Abstract
A non-healing wound is defined as showing no measurable signs of healing for at least 30 consecutive treatments with standard wound care.[1] It is a snapshot of a patient's total health as well as the ongoing battle between noxious factors and the restoration of optimal macro and micro circulation, oxygenation and nutrition. In practice, standard therapies for non-healing cutaneous wounds include application of appropriate dressings, periodic debridement and eliminating causative factors.[2] The vast majority of wounds would heal by such approach with variable degrees of residual morbidity, disability and even mortality. Globally, beyond the above therapies, newer tools of healing are selectively accessible to caregivers, for various logistical or financial reasons. Our review will focus on the use of hyperbaric oxygen therapy (HBOT), as used at our institution (CAMC), and some other modalities that are relatively accessible to patients. HBOT is a relatively safe and technologically simpler way to deliver care worldwide. However, the expense for including HBOT as standard of care for recognized indications per UHMS(Undersea and Hyperbaric Medical Society) may vary widely from country to country and payment system.[3] In the USA, CMS (Centers for Medicare and Medicaid Services) approved indications for HBOT vary from that of the UHMS for logistical reasons.[1] We shall also briefly look into other newer therapies per current clinical usage and general acceptance by the medical community. Admittedly, there would be other novel tools with variable success in wound healing worldwide, but it would be difficult to include all in this treatise.
KEY WORDS: Wound Healing, hyperbaric, oxygen, UHMS, TCOM, Mental Health, Obesity, Diabetes, Compartment syndrome
INTRODUCTION
HBOT, as an effective tool helping wound healing, is defined as delivering 100% oxygen above one atmospheric pressure (ATA) into the core of the wound.[4] This increased amount of oxygen delivered at the cellular level of unhealed tissues helps expedite healing of sub-acute and chronic cutaneous and epithelial surface wounds.[5] This article will survey HBOT and other tools including standard wound care, growth factors, pressure off-loading, and anabolic steroids in wound healing. Overall, delivering wound healing in a cost effective way can be a challenge for various reasons. Improving access and delivery of health care globally remains our goal. It is a team effort by the willing including the patient, for total care to healing.
BACKGROUND
Current paradigm
Standard wound care, as briefly described below, remains the mainstay of treatment. The final common pathway to healing by repair is reversal of tissue hypoxia by mitigating the noxious factors, restoring the healing factors, using antibiotics for soft and hard tissue infection, addressing general medical and mental health issues (e.g. diabetes, heart failure, major depression etc…) comprehensively.
Nutrition
Other key steps include restoring nutrition, off-loading the wound over the bony prominences (e.g. bed sores, sole of the foot ulcers) and monitoring transcutaneous oxygen measurement around the wound is the most cost effective way to evaluate the macro and microcirculation to the target tissue as well as the prospect for healing.
Protective senses
Improving protective senses for neuropathic ulcers by decompression as in diabetes or leprosy, for example, is invaluable. Importing a sensate flap into the insensate target area may prevent re-ulceration in paralytic patients.[6]
Uncommon ulcers
A cutaneous biopsy may be needed for understanding atypical ulcers that do not heal with standard care, such as those caused by cancer or by pathological microorganisms, such as bacteria, parasites, fungi, or actinomycoses present endemically worldwide.[6]
A total care approach is integral to get the patient back to his or her social and work life at the soonest and stay healed for the longest time. Ambulatory wound care is the order of the day. Due diligence in prevention in all aspects of wound healing could not be over emphasized. It cuts cost, healing time, and prevents recurrence through aggressive patient education.
Infection control: Appropriate antibiotic usage per culture and sensitivity report is essential to treat any underlying infection of soft tissues and bone e.g. osteomyelitis as well as minimize developing drug resistance.
Medical management of the underlying cause of non-healing e.g. Diabetes treatment keeping HbA1C under 7.0, eliminating lower extremity edema, minimizing heart failure, preventing respiratory failure, correcting anemia to an optimal level, and restoring nutrition by monitoring Prealbumin level. Monitoring serum creatinine, glomerular filtration rate (GFR), Vitamin D, B12, Folate, and iron metabolism in chronic renal disease is important.
-
Mechanical off-loading of the pertinent body anatomy:
- Sole of the foot ulcer: Using an appropriate total contact cast, targeted offloading by custom-made foot wear in ulcers on the sole of the foot.[7]
- Decubitus ulcers: Prevention is the best cure for decubitus ulcers. It is not unusual that patients come through critical medical and surgical challenges through highly technical and expensive medical care yet suffer from a prolonged non-healing wound.[8] Much of it is preventable by dogged attention to pressure points as well as addressing global medical issues playing in the backdrop[8]
- Prevent prolonged pressure (realign) Decubitus ulcer or bed sores are often triggered by undue sustained pressure, usually more than two hours at a time, in one body habitus.[8] It is the dominant pathophysiology behind skin breakdown in wide variety of patients e.g. in post stroke, post trauma paralytics, chemically paralyzed while on ventilator, and infirmity from any cause.[8]
For prevention, it requires optimally turning, usually every two hourly, preferably with specialized offloading beds and innovative mattresses as bed cushions.[8]
Lack of optimal tissue perfusion, nutrition, physical therapy, prevention of deep vein thrombosis, and keeping stool and urine away play a significant role. Dogged vigilance against decubitus ulcers is the best protection.[8]
-
d.
Quit Smoking
-
e.
Quit Chemical dependence cessation.
-
f.
Life style modification for better health and nutrition, at all stations in life.
-
g.
Addressing general medical and mental health adequately.
-
h.
Garnering help from appropriate Specialists e.g. Vascular, Plastic, Neuro or Orthopedic surgeons is invaluable.[9] Emerging medical sciences and technology should be rigorously tested before being part of the main stream paradigm to the world of wound care.
-
i.
It is a team effort by the willing including the patient, for total care to healing.
With inadequate circulation due to any cause e.g. arteriosclerosis, Diabetes, venous stasis, morbid obesity, peripheral vascular disease (PVD), and vasculitis etc., wounds may not heal, despite treatment delivered per standard of care, with or without HBOT.[9] Chronic vasospasm can be a cause of insufficient blood flow, due to conditions such as Raynaud's disease, cold agglutinins (autoimmune hemolytic anemia), or chronic tobacco abuse may delay wound healing.[9]
Other systemic conditions that may cause clinically significant tissue hypoxia are congestive heart failure, terminal chronic obstructive pulmonary disease (COPD), chronic lymphedema or chronic venous edema of morbid obesity alone from any cause, and obstructive sleep apnea while asleep may compromise healing.[9] Dependent edema from any cause is detrimental to healing. Thus, all of these illnesses either alone or in combination, if present, must be addressed by a designated physician to give the best chance at wound healing. In the presence of mental health issues and personality disorders where the patient is not part of the solution, a non-healing of wound may persist.
Hyperbaric Oxygen therapy
Definition
HBOT, as an effective tool helping wound healing, is defined as delivering 100% oxygen above one atmospheric pressure (ATA) into the core of the wound.[2] Per UHMS (Undersea and Hyperbaric Medical Society)[3] guidelines, HBOT pressurization should be 1.4 atmospheres (ATM) absolute pressure or higher.
In practice, the UHMS and CMS approved definitions for HBOT are similar.[1] This increased amount of oxygen, delivered by HBOT to the cellular level of unhealed tissues, helps expedite healing of various sub-acute and chronic cutaneous and other epithelial surface wounds.[5] However, HBOT doses delivered, in practice, may be variable around these recommended doses depending on local logistical issues.
In spite of existing comorbidities, HBOT can deliver increased amounts of oxygen to local tissues. Hence, HBOT can be used to help expedite healing of various subacute or chronic wounds.[5] For example, the adjunctive use of HBOT in chronic diabetic foot ulcers is well-established.[10] The need for an individualized approach for any complex wound could not be over emphasized. Hence, a systematic review indicates that HBOT is useful as an adjunctive super-tool in healing various wounds while standard medical treatment alone faces stalled healing process in any given ulcer. HBOT is used in diabetic foot ulcers, crush injuries, burns, split-skin grafts and flap covers to name a few.[5]
It is important to note that topical oxygen (e.g. Topox) applied by placing a small chamber of pressurized oxygen over an extremity, is NOT equivalent to hyperbaric oxygen.[9] The patient must breathe the pressurized oxygen, as with HBOT, to allow oxygen to deeply penetrate wounds and provide true wound healing benefit.[9] Topox, a topical oxygen application, is neither covered by insurance companies for monetary compensation nor endorsed by the journal of Diabetes Care for the treatment of foot ulcers.[9]
A brief history of HBOT
Recruiting new blood to enhance perfusion and oxygenation by turning a skin flap is an age old technique in wound healing.[11] In the 6th century BC, Sushruta did this by his, now famous, Indian Rhinoplasty.[11] He pioneered a forehead or cheek flap. Hence today, a pedicled forehead flap is referred to as the Indian flap.[11] It was not until 1895 when hyperbaric oxygen was used as medicine to improve oxygenation.[9] In 1895, Haldane, first demonstrated with evidence the benefit of HBOT at 2 ATA in CO poisoning. About 100 years later, in 1999, HBOT was used in mainstream medicine.[9]
Pathophysiology of HBOT[12]
Hyperbaric oxygen works to help heal these various conditions by four dominant mechanisms (see Figure 1 for detailed mechanisms). Those are as follows.
Figure 1.
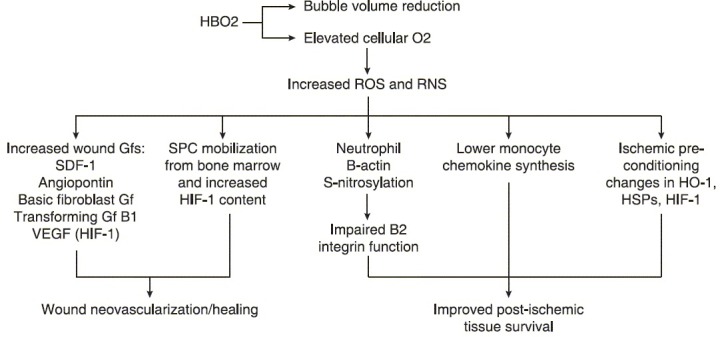
Pathophysiology behind improved wound healing of hyperbaric oxygen therapy,[49] HBO2 reduce bubble volumes and elevate cellular pO2 leading to increased production of ROS (reactive oxygen species) and RNS (reactive nitrogen species). GFs (growth factors); VEGF (vascular endothelia growth factor); HIF-1 (hypoxia inducible factor-1); SPCs, (stem/progenitor cells); HO-1 (heme oxygenase-1), HSPs (heat shock proteins).
Hyperoxygenation: HBOT increases concentration of oxygen in blood, dissolved in the plasma, due to the increased partial pressure of oxygen at the alveoli.
Decrease interstitial tissue edema: By reducing edema by 20% through the reabsorption of tissue fluids. Mechanisms include facilitatory vasoconstriction, despite no hypoxia, causing decreased tissue edema at the site of trauma and inflammation. Resulting vasoconstriction favorably reduces inflow of blood by approximately 20% while maintaining adequate outflow of blood, thus, reducing edema by 20%. This is helpful with decompression in compartment syndrome and reducing interstitial edema in a flap.
Augmented hydroxylation: Help improve collagen synthesis. Also HBOT provides increased oxygen needed for hydroxylation that occurs in collagen synthesis during wound healing.
Angiogenesis: HBOT creates a large oxygen gradient between the center and periphery of the wound, causing a strong stimulus for angiogenesis which is seminal in wound healing.[12]
Bactericidal activity: Increased
Collagen deposition: Increased
Nitric Oxide (NO) production in the target tissue is increased[12]
HBOT, by increasing the diffusion distance of oxygen, helps ischemic tissue fields, overlapping one another but now re-perfused with oxygen. Hence it obliterates the blind spots of hypoxia in the core of the unhealed wound.
The partial pressure of oxygen at the tissue level rises to about 1400 mm of Hg in the HBOT chamber. Subsequent HBOT treatments, play a facilitatory role, causing an “oxygen bump” to initial pO2 at the core tissue, and help augment oxygenation and healing. In practice, twice a day HBOT treatments thus become not that cost-effective.
These physiologic benefits of HBOT not only cause immediate improvement in tissue perfusion and oxygenation, but also create a sustained advantage for wound healing process. Depending on tissue elasticity, the sustained benefit of HBOT, post-treatment, may last from 2-8 hours. HBOT causes increased bactericidal activity, angiogenesis, and collagen deposition that are cumulative.[13] Though bacteria are killed during HBOT, the bacterial count cannot bounce back to pre-treatment level for hours after HBOT is completed for the day.[13] NO (Nitric Oxide) production in the target wounds also rises temporarily, leading to increased microcirculation and tissue perfusion.
Kalani et al. (2002) showed that using HBOT for diabetic foot ulcers, (stay) healed completely in 76% of patients, treated after 3 years of therapy, whereas only 48% (stay) healed completely with conventional treatment.[14] In a randomized study by Kessler et al. (2003), HBOT versus standard treatment were given to 28 hospitalized patients with neuropathic ulcers (Wagner grade I to III). After two weeks of treatment, the reduction in ulcer area was doubled in the HBOT group (41.8 +/- 25.5 vs. 21.7 +/- 16.9%, P = 0.037). This improvement however disappeared at the two week follow-up.[15] A retrospective study by David et al. (2001) on treatment outcomes involving hyperbaric oxygen and osteoradionecrosis (ORN) showed that, when HBO was used as the sole treatment for patients with overt ORN, success or improvement occurred in 94.7% of patients.[16] Figure 1a below, illustrates numerous studies, one with 469 patients, that exemplify the increase in healing and decrease in amputations associated with using HBOT with standard wound care.
Amputations
In our study at CAMC of 72 patients, 16 patients required amputations of various sorts. Fourteen of sixteen (87.5%) of these patients had diabetes. Nationally, more than 60% of non-traumatic lower-limb amputations occur in people with diabetes.[17] In 2006, about 65,700 non-traumatic lower-limb amputations were performed in people with diabetes.[17]
Figure 3 illustrates US census data of lower extremity amputation rates in a diabetic population from 1988 to 2009.[38] As evidenced from the graph, amputation rates range from 9 per 1000 in 1988, to a maximum of 11/1000 in 1996, to about 3 per 1000 in 2009.[20]
Figure 2b.
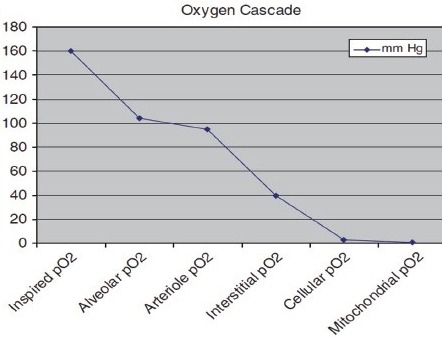
The diffusion gradients along the oxygen supply chain to the tissues of normal body at sea level. Modified with permission from Nuu's applied respiratory physiology[11] (Elsevier Publishing Inc.)
The various studies, shown in Figure 2a, demonstrate how HBOT decreases amputation rates in diabetic populations.
Figure 2a.
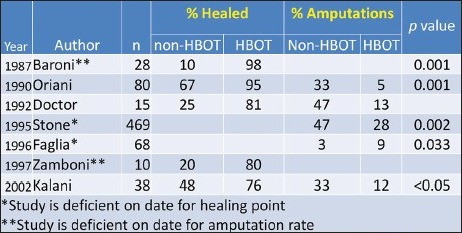
This table shows numerous studies from 1987 to 2002 that show the benefit of hyperbaric oxygen therapy (HBOT). HBOT significantly increases the percentage of patients that will heal completely and minimizes the number of amputations relative to standard wound care alone[3]
Comorbidities
Published literature is rather sparse in reporting concomitant medical conditions, which are suspected to delay wound healing. The identified conditions that can contribute to delayed wound healing are Heart failure, chronic obstructive pulmonary disease (COPD), those on dialysis, and anemia of chronic kidney disease (CKD), liver dysfunction, hypoproteinemia, anemia of chronic illness, rheumatoid arthritis, gout, immune suppression (i.e. as in long-term steroid use. Lack of adequate nutrition, financial and physical support for activities of daily living (ADLs), poor mobility etc., delay healing.
Mental Health: Similarly, personality disorders affecting meaningful compliance, lack of drive and motivation, concomitant major depression, bipolar disorder, schizophrenia and combination thereof, delay healing. Other factors like morbid obesity, uncontrolled chemical dependence, excessive smoking affect microcirculation and macrocirculation.[1]
CKD is often closely linked to diabetes mellitus. Patients with CKD stage III/IV should be weighed naked prior to HBOT to avoid respiratory distress from fluid overload.[21] Daily naked weight before treatment is a cheap, but reliable, way to measure CKD and CHF for practical purposes.[21] Monitoring microalbumin in urine is a useful marker of advanced CKD particularly in the presence of diabetes mellitus.[21]
Blood glucose in HBOT
A study by Uhlmeyer et al. (2005) studied how blood glucose changes with hyperbaric oxygen treatment.[22] They studied 2,459 patients who received 57,124 HBOT treatments, averaging 23.4 treatments per patient. The authors noted a decrease in blood glucose in 79% of patients presenting with a glucose level greater than 150 mg/dl. Only 46% of patients who were fed before HBOT showed a decrease in blood glucose. Despite feeding, blood glucose dropped below 100 mg/dl after HBOT in 19.6% of patient treatments. Uhlmeyer et al. (2005) had an incidence of 0.8 symptomatic or asymptomatic hypoglycemic events per 1000 patient treatments, 1.6 events per 1000 diabetic patient treatments, and 0.05 events per 1000 diabetic patient treatments with protocol.[22]
Hypoglycemic events are more dangerous than hyperglycemia. At the CAMC Wound Care center, patients may eat their regular breakfast before their blood glucose is checked prior to getting in the chamber. We watch closely for hypoglycemic behavior in the chamber, such as sweating, jitteriness, etc. It takes nine minutes to dive out of depth, so this means it takes nine minutes for any intervention for a hypoglycemic event. At CAMC, insulin-dependent diabetic patients are individualized based on their glycemic response to HBOT.
We, at the Charleston Area Medical Center Wound Healing Center (CAMCWHC), have developed an empiric clinical approach to prevent hypoglycemic episodes. Before HBOT, the patient is left at 200 mg/dl+ and blood glucose is re-checked after treatment. If the blood glucose is less than 150 mg/dl after treatment, the patient is given a sugar rich snack before their next treatment. This prevents hypoglycemic events or seizures. The glycemic response under HBOT is individualistic and needs a prospective multi-center study with a large number of patients.
Sleep apnea
Sleep apnea is becoming a more common problem associated with the rise in obesity and diabetes for lac of adequate physical activities! It is also becoming an independent factor that delays wound healing, as the link between sleepapnea, insulin resistance and glucose intolerance become more clear.[23] Sourabh B. and Vishwanath G. (2012) state that HBOT improves microcirculation through hyperoxia and an anti-edema effect.[12] HBOT improves microcirculation through reduction of reperfusion injury and “no reflow” phenomenon.[12]
This vasoconstriction, does not cause hypoxia at the target tissue as this is over compensated by increased plasma oxygen content and microvascular blood flow.[12]
Recall the “oxygen bump” indicates once daily HBOT is just as effective as HBO treatments over two or three times a day. Further, it illustrates how the benefit of 2 hours of HBOT treatment benefit lingers on for many hours. Minimizing the hypoxia time during over- night sleep e.g. in obstructive sleep apnea, using calibrated continuous positive airway pressure (CPAP) maintains the patient's physiological oxygen saturation overnight.
CPAP is continuous, to provide constant pressure, and it is positive, to prevent airway collapse, thus ensuring adequate oxygen flow throughout all stages of sleep.[24] CPAP, delivered by facemask overnight, shows benefit for the majority of mild to moderate obstructive sleep apnea patients.[24] One study by Naeser et al. (2010) showed that CPAP restores adequate oxygen flow throughout all stages of sleep and may improve cognition in post-stroke patients.[25]
We postulate that whatever gains the patient makes in oxygenation in ulcers, HBOT treatment benefit would be blunted by facing hypoxia for eight hours every night in people with Sleep apnea. We would like to investigate the hypothesis that patients with obstructive sleep apnea being treated with HBOT, will maintain a more of a physiologic oxygen level and promote improved healing by adding CPAP therapy in them.
A study by Weinstock et al.(2012) showed that, with CPAP, insulin sensitivity improves in those with an apnea-hypopnea index ≥30.[24] This suggests beneficial metabolic effects of CPAP in severe OSA. Thus, treating patients with CPAP in severe OSA may improve wound healing in chronic diabetic ulcers with edema. A prospective random study is overdue in here.
Sleep disorder and poor wound healing
Insufficient sleep is linked to an increased risk for the development of Type 2 diabetes.[23]
Sleep apnea and atherosclerosis appear to share some common physiological characteristics, further suggesting that sleep apnea may be an important predictor of cardiovascular disease.[26]
Increased neck size in obese people, was the strongest predictor of sleep disordered breathing among all anthropometric variables.[27]
In our populations, a neck circumference above 43 cm positively correlates to OSA. CPAP support during sleep is the most cost effective remedy for OSA.[23]
Diabetes, obesity, sleep apnea and non-healing foot ulcers: Some salient facts
Diabetes is by far the most common cause of foot ulcers worldwide.[28]
Comorbidities like sleep apnea and obesity compound the challenges of non-healing wound.[28]
Persons with diabetes are at higher risk for both cardiovascular and microvascular disease.[26]
There is a significant and consistent association of diabetic complications and depressive symptoms.[29]
Obesity-related conditions include heart disease, stroke, type 2 diabetes and certain types of cancer, some of the leading causes of preventable death.[20]
West Virginia had a prevalence of diabetes equal to or greater than 30%[20] Now, obesity is becoming an epidemic in the first world.[31]
Lower extremity diabetic wounds
A diabetic foot wound is the most common cause for hospitalization of patients with diabetes.[6] The most significant risk factor for ulceration of a diabetic foot is the presence of neuropathy; therefore, basic care of the neuropathic diabetic foot is essential.[6] For Wagner grade III and IV diabetic ulcers,[32] there are seven elements to standard wound care- correcting vascular insufficiency, nutritional status, glycemic control, debridement, dressing, off-loading, and resolving infection. If there is no significant decrease in wound size in 30 days, then HBOT should be initiated. Given the multiplicity of complications associated with diabetes, it is always important to address every aspect of the disease to ensure wound healing.
Calhoun et al. (2002) listed six essential steps to caring for a neuropathic diabetic foot to prevent ulceration.[6] These steps, as listed below, are necessary before consideration of HBOT.
We included these seven steps for the sake of completion.
Daily inspection of the toes and feet for protective sensation and infection.
Wear well-fitting shoes and socks and to inspect their shoes daily for foreign objects, and in the absence of protective sensation, irregularities that can cause wounds.
Toenails should be trimmed without any injury to the skin.
Wash their feet daily and remove any harmful agent.
Lotion should be used to avoid dryness and cracking of the skin.
Exercise, proper nutrition, and smoking cessation.[6]
Periodically check for microalbuminuria, hypertension, smoking, infection, HbA1c titrated to around 6.5%, eye exam, and renal function (serum creatinine, estimated GFR, significant anemia, Vitamin D level) in CKD III-IV.
Diabetes combined with reduced blood flow, mechanical and chemical neuropathy in the feet increases the chance of foot ulcers, infection and eventual need for limb amputation.[28] Kalani et al. (2002) studied 38 patients with chronic foot ulcers where patients had diabetes for a mean duration of 27 years.[14] Their baseline trans-cutaneous pressure of oxygen (TcPO2) was under 40 mmHg. Seventeen of the patients received HBOT while 21 received standard wound care alone. At three years out, 76% of the patients in the HBOT group healed with intact skin whereas only 48% in the standard wound care group healed. Thirty-three percent of the control group required amputation, while only 12% of the HBOT (treated group) required amputation. Blood pressure, HbA1c, diabetes duration and base TcPO2 values were comparable in both groups.[14]
Along with standard wound care, newer techniques such as tarsal tunnel decompression are being used to restore sensation in feet with established ulcers.[7] Tarsal tunnel syndrome is an entrapment neuropathy caused by pressure on the posterior tibial nerve as it passes posterior and inferior to the medial malleolus beneath the fibrous origin of the Abductor Hallucis muscle.[33] Baba et al. (1997) studied 34 patients who had posterior tibial nerve decompression and found that better outcomes occurred when there was a short history, the presence of a ganglion, no sprains, and light work.[33]
It is also worth noting the peripheral neuropathy and neuropathic pain are not unique to diabetes. In countries like India, Leprosy can be significant cause of neuropathic pain.[34] Estrella et al. (2011) studied 101 patients in Mumbai treated with multi-drug therapy for leprosy and found that 21.8% had neuropathic pain, including numbness, tingling, hypoesthesia to touch and pinprick.[35] The neuropathic pain was also associated with nerve enlargement and tenderness, painful skin lesions, and psychological morbidity.[35]
Mental health
Mental health may be a progressively challenging issue causing non-healing: There is a significant and consistent association of diabetes complications and depressive symptoms.[29]
We are specifically concerned about impact of mental health in general and depression in particular, and its impact to the wound healing industry. Today an estimated 18.8 million Americans suffer from depressive disorders, including depression, dysthymic disorder or bipolar disorder.[36]
They have significant influence on the outcome data in wound healing. Based on our clinical experience at CAMC, patients with untreated or undertreated depression are more likely to not begin or discontinue HBO treatment. In fact, the prevalence of depression, bipolar disorder and anxiety in our HBO-treated population (n = 72) was nearly twice that of the estimated national prevalence (19.4% versus 9.0% in USA).[36] A study in 2004 (Goldney et al.) showed that the prevalence of depression in a diabetic population was 24% compared with 17% in a nondiabetic population (n = 3010).[37]
We found it important to spend time assessing barriers, real or imagined, that prevented the patient from continuing treatment as well as prevention of recurrence of ulcers. In our experience, a dose of short acting benzodiazepine, like alprazolam, prior to entering the HBOT chamber, can alleviate most acute confinement anxiety. However, the physician should be vigilant against chemical dependence in the long run. Furthermore, in our general experience, patients with depression and personality disorders are more apathetic in taking care of their health, including foot ulcers, diabetes and otherwise. This association further supports the notion that it is vitally important to assess for mental health issues prior to beginning of HBOT. A prospective study would be useful to assess the impact of mental health on the outcome as well as economics of wound healing.
Trans-cutaneous oxygen measurement (TCOM) is the best indicator for cost: benefit and risk: benefit analyses[38]
If a patient has a CMS-approved indication for HBOT, then trans-cutaneous oxygen (TCOM) is used to predict the potential outcome.[39]
Clinically, TCOM helps decide:
Is the Wound healing complicated by hypoxia?
When present, is hypoxia reversible?
Is the patient responding to HBOT?
Has the patient reached the therapeutic endpoint?
If TcpO2, in room air value is less than 40 mm of Hg, there is a progressive compromise in healing. For angiogenesis to occur, fibroblasts and vascular endothelial cells must replicate. These cells replicate most rapidly at TcpO2 of 40 mmHg and above [Figure 2b]. TCOM is the best indicator for cost: benefit and risk: benefit analysis.[38,40]
This procedure involves placing oxygen sensors around the wound and measuring oxygen saturation before and during hyperbaric oxygen challenge. Without diabetes and tissue edema, wounds are likely to heal if oxygen tension is greater than 40 mmHg Figure 2b. With diabetes, increased oxygen tension is needed. Patients with values of <20 mmHg are severely ischemic and are likely to need revascularization procedures for wound healing. A meta-analysis of four studies found a more than threefold risk of developing a chronic wound healing complication in patients with a TcpO2 below a threshold of 20 to 30 mmHg (odds ratio 3.26, 95% CI 1.07-9.69).[38,40] A challenge of hyperbaric oxygen (HBOT) can improve the intracellular and subcellular oxygen levels. TCOM helps detect if this increase in microscopic oxygen levels will likely lead to clinical benefit.[38]
Figure 3.
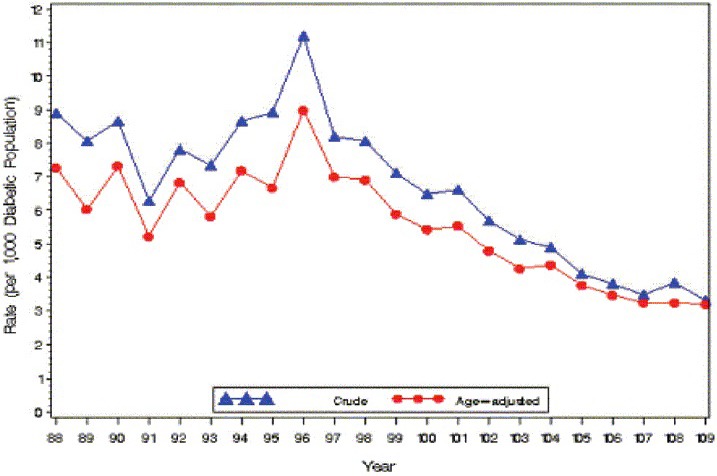
Crude and age-adjusted hospital discharge rates for nontraumatic lower extremity amputation per 1,000 diabetic population, United States, 1988-2009[38]
It is vital to improve the TCOM values e.g. by proximal macro revascularization before contemplating HBOT to be in tune with the cost: benefit and risk: benefit analysis at its best.
By pass surgery vs. stenting: TCOM also can help indicate whether bypass may be appropriate. Generalized vascular narrowing, multiple short segments of narrowing, or vasculitis may indicate bypass surgery as opposed to stenting for localized narrowing. In the case of localized narrowing, a stent would be placed where there is that single point of obstruction.
In summary:
Patients with TCOM values of <20 mmHg are severely ischemic and are likely to need revascularization for wound healing.[38,40]
Need for bypass could occur past the documented narrowed segment, as indicated by CT angiogram. However, with femoral bypass or femoral-popliteal bypass for example, these bypasses can be done only so far distally because the arteries (significantly) decrease in size.[38,41] Less than 1 mm diameter of the vessels makes bye pass anastomosis harder to do. However, Robotic surgery may overcome that hurdle to some extent in future.
Lastly, TCOM may be used as a pointer to help decide amputation level as well as how well an amputation stump wound will heal.[41]
However, surgical level of amputation depends on lifestyle, accessibility and affordability.[41] General infirmity and old age may pose some challenges.
Contraindications for HBOT
Absolute contraindications to HBOT include untreated pneumothorax, a history of spontaneous pneumothorax, or chemotherapy with certain agents (bleomycin, cisplatin, Adriamycin, disulfiram, or Sulfamylon).
Relative contraindications include seizure disorder or possible cocaine use. High fever, retinal or middle ear surgery, CHF, cataract exacerbation, systemic viral infections, spherocytosis, and optic neuritis are some other conditions where you would want to take caution.[3]
There would be other significant causes, prevalent in specific parts of the world including difficulty to access adequate health care delivery e.g. in the third worlds as in Sub Saharan Africa.
Complications of HBOT
Each patient's individual outcome not only depends on how well the wound had healed, but also if they experienced any untoward complications during the course of treatment which are recognized to be HBOT-related.
There are a few possible complications of HBOT including ear pain, confinement anxiety, a hypo and hyperglycemic event, shortness of breath (SOB), a seizure out of medical condition or chemical dependency e.g. cocaine abuse, para-nasal sinus pain, or chest pain[9] [Figure 4]. Serious complications include myopia lasting weeks or months, sinus damage, ruptured middle ear, and lung barotrauma. This risk, however, is decreased with “air breaks”. Air breaks are when the patient breathes normal room air for short periods during treatment.[42]
Figure 4.
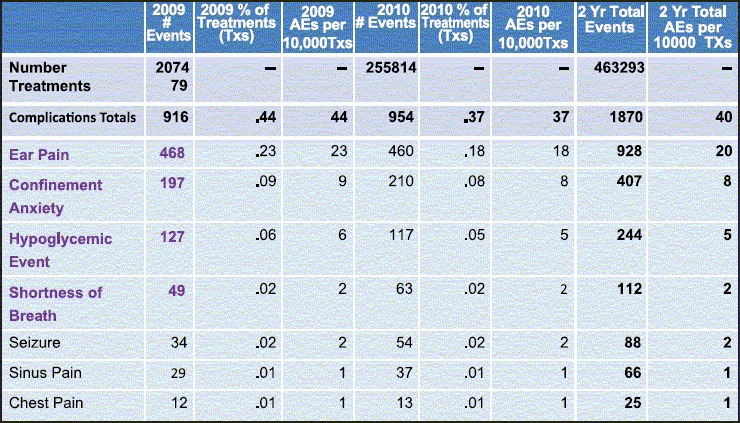
Summary of corporate data by diversified clinical services[48]
Any clinician should be aware of the symptoms of possible middle ear barotrauma. These include dizziness and ear pain specifically with certain otoscopic findings, shown in Figure 5 below.[17] This barotrauma may need urgent myringotomy and tube placement to equalize the pressure.[17]
Figure 5.
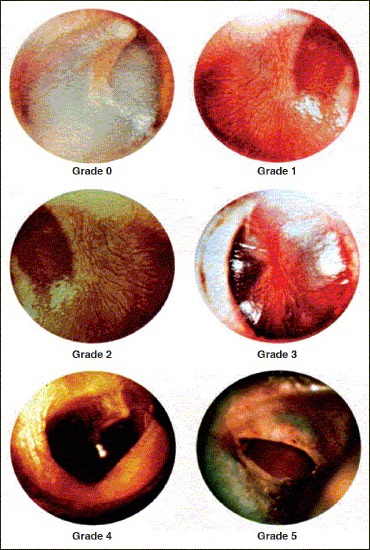
Otoscopic findings in middle ear barotrauma related to hyperbaric oxygen
Adverse event data is entered concurrently in a central proprietary database. An adverse event data dictionary defines each adverse event. Reporting data was reviewed from 463,293 monoplace hyperbaric oxygen treatments provided in hospital based outpatient settings involving 17,267 patients (average of 27 treatments per patient). Air brakes were provided for all treatments at pressures greater than 2.0 ATA. The 2 year total of adverse events per 10,000 treatments were 20 for ear pain, 8 for confinement anxiety, 5 for hypoglycemic event, and 2 for shortness of breath[4] [Figure 4].
Finally, each patient's individual outcome not only depends on how well the wound had healed, but also if they experienced any untoward complications during the course of treatment which are recognized to be HBOT-related. Again cost: benefit and risk: benefit analysis should include these factor.
Inclusion criteria for HBOT[4]
hen a patient meets these inclusion criteria and TCOM has shown adequate oxygenation with hyperbaric oxygen, HBOT can be an attractive choice.
Peripheral arterial insufficiency with poor TCOM response.
Chronic refractory osteomyelitis, hitherto unresponsive to conventional medical and surgical management
Osteoradionecrosis (ORN) e.g. of the mandible, as a complication of conventional radiation treatment of established cancer in the Head and Neck region.
Soft tissue radionecrosis as a complication of conventional radiation treatment, e.g. Head and Neck cancer. Recent advances in Radiation treatment planning and delivery systems have improved such outcome.
Unintended painful periosteal injury from the radiation beam
-
Diabetic wounds of the lower extremities in patients who meet the following three criteria
- Patient has type I or type II diabetics and has a lower extremity chronic wound that is due to diabetes;
- Patient has a wound classified as Wagner grade III or higher; and
- Patient has failed an adequate course of standard wound therapy (30 days of conventional treatment)
Decubitus ulcers with neuropathy including paraplegia[1]
Exclusion criteria for HBOT
Per UHMS (Undersea and Hyperbaric Medical Society)[3] general guidelines, HBOT pressurization should be 1.4 atmospheres (ATM) absolute pressure or higher. However, specific guidelines that dictate the pressure, daily treatment duration, and number of treatments are established per recommendations of the UHMS:[3] Those guidelines are included as an attachment to the data collection form.
Psychiatric diagnosis: Major depression, dementia and other personality disorders in patients should be judged on a case by case basis.
Conservative care: When the reasonable possibility of healing is strongly questionable, under the given circumstances and limitations. For statistical purposes, patients were diverted into conservative care for the purposes of this study. However, their meaningful treatment of non-healing wound was not withheld.
Cocaine abuse: May trigger an unpredictable seizure while in the HBOT chamber and that could require a hazardous rescue exercise. It may be not be wise to offer HBOT in spite of valid a medical indication as the risk and benefit ratio is unfavorable and withholding HBOT from such patient may be prudent.
-
Severe congestive heart failure.
- HBOT can decrease heart rate while maintaining stroke volume which may cause decrease in cardiac output/minute. Simultaneously, through systemic vasoconstriction, HBOT increases afterload. This combined effect can exacerbate congestive heart failure in patients with severe disease.[9]
- Heart failure patients an ejection fraction <30%, is considered high risk for HBOT.[21]
Advanced chronic obstructive pulmonary disease (COPD), as it may obliterate the central respiratory drive.
Upper respiratory tract infection and
Chronic sinusitis,
Retinal surgery in the last 6 weeks,
A patient with a seizure disorder.
Untreated Claustraphobia.[42]
When a patient falls into the inclusion criteria and TCOM has shown adequate oxygenation with hyperbaric oxygen, one can begin treatment per protocol which typically lasts for 118 minutes. This protocol includes 90 minutes of hyperbaric oxygen, two 5 minute air breaks, and it takes 9 minutes to get to and from targeted ATM pressure. This 9 minute “dive” of ascent and decent into ATM pressure, prevents decompression sickness. The exact number of HBOT treatments depends on the clinical response of the patient. Figure 6 shows the recommended number of HBOT treatments for the varying indications, such as diabetic ulcer or crush injury. The dose of oxygen is typically 2.5 atmospheres (ATA) for 90 minutes, while the maximum dose is 3.0 ATA per recommendation of the UHMS (Undersea Hyperbaric Medical Society).[42] HBOT in higher doses (>3 ATA) can trigger oxygen toxicity and could cause damage to the lung or brain.[43]
Figure 6.
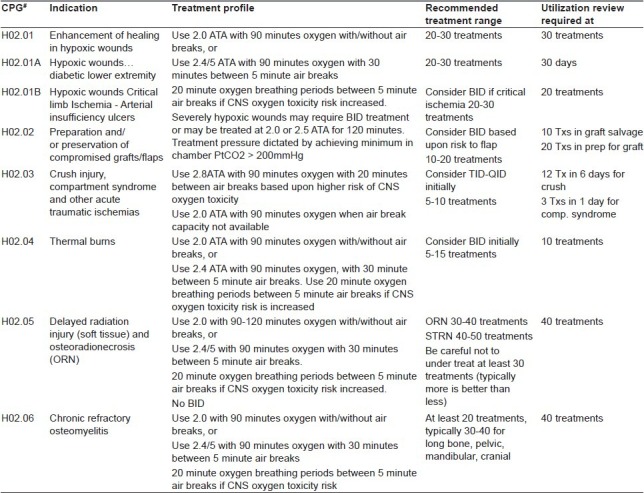
Summary of recommended HBOT treatment protocol for varying indications (per UHMS) with some local modifications for logistical reasons recommended by Diversified Clinical Sciences[19]
Monoplace versus multiplace chambers
Leach et al. (1998) notes that monoplace and multiplace chambers are available options for administering hyperbaric oxygen treatment.[44] Choice of the chamber is driven by logistics and risk of nosocomial infection. A Multiplace chamber is larger in size and where multiple patients can receive treatment simultaneously or where care givers can accompany patients during therapy. Multiplace chambers are particularly useful for critically ill patients who require treatment for acute problems. An assistant could deal with acute problems, like pneumothorax, if they arise unexpectedly. Claustrophobia should not be an issue either with a multiplace chamber. Additionally, multiplace chambers offer benefits such as reduced fire risk since patients receive hyperbaric oxygen via a tight fitting mask in a chamber filled with room air in composition. With these benefits, however, there is also a risk of cross-infection when used for ulcers with complex infection. Lastly, the multiplace chambers are not easily portable and also more expensive relative to monoplace HBOT chambers.[44]
When a patient meets the inclusion criteria and TCOM has shown adequate oxygenation with trial hyperbaric oxygen, the treatment per protocol is offered.
Radiation injury and HBOT
Indications
Today, Radiation-induced ulcers are uncommon when proper precautions are observed. However, such radiation ulcers remain a possible indication for using HBOT. Besides anatomical healing, HBOT also relieves the patient of intractable local and visceral pain, and recurrent bleeding.
Radiation therapy, surgery and chemotherapy are the three branches of cancer therapy.[45] Any one or two, or may even have all three in a strategic order. Injury can occur from implantation of radioisotope seeds in brachytherapy. This therapy is used in prostate, uterine cervix, endometrium, bladder, tongue, thyroid cancer, etc. Unlike Cobalt treatment of yester years, teletherapy in the industrial world today uses Linear Accelerator (LINAC) with many modifications e.g. Intensity-Modulated Radiation Therapy (IMRT), Image-guided Radiation Therapy (IGRT) as delivery systems. Though these IMRT, IGRT radiation techniques of Linear Accelerator are more refined than before, but still conventional LINAC may occasionally cause significant non-healing ulcers. This lack of healing is due to progressive (parenchymal) fibrosis and a decrease in transcutaneous oxygen pressure at the tissue level.[45] Again, persistent hypoxia at the core of the wound is the central cause.
We treated of 72 patients with nonhealing wounds. These included five patients (5/72) who were treated for radiation injured non healing wound. Four of the five of these XRT induced ulcers healed completely. The first patient, with a history of bipolar disorder and CKD stage IV-V healed partially. Second patient had painful non healing rectal ulcer from radiation treatment for prostate cancer. It was treated successfully with HBOT, as other therapies failed. Patient's pain was gone by the end of HBOT treatment. She also had a recto-vaginal fistula which, after 35 HBOT treatments, exhibited decreased bleeding and pain. However, a definitive closure procedure was pending. The third and the fourth patients, who had radiation injury from breast cancer, treated by XRT, were treated with HBOT for nonhealing wound. The third patient ended treatment as she was satisfied with the amount of healing she achieved while the fourth woman healed the wound completely. Corman et al. (2003) treated 62 patients with hemorrhagic cystitis with hyperbaric oxygen therapy.[46] Of the 57 available for analysis at the conclusion of the study, 49 experienced complete resolution or marked improvement of hematuria after HBO treatment.[21]
Recent advances in HBOT
In many areas HBOT is shown to be effective and the use in novel indications are in progress [Figure 6]. However, the indications supported by CMS are only discussed here.
Recent advances in offloading
We have to always be able to think outside of the box and be prepared to challenge the current dogma. In fact, common wound care practice in the West may not work in a relatively disadvantaged population in another part of the world. HBOT is very expensive in the West. It requires trained personnel, sophisticated equipment, and rigorous compliance to safety and medico-legal issues. However, cost varies from country to country. If one can get a comparable result with simpler and locally available wound care resources and procedures, then that is something important to consider.
One new modality of wound care involves analyzing a Power Ratio, which is an advanced pressure parameter used to measure pressure on the planter aspect of the feet. It is based on the idea that insensate diabetic feet are susceptible to planter ulceration particularly in areas of high pressure. In a recent review, using pressure-reducing-shoes while monitoring the Power Ratio showed no re-ulceration after 6-15 years. Tarsal tunnel decompression is also used to restore sensation in feet with established ulcers.[7,47]
Charanya, Patil, Narayanamurthy, Parivalavan, Visvanathan (2004)[47] found that providing microcellular rubber insole footwear based on optimum hardness and thickness was found to be helpful in healing plantar ulcers in three to four weeks.[47] They also concluded that wearing such preventive footwear for six months reduced hardness of the foot sole and power ratio values to near-normal values.[47] In a selected group, this practice has claimed, to have healed complex diabetic foot ulcers without a complex surgical approach.
Total contact casts are another offloading modality shown to help heal foot ulcers while still allowing the patient to walk.[6] These total contact casts are minimally padded, well-molded plaster casts that allow for even distribution of pressure across the plantar surface of the foot.[6] This then eliminates the excessive concentration of localized pressure responsible for the ulceration.[6] Furthermore, patients cannot remove the casts, so they must be compliant.[6] Total contact casts typically heal plantar ulcers in about 8 weeks.[6]
Recent advances in anabolic steroids
Stanozolol, an anabolic steroid, has been shown in vitro to significantly enhance collagen synthesis when applied to human dermal fibroblasts.[48] Animals with full thickness wounds, when treated with oxandrolone, show early closure and increased tensile strength of the wound.[48]
Another study provided evidence that Insulin is the most natural anabolic agent and, when topically applied to skin excision wounds, accelerates re-epithelialization and stimulates “maturation” of the healing tissue.[18] Figure 7 is re-printed from an article by Liu et al. (2009) showing how a 0.03 μgm insulin/30 ml solution applied to skin excision wounds in mice accelerates re-epithelialization.[49] These studies provide compelling evidence of the use of novel agents in chronic wound healing. Particularly in areas of the world where HBOT may not be feasible, for economic or practical reasons, these new avenues should be explored.
Figure 7.
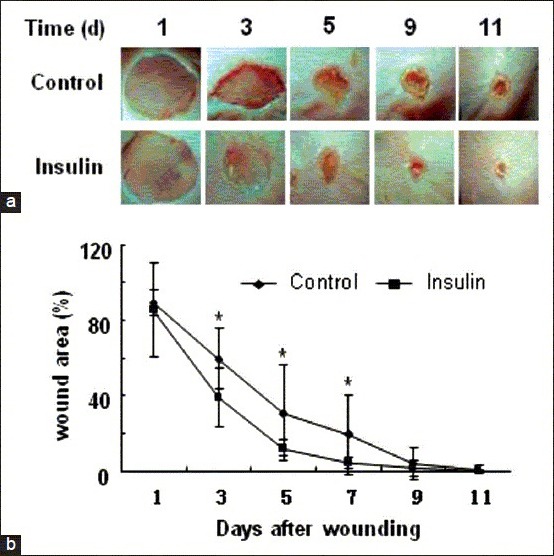
Insulin accelerates wound healing and improves re-epithelialization. Excision wounds were performed in C57BL/6J mice, and the healing process was monitored at different time points. (a) Representative images of wounds which were treated with vehicle (30 μl saline solution) or 0.03 u insulin/30 μl saline solution every two days (b) Wound area was quantified every two days and expressed as the percentage of the original wound area (n = 9; Statistics are shown as comparisons between the treatment and control. *P < 0.05). Insulin significantly decreased wound area.[49] HBOT[17]
Recent advances in growth factors
Growth factors of different kinds, which cause multiplication of the nascent cells, are very expensive to handle as well as to acquire. There are a variety of different growth factors that have shown promise in wound healing.[48] Platelet-derived growth factor (PDGF) attracts fibroblasts, neutrophils and monocytes and promotes the production of new extracellular matrix components.[48] Insulin-like growth factors I and II also play a role in being mitogenic for keratinocytes and fibroblasts, inhibiting apoptosis pathways, attenuating pro- and anti-inflammatory cytokine production, and stimulating extracellular matrix component production.[48] A study by Asai et al. (2012) applied endothelial progenitor cells to induced full-thickness skin wounds in diabetic mice. The cells significantly promoted wound healing by increasing local cytokine expression and enhancing neovascularization of the wound.[49]
CONCLUSION
In any situation, the best practice delivering best wound healing in a cost effective way can be a challenge for various reasons. Improving access to and delivery of health care globally would be our goal.
Unique local microbes and parasites causing non-healing ulcers have specific pathophysiology as well as need specific treatment. Cutaneous ulcers from filarial infections, schistosomiasis, leprosy, tuberculosis and leishmaniasis, are endemic in Morocco, Libya, Syria, around the Mediterranean Sea, Iraq, and Iran.[34] Indian subcontinent and elsewhere in the world have its unique set of challenges. No one paradigm can be the answer to all wounds.
Preventive measures, effective locally and globally, are the essence to uproot these nonhealing tropical ulcers. UNESCO, Bill and Malinda Gates foundation, Clinton Global initiatives, and the Carter Foundation are a few organizations who are making great strides in eradicating these parasitic diseases. But wider coordinated initiatives are needed.
It remains to be seen what the future of wound care holds, particularly with regard to using CPAP, off-loading techniques, using growth factors and other technological innovations and breakthroughs.
The age old battle of wound healing will remain with us. We should continue to invigorate the art and science of wound healing by using HBOT and other novel modalities of the day. Although various challenges will exist, a good wound care paradigm should prevail as the essential pathway to healing. Prevention is the best cure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Decision Memo for Hyperbaric Oxygen Therapy for Hypoxic Wounds and Diabetic Wounds of the Lower Extremities (CAG- 00060N). Decision Memo for Hyperbaric Oxygen Therapy for Hypoxic Wounds and Diabetic Wounds of the Lower Extremities (CAG-00060N) 2014. [Last accessed on 2014 August 16]. Available from: http://www.cms.gov .
- 2.Feldmeier JJ, Matos LA. Kensington, Maryland: Undersea and Hyperbaric Medical Society; 2003. Hyperbaric Oxygen 2003. Indications and Results: The Hyperbaric Oxygen Therapy Committee Report. [Google Scholar]
- 3.Undersea & Hyperbaric Medical Society. Indications for Hyperbaric Oxygen Therapy. 2014 [Google Scholar]
- 4.Sheffield PJ, Sheffield JC. “Complication rates for hyperbaric oxygen therapy patients and their attendants: A 22-year analysis” Gas 6.25. 2003. p. 139. http://hyperbaricinformation.com/HBOArticles/HBO-Complications/4th-ICHM-2003-Complicationrates-in-HBO-Sheffield.pdf .
- 5.Eskes AM, Ubbink DT, Lubbers MJ, Lucas C, Vermeulen H. Hyperbaric oxygen therapy: Solution for difficult to heal acute wounds. Systematic review? World J Surg. 2011;35:535–42. doi: 10.1007/s00268-010-0923-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calhoun JH, Overgaard KA, Stevens CM, Dowling JP, Mader JT. Diabetic foot ulcers and infections: Current concepts. Adv Skin Wound Care. 2002;15:31–45. doi: 10.1097/00129334-200201000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Narayanamurthy VB. Personal Communication [Google Scholar]
- 8.Bansal C, Scott R, Stewart D, Cockerell CJ. Decubitus ulcers: A review of the literature. Int J Dermatol. 2005;4410:805–10. doi: 10.1111/j.1365-4632.2005.02636.x. [DOI] [PubMed] [Google Scholar]
- 9.Hyperbaric Oxygen Therapy. Hyperbaric Oxygen Therapy. 2014. [Last accessed on 2014 August 16]. Available from: http://www.emedicine.medscape.com/article/1464149-overview .
- 10.Löndahl M, Katzman P, Nilsson A, Hammarlund C. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes. Diabetes Care. 2010;33:998–1003. doi: 10.2337/dc09-1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saraf S, Parihar R. Sushruta: The first Plastic Surgeon in 600 B.C. Int J Plast Surg. 2007;4:2. https://ispub.com/IJPS/4/2/8232 . [Google Scholar]
- 12.Bhutani S, Vishwanath G. Hyperbaric oxygen and wound healing. Indian J Plast Surg. 2012;45:316–24. doi: 10.4103/0970-0358.101309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gordillo GM, Sen CK. Revisiting the essential role of oxygen in wound healing. Am J Surg. 2003;186:259–63. doi: 10.1016/s0002-9610(03)00211-3. [DOI] [PubMed] [Google Scholar]
- 14.Kalani M, Jörneskog G, Naderi N, Lind F, Brismar K. Hyperbaric oxygen (HBO) therapy in treatment of diabetic foot ulcers. Long-term follow-up. J Diabetes Complications. 2002;16:153–8. doi: 10.1016/s1056-8727(01)00182-9. [DOI] [PubMed] [Google Scholar]
- 15.Kessler L, Bilbault P, Ortega F, Grasso C, Passemard R, Stephan D, et al. Hyperbaric oxygenation accelerates the healing rate of nonischemic chronic diabetic foot ulcers: A prospective randomized study. Diabetes Care. 2003;26:2378–82. doi: 10.2337/diacare.26.8.2378. [DOI] [PubMed] [Google Scholar]
- 16.David LA, Sàndor GK, Evans AW, Brown DH. Hyperbaric oxygen therapy and mandibular osteoradionecrosis: A retrospective study and analysis of treatment outcomes. J Can Dent Assoc. 2001;67:384. [PubMed] [Google Scholar]
- 17.Millar I. Middle ear barotraumas scoring. In: Barach P, Mueller PH, Pirone C, editors. Patient Safety: Prevention and Treatment of Complications in Hyperbaric Medicine. Undersea and Hyperbaric Medical Society (UHMS) Workshop, Kensington. 52nd ed. Maryland: Undersea and Hyperbaric Medical Society; 2002. pp. 101–6. [Google Scholar]
- 18.Thom SR. Oxidative stress is fundamental to hyperbaric oxygen therapy. J Appl Physiol (1985) 2009;106:988–95. doi: 10.1152/japplphysiol.91004.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beard T, Watson B, Barry R, Stewart D, Warriner R. Analysis of adverse events occurring in patients undergoing adjunctive hyperbaric oxygen treatment: 2009-2010. 2011 [Google Scholar]
- 20.National Diabetes Fact Sheet, 2011. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. 2014 [Google Scholar]
- 21.Lohr VL, Norvell HC. Best Publishing Company; 2002. Hyperbaric Nursing. [Google Scholar]
- 22.Uhlmeyer D, Warriner RA, III, Pasceri P, Fife CE, Otto G. Pre and post hyperbaric oxygen therapy (HBOT) blood glucose levels. 2005 [Google Scholar]
- 23.Pamidi S, Tasali E. Obstructive sleep apnea and type 2 diabetes: Is there a link? Front Neurol. 2012;3:126. doi: 10.3389/fneur.2012.00126. eCollection 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinstock TG, Redline S. Comparative effectiveness research in obstructive sleep apnea: Bridging gaps between efficacy studies and clinical practice. J Comp Eff Res. 2012;1:83–105. doi: 10.2217/cer.11.12. [DOI] [PubMed] [Google Scholar]
- 25.Naeser MA, Martin PI, Lundgren K, Klein R, Kaplan J, Treglia E, et al. Improved language in a chronic nonfluent aphasia patient following treatment with CPAP and TMS. Cogn Behav Neurol. 2010;23:29–38. doi: 10.1097/WNN.0b013e3181bf2d20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kasasbeh E, Chi DS, Krishnaswamy G. Inflammatory aspects of sleep apnea and their cardiovascular consequences. South Med J. 2006;99:58–69. doi: 10.1097/01.smj.0000197705.99639.50. quiz 81. [DOI] [PubMed] [Google Scholar]
- 27.Davies RJ, Ali NJ, Stradling JR. Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax. 1992;47:101–5. doi: 10.1136/thx.47.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO. Diabetes. 2014. [Last accessed on 2014 August 16]. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/
- 29.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: A meta-analysis. Psychosom Med. 2001;63:619–30. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention 2014. [Last accessed on 2014 August 16]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5345a2.htm./http://www.cdc.gov/diabetes/statistics/lea/table6.htm .
- 31.Adult Obesity Facts. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention 2013. [Last accessed on 2014 Mar 17]. Available from: http://www.cdc.gov/obesity/data/adult.html .
- 32.Calhoun JH, Cantrell J, Cobos J, Lacy J, Valdez RR, Hokanson J, et al. Treatment of diabetic foot infections: Wagner classification, therapy, and outcome. Foot Ankle. 1988;9:101–6. doi: 10.1177/107110078800900301. [DOI] [PubMed] [Google Scholar]
- 33.Baba H, Wada M, Annen S, Azuchi M, Imura S, Tomita K. The tarsal tunnel syndrome: Evaluation of surgical results using multivariate analysis. Int Orthop. 1997;21:67–71. doi: 10.1007/s002640050122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hotez PJ, Savioli L, Fenwick A. Neglected tropical diseases of the Middle East and North Africa: Review of their prevalence, distribution, and opportunities for control. PLoS Negl Trop Dis. 2012;6:e1475. doi: 10.1371/journal.pntd.0001475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lasry-Levy E, Hietaharju A, Pai V, Ganapati R, Rice AS, Haanpää M, et al. Neuropathic pain and psychological morbidity in patients with treated leprosy: A cross-sectional prevalence study in Mumbai. PLoS Negl Trop Dis. 2011;53:e981. doi: 10.1371/journal.pntd.0000981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC). Current depression among adults — United States, 2006 and 2008. MMWR Morb Mortal Wkly Rep. 2010;59:1229–35. [PubMed] [Google Scholar]
- 37.Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life: A population study. Diabetes Care. 2004;27:1066–70. doi: 10.2337/diacare.27.5.1066. [DOI] [PubMed] [Google Scholar]
- 38.Padberg Jr, Back TL, Thompson PN, Hobson RW., 2nd Transcutaneous Oxygen (TcPO2) Estimates Probability of Healing in the Ischemic Extremity. J Surg Res. 1996;60(2):365–9. doi: 10.1006/jsre.1996.0059. [DOI] [PubMed] [Google Scholar]
- 39.Faglia E, Favales F, Aldeghi A, Calia P, Quarantiello A, Oriani G, et al. Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer: A randomized study. Diabetes Care. 1996;19:1338–43. doi: 10.2337/diacare.19.12.1338. [DOI] [PubMed] [Google Scholar]
- 40.Mohler ER, III, Mitchell E. Noninvasive Diagnosis of Arterial Disease. In: Post TW, editor. UpToDate. Waltham, MA: [Last accessed on 2014 April 5]. UpToDate. [Google Scholar]
- 41.Katsamouris A, Brewster DC, Megerman J, Cina C, Darling RC, Abbott WM. Transcutaneous oxygen tension in selection of amputation level. Am J Surg. 1984;1474:510–7. doi: 10.1016/0002-9610(84)90014-x. [DOI] [PubMed] [Google Scholar]
- 42.Mueller PH. Review of screening procedures for elective hyperbaric admission. In: Barach P, Mueller PH, Pirone C, editors. Patient Safety: Prevention and Treatment of Complications in Hyperbaric Medicine 52nd ed. Undersea and Hyperbaric Medical Society (UHMS) Workshop, Kensington. Maryland: Undersea and Hyperbaric Medical Society; 2002. pp. 126–32. [Google Scholar]
- 43.Bitterman N, Bitterman H. Oxygen toxicity. In: Mathieu D, editor. Handbook on Hyperbaric Medicine. Chapter 3.7.2. Netherland: Springer; 2006. pp. 731–65. [Google Scholar]
- 44.Leach RM, Rees PJ, Wilmshurst P. Hyperbaric oxygen therapy. BMJ. 1998;317:1140–3. doi: 10.1136/bmj.317.7166.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rudolph R. Plastic Surgery-epitomes of progress: Chronic skin ulceration after radiotherapy for cancer. West J Med. 1982;136:525. [PMC free article] [PubMed] [Google Scholar]
- 46.Corman JM, McClure D, Pritchett R, Kozlowski P, Hampson NB. Treatment of radiation induced hemorrhagic cystitis with hyperbaric oxygen. J Urol. 2003;169:2200–2. doi: 10.1097/01.ju.0000063640.41307.c9. [DOI] [PubMed] [Google Scholar]
- 47.Charanya G, Patil KM, Narayanamurthy VB, Parivalavan R, Visvanathan K. Effect of foot sole hardness, thickness and footwear on foot pressure distribution parameters in diabetic neuropathy. Proc Inst Mech Eng H. 2004;218:431–43. doi: 10.1243/0954411042632117. [DOI] [PubMed] [Google Scholar]
- 48.Liu Y, Petreaca M, Yao M, Martins-Green M. Cell and molecular mechanisms of keratinocyte function stimulated by insulin during wound healing. BMC Cell Biol. 2009;10:1. doi: 10.1186/1471-2121-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Asai J, Takenaka H, Ii M, Asahi M, Kishimoto S, Katoh N, et al. Topical application of ex vivo expanded endothelial progenitor cells promotes vascularisation and wound healing in diabetic mice. Int Wound J. 2013;10:527–33. doi: 10.1111/j.1742-481X.2012.01010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


