Sir,
Isolated cases of postoperative flare-up of tuberculosis (TB) have been described earlier. We want to report a postoperative flare-up of TB following McIndoe's vaginoplasty in a patient with Meyer Rokitansky Kuster Hauser (MRKH) syndrome.
A 21-year-old nulliparous female presented with primary amenorrhoea and inability to have sexual intercourse.
On examination, secondary sexual characteristics and external genitals were normal. However per speculum examination showed a blind vagina of 2 cm. Routine investigations were normal. Ultrasound pelvis showed absent uterus with bilateral normal ovaries.
With the diagnosis of MRKH syndrome, the patient underwent McIndoe's vaginoplasty. A neovagina was created, and a soft mould with split thickness skin graft taken from thigh. Patient stood the procedure well and the postoperative course was uneventful till postoperative day 2 when the patient developed abdominal distension and high grade fever (101°F-102°F). She had tachycardia and no bowel sounds. The distension was progressive and ultrasound revealed intra-abdominal collection. As the condition of the patient deteriorated, the patient was taken up for exploratory laparotomy for suspected pyo-peritoneum. Intraoperative approximately 2l of straw coloured fluid was present in the peritoneal cavity. Upper abdomen was plastered with matted bowel loops [Figure 1]. Multiple caseating coagula [Figure 2] were seen on surface of bowel, peritoneum and pouch of Douglas. Multiple loculi filled with straw coloured fluid were present diffusely in the abdomen. Both the ovaries and the urinary bladder were healthy.
Figure 1.
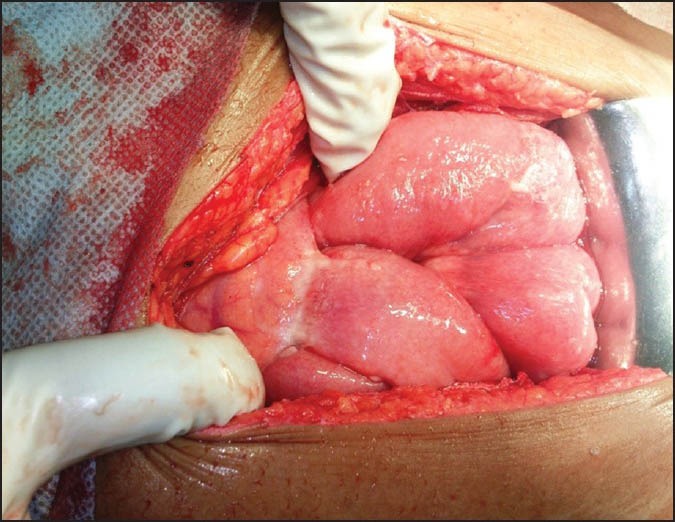
Picture showing matted bowel loops
Figure 2.
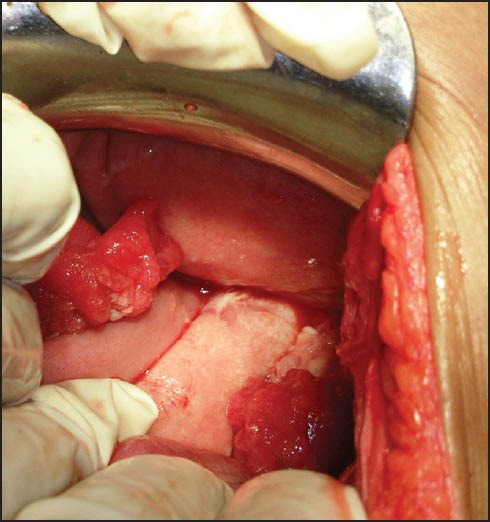
Picture showing intraperitoneal collection
Caseating granuloma was seen in histopathology and acid-fast bacilli culture of fluid was positive. Hence, she was diagnosed as the case of postoperative flare-up of abdominal TB and started on anti-TB treatment (ATT) comprising of (isoniazid, rifampicin, pyrazinamide and ethambutol). The patient responded well and underwent mould change after a week after the vaginoplasty and was discharged in stable condition. She followed up for a mould change and was alright.
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis. The modes of infection include haematogenous, lymphatics, ingestion of bacilli, or direct spread. Involvement of the abdominal lymph nodes and the peritoneum may occur without other organ involvement.[1]
The clinical presentation of peritoneal TB is abdominal pain and slowly progressive abdominal swelling from ascites. Constitutional symptoms of fever and night sweats may be present. Small-bowel obstruction can occur due to adhesions.
A detailed literature review did not yield many cases of postoperative flare-up of TB. However, the few cases which have been reported are worth mentioning. Singh et al. reported three cases of flare-up of TB following genital surgery.[2] In early postoperative period the all developed abdominal distension, fever, and symptoms similar to as in our case. On further evaluation, they all were diagnosed with postoperative flare-up of TB and responded to ATT.
Another case of TB flare has also been reported in a 28-year-old nulliparous woman with generalized miliary TB who underwent endometrial aspiration.[3] In another retrospective study on women who underwent vaginal hysterectomy for uterovaginal prolapse, four out of seven women who developed postoperative peritonitis and flare-up were found to have genital TB on histopathology as opposed to none out of 63 women who did not have genital TB.[4]
Postoperative flare-up of TB is not an uncommon clinical entity particularly in countries with high prevalence of TB. A high index of suspicion in cases of postoperative peritonitis should be kept in mind. However in a young asymptomatic patient in case of plastic surgery; it is perplexing presentation of tubercular flare-up and in extensive literature search not reported until date.
REFERENCES
- 1.Lazarus AA, Thilagar B. Abdominal tuberculosis. Dis Mon. 2007;53:32–8. doi: 10.1016/j.disamonth.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Singh N, Sharma AK, Dadhwal V, Gupta N, Mittal S. Postoperative flare-up of genital tuberculosis: A clinical reality. Int J Tuberc Lung Dis. 2008;12:981–3. [PubMed] [Google Scholar]
- 3.Dadhwal V, Gupta N, Bahadur A, Mittal S. Flare-up of genital tuberculosis following endometrial aspiration in a patient of generalized miliary tuberculosis. Arch Gynecol Obstet. 2009;280:503–4. doi: 10.1007/s00404-009-1082-4. [DOI] [PubMed] [Google Scholar]
- 4.Sharma JB, Mohanraj P, Jain SK, Roy KK. Increased complication rates in vaginal hysterectomy in genital tuberculosis. Arch Gynecol Obstet. 2011;283:831–5. doi: 10.1007/s00404-010-1463-8. [DOI] [PubMed] [Google Scholar]


