Abstract
Aim:
The purpose of this study was to evaluate patients with sacrococcygeal pilonidal sinus disease (SPSD) who underwent Karydakis procedure at our centre with reference to the perioperative findings, early and late postoperative results and recurrence.
Materials and Methods:
A total of 103 patients presenting with SPSD at our centre underwent Karydakis flap repair from January 2001 to December 2010. These patients were then followed-up and evaluated with respect to operative time, drain use, hospital stay, suture removal, complications, and recurrence.
Results:
The mean operative time was 74.9 min with a median hospital stay of 5 days. Drains were removed at a median of 7 days and sutures at a median of 15 days. Twenty-one patients presented with serous collection in the wound. Six patients had wound infection. Patients were followed-up for a median of 29 months. No recurrences were noted in any of the cases.
Conclusion:
Karydakis flap procedure is a relatively simple procedure for SPSD with reproducible low recurrence rates.
KEY WORDS: Complications, Karydakis flap repair, recurrence, sacrococcygeal pilonidal sinus disease
INTRODUCTION
Sacrococcygeal pilonidal sinus disease (SPSD) is a worldwide problem affecting, usually, young men and women with a propensity for recurrence that causes significant problems if not dealt appropriately in the primary setting. The higher incidence of the disease is noted among males and army recruits.[1,2,3,4]
An understanding of the pathophysiology of the formation of the sinus and progression of the disease had been a matter of controversy and debate till the elucidation of the same in works of Karydakis in the year 1992.[5]
The management of the disease is primarily surgical with a variety of procedures being described ranging from wide excision, excision with midline closure, oblique excision and asymmetric closure to flap procedures such as Karydakis and Limberg flap procedures.[1,4,6] It has been proved that flap procedures are superior to traditional methods of excision of the tract in terms of preventing recurrence of the lesion.[1,6] The procedure of choice however remains debatable. On the other hand, flap procedures are often accused of being time-consuming and technically demanding.
In this study, we attempt to evaluate patients with SPSD who underwent Karydakis procedure at our centre with reference to the perioperative findings, early and late postoperative results and recurrence. The principle of Karydakis procedure being flattening of the natal cleft and lateral shift of midline (scar), which prevents lodging of hair in the natal cleft and hence recurrence.
MATERIALS AND METHODS
Study group
The present study was undertaken as a prospective study from January 2001 to December 2010. All patients who were subjected to Karydakis procedure for SPSD at our centre were included in the study whether presenting with primary [Figure 1a] or recurrent disease [Figure 1b]. All procedures were performed by a single surgeon.
Figure 1.
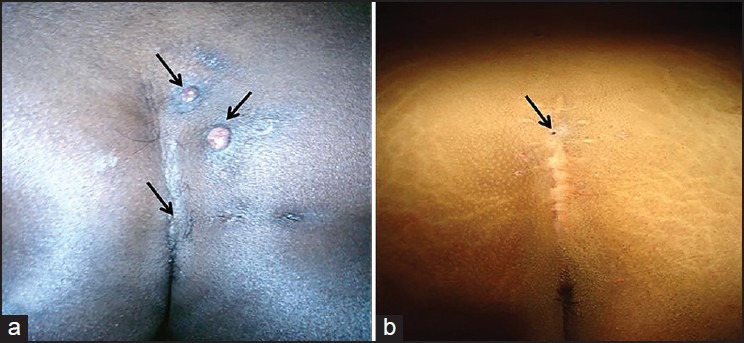
(a) Primary (arrows indicate primary and secondary openings) (b) recurrent sacrococcygeal pilonidal sinus disease post excision and primary midline closure
Patients with acute pilonidal abscess were excluded from this study.
Procedure
All patients underwent routine workup for surgery. A third-generation cephalosporin was used as premedication administered 1 h before surgery.
All procedures were done under spinal anaesthesia. Patients were placed in prone jack knife position. A small quantity of dilute methylene blue is instilled into the sinus tracts. An asymmetrical ellipse was marked to encompass the pilonidal complex [Figure 2a]. The upper and lower ends of the ellipse thus marked were at least 2 cm away from the midline.
Figure 2.
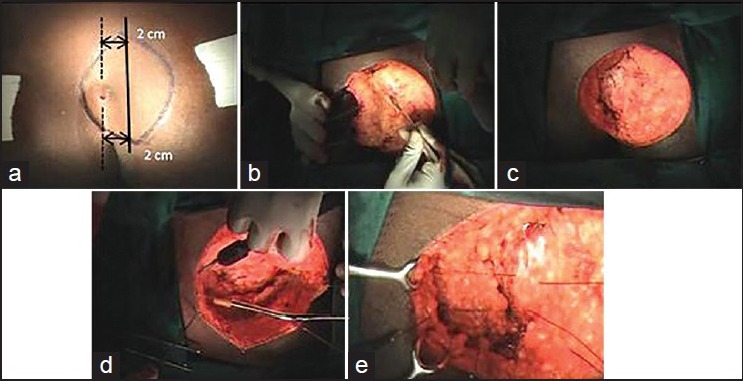
Stages of surgery (a) marking incision, (b) excision, (c) post excision, (d) raising the flap, (e) securing the flap
The area thus marked was then excised full thickness up to the sacral fascia [Figure 2b and c] with a straight edge on the side of flap mobilisation and a sloping edge on the other side [Figure 3a]. This is followed by mobilisation of the flap across the midline [Figure 2d and 3b]. A layer of 1-0 polyglactin sutures was placed, the needle being passed into the sacral fascia in the midline and then into the V junction of the flap [Figure 2e] and secured. A suction drain was placed and brought out well laterally.
Figure 3.
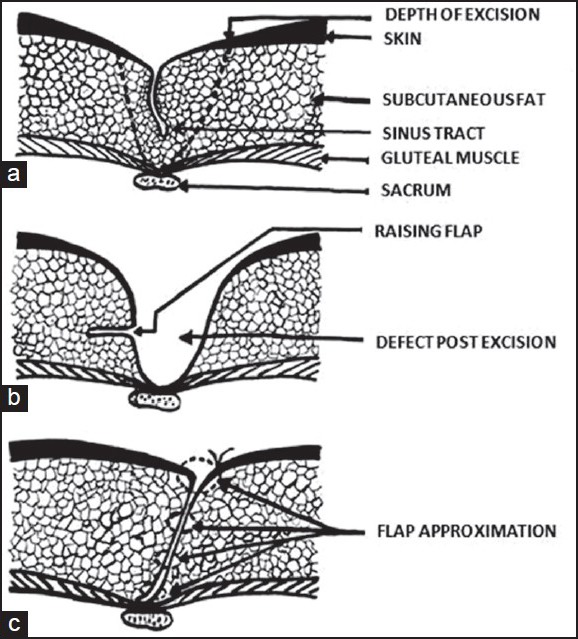
Stages of surgery (a) depth of excision, (b) raising the flap, (c) securing the flap
A second layer of polyglactin sutures was then placed to secure the flap to the lateral edge of the wound. Skin was approximated using 2-0 nylon mattress sutures [Figure 3c] and a pressure dressing was applied.
Wound inspection was done on 2nd postoperative day [Figure 4a] and patient was discharged, usually, on the 4th or 5th postoperative day sometimes with drains in-situ. Drains were removed 7 to 12 days later. Sutures were, usually, removed on the 11th or 12th postoperative day.
Figure 4.
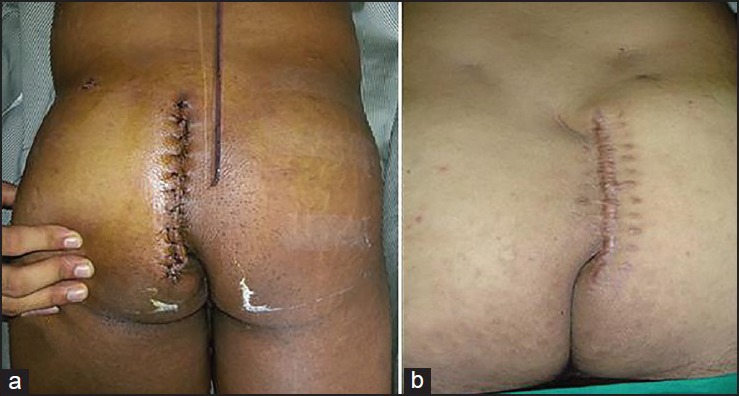
(a) Case 1 - Post-operative day 2 (b) Case 2 - After 4 weeks (note flattening of natal cleft and lateral shift of midline)
Following suture removal patients were followed-up once in 2 weeks for the next one and a half months [Figure 4b], followed by once every 2 months for the next 6 months and then once in 6 months henceforth.
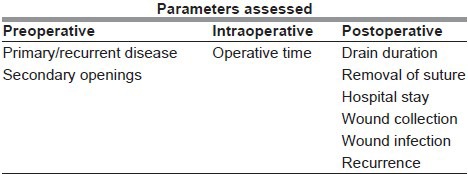
The following parameters as mentioned in table below were assessed with respect to each patient.
RESULTS AND ANALYSIS
A total of 103 patients underwent this procedure over a period from January 2001 to December 2010 of which 87 were males, and 16 were females. The age of patients ranged from 15 to 57 years with a mean age of 26.45 years with the majority (78 out of 103-75.72%) in the 21 to 40 year's age group. The presenting complaints were discharge from the natal cleft in 95 patients, followed by pain in 51 patients. Eight of these patients had recurrent disease and had undergone a primary procedure like excision and curettage or excision and primary midline closure. Sixty-four patients were found to have one or more secondary openings. All cases were found to have these openings within 4 cm cranial or caudal to the primary opening and secondary openings situated laterally were within 2 cm on one side of the midline.
The mean operative time was 74.9 min (range of 60-120 min). Hospital stay was a median of 5 days with a minimum of two and maximum of 15 days. Drains were removed at a median of 7 days (range: 4-12 days). Suture removal was done at a median of 15 days.
Twenty-one patients presented with serous collection in the wound. Six patients had wound infection. In patients with serous collection, the collection was let out following which wounds healed within 2 weeks of regular dressings. In patients with wound infection, pus was drained, and they were administered appropriate antibiotics and underwent regular dressing. In five patients, the wounds healed by secondary intention within 3-4 weeks. Only one patient in the above group had to be taken up for secondary suturing at the end of 4 weeks and healing was complete in another 3 weeks. This was an obese patient who had recurrence twice following excision and primary midline closure and underwent Karydakis procedure the 3rd time.
The patients were followed-up for a median of 29 months with the minimum follow-up being 4 months and the maximum of 78 months. No recurrences were noted in any of the cases.
DISCUSSION
Sacrococcygeal pilonidal sinus disease is a health issue affecting young adults worldwide that requires surgical intervention. Recurrences have led to a variety of procedures being practiced from simple excision to complicated flap procedures. Procedures like wide excision or excision with primary midline closure though simple pose a greater risk of recurrence (up to 16%) compared with flap procedures.[6] A study by Awad et al.[7] put forward a scoring system to classify the cases into three groups. Depending on the scores, the patients underwent excision with secondary healing, excision with primary midline closure or flap procedure. Though it was a novel attempt to address this issue, simple wide excision is seldom practised in centres dealing with pilonidal sinus regularly given the longer time taken for healing and also propensity to recur. Hence, procedure of choice remains controversial often led by the merits of the individual case and also the surgeon's school of training and experience.
In our study, most patients were young adult males with a ratio of 5.4:1 = Male:female that corroborates with the natural presentation of the disease.[1] These patients underwent Karydakis procedure. Complications noted were serous wound collection in 21 patients (20.3%) and wound infection in 6 patients (5.8%). Most of the patients were discharged within 5 days with only eight patients staying >10 days. Other studies have quoted hospital stay ranging from 1 to 4 days.[8] The longer hospital stay for a few patients in our study can be attributed to our initial apprehension as well as the fact that patients with complications like wound infection and those who were reluctant to go home with drain in-situ stayed back for longer periods.
Patients were followed-up according to the aforementioned protocol and the largest follow-up time was 78 months with a median of 29 months. Some of the patients were lost to follow-up with the resultant lowest follow-up being 4 months.
None of the patients had any recurrence, which is comparable to other studies like Kitchen (4%),[9] Anyanwu et al. (0%)[10] and Amir (0%).[11]
Karydakis in his work “Easy and Successful Treatment of Pilonidal Sinus after explanation of it's Causative Process” published in The Australian and New Zealand Journal of Surgery May, 1992[5] opined that three main factors play a part in the hair insertion process: The invader (H), consisting of loose hair; some force (F) which causes hair insertion; and the vulnerability of the skin (V) to the insertion of hair at the depth of the natal cleft. Karydakis procedure is a technically simple one that follows the objective of “no raphe, no wound and scar at depth.” This procedure results in flattening of the natal cleft with lateral shift of the midline.
A number of other flap procedures like Z plasty,[12] W plasty,[13] Limberg flap repair,[14] V-Y flap,[6] bilateral rotation flap,[15] have been used to achieve flattening of the natal cleft. They are relatively complex procedures requiring surgical expertise as compared to the Karydakis procedure.[16] These techniques have reported problems like flap tip necrosis[7,15] which is seldom seen with Karydakis procedure and was not seen in our study too. Another fundamental issue is that in these procedures the scar crosses or is in close association with the midline that again predisposes to disease recurrence with these procedures.[7,15] A number of studies have also found patients complaining of postoperation hypoesthesia over the operated site. None of the patients in our study complained of the same.
During the latter part of our study, we made subtle changes, which helped in improving the outcome. These we highlight below:
Catheterization of female patients in the immediate postoperative period — will prevent contamination and wound infection as patient is not actively mobile
Proper perineal hygiene in the postoperative period
Curving the lower 2-3 cm of the incision laterally away from the midline will prevent the wound and the scar from dipping towards the perianal region which in turn will reduce wound contamination.
Karydakis procedure is thus an effective procedure for management of pilonidal disease. One limitation we noticed during our study is that, in patients having secondary sinuses too far away from the midline, Karydakis procedure would be difficult to perform as the area of excision and advancement becomes very large. In these cases, a rotational flap procedure would probably be a better choice.
CONCLUSION
Karydakis flap procedure is a relatively simple procedure for SPSD with reproducible low recurrence rates. However, in patients with secondary sinus openings on both sides of the midline or in cases where the openings are placed too lateral to the midline, it would be difficult to perform this procedure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Goligher J. Pilonidal sinus. In: Goligher J, editor. Surgery of the Anus, Colon and Rectum. London: Balliere Tindall; 1984. pp. 221–36. [Google Scholar]
- 2.Buie LA. Jeep disease (pilonidal disease of mechanized warfare) Dis Colon Rectum. 1982;25:384–90. [PubMed] [Google Scholar]
- 3.Søndenaa K, Andersen E, Nesvik I, Søreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10:39–42. doi: 10.1007/BF00337585. [DOI] [PubMed] [Google Scholar]
- 4.Bendewald FP, Cima RR. Pilonidal disease. Clin Colon Rectal Surg. 2007;20:86–95. doi: 10.1055/s-2007-977486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992;62:385–9. doi: 10.1111/j.1445-2197.1992.tb07208.x. [DOI] [PubMed] [Google Scholar]
- 6.Hull TL, Wu J. Pilonidal disease. Surg Clin North Am. 2002;82:1169–85. doi: 10.1016/s0039-6109(02)00062-2. [DOI] [PubMed] [Google Scholar]
- 7.Awad MM, Elbaset AA, Ebraheem S, Tantawy E, Elhafez MA, Elsayed AM. A scoring system as a method to evaluate pilonidal sinus disease to make an easy decision for its management. Indian J Plast Surg. 2009;42:43–8. doi: 10.4103/0970-0358.53011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gönenç M, Yırgın H, Dinç M, Kapan A, Turhan AN, Alış H. Karydakis flap for sacrococcygeal pilonidal sinus disease: Long-term outcomes. A retrospective analysis. Med J Bakıköy. 2011;7:153–5. [Google Scholar]
- 9.Kitchen PR. Pilonidal sinus: Experience with the Karydakis flap. Br J Surg. 1996;83:1452–5. doi: 10.1002/bjs.1800831040. [DOI] [PubMed] [Google Scholar]
- 10.Anyanwu AC, Hossain S, Williams A, Montgomery AC. Karydakis operation for sacrococcygeal pilonidal sinus disease: Experience in a district general hospital. Ann R Coll Surg Engl. 1998;80:197–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Amir M. Karydakis flap operation for chronic pilonidal sinus. Pak J Surg. 2007;23:65–9. [Google Scholar]
- 12.Monro RS, Mcdermott FT. The elimination of causal factors in pilonidal sinus treated by Z-plasty. Br J Surg. 1965;52:177–81. doi: 10.1002/bjs.1800520306. [DOI] [PubMed] [Google Scholar]
- 13.Roth RF, Moorman WL. Treatment of pilonidal sinus and cyst by conservative excision and W-plasty closure. Plast Reconstr Surg. 1977;60:412–5. [PubMed] [Google Scholar]
- 14.Urhan MK, Kücükel F, Topgul K, Ozer I, Sari S. Rhomboid excision and Limberg flap for managing pilonidal sinus: Results of 102 cases. Dis Colon Rectum. 2002;45:656–9. doi: 10.1007/s10350-004-6263-4. [DOI] [PubMed] [Google Scholar]
- 15.Awad MM, Saad KM, Tolba AM, Gharib OH. A simple novel technique for closure of simple and complex pilonidal sinus with either simple (tongueshaped) or bilobed rotation flap. Indian J Plast Surg. 2007;40:47–50. [Google Scholar]
- 16.Awad MM, Saad KM. Does closure of chronic pilonidal sinus still remain a matter of debate after bilateral rotation flap? (N-shaped closure technique) Indian J Plast Surg. 2006;39:157–62. [Google Scholar]


