Abstract
Background:
In 1953, the sagittal ramus split osteotomy was introduced by Obwegeser. For many years, and in some countries still, this technique has defined the term oral and maxillofacial surgery.
Methods:
The basic design of the sagittal ramus split surgical procedure evolved very quickly. The original operation technique by Obwegeser was shortly after improved by Dal Pont’s modification. The second major improvement of the basic technique was added by Hunsuck in 1967. Since then, the technical and biological procedure has been well defined. Resolution of the problems many surgeons encountered has, however, taken longer. Some of these problems, such as the unfavorable split or the damage of the inferior alveolar nerve, have not been satisfactorily resolved.
Results:
Further modifications, with or without the application of new instruments, have been introduced by Epker and Wolford, whose modification was recently elaborated by Böckmann. The addition of a fourth osteotomy at the inferior mandibular border in an in vitro experiment led to a significant reduction of the torque forces required for the mandibular split.
Conclusions:
The literature was reviewed, and the last modifications of the successful traditional splitting procedure are presented narrowly. It indicates the better the split is preformatted by osteotomies, the less torque force is needed while splitting, giving more controle, a better predictability of the lingual fracture and maybe less neurosensory disturbances of the inferior alveolar nerve.
The historical development of orthognathic surgery has followed a rather stepwise, intermittent course. The first mandibular osteotomy is considered to be Hullihen’s1 procedure in 1849 for the correction of a protruded alveolar mandibular segment. The first osteotomy of the whole mandibular body for the correction of prognathism was performed by Blair2 in 1897. He was also the first author to present a classification of jaw deformities. The operations performed, described, and published by Blair and Angle3 marked the beginning of the development of oral surgery. In 1953, the sagittal split osteotomy evolved into a procedure that could be accomplished intraorally, without transfacial approaches and without leaving visible scars. The bilateral sagittal split osteotomy (BSSO) can be considered a milestone in surgery in general.4,5 The following review of the literature is an attempt to isolate the modifications, which marked significant advances of this technique.
REVIEW OF THE LITERATURE
In 1907, Blair2 published the horizontal subcondylar osteotomy of the mandible to correct class II dysgnathias by advancement of the mandibular body. This technique required prolonged intermaxillary fixation, which was already regarded as an inconvenience due to a lack of bone contact between the osteotomized segments. A modification of this technique was recently published again by Hågensli et al.6 Using an overlapping segmentation technique and osteosynthesis plates, they claimed to achieve good bone healing. Schuchardt7 modified the horizontal flat osteotomy by introducing a technique in which a cortical osteotomy was performed in an oblique way starting from just above the lingula and reaching the buccal cortex 1 cm more caudally without touching the intra-alveolar nerve (IAN). The Schuchardt operation could be performed intraorally and led to a more sufficient medullary bone attachment. However, without fixation of the proximal and distal segments, this procedure only led to a minor reduction of complications. Trauner and Obwegeser4,5 further developed Schuchardt’s technique by increasing the gap between the horizontal cuts to 25 mm, requiring the surgeon to address the IAN. Their innovation resulted from connecting 2 horizontal cortical cuts along the lateral oblique ridge and leaving the posterior border of the ramus untouched. Eventually, the fracture of the ramus was achieved by chiseling along the lateral cortex. This procedure was called the sagittal splitting procedure, and it kept the IAN intact. The wider distance between the lingual and buccal cuts increased the overlapping bony amount of the segments, which rendered better stability and better results at a lower risk of pseudarthrosis (Fig. 1). Obwegeser revolutionized oral and maxillofacial surgery by introducing the BSSO as a standardized and safe procedure, which is performed worldwide to date in the originally described manner.
Fig. 1.
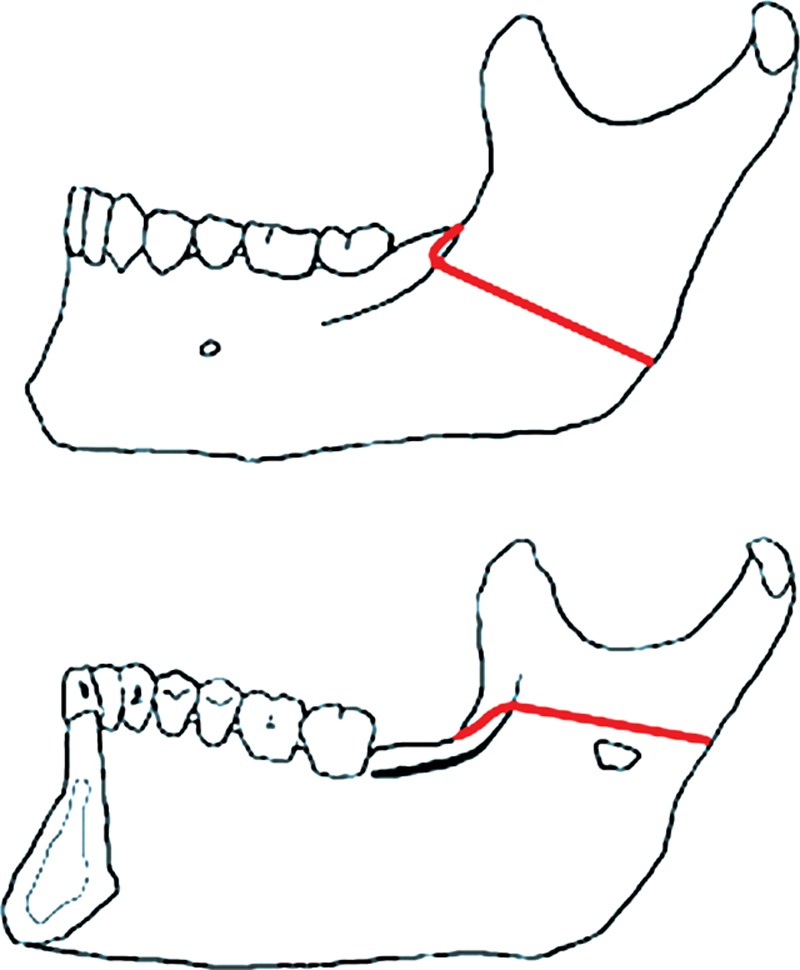
The sagittal split as described by Obwegeser. The buccal and lingual osteotomy lines are indicated.
In times of osteosynthesis by wiring, Dal Pont’s8 modification advances and rotates the lower horizontal cut even further to the buccal cortex of the mandibular body as a vertical cut between the first and second molars. The angle created between the lingual and buccal cortical cuts was approximately 90 degrees, leading to an extension of the connecting cut along the oblique line on the lateral mandibular aspect through the mylohyoid groove on the lingual side (Fig. 2). In the same article, Dal Pont reported a less quoted alternative technique that he called the “oblique retromolar osteotomy.” The lingual horizontal corticotomy ended just behind the lingula. However, it was Hunsuck9 who thought that it was not necessary to make an actual cut through the lingula as Dal Pont had done in his technique. Hunsuck was convinced that the lingual split of the Dal Pont osteotomy would occur naturally given that chisels were used to split the mandible. The buccal vertical cut by Hunsuck was located at the “union of the ascending ramus and the body of the mandible in the tooth bearing region.” In Hunsuck’s illustrations, this area was just distal of the second molar running down to the mandibular notch anterior of the insertion point of the masseteric muscle (Fig. 3). As with Obwegeser, a single wire was placed at the anterior aspect of the ascending ramus at the height of the occlusal plane. All 3 techniques by Obwegeser, Dal Pont, and Hunsuck required tunneling of the lingual pterygomandibular space with only minimal muscular or periosteal stripping. A massetericomandibular tunnel was only necessary in the original technique described by Obwegeser.4
Fig. 2.
The first modification of the sagittal split by Dal Pont. The buccal and lingual osteotomy lines are indicated.
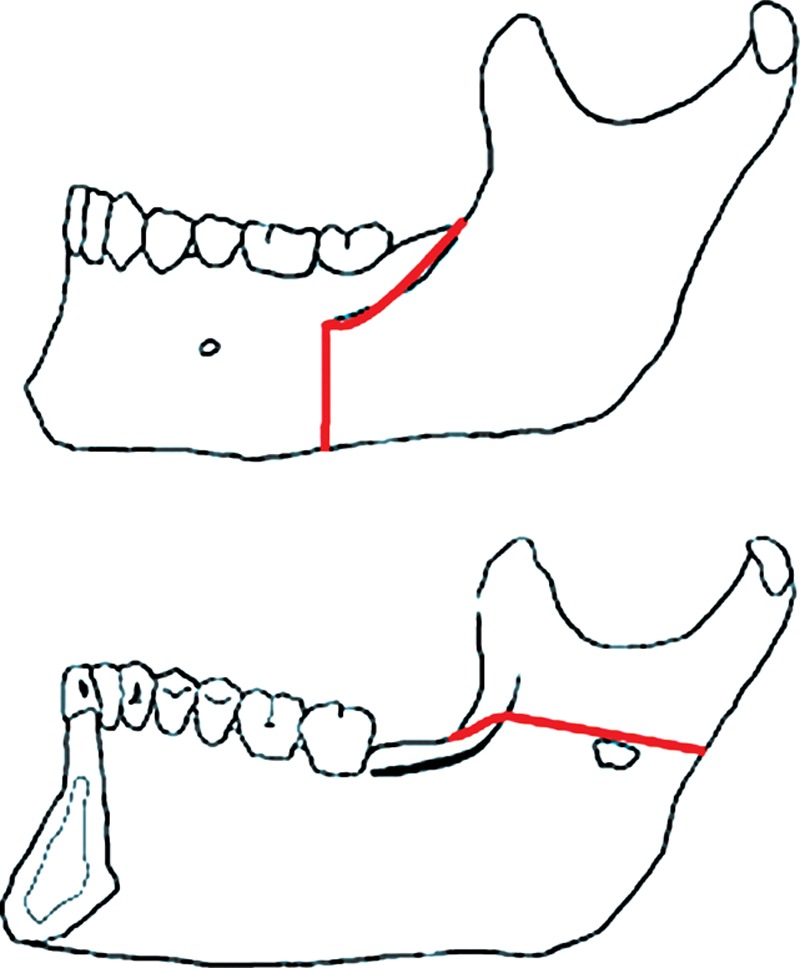
Fig. 3.
The modification of the lingual cut according to Hunsuck and Epker. Notice the short horizontal cut on the lingual side.
In 1977, a very important article on the biological basis of the BSSO was published by Bell and Schendel.10 This article tried to explain some of the problems biologically, and it laid the path for future modifications. It was a reminder that the clinical success of a surgical technique must be based on or proven or at least guided by laboratory research. The Bell and Schendel publication delineated the basic principles leading to the article published by Epker in 1977.11 Based on the growing knowledge on muscular and temporomandibular joint function, a more biological modification evolved. Wide reflection of the masseteric muscle to prevent relapse was denied by Epker in favor of a 2-wire stabilization of both segments proximally low and distally high. Therefore, the condylar sag leading to relapse could be prevented. Furthermore, Epker refined the original Dal Pont technique by explaining the buccal corticotomy in detail, emphasizing the need for a complete osteotomy of the inferior mandibular cortex to avoid bad splits.
Following the foundation of the “Arbeitsgemeinschaft für Osteosynthesefragen” (AO) at Biel, Switzerland, in 1958, the next revolution started affecting the BSSO technique. In 1976, Spiessl12 published their book New Concepts in Maxillofacial Bone Surgery in which they introduced rigid internal fixation in the form of interfragmentary bone screws. Their research showed that the screws added to the stability of the fragments and decreased healing time because of fragment compression osteosynthesis. In addition, Spiessl also favored the use of thin bone saws for precise osteotomies over thicker burrs, thereby saving as much bone as possible to reduce the gap between the split segments. Only small gaps were allowed for stable compression osteosynthesis. Spiessl also introduced a new osteotomy technique by removing the lingual aspect of the cortical bone plate covering the oblique line in the retromolar region. By its removal, a good overview was created to discern the cancellous and cortical bone structures of the retromolar lingual mandible. He also performed the first preliminary anatomical studies on the variation of the location of the mandibular nerve in relation to the lateral mandibular cortex.
In the 1980s, Bell et al13,14 and Steinhäuser and Rudzki-Janson15 published 2-volume book sets about the basic principles of the osteotomy techniques in orthognathic surgery. These books continue to be used as basic literature for those beginning to perform orthognathic surgery. Whereas Bell failed to introduce rigid screw fixation, Steinhäuser did follow the principles of the AO and reported on it to his American colleagues. Bell et al16 then switched from the wire osteosynthesis to rigid fixation in 1985 by adding a third volume to his existing 2-volume book sets.
Nevertheless, the problem of injuring the inferior alveolar nerve remained. In 1986, using the new computed tomography scan technology at that time, Rajchel et al17 suggested rethinking the position of the anterior buccal osteotomy. He was the first author to report specifically on the mediolateral position of the mandibular nerve, and he concluded that the buccal vertical corticotomy has to be located in the region of the first molar for the safety of the IAN. He described this region as a “bony prominence, an extension of the lateral oblique line.” Anatomically, this description is correct, as the area just distal to the second molar is the region where the neurovascular bundle is most often located in direct contact with the buccal cortex. Occasionally, the neurovascular bundle and canal seem to be within the buccal cortical plate. The risk of injuring the inferior alveolar nerve is high.
Wolford et al18 and Obwegeser and Hadjianghelou19 reacted to this article. Wolford agreed on moving the vertical cut further anterior in the region of the first and second molars to avoid direct trauma to the inferior alveolar nerve. Furthermore, he was in favor of using position screws over compression screws to prevent possible traumatic nerve compression and condylar displacement. He was the first author to recommend early mobilization of the mandible resulting from the rigid osteosynthetic fixation. This early functional approach was intended to mobilize the temporomandibular joints as early as possible. Obwegeser responded to the discussion started by Rajchel with an article titled “Two ways to treat bird-face deformity.” The interesting aspect of that article was his use of a vertical cut that was even further forward than in any previously published article. The vertical cut was located between the second premolar and first molar. Based on the studies performed by Rajchel, this modification is reasonable because depending on the location of the mental foramen, the inferior alveolar nerve is usually still located medially at that point.
Radiological studies on the lingual split design revealed that in the conventional technique, the split usually occurred in the lingual cortical plate. A high lingual split made it impossible to place the third screw inferiorly to the alveolar canal, as there was no bone for fixation on the lingual side. Therefore, Wolford and Davis20 introduced the concept of the inferior border split in 1990. A specially designed saw was used to cut the inferior border, thus leading to a low lingual split. Another advantage of the Wolford modification was that the inferior alveolar nerve was less frequently found in the proximal segment, where the nerve is more prone to trauma due to tension, bad visualization, and separation of the nerve from the canal.
Rigid internal fixation has been the state-of-the-art fixation in orthognathic surgery since the 1980s. Its advantages are obvious: no rigid intermaxillary fixation is necessary, which contributes to patient comfort, and fragments tend not to displace after they have been rigidly, internally fixed, compared with fixation using wire osteosynthesis. The latter advantage is extremely important because pull of the masticatory and anterior neck muscles tends to dislocate the fragments, particularly in the mandible when advancing the mandible after a BSSO procedure.
In essence, a sagittal split osteotomy can be fixed in 3 ways: using lag screws, positional screws, and miniplates with monocortical screws. Lag screws were introduced by Spiessl21 and were later popularized by Paulus and Steinhäuser.22 Three screws are usually used, engaging the buccal cortex of the proximal fragment and the lingual cortex of the distal fragments. Screw threads only engage the lingual cortex. Positional screws are most likely used more often and follow the same principle as lag screws in that usually 3 screws are used, engaging both cortices. The difference is that the fragments are not pulled together as tightly as in the case of lag screws because screw threads engage both cortices. The principle of the use of miniplates was introduced by Michelet et al.23 Michelet and Champy started to use small osteosynthesis plates with monocortical screws in trauma and orthognathic patients, thus introducing the term “functional stability” versus rigid compression osteosynthesis as defined by the AO. The advantages of miniplate fixation are well documented in the literature.24–26
Recently, distraction osteogenesis (DO) for mandibular retrognathia has become of increasing interest. Although randomized clinical trials are lacking, some support was found for DO having advantages over the classical BSSO in the surgical treatment of low and normal mandibular plane angle patients needing greater advancement of more than 7 mm. The technique of bone splitting tends to prefer the Dal Pont osteotomy as this approach enables better fixation of the distraction device. Long-term results as presented by de Lange and coworkers showed no advantage of DO against the classical splitting procedures. There might be an indication for DO in extreme cases of mandibular micrognathia as, for example, in syndromal diseases.27–29
However, the introduction of DO in combination with ultrasonic bone-cutting surgery (piezosurgery) has changed the way of cutting the mandibular bone.30 The piezosurgery medical devices allow the efficient cutting of mineralized, hard tissues with minimal trauma to soft tissues. The advantages include minimal risks to critical soft structures, such as the vessels and nerve in the mandibular canal. The oblique osteotomy line can be placed in the retromolar region and runs from the anterobuccal side in a posteromedian direction to the lingual side of the mandibular body. Due to the osteogenic effect of DO, a wide overlap of bone segments as in the classical BSSO is not required. Thus, the introduction of piezosurgery in combination with DO seems to put the old osteotomy techniques into perspective.
Despite a large number of variations of the original Obwegeser–Dal Pont splitting technique, the risk of unexpected fractures is a major disadvantage of the BSSO,31 known as “bad splits.” Previous reports have cited an incidence of bad splits of up to 5% despite improved preoperative diagnostics. In addition, the temporary or lasting damage of the IAN remains relevant. According to the literature, postoperative damage varies from 13% to 40%.32,33
Teerijoki-Oksa et al34 identified the splitting maneuver itself as one of the 2 main risks of damaging the IAN. It is common sense that a sufficiently deep cut to the inferior mandibular rim is crucial for a good splitting. This problem has previously been addressed by Wolford and Davis20 with the development of a special cutting saw. Due to its design and consequent risk of damaging the facial artery, this instrument never became popular.
In their studies, Böckmann et al35 continued to investigate the advantages of adding a fourth caudal osteotomy parallel with inferior mandibular rim (Figs. 4–6). Wolford’s hypothesis was that weakening the inferior mandibular border would result in the proximal cortical border of the ramus as the only cortex to split spontaneously. In doing so, one may achieve a more predictable splitting (Fig. 7). The acquired data confirmed the theory.35 In the animal cadaver study, it could be demonstrated that with support of a fourth osteotomy, a reasonable splitting result was always possible to achieve, staying off the IAN during the splitting procedure at the same time.
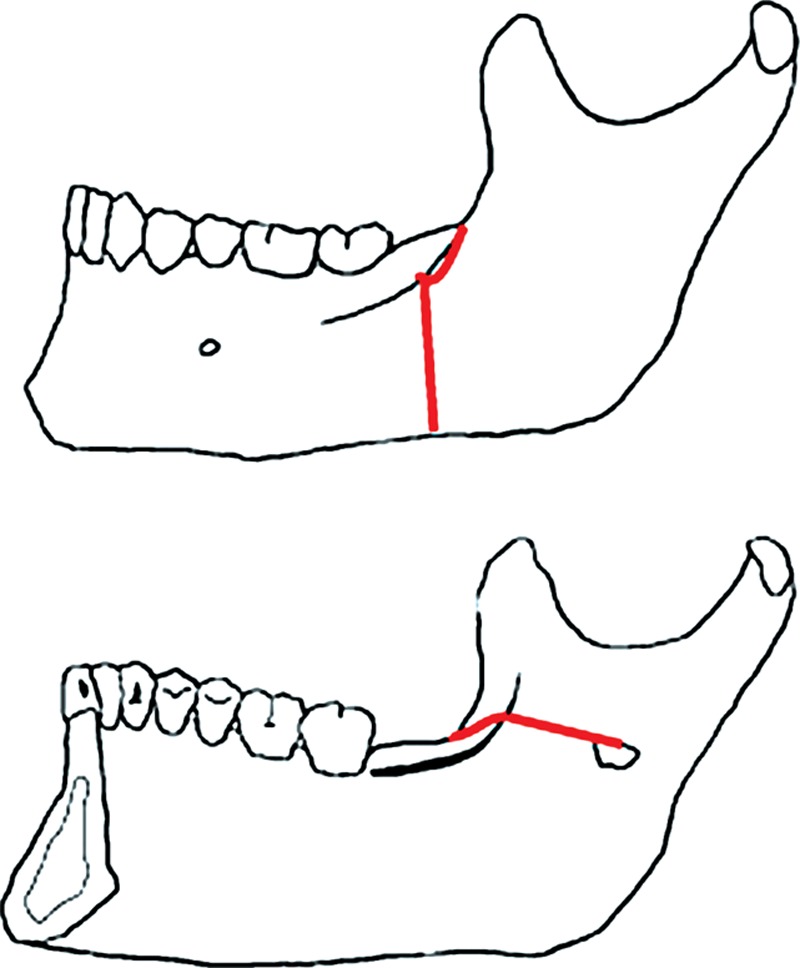
Fig. 4.
Introduction of the caudal (fourth) osteotomy. As the osteotomy reaches the mandibular angle, it allows the surgeon to split the mandible as if opening a book.
Fig. 6.
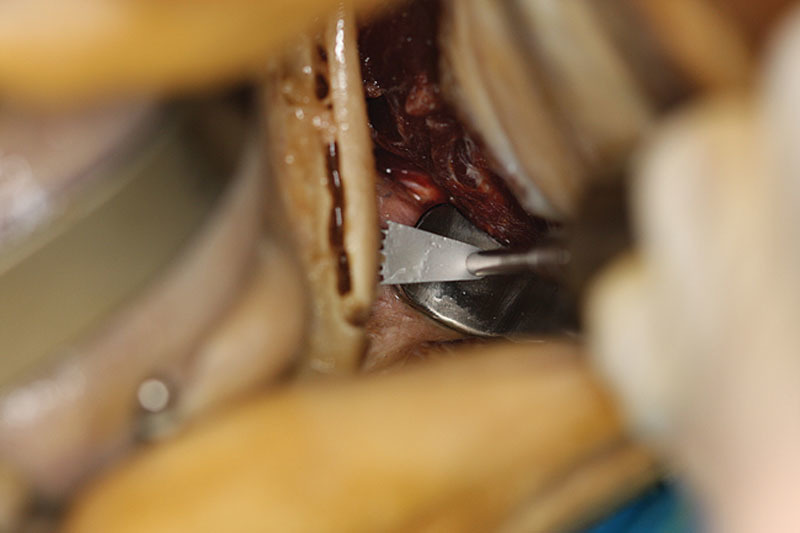
Oscillating saw in situ for preparation of the fourth osteotomy line at the inferior mandibular rim. An L-shield protects the surrounding soft tissue and guides the saw.
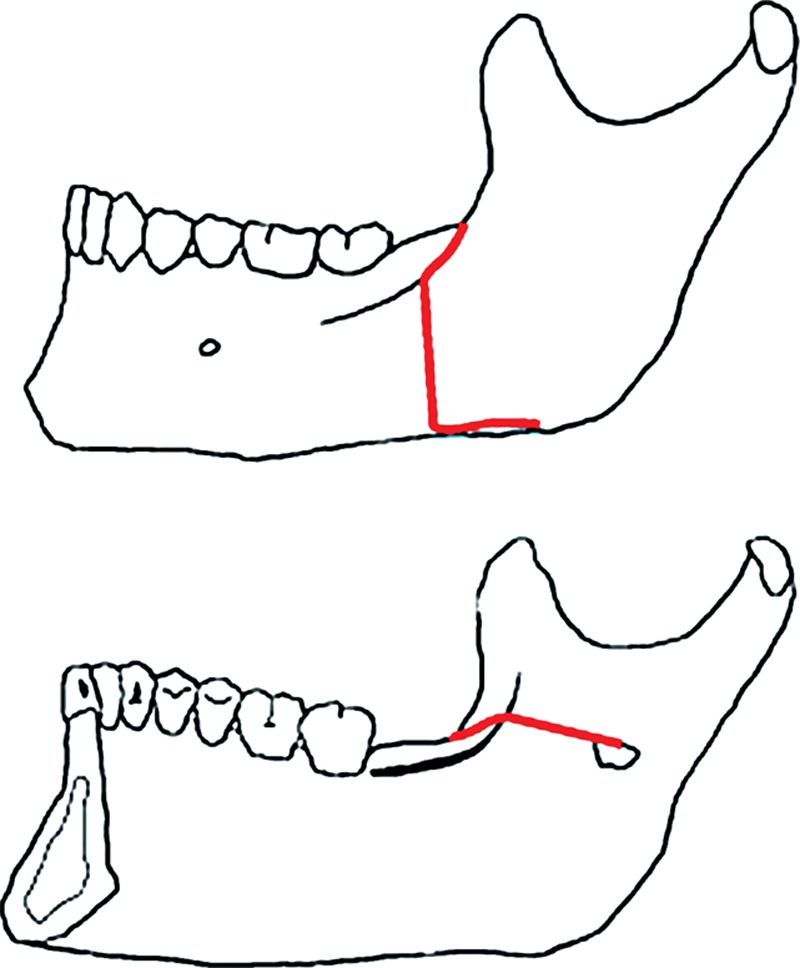
Fig. 7.
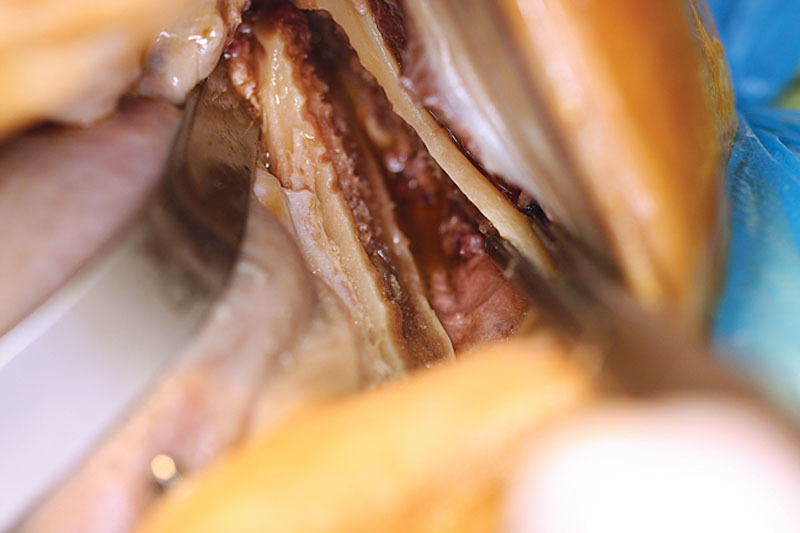
Splitting pattern in the same mandible supported by a fourth osteotomy.
Fig. 5.
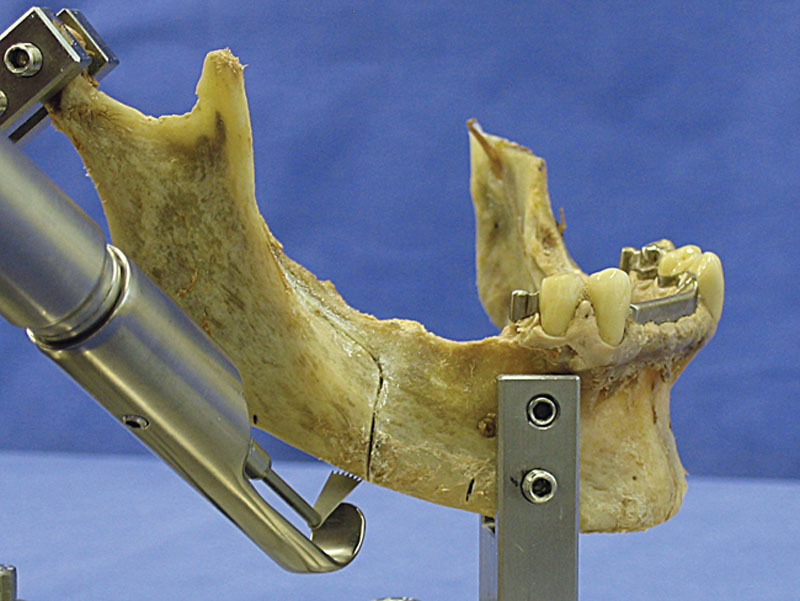
Buccal view of the fourth osteotomy line in a human mandible mounted on a test rack.
DISCUSSION
The literature review indicates that all of the major aspects of the design of the sagittal split technique were in place with Hunsuck’s modification of the basic Obwegeser–Dal Pont technique. The fact that there are continued attempts to improve this technique is a testament to the understanding of the value of this 60-year-old procedure.35 The subsequent modifications have generally focused on the attempts to manage or minimize the intra- or postsurgical problems that have since emerged. The major problems include neurological injuries, unfavorable splits, relapse, fragment, and condylar resorption. There are, however, no easy solutions to the problems that continue to occur, and most of these problems will likely always be associated with the BSSO technique.
Modifying the Obwegeser–Dal Pont technique by adding an osteotomy of the inferior border of the mandible might be a step in this direction. The research published by Wolford et al has been a valuable guide for locating the additional osteotomy line. The Dal Pont modification, backed up with the anatomical studies by Rajchel et al, indicates that the most favorable area for the buccal cut is in the region between the first and second molars. The distance between the inner aspect of the buccal cortical plate and the mandibular canal is consistently bigger in that location than elsewhere, though the exact spot varies from patient to patient. When considering possible fracture lines on the lingual mandibular aspect connecting the posterior end of the horizontal osteotomy and the inferior end of the vertical osteotomy, it is obvious that a fourth osteotomy line at the inferior rim of the mandibular corpus will shorten the necessary connecting fracture line. In an ideal setting, the inferior cut will naturally be located in the middle of the inferior border. The length of the fourth osteotomy line is essential, in facilitating a safe split, as this line has to connect the buccal cut with the region where the ascending ramus and the body of the mandible meet.
CONCLUSION
Most of the modifications of the original splitting procedure in the first 20 years after its introduction were meant to minimize the risk of pseudarthrosis, nonunion, and 2 split segments. With the introduction of osteosynthesis by screws or by miniplates, this problem has been solved, and the focus has shifted to other complications such as the unfavorable split or the damage of the IAN. These 2 problems are partially linked to one another. One imaginable approach to target both problems is the use of a caudal, a fourth, osteotomy of the mandibular body. Currently, there is no suitable instrument at hand that is easy to handle and that allows the surgeon to cut the inferior border in a predictable and safe way to reduce complications in orthognathic splitting procedures.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. A portion of the Article Processing Charge was paid for by PRS Global Open at the discretion of the Editor-in-Chief. The remainder of the Article Processing Charge was paid for by the academic hospital Maastricht, The Netherlands.
REFERENCES
- 1.Hullihen SP. Case of elongation of the underjaw and distorsion of the face and neck, caused by a burn, successfully treated. Am J Dent Sci. 1849;9:157–161. [PMC free article] [PubMed] [Google Scholar]
- 2.Blair V. Operations on the jaw-bone and face. Surg Gynecol Obstet. 1907;4:67–78. [Google Scholar]
- 3.Biederman W.: The strange story of the Angle operation. Ann Dent. 1956;15:1–9. [Google Scholar]
- 4.Trauner R, Obwegeser HL. Zur Operationstechnik bei der Progenia und anderen Unterkieferanomalien. Dtsch Zahn Mund Kieferheilkd. 1955;23:11–25. [Google Scholar]
- 5.Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957;10:677–689; contd. doi: 10.1016/s0030-4220(57)80063-2. [DOI] [PubMed] [Google Scholar]
- 6.Hågensli N, Stenvik A, Espeland L. Extraoral vertical subcondylar osteotomy with rigid fixation for correction of mandibular prognathism. Comparison with bilateral sagittal split osteotomy and surgical technique. J Craniomaxillofac Surg. 2013;41:212–218. doi: 10.1016/j.jcms.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Schuchardt K. Ein Beitrag zur chirurgischen Kieferor thopädie unter Berücksichtigung ihrer für die Behandlung angeborener und erworbener Kieferdeformitäten bei Soldaten. Dtsch Zahn Mund Kieferheil. 1942;9:73–89. [Google Scholar]
- 8.Dal Pont G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anesth Hosp Dent Serv. 1961;19:42–47. [PubMed] [Google Scholar]
- 9.Hunsuck EE. A modified intraoral sagittal splitting technic for correction of mandibular prognathism. J Oral Surg. 1968;26:250–253. [PubMed] [Google Scholar]
- 10.Bell WH, Schendel SA. Biologic basis for modification of the sagittal ramus split operation. J Oral Surg. 1977;35:362–369. [PubMed] [Google Scholar]
- 11.Epker BN. Modifications in the sagittal osteotomy of the mandible. J Oral Surg. 1977;35:157–159. [PubMed] [Google Scholar]
- 12.Spiessl B. Rigid internal fixation after sagittal split osteotomy of the ascending ramus. In: Spiessl B, editor. In: New concepts in maxillofacial bone surgery. Berlin: Springer-Verlag; 1976. pp. 115–122. [Google Scholar]
- 13.Bell WH, Proffit WR, White RP. Surgical Correction of Dentofacial Deformities. Vol. 1. Philadelphia: W.B. Saunders Company; 1980. [Google Scholar]
- 14.Bell WH, Proffit WR, White RP. Surgical Correction of Dentofacial Deformities. Vol. 2. Philadelphia: W.B. Saunders Company; 1980. [Google Scholar]
- 15.Steinhäuser EW, Rudzki-Janson IM. Kieferorthopädische Chirurgie. 2. Behandlungsablauf bei typischen Dysgnathie formen. Vol. 2. Berlin: Quintessenz-Verlag; 1994. [Google Scholar]
- 16.Bell WH, Proffit WR, White RP. Surgical Correction of Dentofacial Deformities. Vol. 3. Philadelphia: W.B. Saunders Company; 1985. [Google Scholar]
- 17.Rajchel J, Ellis E, III, Fonseca RJ. The anatomical location of the mandibular canal: its relationship to the sagittal ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 1986;1:37–47. [PubMed] [Google Scholar]
- 18.Wolford LM, Bennett MA, Rafferty CG. Modification of the mandibular ramus sagittal split osteotomy. Oral Surg Oral Med Oral Pathol. 1987;64:146–155. doi: 10.1016/0030-4220(87)90080-6. [DOI] [PubMed] [Google Scholar]
- 19.Obwegeser HL, Hadjianghelou O. Two ways to correct bird-face deformity. Oral Surg Oral Med Oral Pathol. 1987;64:507–518. doi: 10.1016/0030-4220(87)90023-5. [DOI] [PubMed] [Google Scholar]
- 20.Wolford LM, Davis WM., Jr. The mandibular inferior border split: a modification in the sagittal split osteotomy. J Oral Maxillofac Surg. 1990;48:92–94. doi: 10.1016/0278-2391(90)90190-d. [DOI] [PubMed] [Google Scholar]
- 21.Spiessl B. The sagittal splitting osteotomy for correction of mandibular prognathism. Clin Plast Surg. 1982;9:491–507. [PubMed] [Google Scholar]
- 22.Paulus GW, Steinhauser EW. A comparative study of wire osteosynthesis versus bone screws in the treatment of mandibular prognathism. Oral Surg Oral Med Oral Pathol. 1982;54:2–6. doi: 10.1016/0030-4220(82)90408-x. [DOI] [PubMed] [Google Scholar]
- 23.Michelet FX, Benoit JP, Festal F, et al. [Fixation without blocking of sagittal osteotomies of the rami by means of endo-buccal screwed plates in the treatment of antero-posterior abnormalities]. Rev Stomatol Chir Maxillofac. 1971;72:531–537. [PubMed] [Google Scholar]
- 24.Stoelinga PJ, Borstlap WA. The fixation of sagittal split osteotomies with miniplates: the versatility of a technique. J Oral Maxillofac Surg. 2003;61:1471–1476. doi: 10.1016/j.joms.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, et al. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part I. Clinical parameters. Int J Oral Maxillofac Surg. 2004;33:433–441. doi: 10.1016/j.ijom.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 26.Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, et al. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part III—condylar remodelling and resorption. Int J Oral Maxillofac Surg. 2004;33:649–655. doi: 10.1016/j.ijom.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 27.Schreuder WH, Jansma J, Bierman MW, et al. Distraction osteogenesis versus bilateral sagittal split osteotomy for advancement of the retrognathic mandible: a review of the literature. Int J Oral Maxillofac Surg. 2007;36:103–110. doi: 10.1016/j.ijom.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Wiltfang J, Hirschfelder U, Neukam FW, et al. Long-term results of distraction osteogenesis of the maxilla and midface. Br J Oral Maxillofac Surg. 2002;40:473–479. doi: 10.1016/s0266435602002474. [DOI] [PubMed] [Google Scholar]
- 29.Baas EM, Pijpe J, de Lange J. Long term stability of mandibular advancement procedures: bilateral sagittal split osteotomy versus distraction osteogenesis. Int J Oral Maxillofac Surg. 2012;41:137–141. doi: 10.1016/j.ijom.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 30.Rana M, Gellrich NC, Rana M, et al. Evaluation of surgically assisted rapid maxillary expansion with piezosurgery versus oscillating saw and chisel osteotomy—a randomized prospective trial. Trials. 2013;14:49. doi: 10.1186/1745-6215-14-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kriwalsky MS, Maurer P, Veras RB, et al. Risk factors for a bad split during sagittal split osteotomy. Br J Oral Maxillofac Surg. 2008;46:177–179. doi: 10.1016/j.bjoms.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 32.Colella G, Cannavale R, Vicidomini A, et al. Neurosensory disturbance of the inferior alveolar nerve after bilateral sagittal split osteotomy: a systematic review. J Oral Maxillofac Surg. 2007;65:1707–1715. doi: 10.1016/j.joms.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 33.Nesari S, Kahnberg KE, Rasmusson L. Neurosensory function of the inferior alveolar nerve after bilateral sagittal ramus osteotomy: a retrospective study of 68 patients. Int J Oral Maxillofac Surg. 2005;34:495–498. doi: 10.1016/j.ijom.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 34.Teerijoki-Oksa T, Jääskeläinen SK, Forssell K, et al. Risk factors of nerve injury during mandibular sagittal split osteotomy. Int J Oral Maxillofac Surg. 2002;31:33–39. doi: 10.1054/ijom.2001.0157. [DOI] [PubMed] [Google Scholar]
- 35.Böckmann R, Schön P, Frotscher M, et al. Pilot study of modification of the bilateral sagittal split osteotomy (BSSO) in pig mandibles. J Craniomaxillofac Surg. 2011;39:169–172. doi: 10.1016/j.jcms.2010.04.002. [DOI] [PubMed] [Google Scholar]


