Abstract
We present a rare complication of abdominal liposuction: bowel perforation and necrotizing fasciitis. Because of bilateral lumbar hernia, a 56-year-old woman had caecum and descending colon perforation during lipoplasty. She had septic shock syndrome at her admission. The authors treated this complex wound with several debridement, omental flap, NPWT and split-thickness skin graft. The incidence of abdominal wall perforation with visceral injury is 14 in 100,000 liposuctions performed. There are only 12 cases of bowel perforation in literature but this complication is probably underestimated. Prompt surgical debridement is absolutely mandatory in this life threatening scenario. Lumbar hernia is very rare and should be ruled out before every abdominal liposuction clinically or with imaging modalities.
KEY WORDS: Bowel perforation, liposuction, lumbar hernia, necrotizing fasciitis, negative pressure large wound therapy
INTRODUCTION
Abdominal liposuction is one of the most frequently performed aesthetic surgeries. It is universally considered to be a safe surgical procedure with a reportedly low overall complication rate. However from the time of Dujarrier in the 1920s, some cases of dramatic complication have been reported.[1] Minor complications of liposuction include contour irregularities, infection, hypoesthesia, oedema, ecchymosis, seroma, haematoma and skin discolouration, especially at the site of lipoaccess. More serious complications such as pulmonary embolism, viscera perforation, lidocaine toxicity or even death are rare but have been documented. The possibility of bowel perforation during liposuction is well known but is probably an underestimated complication of abdominal liposuction. It may be difficult to diagnose but has the potential to be life-threatening.
CASE REPORT
A 56-year-old woman presented to the emergency department 24 h after undergoing abdominal liposuction in another aesthetic centre. Few hours after the procedure, she experienced severe, diffuse and persistent abdominal pain. There was no relief despite a high dose of non-steroidal anti-inflammatory drugs. Later she was transferred to the surgical intensive therapy unit for “septic shock syndrome.” She presented with large necrotising cutaneous lesions of abdomen and flank areas. She was electively intubated, and initial therapies were resuscitation and hemodynamic stabilization. She needed vaso-pressors to maintain her blood pressure. The diagnosis of intestinal perforation had been missed intra-operatively as well as in the immediate postoperative period.
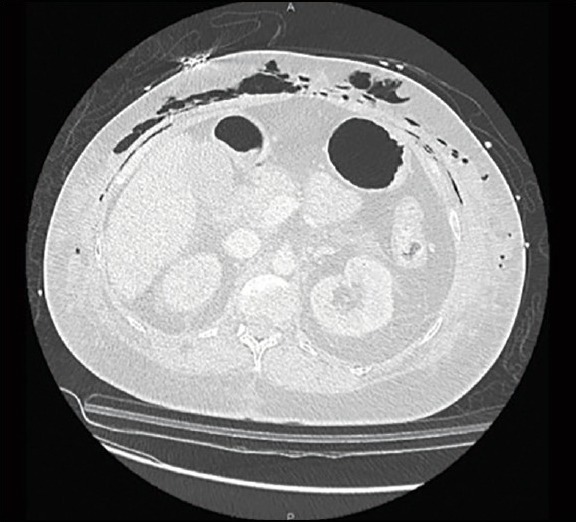
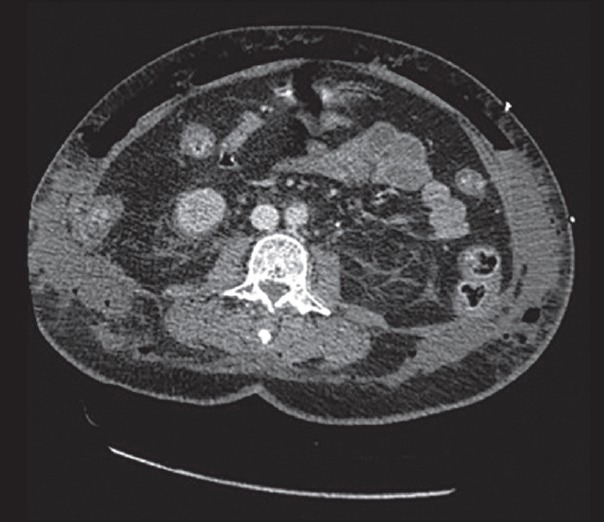
A computed tomography (CT) scan was done, which showed extensive subcutaneous air in the abdominal wall from the xiphoid process down. Pockets of free air and inflammatory changes also were present within the peritoneal cavity surrounding the region of the caecum and ascending colon as seen on Figures 1 and 2. Bilateral congenital lumbar herniae of the abdominal wall were identified [Figure 3].
Figure 1.
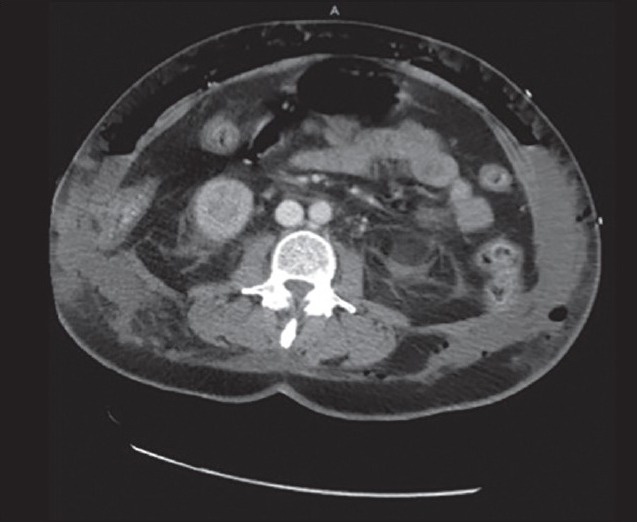
Subcutaneous air in the anterior abdominal wall
Figure 2.
Subcutaneous air in the anterior abdominal wall
Figure 3.
Bilateral lumbar hernia with caecum hernia
Her vital functions were too unstable to perform an immediate debridement of the necrotizing tissue or bowel repair. Therefore, only releasing incisions up to muscular layer in flanks and infra umbilical areas were made [Figure 4].
Figure 4.

Pre-operative view
After a period of 12 days, her condition stabilized enough for us to perform surgery. We performed extensive debridement of all necrotizing tissue injuries. In the area of the right lumbar hernia, there were multiple perforations in the ascending colon and the caecum [Figure 5]. A colostomy was made in the remaining healthy skin, in the right hypochondrium. We next dissected an omental flap to repair the right lumbar hernia [Figure 6]. During left lumbar debridement, in the area of the left lumbar hernia, we found multiple perforations in the descending colon [Figure 7]. There was no reliable flap on hand to cover this area and hence we decided to close this perforation. She had no sign of peritoneal infection. Negative pressure large wound therapy (NPWT) with 2 motors was initiated [Figure 8].
Figure 5.

Caecum hernia with perforations
Figure 6.

Right abdominal debridement with epiploon flapon right flank
Figure 7.

Left lumbar hernia with descending colon perforation
Figure 8.

Negative pressure large wound therapy dressing
We repeated serial debridement and NPWT dressing twice a week during the next 10 weeks. The wound healed gradually in 12 weeks [Figure 9].
Figure 9.

Wound healing on right side with granulation tissue on epiploon flap
Finally, this large wound was covered with a 2:1 meshed skin graft in a single stage. The back and the right thigh were the donor site. On the left lumbar area, sutures to repair the colon repeatedly failed to hold. We then decided to convert the perforated colon into a colostomy [Figures 10 and 11]. When the patient was well enough to be ambulatory, she was transferred to a rehabilitation centre.
Figure 10.

Result 3 weeks after shin graft (abdominal view)
Figure 11.

Left colostomia remaining
DISCUSSION
Major surgical complications are even more regrettable in aesthetic surgeries like liposuction because the patients are typically healthy liposuction conducted by trained physicians in patients without contraindications has an abdominal perforation rate as low as 0.014%.[2]
Our case is unique for many reasons:
Patient with bilateral congenital muscle anomaly (lumbar herniae) which were undetected pre-operatively.
Double localisations of colonic perforations in these herniae.
Large necrotising fasciitis in abdominal and lumbar areas.
Bowel perforation during liposuction is rare with only 12 cases reported in the literature but probably underestimated.[3,4]
In our case, the patient had severe pain immediately after surgery and was not soothed with high doses of non-steroidal anti-inflammatory drugs. Hence, the diagnosis of intestinal perforation was not only missed intra-operatively but also in the immediate postoperative period. It is important that physicians diagnose symptoms of such complications as early as possible because the consequences are dramatic with severe sequelae and could be potentially fatal.[2,5]
The incidence of necrotising fasciitis after liposuction is unknown although cases of necrotizing fasciitis after liposuction without intestinal perforation have been described.[6]
Quick transfer to an intensive therapy unit and surgical debridement is the key to saving the patient. Without radical surgery, patient could die of septic complications or multiple organ failure. It could be useful to add hyperbaric oxygen treatment.[7] NPWT therapy improves the management of extensive wound and allows grafting earlier with good healing results.
Lumbar hernia is an uncommon defect of the posterior abdominal wall that represents less than 1% of all abdominal wall hernias.[8,9] Congenital and bilateral lumbar hernia is more unusual. In our case, there were no clinical symptoms and no previous abdominal surgery. Pre-operative clinical examination did not diagnose these hernias. The need for medical imaging like CT scan or ultrasonography should be discussed with patients who have ventral hernias, previous abdominal surgery, a high body mass index, and abnormal abdominal contour.[10] Such imaging would be useful to diagnose such hidden herniae provided one has knowledge of the possible presence of such issues and therefore a high index of suspicion in such cases. The purpose of this case report is to call attention to the same.
CONCLUSION
The complication reported here is very rare following abdominal liposuction but prevention is possible if pre-operative clinical examination includes thorough clinical examination of the abdominal wall. For potentially high-risk patients a pre-operative ultrasonography or CT scan may be helpful. Surgeons also need to perform a careful postoperative follow-up assessment for early diagnosis of such complications. This case and the sequelae would help us to remember how serious the complications of liposuction can be and how to avoid them if possible.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grazer FM. Suction-assisted lipectomy, suction lipectomy, lipolysis, and lipexeresis. Plast Reconstr Surg. 1983;72:620–3. doi: 10.1097/00006534-198311000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Grazer FM, de Jong RH. Fatal outcomes from liposuction: Census survey of cosmetic surgeons. Plast Reconstr Surg. 2000;105:436–46. doi: 10.1097/00006534-200001000-00070. [DOI] [PubMed] [Google Scholar]
- 3.Talmor M, Hoffman LA, Lieberman M. Intestinal perforation after suction lipoplasty: A case report and review of the literature. Ann Plast Surg. 1997;38:169–72. doi: 10.1097/00000637-199702000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Ovrebø KK, Grong K, Vindenes H. Small intestinal perforation and peritonitis after abdominal suction lipoplasty. Ann Plast Surg. 1997;38:642–4. doi: 10.1097/00000637-199706000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Engl J Med. 1999;340:1471–5. doi: 10.1056/NEJM199905133401904. [DOI] [PubMed] [Google Scholar]
- 6.Heitmann C, Czermak C, Germann G. Rapidly fatal necrotizing fasciitis after aesthetic liposuction. Aesthetic Plast Surg. 2000;24:344–7. doi: 10.1007/s002660010056. [DOI] [PubMed] [Google Scholar]
- 7.Sharma D, Dalencourt G, Bitterly T, Benotti PN. Small intestinal perforation and necrotizing fasciitis after abdominal liposuction. Aesthetic Plast Surg. 2006;30:712–6. doi: 10.1007/s00266-006-0078-8. [DOI] [PubMed] [Google Scholar]
- 8.Zhou X, Nve JO, Chen G. Lumbar hernia: Clinical analysis of 11 cases. Hernia. 2004;8:260–3. doi: 10.1007/s10029-004-0230-9. [DOI] [PubMed] [Google Scholar]
- 9.Fontoura RD, Araújo ES, Oliveira GA, Sarmenghi Filho D, Kalil M. Spontaneous bilateral Petit hernia. Rev Col Bras Cir. 2011;38:369–70. doi: 10.1590/s0100-69912011000500016. [DOI] [PubMed] [Google Scholar]
- 10.Di Candia M, Malata CM. Aesthetic and functional abdominal wall reconstruction after multiple bowel perforations secondary to liposuction. Aesthetic Plast Surg. 2011;35:274–7. doi: 10.1007/s00266-010-9591-x. [DOI] [PubMed] [Google Scholar]


