Abstract
Tuberculosis (TB) of the hip is second to spine only hence a good number of cases are visiting the medical facilities every year. Many present in the advanced stage of the disease due to delayed diagnosis. In early stages of TB of hip, there is a diagnostic dilemma when plain X-rays are negative. In the present time, diagnostic modalities have improved from the days when diagnosis was based essentially on clinicoradiological presentation alone. By the time definite radiological changes appear on plain X-ray, the disease has moderately advanced. The modern diagnostic facilities like ultrasonography (USG) or magnetic resonance imaging of the hip joint, USG guided aspiration of synovial fluid and obtaining the material for polymerase chain reaction and tissue diagnosis must be utilized. In the treatment, current emphasis is more on mobility with stability at hip. Joint debridement, skeletal traction, and mobilization exercises may give more satisfying results as compared to the immobilization by hip spica. Adults with advanced arthritis and healed infection should be informed and discussed the various treatment modalities including the joint replacement. More and more surgeons are taking up the challenge of putting the total hip replacement in the active stage of the disease. Until the long term results in active disease are well established, we recommend it for the healed disease only in selected cases.
Keywords: Tubercular arthritis, hip, children, total hip replacement
MeSH terms: Tubercular osteoarticular, hip, hip prosthesis, arthroplasty
INTRODUCTION
Tuberculosis (TB) of the musculoskeletal system, though accounts for only 1-3% of total TB cases,1 however, as one fourth of all TB cases are in India,2 the absolute number of cases with musculoskeletal TB become large. TB of hip constitutes 15-20% of the musculoskeletal system.1 The majority of cases of hip TB are presenting as painful, restricted movements of the hip and there comes, the dilemma of accurate diagnosis as several pathologies may mimic this presentation. For example in children, Perthes disease, juvenile rheumatoid arthritis, transient synovitis, bleeding disorders, pyogenic arthritis etc., has to be differentiated. Similarly in adult's avascular necrosis (AVN), degenerative and inflammatory conditions may pose a problem in the diagnosis. Though the diagnosis of TB hip conventionally is still largely based on clinicoradiological findings, however, it is desirable to make a early diagnosis for good results. How helpful are the modern diagnostic imaging modalities like ultrasonography (USG), magnetic resonance imaging (MRI), bone scan or immunological and molecular diagnostic tests like polymerase chain reaction (PCR) to diagnose TB hip at an early stage? Is it mandatory to subject every patient for tissue diagnosis particularly in the endemic zones for TB, before we start the antitubercular treatment? Even after the diagnosis is made in early stages, what should be our treatment protocol? When presenting late, there are permanent changes in the joint with varying disability and there is a dilemma of dealing with this morbid anatomical and pathological changes in the joint. Literature has described various treatment options both nonoperative3 and operative.4,5,6,7 The surgical options vary from excision arthroplasty to hip replacement. Total hip replacement (THR) in the active stage of the disease is yet another area of controversy. We have discussed some of these issues on the basis of available knowledge on the subject. We suggest that treatment options offered to the patients should depend on the stage of involvement and must be discussed thoroughly with the patient, despite the stage of involvement before decision is taken.
MATERIALS AND METHODS
A PubMed search was done with the key word “TB of hip joint, tubercular arthritis of the hip, THR in tubercular arthritis of the hip, TB hip in children and epidemiology of TB.” We could trace about 250 papers on the subject. In addition, our good source of information was a book from co-author Tuli1 We also looked into in details the various articles published in the symposium on “musculoskeletal TB”.8,9,10,11 The data from all these sources were pooled and the relevant information for this review was included.
Pathogenesis and pathology
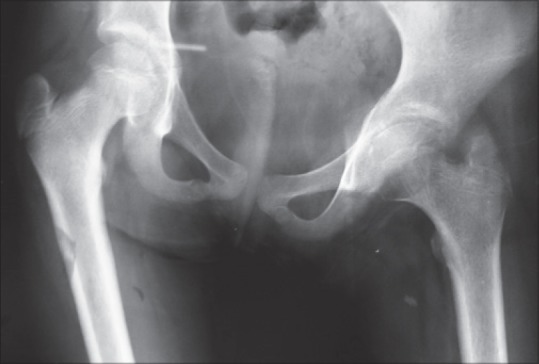
Osteoarticular TB is secondary to primary pathology in lungs, lymph nodes or any of the viscera. Through the hematogenous route, the bacteria reach either to synovium or bone. When it lodges first in synovium, the synovial membrane becomes swollen and congested. The granulation tissue from the synovium extends over the bone resulting in necrosis of sub chondral bone, sequetra and may be kissing lesion on either side of joint.8 The bacteria may also lodge first in the epiphyseal or metaphyseal region of the adjoining bones like head or neck of femur, greater trochanter or acetabulum to start the destructive process [Figure 1]. It may start as extra articular or juxta articular lesion. When the disease starts as intraarticular, it progresses fast to involve the whole joint. An extra articular lesion can also progress further to involve the joint. Cold abscess that usually forms within the joint may perforate the capsule to present around the hip joint in the femoral triangle, medial, lateral or posterior aspects of thigh, ischio rectal fossa.1
Figure 1.

Diagrammatic representation of the location of osseous origin of tuberculosis of left hip joint; (1) acetabulum (2) femoral head/epiphysis (3) femoral neck/metaphysic (4) greater trochanter (reprinted with permission from Tuli[1])
Clinical presentations
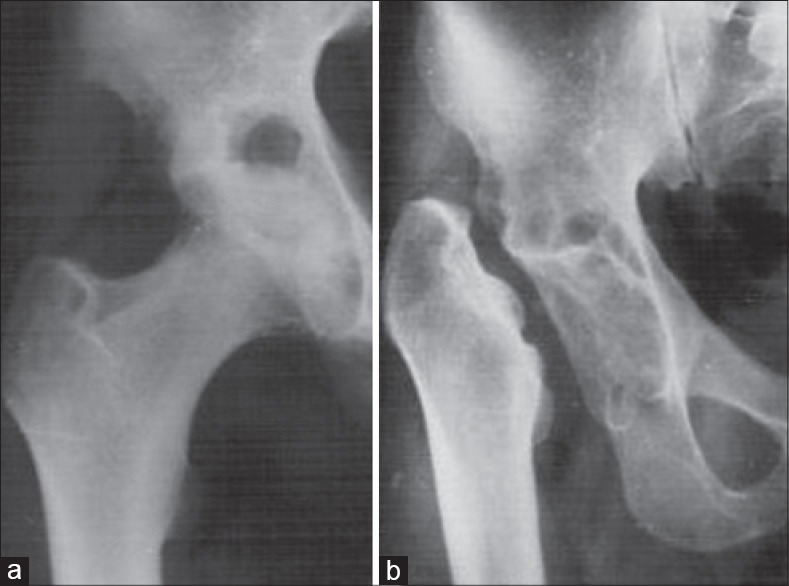
Disease usually starts during first three decades but no age is immune. Pain in the hip, limp, restriction of movements is present in almost all the cases. Depending upon the extent of involvement there can be deformity, shortening of the limb, swelling, pathological dislocations, and sinuses. In the stage of synovitis, there is effusion in the joint and the affected limb is flexed, abducted, and externally rotated with an apparent lengthening of the extremity. There is a restriction essentially of terminal range of movements. In the stage of early arthritis, with progressive destruction of the joint, the limb goes into flexion, adduction, and internal rotation, with an apparent limb shortening. In the active stage, there is muscle spasm, every attempted movement of the hip can be painful, and child walks with an antalgic gait. The joint space is still maintained in this stage. In the stage of advanced arthritis the destruction leads to irregular and hazy joint margins with diminished joint space [Figure 2]. The hip movements are painful and grossly restricted with shortening of the limb. Pathological dislocation/subluxation occurs in the stage of advanced arthritis as a result of gross destruction of the femoral head or the superior acetabular margin (wandering acetabulum), it adds to further shortening and deformity. The attitude of the limb and deformity does not always correspond with the stage of arthritis. The hip is subluxated posteriorly and superiorly with true shortening of the involved limb.12 Sometimes head of the femur, instead of displacing posteriorly may protrude medially through weakly destroyed acetabulum. Babhulkar and Pande9 introduced a classification, based on above clinicoradiological presentations into stage of synovitis, early arthritis, stage of arthritis and stage of advanced arthritis. The presence of apparent shortening or true shortening separated early arthritis and arthritis [Table 1]. Tuli1 suggested modification in this classification [Table 2]. He classified it as synovitis, early arthritis, advanced arthritis and advanced arthritis with subluxation/dislocation.
Figure 2.
Plain X-ray showing “stage of arthritis;” pathology involving articular surface. Irregular and hazy joint margins with diminished joint space on left side
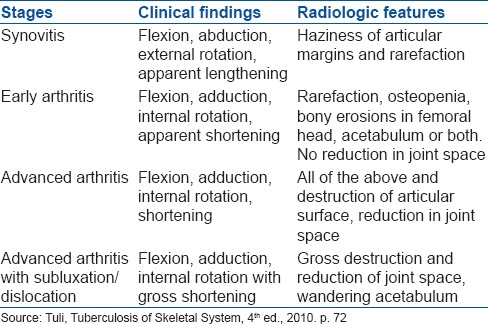
Table 1.
Clinicoradiological classification of tuberculosis of the hip

Table 2.
Clinicoradiological classification of tuberculosis of the hip
Investigations
It is suggested that in the endemic regions for TB, a clinical diagnosis supported by radiographs is adequate for starting the treatment.8,13,14 The patient presenting with clinical features of pain, limp, painful restriction of joint movements and deformity at hip supported by radiological features of para articular osteoporosis, soft tissue swelling, diminishion of joint space and irregular and fuzzy joint margins is suggestive of tubercular disease of hip joint. In the stage of synovitis, there may not be changes in the joint and many a time's diagnosis is missed; hence confirmation of diagnosis by demonstration of tubercular bacilli or histological features in biopsy is recommended. In advance stages of arthritis, radiological changes are typical and tissue diagnosis may not be required. Some other hip conditions presenting with pain and limp are transient synovitis of the hip, Legg–Calve–Perthes disease, osteomyelitis of the upper end of the femur, injury hip, acute infective arthritis of infancy and childhood, osteoid osteoma of the neck of the femur with synovial involvement, villonodular synovitis, rheumatoid arthritis, AVN of the head of the femur, giant cell variants of upper femur, etc., Tissue biopsy can help in reaching a conclusive diagnosis. In the stage of synovitis in TB of hip, plain X-rays do not show any findings or at the most only soft tissue swelling is visible. With further progression of the disease, periarticular osteoporosis, hazy, and irregular joint margins with reduction in the joint space is seen. In advanced arthritis, the picture is of travelling/wandering acetabulum [Figure 3], dislocated hip, Perthes type [Figure 4], protusio acetabuli, atrophic type, mortar, and pestle as described in Shanmugasundaram's classification are observed.15 He proposed this classification in 1983 on plain x-rays. Campbell and Hoffman16 suggested that there is a relationship between various radiological types and the functional outcome. In the present time MRI has helped us to detect the early morbid pathology in the joint as it shows the predestructive lesion like edema and inflammation. It is a sensitive test to detect soft tissue abnormalities in and around the joint. MRI is not specific for TB of hip.17 MRI in early stages may show synovial effusion and varying degree of bone edema, minimal areas of bone destruction. The tissue diagnosis may be indicated in such instances.18 Most of the literature on the subject agrees that the diagnosis in endemic regions can be made on the basis of clinical features supported by plain X-ray findings alone, however, in the countries where disease is rare, additional investigations in the form of ultrasound or MRI of the hip, and/or biopsy may be necessary. The tissue obtained from the diseased site must be subjected to histology, AFB staining PCR and also for culture and sensitivity. Singhal et al.17,18,19 opined that arthroscopic synovial biopsy gives definitive diagnosis of various joint ailments. It is an important useful investigative adjunct to correlate and confirm the diagnosis after clinical and synovial fluid evaluation. Synovial biopsy may give conclusive diagnosis where clinical diagnosis is equivocal.
Figure 3.

X-ray left hip joint anteroposterior view showing the “wandering acetabulum”
Figure 4.

X-ray pelvis with both hip joints showing the “Perthes type” of appearance on left side
Management
Early diagnosis and effective chemotherapy are vital to save the joint.20 In view of the nonspecific findings early in the course of the disease, failure to consider TB can lead to devastating outcomes.21 We recommend the standard chemotherapy as accepted universally with four anti tubercular drugs to start with in all the stages of presentation. In addition to medical treatment, traction preferably skeletal is recommended to all patients. In the case of the abduction deformity, traction on the other limb is also applied to stabilize the pelvis. Traction relieves the muscle spasm, prevents or corrects deformity and subluxation, maintains the joint space, minimizes the chances of development of migration of acetabulum and permits close observation of the hip region. Another advantage with traction is that it keeps the joint surfaces apart; hence with an early start of mobilization exercises of the hip, functional range of movements can be achieved. With late presentation, the deformities may become permanent. The TB heals with fibrosis, hence may not respond to traction. Unlike pyogenic infections, proteolytic enzymes are not produced in tubercular infection; articular cartilage survives for a long time thus preserving mobility in many patients. Tuli8 earlier was recommending partial weight-bearing only after 4-6 months of treatment, and full weight-bearing only at 18 months. However, in the present day scenario, we recommend weight-bearing earlier, whenever patient can tolerate the pain. Moon et al. Recommends early rehabilitation regimen for ambulation as it boosted the patients’ confidence and activity level.22 In addition to ATT, nutritional supplementation and traction, the specific treatment depends upon the stage of involvement at the time of diagnosis.
Synovitis stage
To establish the diagnosis the patient should be subjected to USG examination; synovial effusion can be aspirated and subjected for cytology, AFB smear and PCR examination. If necessary, biopsy can be taken from diseased tissue to establish the diagnosis. The prognosis after chemotherapy, traction, rest and mobilization exercises is very good in this stage and the surgical interventions usually are not required.
Early arthritis
As clinical features of pain, spasm, limp, painful movements are more pronounced, supported by radiological features of para articular osteoporosis, localized erosions in the head/acetabulum, a high suspicion index of early arthritis is kept. MRI may show synovial effusion, osseous edema and areas of bone destruction. In addition to traction and chemotherapy, analgesics supplementation is necessary till spasm of the muscles is relieved. Nonweight bearing range of motion exercises are started whenever patient is able to co-operate. A vigorous passive exercise may produce further pain and spasm and should be avoided. Failure to respond in the form of improvement in constitutional features, reduction of pain around hip, increase in the range of movements to nonoperative treatment may call for confirmation of diagnosis. Synovectomy and joint debridement are done with an aim to reduce the disease tissue load and ascertain diagnosis. Vora23 cautioned that during synovectomy, utmost attention should be given to safeguard the feeding vessels to the head, located beneath the hypertrophied synovium. He also suggested that femoral head should not be dislocated to facilitate the synovectomy procedure. Moon et al.22 however, observed that the response to chemotherapy in the hips appearing normal on X-rays is same in different therapeutic groups (nonsynovectomy and synovectomy). The prognosis in general is good. Deformities are correctable, shortening is minimal and range of movements can be more than functional depending upon how seriously exercises regimen is followed.
Advanced arthritis
The clinicoradiological presentation is typical of tubercular arthritis in this stage. Irregular and hazy joint margins, destruction of bone on either side of joint, erosions and reduced joint space are classical plain X-ray findings. There is gross destruction of capsule, synovium, bones and articular cartilage. Shortening of limb and deformity further complicates the condition. In addition to the treatment as advocated above, arthrolysis of joint with joint debridement can be very helpful. The end result after the procedure is usually a healed disease with shortening of limb and moderate to gross restriction of movements. Arthrolysis aims to achieve the useful range of movements in the cases with gross limitation of movements not responding to traction and exercises.8,9 The arthrolysis helps in the cases where limitation of movement is because of fibrous ankylosis and not to mechanical restriction as a result of mainly alteration in the anatomy of the joint. For example, it may not help in wandering acetabulum type or pathological dislocation or even in pestle and mortal appearance. All pathological and fibrous tissues are excised carefully without compromising with vascularity of remaining part of the upper end of the femur. It is wise to leave the posterior capsule undisturbed because it carries vital blood supply to the femoral head. Posterior capsule is generally not shortened as most of the patients have flexion deformity. Before the completion of the operative procedure, ensure that adequate range has been achieved by passive movements (while under anesthesia). After surgery, skeletal traction is applied, and movements of the hip are allowed under supervision as soon as patient is able to do.
Advanced arthritis with subluxation/dislocation
As expected, gross destructive changes in the joint will not allow for even functional range of movements. Gross deformities and shortening are another problems to tackle. The different lines of management of this complex problem could be as follows.
Conservative traction regimen
Sandhu et al.3 reported healing of disease in 98% of cases by advocating ATT and traction. Of his 41 patients of the advance arthritis, 40 had appreciable range of movements. Patients presenting with sound ankylosis, short fibrous or bony in a bad position required upper femoral corrective osteotomy. This operation is a simple extra capsular procedure and can be done at any age. The ideal site for corrective osteotomy is as near the deformed joint as possible.1
Excision arthroplasty
In the Indian subcontinent and in many Asian countries, people do not accept a stiff hip joint as squatting, sitting cross-legged, and kneeling are essential socioeconomic actives in their day to day life. Girdlestone's excision arthroplasty can be safely carried out in healed or active disease after the completion of growth potential of bones of the hip joint [Figure 5a and b]. This procedure provides a mobile, painless hip joint with control of infection and correction of deformity. However, some degree of shortening and instability is unavoidable. Application of postoperative traction for 3 months minimizes shortening and gross instability.4 With the employment of effective antitubercular drugs the chances of recrudescence reduces significantly in such patients than in those who obtained sound ankylosis. About 90% of patients are able to squat and kneel and able to sit cross-legged. With the help of the stick, all are able to stand on the operated extremity and able to climb up the stairs. We would safely recommend excision arthroplasty for active or healed tuberculous arthritis in adults without any apprehension of increased incidence of reactivation of the infection. The shortcomings of excision arthroplasty like shortening of the limb and instability of hip joint can be minimized to some extent by prolonged skeletal traction upto 3 months with on traction exercises in bed. The patient should bear weight with support by holding stick in opposite hand. For further improvement in instability, one can do Tactoplasty as advocated by Saito et al.24 The pelvic support osteotomy as advocated by Milch25 can be another procedure to reduce the instability. If warranted, limb lengthening can be done to take care of limb shortening.
Figure 5.
X-ray of right hip joint anteroposterior view showing (a) active tubercular arthritis of right hip. (b) After Girdlestone excision arthroplasty
Arthrodesis
Arthrodesis of the hip, though relieves the pain, and corrects the deformity. However it is at the cost of loss of movements. Its acceptance in Indian subcontinent is very low due to socio cultural reasons. Young adult with sound bony ankylosis in functioning position has to learn to adopt himself for the active life. One has however to resort to chair and commode toilet system for whole life.
Hip replacement
In tubercular arthritis, as acetabulum is involved, there is no role of hemi replacement. Total hip arthroplasty (THA) in the hip with active tuberculous infection is a controversial issue due to the potential risk of reactivation of TB.26 The acceptability of the THA is gradually increasing globally [Figure 6a and b] with reports that metal can be safely used in tuberculous lesions.5,10 THA in a patient with healed TB of the hip is now an accepted procedure27,28,29 Majority perform it in the stage of the advance arthritis or in sequalae of advance arthritis when the joint is unsalvageable. Babhulkar and Pande9 recommended it to be performed after 10 years or more between active infection and replacement surgery. Its role in active TB is debatable. Wang et al.5 recommend a combination of antituberculous drugs for at least 2 weeks prior to the operation and subsequently for at least 12 months after operation. Neogi et al.30 recommends routine preoperative computed tomography-guided biopsy, with specimens subjected to culture and sensitivity testing, in view of the emergence of drug resistant Tubercular bacilli.
Figure 6.
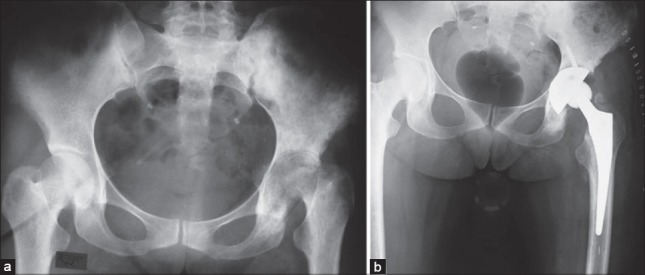
X-ray pelvis with both hip joints anteroposterior view showing (a) tubercular arthritis of left hip. (b) After uncemented total hip arthroplasty (with permission from A K Rai, BHU)
Sidhu et al.6 performed cemented THR in 23 patients with active tuberculous arthritis of the hip. His patients had received at least 3 months of antitubercular therapy before surgery and treatment were continued for a total of 18 months. With a mean followup of 4.7 years, no activation of the infection or implant-loosening was recorded. They concluded that hip replacement in the presence of active tuberculous arthritis of the hip may be a safe procedure when peri operative chemotherapy was used. Kim et al.27 had reported good results with THR. The interval between active disease and THA in his cases ranged from 3 months to 45 years. The mean Harris hip score at averaged 4 years was 85. Wang et al.5 opined that in advanced active TB of the hip, THR is a safe procedure providing symptomatic relief and functional improvement. Thorough debridement of infected tissues and postoperative antituberculous chemotherapy are the keys to lowering the potential risk of reactivation of TB. Neogi et al.30 reported similar opinion and results. The adequate surgical debridement and ATT was the key for a successful outcome.27,31 Kim et al.26 evaluated the outcome of THR in patients with active TB of the hip in referenced articles published between 1950 and 2012. A total of 65 patients of histologically confirmed TB were reviewed with a mean followup was 53.2 months (24-108). Antitubercular treatment continued postoperatively between 6 and 15 months. Their analysis concluded that THR in patients with active TB of the hip is a safe procedure. If undertaken in association with extensive debridement and appropriate anti-TB treatment, it provides symptomatic relief and functional improvement It is reasonable to believe that THA placed in an active disease with structurally weak bone would fail biomechanically more often, however, the follow of THR in such cases hardly show recurrence of disease or loosening of implant. Oztürkmen et al32 did not observed any reactivation of disease in his 9 cases. At an followup of average 5.6 years, all the femoral stems and acetabular cups were radiologically stable and demonstrated signs of bone ingrowth. Similarly in Wang et al.5 series, after mean followup of 49 months, there was no case of hip dislocation, loosening of implant or recrudescence. Similar observations were made by Yoon et al.,31 Neogi et al.30 or in Kim's multidata analysis26 of 65 cases in mean followup ranging between 41 to 56 months.
However, Kim et al.33 warned on the difficulty with exposure related to contracted scar tissue and the difficulty with wound healing. Kim et al. observed no difference in the reactivation or healing with cemented or cementless implants.27 Till long term followup results are established, we may not agree with the statement of Wang et al.5 that THA in advanced active TB of the hip is a safe procedure providing symptomatic relief and functional improvement. Yoon et al.27,31 reported advanced active tuberculous arthritis of the hip patients treated with cementless THA. Postoperatively antituberculous medications were continued for 1-year. With average followup of 4.8 years, reactivation of the infection was not detected. They concluded that THA in the tuberculous hip is a safe procedure and produces superior functional results compared with resection arthroplasty or arthrodesis.
Thorough debridement of infected tissues and postoperative antituberculous therapy are the keys to lowering the potential risk of reactivation of TB.5 Babhulkar and Pande9 insisted that the joint replacement in patients with the active stage of the disease is contraindicated because of a probable high reactivation rate. The senior author (SMT) has observed a few patients with persistent sinuses and continued activity of infection after THA. The implants were removed in four patients. The disease healed and the excision arthroplasty like clinical presentation was accepted by the patient and family. In healed TB with subluxation/dislocation of long duration, where replacement surgery is not advisable, the stability can be provided by tectoplasty24 an acetabuloplasty, which aims to provide an extra-articular weight-bearing surface in cases of dysplastic acetabulum, hip subluxation or dislocation with a false acetabulum [Figure 7a and b] (Reproduced from Saito et al. J Bone Joint Surg 1986; 68: 55-60)]. After raising the outer table of the iliac bone at the lateral edge of the affected acetabulum, as a proximally-based flap, bone grafts are inserted in the space to provide a congruous, nonabsorbable roof for the femoral head [Figure 8a and b].
Figure 7.
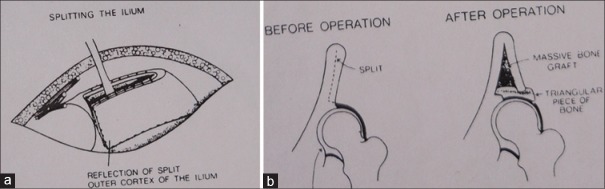
Schematic diagram of steps of tectoplasty. (a) The outer cortex of ilium is split away from the inner cortex and reflected outwards. The cavity thus created is filled up with bone graft. (b) Sectional diagram to show the aim of the operation (reproduced from Saito et al.24)
Figure 8.
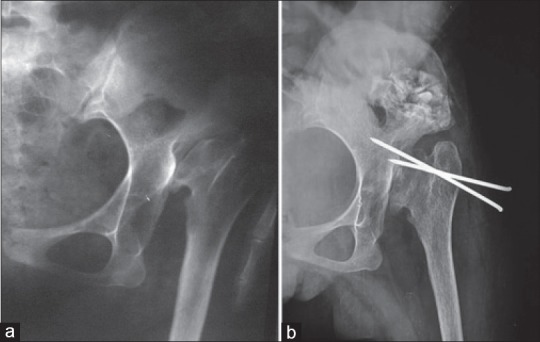
X-ray left hip anteroposterior view showing (a) old healed tubercular arthritis hip with dislocation. (b) Tactoplasty after pulling the head down. For initial six weeks, temporary stabilization is provided by k wire fixation, to be removed around 6 weeks
Prognosis
Outcome of treatment depends upon the stage of the disease at the time of presentation. Synovial involvement alone will show a very good result with chemotherapy and functional exercises. There is always some residual deformity with late presentation. Campbell and Hoffman16 observed relationship between radiological type and results with treatment. Good results were observed with “normal type” and “Perthes type;” whereas the “travelling acetabulum type,” “dislocation type,” “mortar and pestle” type showed bad prognosis. With modern diagnostic facilities, the patients are being diagnosed early along with very effective antitubercular drugs, hence the number of patients with advanced radiological changes are going down. On the other hand there is a worldwide threat of an untreatable epidemic of multidrug resistant TB with the global explosion of HIV and irrational treatment in some parts of the world.11 In HIV positive patients, the prognosis also depends upon the stage of HIV infection and CD counts. The good nutritional status and control of any co morbidities helps in minimizing the chances of recrudescence.
Management in children
The aim of management is to have a painless, mobile hip with anatomy of the hip joint as near to normal as possible. The late secondary osteoarthritis is always a concern despite the healing of the disease. For this reason, early detection and management is even more important in this age group. With pathological subluxation and dislocation, it may be impossible to obtain a congruous hip. Further, a fixed hip in nonanatomical position puts the other hip, spine and knee in mechanical disadvantages with resulting consequences.
The cornerstone of management is early diagnosis. Once suspected clinically, radiological examination of both hips and lungs should be analyzed critically. The other investigations like complete blood count, erythrocyte sedimentation rate, C-reactive protein, Mantoux test are either supportive or to exclude pyogenic and other types of arthritis. Since the bone and joint TB is secondary to primary pathology somewhere else in the body, investigations should also aim to find the primary site of lesion, like lungs, lymph nodes, etc., The diagnosis of the primary site may not be possible many a times. Shiv et al. recommends USG of the hip to confirm fluid inside before patient is subjected to arthrotomy or drainage.34 however, in our opinion absence of fluid, is not a contraindication for arthrotomy. Analysis of joint aspirate may help in excluding some of the other causes of painful hip in children like septic arthritis, transient synovitis, hemarthrosis, etc., In children, arthrotomy for diagnosis purpose is usually not required; however, if joint is opened as part of management strategies, the tissue should be subjected for microbiological, histological, and PCR.
The management in children as in adults depends upon the stage at presentation. Moon et al.20,22 introduced a working classification system based on the joint stability, cephalocotyloid morphology and its anatomical relationship. Synovitis and early arthritis are treated by nonoperative measures. In addition to anti tubercular chemotherapy, skin traction/skeletal traction in mild to severe deformity is sufficient in most of the cases. We prefer the traction, since assisted movements of the hip joint can be started earlier. Whenever there is an issue of compliance with continuous traction as in very young children or if joint is very painful, hip spica can be applied for 4-6 weeks to reduce the pain before movements are started. The management in advanced joint destruction, wandering acetabulum or with pathological subluxation and dislocation is difficult and controversial.31,35 Our opinion is that though the majority of the hips can be made painless eventually by ATT and traction alone, however, an arthrotomy and surgical debridement will give early resolution of the disease. It can also take care of deformities. For example, with anterolateral approach to the joint, one can correct the flexion deformity of the hip. In children, we should try to preserve the viable bone as much as possible. Children have great potential for regeneration and remodeling. In the current scenario, we do not recommend excision arthroplasty or arthrodesis before skeletal maturity. Instead, a stabilization procedure can be done to provide stability. Moon et al. recommended early variation osteotomy to restore a normal cephalocotyloid relation of the travelling acetabulum secondary to hip TB in children.22
CONCLUSION
The TB of hip is still a common condition in developing countries. Early presentations are pain around hip and limp. Later the patient presents with deformities, shortening of limb and restriction of movements. The constitutional symptoms may or may not be present in all the cases. Diagnosis is mainly clinicoradiological, however, supportive blood investigations and imaging modalities like USG and MRI are helpful. Histological proof may not be necessary in all the cases in the endemic zones for TB. The management depends upon the stage of clinical presentation and the severity of destruction as visible radiologically. From conservative therapy in the form of ATT and traction to debridement and joint replacement, a variety of surgical procedures have been described. On an average 2-5% of patient's report back with reactivation of the disease within about 20 years after the apparent clinical healing of the first lesion.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Tuli SM. 4th ed. New Delhi: Jaypee Brothers Medical Publishers Pvt. Ltd; 2010. Tuberculosis of the Skeletal System (Bones, Joints, Spine and Bursal sheaths) pp. 4, 69–110. [Google Scholar]
- 2.Global Tuberculosis Report 2013; Executive Summary, WHO/HTM/TB/2013.15.pp2. [Last accessed 2014 Jun 13]. Available from: http://www.who.int/tb/publications/global_report/en/
- 3.Sandhu HS, Kalhan BM, Dogra S. Shanmughasundaram TK, editor. Management of tuberculosis of the hip joint. Current Concepts in Bone and Joint Tuberculosis. 1983 147, EVR Periyar Road, Madras, India. [Google Scholar]
- 4.Tuli SM, Mukherjee SK. Excision arthroplasty for tuberculous and pyogenic arthritis of the hip. J Bone Joint Surg Br. 1981;63-B:29–32. doi: 10.1302/0301-620X.63B1.7204469. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Wang J, Xu Z, Li Y, Wang H. Total hip arthroplasty for active tuberculosis of the hip. Int Orthop. 2010;34:1111–4. doi: 10.1007/s00264-009-0854-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sidhu AS, Singh AP, Singh AP. Total hip replacement in active advanced tuberculous arthritis. J Bone Joint Surg Br. 2009;91:1301–4. doi: 10.1302/0301-620X.91B10.22541. [DOI] [PubMed] [Google Scholar]
- 7.Wilkinson MC. Tuberculosis of the hip and knee treated by chemotherapy, synovectomy, and débridement. A followup study. J Bone Joint Surg Am. 1969;51:1343–59. doi: 10.2106/00004623-196951070-00013. [DOI] [PubMed] [Google Scholar]
- 8.Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;398:11–9. doi: 10.1097/00003086-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Babhulkar S, Pande S. Tuberculosis of the hip. Clin Orthop Relat Res. 2002;398:93–9. doi: 10.1097/00003086-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Govender S. The outcome of allografts and anterior instrumentation in spinal tuberculosis. Clin Orthop Relat Res. 2002;398:60–6. doi: 10.1097/00003086-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Babhulkar SS. Editorial comments. Clin Orthop Relat Res. 2002;398:2–3. [Google Scholar]
- 12.Sankaran B. Tuberculosis of bones and joints. Indian J Tuberculosis. 1993;40:109–19. [Google Scholar]
- 13.Shanmugasundaram TK. Tuberculosis of Spine. Ind J Tuberculosis. 1982;29:213–21. [Google Scholar]
- 14.Hoffman EB, Crosier JH, Cremin BJ. Imaging in children with spinal tuberculosis: A comparison of radiography, computed tomography and magnetic resonance imaging. J Bone Joint Surg Am. 1993;75:223–9. doi: 10.1302/0301-620X.75B2.8444943. [DOI] [PubMed] [Google Scholar]
- 15.Shanmugasundaram TK. A clinicoradiological classification of tuberculosis of the hip. In: Shanmugasundaram TK, editor. Current Concepts in Bone and Joint Tuberculosis. Madras, India: Proceedings of Combined Congress of International Bone and Joint Tuberculosis Club and the Indian Orthop Assoc; 1983. p. 60. [Google Scholar]
- 16.Campbell JA, Hoffman EB. Tuberculosis of the hip in children. J Bone Joint Surg Br. 1995;77:319–26. [PubMed] [Google Scholar]
- 17.Midiri M, Filosto L, Lo Casto A, Masciocchi C. Magnetic resonance in the study of tubercular coxitis. Radiol Med. 1992;83:38–42. [PubMed] [Google Scholar]
- 18.Shanmugasundaram TK. Bone and joint tuberculosis – Guidelines for management. Indian J Orthop. 2005;39:195–8. [Google Scholar]
- 19.Singhal O, Kaur V, Kalhan S, Singhal MK, Gupta A, Machave Y. Arthroscopic synovial biopsy in definitive diagnosis of joint diseases: An evaluation of efficacy and precision. Int J Appl Basic Med Res. 2012;2:102–6. doi: 10.4103/2229-516X.106351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moon MS, Lee KS, Kim YS. Varisation osteotomy in subluxated hip as sequella of healed tuberculosis in children. J Korean Orthop Assoc. 1982;17:203–5. [Google Scholar]
- 21.Silber JS, Whitfield SB, Anbari K, Vergillio J, Gannon F, Fitzgerald RH., Jr Insidious destruction of the hip by Mycobacterium tuberculosis and why early diagnosis is critical. J Arthroplasty. 2000;15:392–7. doi: 10.1016/s0883-5403(00)90900-8. [DOI] [PubMed] [Google Scholar]
- 22.Moon MS, Kim SS, Lee SR, Moon YW, Moon JL, Moon SI. Tuberculosis of hip in children: A retrospective analysis. Indian J Orthop. 2012;46:191–9. doi: 10.4103/0019-5413.93686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vora PH. Role of early surgery in management of tuberculosis of hip. In: Shanmugasundaram TK, editor. Current Concept in Bone and Joint Tuberculosis. Madras, India: Proceedings of Combined Congress of International Bone and Joint Tuberculosis Clue and the Indian Orthopedic Association; 1983. p. 22. [Google Scholar]
- 24.Saito S, Takaoka K, Ono K. Tectoplasty for painful dislocation or subluxation of the hip. Long-term evaluation of a new acetabuloplasty. J Bone Joint Surg Br. 1986;68:55–60. doi: 10.1302/0301-620X.68B1.3510216. [DOI] [PubMed] [Google Scholar]
- 25.Milch H. The Pelvic support osteotomy. J Bone Joint Surg Am. 1941;23:581–595. [Google Scholar]
- 26.Kim SJ, Postigo R, Koo S, Kim JH. Total hip replacement for patients with active tuberculosis of the hip: A systematic review and pooled analysis. Bone Joint J. 2013;95-B:578–82. doi: 10.1302/0301-620X.95B5.31047. [DOI] [PubMed] [Google Scholar]
- 27.Kim YH, Han DY, Park BM. Total hip arthroplasty for tuberculous coxarthrosis. J Bone Joint Surg Am. 1987;69:718–27. [PubMed] [Google Scholar]
- 28.Kim YY, Ahn BH, Bae DK, Ko CU, Lee JD, Kwak BM, et al. Arthroplasty using the Charnley prosthesis in old tuberculosis of the hip. Clinical experience with 8-10-year followup evaluation. Clin Orthop Relat Res. 1986;211:116–21. [PubMed] [Google Scholar]
- 29.Jupiter JB, Karchmer AW, Lowell JD, Harris WH. Total hip arthroplasty in the treatment of adult hips with current or quiescent sepsis. J Bone Joint Surg Am. 1981;63:194–200. [PubMed] [Google Scholar]
- 30.Neogi DS, Yadav CS, Ashok Kumar, Khan SA, Rastogi S. Total hip arthroplasty in patients with active tuberculosis of the hip with advanced arthritis. Clin Orthop Relat Res. 2010;468:605–12. doi: 10.1007/s11999-009-0957-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoon TR, Rowe SM, Santosa SB, Jung ST, Seon JK. Immediate cementless total hip arthroplasty for the treatment of active tuberculosis. J Arthroplasty. 2005;20:923–6. doi: 10.1016/j.arth.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Oztürkmen Y, Karamehmetoğlu M, Leblebici C, Gökçe A, Caniklioğlu M. Cementless total hip arthroplasty for the management of tuberculosis coxitis. Arch Orthop Trauma Surg. 2010;130:197–203. doi: 10.1007/s00402-009-0967-9. [DOI] [PubMed] [Google Scholar]
- 33.Kim YY, Ko CU, Ahn JY, Yoon YS, Kwak BM. Charnley low friction arthroplasty in tuberculosis of the hip. An eight to 13-year followup. J Bone Joint Surg Br. 1988;70:756–60. doi: 10.1302/0301-620X.70B5.3192574. [DOI] [PubMed] [Google Scholar]
- 34.Shiv VK, Jain AK, Taneja K, Bhargava SK. Sonography of hip joint in infective arthritis. Can Assoc Radiol J. 1990;41:76–8. [PubMed] [Google Scholar]
- 35.Moon MS, Rhee SK, Lee KS, Kim SS. A natural course of a dislocated healed tuberculous hip in a child. A case report. Clin Orthop Relat Res. 1984;190:154–7. [PubMed] [Google Scholar]


