
- 4.Vermeij-Keers C, Mazzola RF, Van der Meulen JC, Strickler M. Cerebro-craniofacial and craniofacial malformations: An embryological analysis. Cleft Palate J. 1983;20:128–45. [PubMed] [Google Scholar]
- 5.Poleman RE, Vermeij Keers C. Cell degeneration in the mouse embryo: A prerequisite for normal development. In: Berat VM, editor. Progress in Differentiation Research. Amsterdam: North Holland; 1976. [Google Scholar]
- 6.Mann I. London: Cambridge University Press; 1970. Developmental Abnormalities of the Eye. [Google Scholar]
- 7.Patten BM. 3rd ed. New York: McGraw Hill; 1968. Human Embryology. [Google Scholar]
- 8.Tessier P, Guiot G, Rougerie J, Delbet JP, Pastoriza J. Cranio-naso-orbito-facial osteotomies. Hypertelorism. Ann Chir Plast. 1967;12:103–18. [PubMed] [Google Scholar]
- 9.Tessier P. Total facial osteotomy.Crouzon's syndrome, Apert's syndrome: Oxycephaly, scaphocephaly, turricephaly. Ann Chir Plast. 1967;12:273–86. [PubMed] [Google Scholar]
- 10.Tessier P. Paris: Masson; 1977. Chirurgie Orbito-Palpebrale. [Google Scholar]
- 11.Tessier P. Experiences in the treatment of orbital hypertelorism. Plast Reconstr Surg. 1974;53:1–18. doi: 10.1097/00006534-197401000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Tessier P. Anatomical classification facial, cranio-facial and latero-facial clefts. J Maxillofac Surg. 1976;4:69–92. doi: 10.1016/s0301-0503(76)80013-6. [DOI] [PubMed] [Google Scholar]
- 13.Tessier PL. Facial bipartition. A concept more than a procedure. In: Marchac D, editor. Proceedings of the First International Congress of the International Society of Cranio-Maxillo-Facial Surgery. Berlin: Springer-Verlag; 1987. pp. 217–45. [Google Scholar]
- 14.Converse JM, Ransohoff J, Mathews ES, Smith B, Molenaar A. Ocular hypertelorism and pseudohypertelorism. Advances in surgical treatment. Plast Reconstr Surg. 1970;45:1–13. doi: 10.1097/00006534-197001000-00001. [DOI] [PubMed] [Google Scholar]
- 15.van der Meulen JC. Medial faciotomy. Br J Plast Surg. 1979;32:339–42. doi: 10.1016/0007-1226(79)90095-x. [DOI] [PubMed] [Google Scholar]
- 16.van der Meulen JC, Vaandrager JM. Surgery related to the correction of hypertelorism. Plast Reconstr Surg. 1983;71:6–19. doi: 10.1097/00006534-198301000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Ortiz-Monasterio F, del Campo AF, Carrillo A. Advancement of the orbits and the midface in one piece, combined with frontal repositioning, for the correction of Crouzon's deformities. Plast Reconstr Surg. 1978;61:507–16. doi: 10.1097/00006534-197804000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Marchac D, Renier D, Arnaud E. Infrafrontal correction of teleorbitism. In: Whitaker L, editor. Proceedings from the Seventh Meeting of the ISCFS. Santa Fe: Menduzzi; 1997. pp. 173–5. [Google Scholar]
- 19.Sharma RK, Makkar SS, Nanda V. Simple innovation for medial canthal tendon fixation. Plast Reconstr Surg. 2005;116:2046–8. doi: 10.1097/01.prs.0000192544.20408.65. [DOI] [PubMed] [Google Scholar]
- 20.Jackson IT, Adham MN, Marsh WR. Use of the galeal frontalis myofascial flap in craniofacial surgery. Plast Reconstr Surg. 1986;77:905–10. doi: 10.1097/00006534-198606000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Mahatumarat C, Rojvachiranonda N, Taecholarn C. Frontoethmoidal encephalomeningocele: Surgical correction by the Chula technique. Plast Reconstr Surg. 2003;111:556–65. doi: 10.1097/01.PRS.0000040523.57406.94. [DOI] [PubMed] [Google Scholar]


