Abstract
Background:
The present retrospective cohort study was performed to determine the efficacy of contact-mode 1064 nm neodymium-yttrium-aluminum-garnet (Nd:YAG) laser laser for keloids and hypertrophic scars. The indication and limitations of this modality are discussed.
Methods:
The cohort consisted of 102 consecutive Japanese patients (23 males and 79 females) with keloids and hypertrophic scars for more than 1 year. They were treated every 3–4 weeks for 1 year with a long-pulsed 1064 nm Nd:YAG laser (Cutera, Brisbane, Calif.) in contact mode. Thirty-eight patients had hypertrophic scars and 64 had keloids. The scars were evaluated before the treatment commenced and 1 month after the last session by using the Japan Scar Workshop Scar Scale 2011. Recurrence was assessed at 6 months after the termination of treatment.
Results:
The average total Japan Scar Workshop score of the keloid and hypertrophic scar region groups dropped significantly after 1 year of treatment compared with before treatment (all P < 0.05). None of the hypertrophic scars or keloids deteriorated. However, 3 of the 34 anterior chest keloids (8.8%) did not respond. The following recurrence rates were observed 6 months after stopping laser treatment: 1 of the abdomen hypertrophic scars (4%), 18 of the anterior chest keloids (52.9%), 5 of the upper arm keloids (35.7%), and 4 of the scapula keloids (25%).
Conclusions:
Hypertrophic scars responded significantly better to 1064 nm Nd:YAG laser treatment than keloids. However, keloid recurrence occurred when there was remaining redness and induration, even if only a small part of the scar was affected.
Pulsed-dye laser (PDL) has long been the therapy of choice for cutaneous vascular diseases1; however, although PDL is effective for vascular diseases affecting the superficial layers (ie, the epidermis and papillary layers of the dermis), it does not reach the deep dermal regions (ie, the reticular layer of the dermis). Because 1064 nm neodymium-yttrium-aluminum-garnet (Nd:YAG) laser reaches more deeply than PDL, it is increasingly being used to treat deep vascular diseases such as hypertrophic scars and keloids instead of PDL. It has been suggested that it acts by suppressing neovascularization in these pathological scars, which are characterized by vessel overgrowth that results in nerve fibers and collagen in the reticular layer of the dermis.
The 1064 nm Nd:YAG laser (Cutera, Brisbane, Calif.) plays an important role in our treatment algorithms for keloids and hypertrophic scars.2 This long-pulsed (not Q-switched) Nd:YAG laser was developed for the treatment of vascular diseases and scars, for hair removal, and for skin rejuvenation. The depth that is reached is determined by the spot size, laser power, and fluence; the larger the spot size, power, or fluence, the deeper the laser beam penetrates, and thus, a large spot size and/or power are used for deep targets, hair removal, and deep reticular vessels. The 1064 nm Nd:YAG laser can be used in noncontact mode (this method is registered as Genesis) and in contact mode. It is believed that the contact mode penetrates twice as deep as Genesis.3 Moreover, Genesis results in less pain than the contact mode.
Our group initially started using Genesis for pathological scars, including keloids and hypertrophic scars, that are accompanied by itch and pain due to chronic inflammation. However, although Genesis yielded satisfactory results with hypertrophic scars, it was not particularly effective with keloids.2 In summary, 22 Japanese patients with keloids and hypertrophic scars were treated every 3–4 weeks by Genesis using a 5-mm spot size diameter, an energy density of 14 J/cm2, a 300-μs exposure time per pulse, and a 10-Hz repetition rate. Of the 22 patients, 8 exhibited a clear reduction in the size of their lesions (<90% of the original area), 10 exhibited a slight reduction (90–95%), and 4 showed no change (>95%).
Therefore, in 2009, our group started to use the contact mode to treat the thicker and harder keloids and hypertrophic scars. In this retrospective cohort study, the efficacy of contact-mode 1064 nm Nd:YAG laser therapy for keloids and hypertrophic scars was assessed. The indications and limitations of this method are discussed.
STUDY DESIGN AND METHOD
The cohort consisted of all 102 consecutive Japanese patients (23 males and 79 females) with keloids and hypertrophic scars who were treated every 3–4 weeks for 1 year with long-pulsed 1064 nm Nd:YAG laser (Cutera, Brisbane, Calif.) in contact mode at a scar-specialist outpatient clinic of the Department of Plastic, Reconstructive and Aesthetic Surgery of Nippon Medical School in Tokyo, Japan between April 2009 and October 2011. The mean age of the cohort was 34.8 years, and 38 had hypertrophic scars on the upper lip (caused by trauma), lower lip (caused by trauma), or abdomen (caused by abdominal surgery), whereas 64 had keloids on the anterior chest (caused by acne), upper arm (caused by vaccination), or scapula (caused by acne) (Fig. 1). All cases were previously treated for more than 1 year with other therapies such as steroid ointment or tape, but an improvement was not observed. In the present study, a keloid was defined as a scar that extended beyond the confines of the original wound. Cases where it was difficult to judge whether the lesion was a keloid or a hypertrophic scar were excluded from this study. Moreover, large and thick keloids were treated by other treatment modalities such as surgery and postoperative radiation; thus, they were also excluded from this case series. Laser treatment was halted after 1 year, and 6 months later, the scar was assessed for recurrence.
Fig. 1.
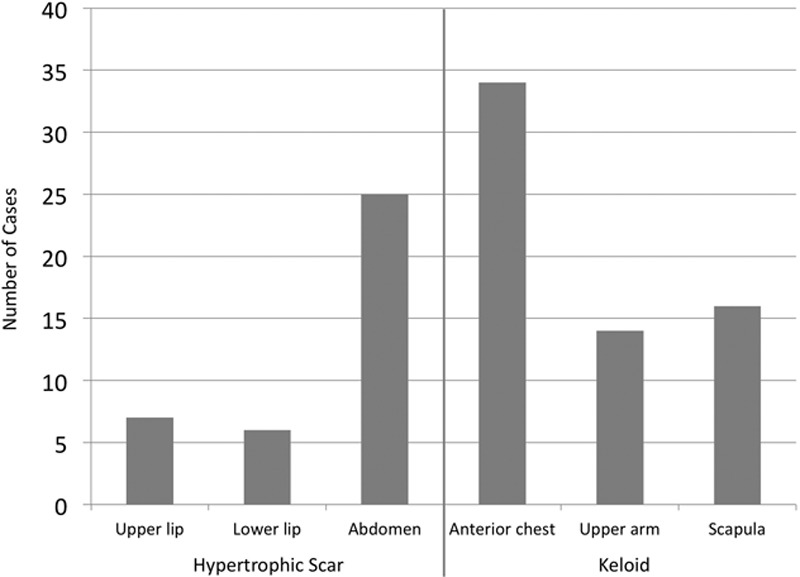
Characteristics of the 102 cases of hypertrophic scars and keloids enrolled in this study. Of the 102 cases, 38 had hypertrophic scars on the upper lip, lower lip, or abdomen and 64 had keloids on the anterior chest, upper arm, or scapula.
The laser irradiation was applied to the skin surface with the following treatment settings: a spot size diameter of 5 mm, an energy density of 65–75 J/cm2, an exposure time per pulse of 250 μs (0.25 millisecond), and a repetition rate of 2 Hz. The copper-cooling tip of the hand piece was used to cool the skin before or after treatment. In terms of the energy setting, the treatment was started at 65 J/cm2 if the scars were strongly red. Each session consisted of 3 passes unless the patient felt strong pain at the second pass; in this case, the session was stopped. Even if the patient felt no pain after 3 passes, the session was stopped. Local anesthesia was not necessary in any of the cases. The intervals between the sessions were 3–4 weeks depending on the patient’s schedule.
CLINICAL EVALUATION
The responsiveness of the pathological scars to the treatment was assessed by determining the total Japan Scar Workshop Scar Scale 20114 evaluation score (Fig. 2). Therefore, the following 6 variables were measured by the first author in each session before starting laser treatment: induration, elevation, scar redness, erythema around the scars, spontaneous and pressing pain, and itch. The 4 variables were scored on the basis of a 4-point scale that ranged from 0 to 3 (0 = none, 1 = weak, 2 = mild, and 3 = strong); thus, the maximum possible total score of a patient’s scar was 18 points. The total scores before and after treatment (ie, before the first session and 1 month after the last session, respectively) were compared by using t test. The Mann-Whitney U test was used to compare the different affected body regions with each other in terms of the change in total score at 1 year (ie, the difference in the total scores before the first session and after the last session).
Fig. 2.
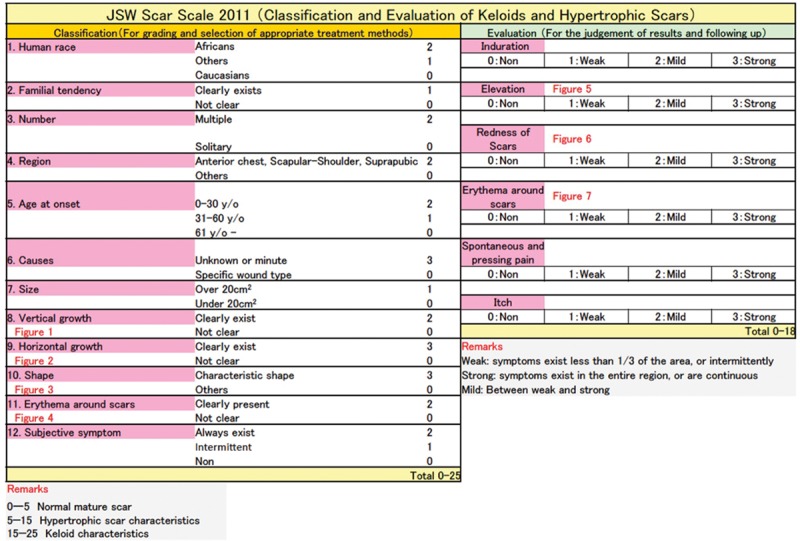
Japan Scar Workshop (JSW) Scar Scale 2011. Depiction of the evaluation part of the JSW Scar Scale 2011 that was used for clinical scar evaluation in the present study. The scars were evaluated before commencing laser treatment and 1 month after the last laser treatment session. Six variables, namely, induration, elevation, redness of scars, erythema around the scar, spontaneous and pressing pain, and itch, are evaluated. Reproduced with permission from Ogawa et al.5
Scar recurrence was assessed 6 months after stopping treatment; recurrence was defined as an increase in the total Japan Scar Workshop score by one or more points relative to the score at the end of the year-long treatment.
RESULTS
The average pretreatment scores are shown in Figure 3. The anterior chest keloids had the highest average score (10.3), whereas the lower-lip hypertrophic scars had the lowest average score (4.3). The main symptoms of the upper- and lower-lip hypertrophic scars were color and elevation. By contrast, the symptoms of the anterior chest keloids included not only objective symptoms but also subjective symptoms such as pain and itch. As a result, the keloids had higher total scores than the hypertrophic scars.
Fig. 3.
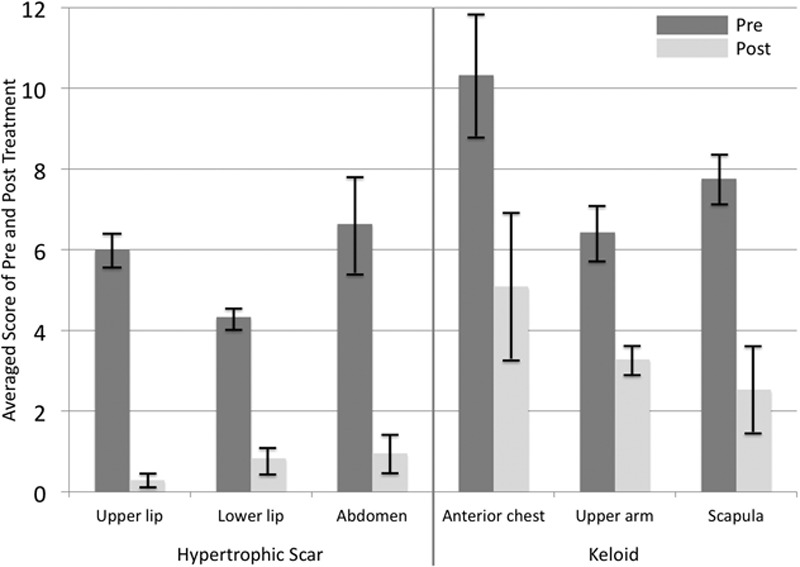
Average pre- and posttreatment scores of the hypertrophic scar and keloid region groups. The anterior chest keloid group had the highest average pretreatment score (10.3), whereas the lower-lip hypertrophic scar group had the lowest average pretreatment score (4.3).
The average scores after 1 year of laser treatment are also shown in Figure 3. The average posttreatment scores of all hypertrophic scar groups were below 2 points, which meant that most of the hypertrophic scars had turned into nearly mature scars.5 By contrast, the average posttreatment scores of all keloid groups were higher than 2 points. The anterior chest keloid group had the highest average total posttreatment score of all keloid groups (5.1). Nevertheless, in all groups, including all keloid groups, there were significant differences between the pre- and posttreatment scores (all P < 0.05). Three of the 34 anterior chest keloids (8.8%) did not respond to 1064 nm Nd:YAG laser therapy at all: the change in total score at 1 year relative to the pretreatment score in these keloids was 0. However, none of the hypertrophic scars or keloids deteriorated during the 1 year of treatment. The average number of sessions was adjusted according to the region: upper lip, 7.4 sessions; lower lip, 6.3 sessions; anterior chest wall, 11.8 sessions; scapula, 10.8 sessions; upper arm, 9.9 sessions, and abdomen, 10.8 sessions.
When the affected body regions were compared with each other in terms of the change in score (ie, the difference between the pre- and posttreatment scores), they did not differ significantly (P > 0.05) (Fig. 4).
Fig. 4.
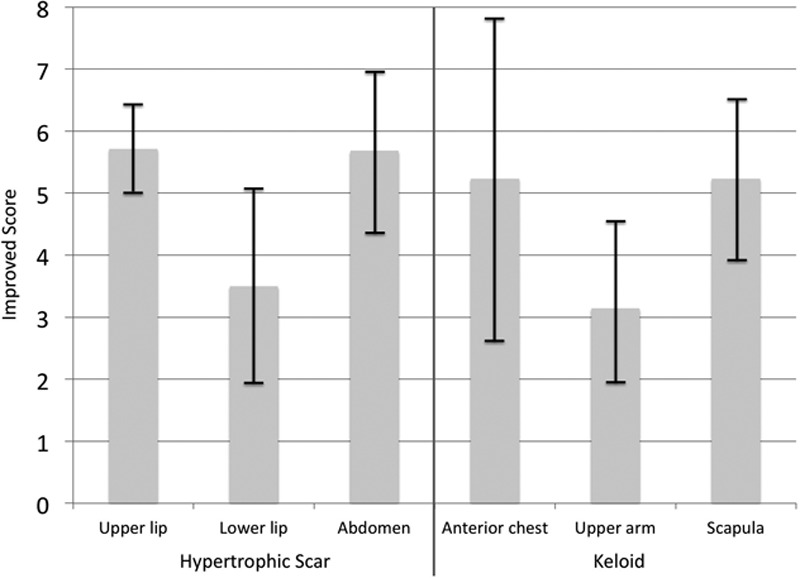
Differences between hypertrophic scar and keloid region groups in terms of change in score. The change in score is the difference between the score before commencing laser treatment and the score 1 month after the last laser treatment session. The different body regions did not differ significantly in terms of change in score (P > 0.05).
Recurrence was measured 6 months after stopping laser treatment, with the following cases observed (Fig. 5): 1 of the abdomen hypertrophic scars (4% of all abdomen hypertrophic scars), 18 of the anterior chest keloids (52.9%), 5 of the upper arm keloids (35.7%), and 4 of the scapula keloids (25%). These observations reflected our clinical observation that the hypertrophic scars and keloids that could not be turned into mature scars after 1 year of laser treatment were more likely to recur when the treatment was stopped.
Fig. 5.
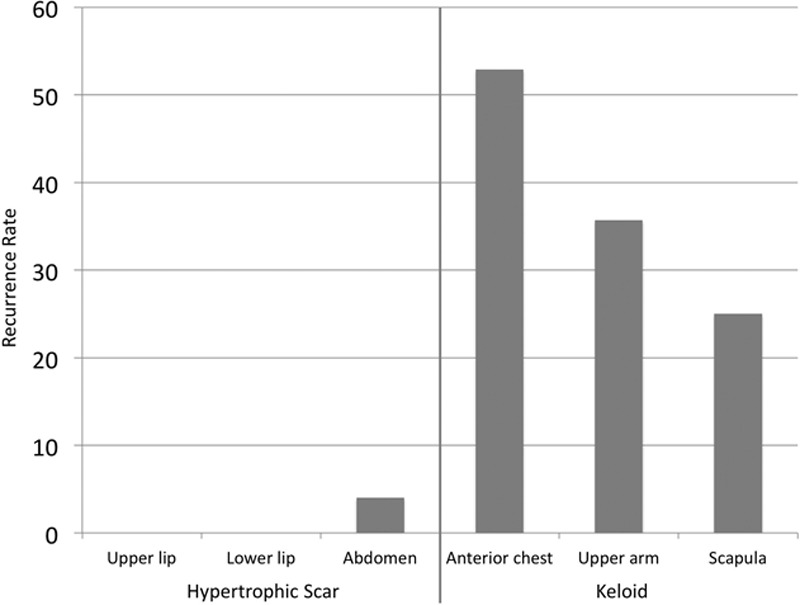
Recurrence rate of each body region. Six months after stopping the laser treatment, the scars were assessed by using the Japan Scar Workshop Scar Scale 2011. Recurrence was defined as an increase of one or more points relative to the score just after the treatment was stopped.
CASES
Case 1
A 20-year-old woman received an abrasion injury to the upper lip 2 years before referral to our clinic that turned into a hypertrophic scar (Fig. 6). Treatment with steroid ointment at another clinic did not yield any improvements. After undergoing 1 year of 1064 nm Nd:YAG laser treatment (5-mm spot, 65–70 J/cm2, 0.25 millisecond, 2 Hz), the scar continued to exhibit textural differences relative to the normal surrounding skin, but its redness and elevation improved. The total score improved from 7 to 0. The scar did not recur after the laser treatment was stopped.
Fig. 6.
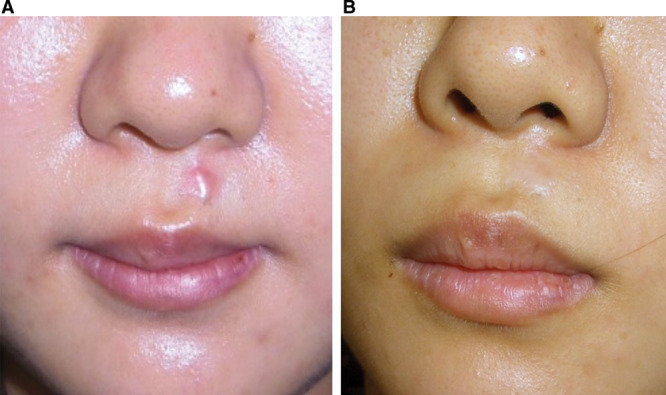
Case 1: Upper-lip hypertrophic scar. A, Pretreatment. B, 1 year after treatment. The 1064 nm Nd:YAG laser was used at 5-mm spot, 65–70 J/cm2, 0.25 millisecond, and 2 Hz. After 1 year of this treatment, the textural difference remained, but there was improvement in the redness and elevation of the scar. The total score improved from 7 to 0.
Case 2
An 11-year-old girl received an abrasion injury to the lower lip 1 year before referral to our clinic that developed into a hypertrophic scar (Fig. 7). Treatment with steroid ointment and tape at another clinic did not yield any improvements. After undergoing 1 year of 1064 nm Nd:YAG laser therapy (5-mm spot, 60–70 J/cm2, 0.25 millisecond, 2 Hz), the scar continued to exhibit textural differences relative to the normal surrounding skin and elevation, but its redness had clearly improved. The total score improved from 5 to 1. The scar did not recur after the laser treatment was stopped; however, scar revision may be considered in the future if the patient complains about having visible mature scars.
Fig. 7.

Case 2: Lower-lip hypertrophic scar. A, Pretreatment. B, 2 years after treatment. The 1064 nm Nd:YAG laser was used at 5-mm spot, 60–70 J/cm2, 0.25 millisecond, and 2 Hz. After 1 year of treatment, the textural differences and elevation remained, but there was clear improvement in the redness. The total score improved from 5 to 1.
Case 3
A 50-year-old woman developed hypertrophic scars on the abdomen after uterine myoma surgery 4 years before referral to our clinic (Fig. 8). The scar was not treated before the patient came to our clinic. After undergoing 1 year of 1064 nm Nd:YAG laser treatment (5-mm spot, 75 J/cm2, 0.25 millisecond, 2 Hz), the scar had almost disappeared. The total score improved from 7 to 0. The scar did not recur after the laser treatment was stopped.
Fig. 8.

Case 3: Abdomen hypertrophic scar. A, Pretreatment. B, 1 year after treatment. The 1064 nm Nd:YAG laser was used at 5-mm spot, 75 J/cm2, 0.25 millisecond, and 2 Hz. After 1 year of treatment, the scar had almost disappeared. The total score improved from 7 to 0.
Case 4
A 29-year-old woman developed butterfly-shaped keloids on the anterior chest 11 years before referral to our clinic (Fig. 9). Treatment with steroid ointment and tape at other clinics did not yield any improvements. Although surgery and radiation therapy were presented as a possible choice, the patient selected conservative therapy with the 1064 nm Nd:YAG laser. After undergoing 1 year of this treatment (5-mm spot, 65–75 J/cm2, 0.25 millisecond, 2 Hz), there were clear improvements in terms of the textural difference and elevation, but the redness on some parts remained. The total score improved from 15 to 3. However, after stopping the laser treatment, recurrence was observed: the redness and induration on several parts increased, and the score increased to 5 from 3. Therefore, 1064 nm Nd:YAG laser treatment was restarted, and the patient remains under observation. Scar revision may be considered in the future if the patient complains about visible mature scars.
Fig. 9.
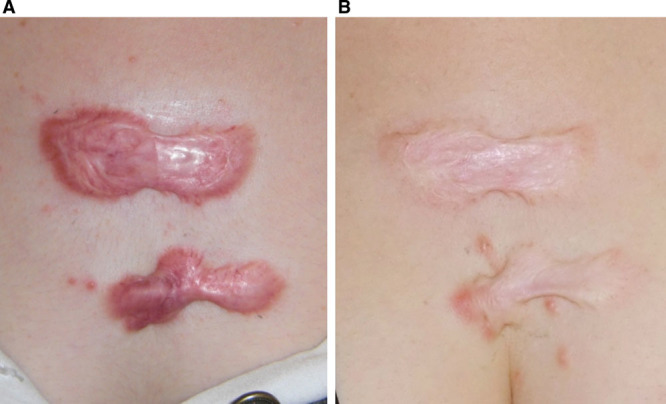
Case 4: Anterior chest wall keloid. A, Pretreatment. B, 1 year after treatment. The 1064 nm Nd:YAG laser was used at 5-mm spot, 65–75 J/cm2, 0.25 millisecond, and 2 Hz. After 1 year of treatment, there were clear improvements in the textural differences and elevation, but there was remaining redness on some parts. The total score improved from 15 to 3.
Case 5
A 52-year-old woman developed butterfly-shaped keloids on the upper arm and shoulder about 20 years before referral to our clinic. Steroid injections at other clinics yielded limited improvement. Moreover, capillary dilation, which is a complication of steroid injections, had developed around the keloid. Although surgery and radiation therapy were presented as a possible choice, the patient selected conservative therapy with 1064 nm Nd:YAG laser. After undergoing 1 year of this treatment (5-mm spot, 70–75 J/cm2, 0.25 millisecond, 2 Hz), there were clear improvements in terms of textural difference and elevation, but redness on some parts and the capillary dilation remained. The total score improved from 9 to 1. The scar did not recur after the treatment was stopped. Figure 10 shows the scar 30 months after stopping treatment. Thereafter, however, 1064 nm Nd:YAG laser treatment using the following settings was restarted to target the dilated capillary vessels: 3-mm spot, 150 J/cm2, 0.25 millisecond, 2 Hz. At the time of writing, we are still treating this patient. However, the capillary dilation is slowly improving.
Fig. 10.

Case 5: Shoulder keloid. A, Pretreatment. B, 30 months after treatment. The 1064 nm Nd:YAG laser was used at 5-mm spot, 70–75 J/cm2, 0.25 millisecond, and 2 Hz. After 1 year of treatment, there were clear improvements in the textural differences and elevation, but redness on some parts and the capillary dilation remained that were the result of past steroid injections. The total score improved from 9 to 1.
Case 6
A 52-year-old woman developed butterfly-shaped keloids on the scapula about 30 years before referral to our clinic. Steroid injections and tape at other clinics yielded little improvement. Although surgery and radiation therapy were presented as a possible choice, the patient selected conservative therapy using 1064 nm Nd:YAG laser. After undergoing 1 year of this treatment (5-mm spot, 70–75 J/cm2, 0.25 millisecond, 2 Hz), there were clear improvements in scar texture, redness, induration, and elevation. The total score improved from 10 to 1. The scar did not recur after the treatment was stopped. Figure 11 shows the scar 3 years after the treatment stopped.
Fig. 11.

Case 6: Scapular keloid. A, Pretreatment. B, 3 years after treatment. The 1064 nm Nd:YAG laser was used at 5-mm spot, 70–75 J/cm2, 0.25 millisecond, and 2 Hz. After 1 year of treatment, there were clear improvements in the scar texture, redness, induration, and elevation. The total score improved from 10 to 1.
DISCUSSION
History and Mechanisms of Laser Treatment for Keloids and Hypertrophic Scars
The ablation of keloids and hypertrophic scars with carbon dioxide laser (CO2 laser 1060 nm) has been widely studied. The CO2 laser can cut and cauterize, creating a dry surgical environment with minimal tissue trauma.5–7 However, the pathological scar recurrence rates associated with this method are substantial. Thereafter, CO2 laser combination therapies with modalities such as steroid treatment, hyaluronidase injections, and cryosurgery were tried. In the 1980s, 585-nm PDL started being used to treat scars by using the effect of coagulation. PDL has a high absorption coefficient for hemoglobin and thus is used to reduce the redness and thickness of cutaneous scars.8,9 Paquet et al10 suggested that PDL improves keloids or hypertrophic scars by inducing capillary destruction, which generates hypoxemia and, in turn, alters the local collagen production. Dierickx et al11 also attributed the therapeutic effect of PDLs to hypoxemia resulting from laser-induced heat and vascular injury. Kuo et al12 found that PDL therapy of keloids stimulated their production of matrix metalloproteinase, including collagenase; however, a single PDL irradiation procedure is not sufficient to completely improve the scar surface conditions. To obtain better clinical outcomes, PDL should be combined with corticosteroid injections and/or 5-fluorouracil treatment.13,14 In 1988, Sherman et al15 reported an in vitro study that showed that Nd:YAG laser decreases collagen production. They also reported clinical results that showed this treatment decreases redness and induration. The limited penetration depth of the yellow light emitted by PDL may also cause resistance to further PDL treatment because of the optical absorption and scattering in the epidermis and dermis at a depth of about 1–2 mm15,16; thus, deeper vessels may be selectively treated with the 1064 nm Nd:YAG laser.9,17 Indeed, due to its deeper penetration and lower absorption by hemoglobin, the 1064 nm Nd:YAG laser has proved to be a much more useful light source for the treatment of deep or thick vascular lesions than the traditionally used shorter wavelength sources.
Indications and Limitations of Nd:YAG Laser for Keloids and Hypertrophic Scars
Both keloids and hypertrophic scars are characterized by chronic inflammation and excessive capillary vessels, which cause red scars.18 A burn wound that heals in less than 10 days has a 4% risk of developing hypertrophic scars,19 whereas a burn wound that takes 21 days or more to heal has a 70% or greater risk of developing hypertrophic scars; thus, it has been suggested that nearly anyone can develop hypertrophic scars and that scars are largely the result of local wound conditions. Keloids, however, are clearly more driven by genetic influences than hypertrophic scars.20 Nevertheless, these 2 fibroproliferative skin disorders bear many similarities.18
Although keloid susceptibility is shaped by genetics,20 it is also known that keloids tend to occur on sites that are highly mobile and on skin that is under high tension. Classical keloid sites are the anterior chest, suprapubic region, and upper arm.21 Our studies on the relationship between skin tension and keloids have suggested that the characteristic butterfly, crab’s claw, and dumbbell shapes associated with keloids are largely determined by the direction of mechanical forces at and around the wound site on skin21,22; thus, it seems that mechanical force is a major factor that drives keloid development and progression.
Pathological scar development may also be shaped by interactions between mechanical force loading and inflammation, collagen production, and angiogenesis. This means that 1064 nm Nd:YAG laser treatment may be useful for treating pathological scars because it could reduce the vascularity of these scars.2,23 This reduction in vascularity may decrease cytokine or growth factor levels in the tissue, which, in turn, promotes collagen deposition. Future studies on these putative mechanisms are warranted. However, because the pathological scar risk factors can interact also means that if the scars continue to be subjected to strong mechanical forces such as tension, 1064 nm Nd:YAG laser may not be successful. In the present study, the hypertrophic scars responded significantly better to the laser treatment than the keloids; however, the data also suggested that if scars can be turned into completely mature scars, recurrence will not be observed. Nevertheless, if even a little keloid redness and induration remains, these scars are highly likely to recur.
Future Perspectives of Laser Treatment for Keloids and Hypertrophic Scars
Histology of a port-wine stain that had been treated with contact-mode 1064 nm Nd:YAG laser at 130 J/cm2, 6 ms, and 5-mm spot revealed that the deepest vessel damage was 2 mm from the dermoepidermal junction.24 Taken together with our own observations,2 this suggests that although a noncontact mode 1064 nm Nd:YAG laser results in much deeper thermal effects and vascular damage than those generated by PDL,2 these effects may be less deep than those produced by the 1064 nm Nd:YAG laser in contact mode. In the present study, 1064 nm Nd:YAG laser in contact mode was used to treat scars in a protocol that aimed to avoid inducing pain. The results suggest that the contact mode may have better clinical outcomes for keloids and hypertrophic scars than the noncontact mode. Future studies that test the effect of combining noncontact mode with contact mode (or PDL with 1064 nm Nd:YAG) in precisely diagnosed keloids and hypertrophic scars by measuring the subjective and objective symptoms are warranted. It may also be useful to combine 1064 nm Nd:YAG with steroid injections to reduce the volume of collagen. The efficacy of such combination therapy also warrants further study.
Conclusions
Hypertrophic scars responded significantly better to 1064 nm Nd:YAG laser treatment than keloids. However, keloid recurrence occurred when there was remaining redness and induration, even if only a small part of the scar was affected.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Dover JS, Arndt KA. New approaches to the treatment of vascular lesions. Lasers Surg Med. 2000;26:158–163. doi: 10.1002/(sici)1096-9101(2000)26:2<158::aid-lsm6>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 2.Akaishi S, Koike S, Dohi T, et al. Nd:YAG laser treatment of keloids and hypertrophic scars. Eplasty. 2012;12:e1. [PMC free article] [PubMed] [Google Scholar]
- 3.Civas E, Koc E, Aksoy B, et al. Clinical experience in the treatment of different vascular lesions using a neodymium-doped yttrium aluminum garnet laser. Dermatol Surg. 2009;35:1933–1941. doi: 10.1111/j.1524-4725.2009.01355.x. [DOI] [PubMed] [Google Scholar]
- 4.Ogawa R, Akaishi S, Akita S, et al. JSW Scar Scale Working Group. Japan Scar Workshop (JSW) Scar Scale 2011 [Japanese]. 2012; Scar Management. 6:19–22. [Google Scholar]
- 5.Ogawa R, Akaishi S, Akita S, et al. JSW Scar Scale Working Group. Japan Scar Workshop (JSW) Scar Scale. Available at: http://www.scar-keloid.com/en/index.html. Accessed October, 2010.
- 6.Norris JCE. The effect of carbon dioxide laser surgery on the recurrence of keloids. Plast Reconstr Surg. 1991;87:44–49. [PubMed] [Google Scholar]
- 7.Norris JCE. The effect of carbon dioxide laser surgery on the recurrence of keloids. [Discussion] Plast Reconstr Surg. 1991;87:50–53. [PubMed] [Google Scholar]
- 8.Stucker FJ, Shaw GY. An approach to management of keloids. Arch Otolaryngol Head Neck Surg. 1992;118:63–67. doi: 10.1001/archotol.1992.01880010067018. [DOI] [PubMed] [Google Scholar]
- 9.Alster TS, Williams CM. Treatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet. 1995;345:1198–1200. doi: 10.1016/s0140-6736(95)91989-9. [DOI] [PubMed] [Google Scholar]
- 10.Paquet P, Hermanns JF, Piérard GE. Effect of the 585 nm flashlamp-pumped pulsed dye laser for the treatment of keloids. Dermatol Surg. 2001;27:171–174. doi: 10.1046/j.1524-4725.2001.00169.x. [DOI] [PubMed] [Google Scholar]
- 11.Dierickx C, Goldman MP, Fitzpatrick RE. Laser treatment of erythematous/hypertrophic and pigmented scars in 26 patients. Plast Reconstr Surg. 1995;95:84–90; discussion 91–92. [PubMed] [Google Scholar]
- 12.Kuo YR, Wu WS, Jeng SF, et al. Suppressed TGF-beta1 expression is correlated with up-regulation of matrix metalloproteinase-13 in keloid regression after flashlamp pulsed-dye laser treatment. Lasers Surg Med. 2005;36:38–42. doi: 10.1002/lsm.20104. [DOI] [PubMed] [Google Scholar]
- 13.Connell PG, Harland CC. Treatment of keloid scars with pulsed dye laser and intralesional steroid. J Cutan Laser Ther. 2000;2:147–150. doi: 10.1080/14628830050516407. [DOI] [PubMed] [Google Scholar]
- 14.Asilian A, Darougheh A, Shariati F. New combination of triamcinolone, 5-Fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32:907–915. doi: 10.1111/j.1524-4725.2006.32195.x. [DOI] [PubMed] [Google Scholar]
- 15.Sherman R, Rosenfeld H. Experience with the Nd:YAG laser in the treatment of keloid scars. Ann Plast Surg. 1998;24:231–233. doi: 10.1097/00000637-198809000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Connell PG, Harland CC. Treatment of keloid scars with pulsed dye laser and intralesional steroid. J Cutan Laser Ther. 2000;2:147–150. doi: 10.1080/14628830050516407. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence WT. In search of the optimal treatment of keloids: report of a series and a review of the literature. Ann Plast Surg. 1991;27:164–178. doi: 10.1097/00000637-199108000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Ogawa R, Akaishi S, Izumi M. Histologic analysis of keloids and hypertrophic scars. Ann Plast Surg. 2009;62:104–105. doi: 10.1097/SAP.0b013e3181855172. [DOI] [PubMed] [Google Scholar]
- 19.Deitch EA, Wheelahan TM, Rose MP, et al. Hypertrophic burn scars: analysis of variables. J Trauma. 1983;23:895–898. [PubMed] [Google Scholar]
- 20.Nakashima M, Chung S, Takahashi A, et al. A genome-wide association study identifies four susceptibility loci for keloid in the Japanese population. Nat Genet. 2010;42:768–771. doi: 10.1038/ng.645. [DOI] [PubMed] [Google Scholar]
- 21.Ogawa R, Okai K, Tokumura F, et al. The relationship between skin stretching/contraction and pathologic scarring: the important role of mechanical forces in keloid generation. Wound Repair Regen. 2012;20:149–157. doi: 10.1111/j.1524-475X.2012.00766.x. [DOI] [PubMed] [Google Scholar]
- 22.Akaishi S, Akimoto M, Ogawa R, et al. The relationship between keloid growth pattern and stretching tension: visual analysis using the finite element method. Ann Plast Surg. 2008;60:445–451. doi: 10.1097/SAP.0b013e3181238dd7. [DOI] [PubMed] [Google Scholar]
- 23.Rossi A, Lu R, Frey MK, et al. The use of the 300 microsecond 1064 nm Nd:YAG laser in the treatment of keloids. J Drugs Dermatol. 2013;12:1256–1262. [PubMed] [Google Scholar]
- 24.Landthaler M, Haina D, Brunner R, et al. Neodymium-YAG laser therapy for vascular lesions. J Am Acad Dermatol. 1986;14:107–117. doi: 10.1016/s0190-9622(86)70014-5. [DOI] [PubMed] [Google Scholar]


