Abstract
Summary:
A significant aesthetic disadvantage to split skin grafts is the obvious transition between the graft and the normal skin. We report on a novel method to interrupt this transition point by using pinking shears, which are dressmaking scissors with saw-toothed blades that create a chevron pattern instead of a straight edge. We describe a case where the pinking shears were utilized on a split skin graft and Integra for reconstruction of the skin on a volar forearm. This technique allows for breaking-up of the transition point between the skin graft and normal skin and gives rise to an improved aesthetic outcome as the boundary is significantly less well-defined. This novel method shows promise and further study is certainly warranted.
Skin grafts are an invaluable tool for plastic surgeons, but they are not without complications. The significant cosmetic disadvantage associated with grafting is the obvious transition between normal skin and skin graft. We describe a novel use of pinking shears to create a serrated edge on both the skin graft and the recipient defect so as to somewhat blur the transition point between the two, thereby creating a more aesthetically pleasing wound.
A 25-year-old female was referred to our service with a view to scar revision on the volar aspect of her left forearm. She had a significant past medical history of depression and had deliberately self-harmed multiple times in the past by lacerating her left arm volar surface with a razor blade. All of these horizontal lacerations had been superficial but had produced significant and unsightly scarring. The patient’s depression had been well managed for several years and she had not deliberately self-harmed during this time frame. She was anxious for excision of the scarred area and reconstruction of the defect.
A 10 × 15 cm area of scarred skin on the volar forearm was excised en bloc under tourniquet control. The edges of the defect were freshened using pinking shears to create a serrated effect. Pinking shears are dressmaking scissors, the blades of which are saw toothed instead of straight, which leave a chevron pattern instead of a straight edge. A 10 × 20 cm piece of Integra was cut to fit the defect, and the edges of the Integra were also freshened with the pinking shears. The Integra edge was carefully lined up with the defect edge and secured with a running 5-0 Vicryl Rapide suture (Ethicon, Somerville, N.J.). A negative pressure wound therapy device was applied over this and suction was set at a continuous 75 mm Hg. The patient was discharged after 5 days, and the negative pressure wound therapy dressing was changed after 1 week. Twenty-one days after the original surgery, the patient was brought back to theater for the definitive skin graft. A split-thickness graft was harvested from the left thigh and fenestrated with a scalpel before being laid onto the Integra surface. The graft was reviewed after 1 week, and there was 100% take. The patient has been followed up as an outpatient, and 6 months postreconstruction, she is extremely happy with the results (Figs. 1–4).
Fig. 1.
The pinking shears used to create the zigzag edges.
Fig. 4.

The appearance of the Integra and skin grafted arm at 6 weeks.
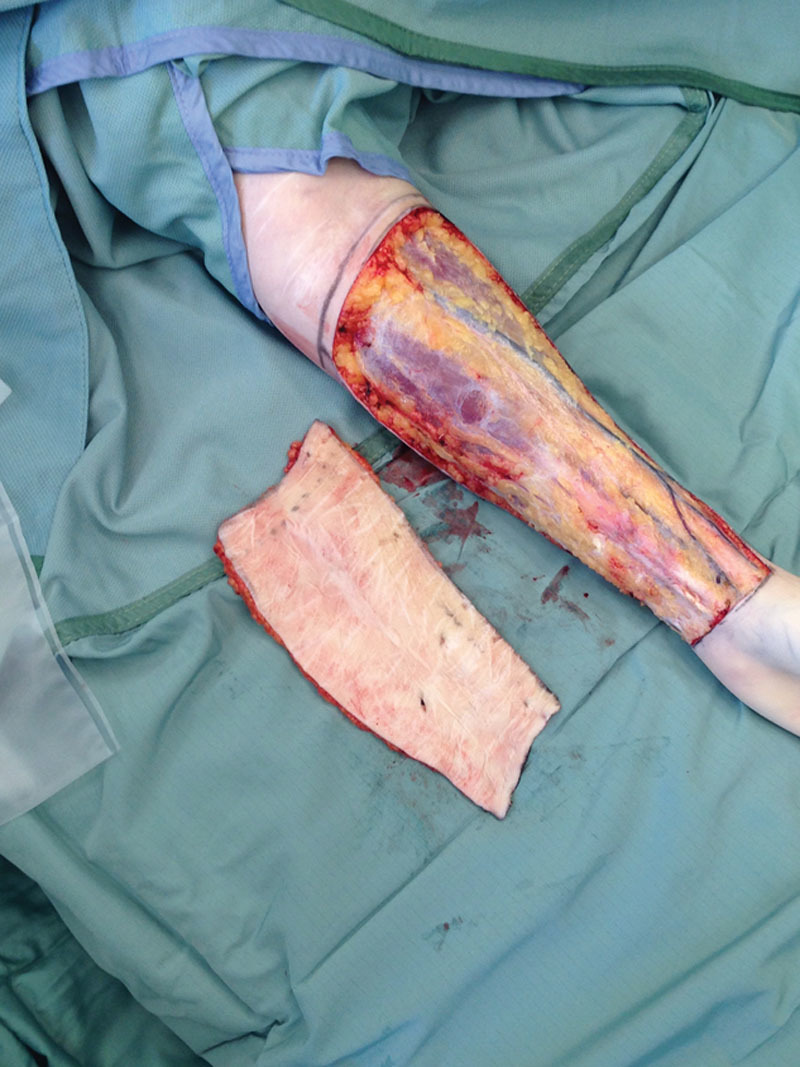
Fig. 2.

The volar forearm defect along with the excised scarred skin.
Fig. 3.

The Integra inset over the defect. The serrated edges were aligned carefully and secured with a running suture.
DISCUSSION
Despite the many documented advantages of autologous split-thickness grafting scar contracture, loss of elasticity and unfavorable aesthetic results remain a considerable problem.1 The transition between the graft and normal skin is typically very sharp and can frequently be hypertrophic. We describe a novel use of pinking shears to create a serrated edge on both the skin graft and the recipient defect, thereby rendering the transition point between the two less obvious. By breaking up the zone of transition between the graft and recipient skin, there is an improved aesthetic outcome as the boundary is less defined. Furthermore, the serrated edges of the pinking shears are at an angle of approximately 45 degrees, therefore elongating the length of the graft edge by nearly 50%.
Split-thickness skin grafts in the forearm often lead to motion restriction and disability through dense scarring of the skin. The combination of Integra and the pinking shears theoretically results in less scar contraction than if a split-thickness skin graft had been used alone.2 The use of pinking shears to obtain serrated edges on both the skin graft and the recipient defect has resulted in an improved aesthetic outcome due to breaking up the scarred boundary. Also, by lengthening the scar, there may be less hypertrophic scarring and also decreased contracture formation. This novel technique described may be most useful in reconstructing unsightly donor sites such as the volar aspect of the forearm after a radial forearm flap.
Conclusion
The use of pinking shears to break up the transition point between the skin graft and normal skin is a novel technique to improve the aesthetic outcome for split thickness skin grafts and we feel it certainly warrants further study.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Park JY, Lee TG, Kim JY, et al. Acellular dermal matrix to treat full thickness skin defects: follow-up subjective and objective skin quality assessments. Arch Craniofac Surg. 2014;15:14–21. doi: 10.7181/acfs.2014.15.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wise DM. Acellular dermal matrix in hand reconstruction. Plast Reconstr Surg. 2013;132:677e–679e. doi: 10.1097/PRS.0b013e3182a015b3. [DOI] [PubMed] [Google Scholar]


