Abstract
We present an adolescent with distal radius nonunion following an open fracture and failed surgery which eventually united when the length and stability was restored for eight weeks duration. The intact periosteal sleeve at the nonunion site formed new bone when its tension was restored by gradual differential distraction. This case report highlights the possibility of stimulating bony union in an established atrophic nonunion by distracting the minimally disturbed soft tissue and thick osteogenic periosteal envelope in the paediatric age group.
Keywords: Distal radius, nonunion, open fracture, pediatric, periosteum, osteogenic, distraction, atrophic
MeSH terms: Fractures ununited, compound, radius fractures, pediatric
INTRODUCTION
Nonunion in pediatric fractures has been reported in diaphyseal regions.1 In the words of Mercer Rang “nonunion is an adversary almost not known to the child orthopedic surgeon”.2 Nonunion following distal radius metaphyseal fracture is rare. The reported incidence in a series including adults was 0.2% in New York State Worker's Compensation Board.3 To the best of our knowledge only three such reports are cited in literature in pediatric age group.4,5,6 We present a case of posttraumatic manus valgus deformity secondary to persistent nonunion of a distal radius metaphyseal fracture.
CASE REPORT
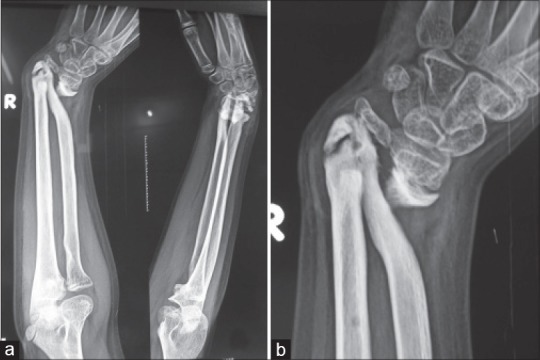
A 14 year old boy presented with the complaints of pain, progressive deformity and difficulty in writing using his right hand of 1 year duration. The deformity occurred following a fall from 10 feet height when he sustained an injury of his right forearm. He was initially managed by an osteopath with cleaning, dressing and splint immobilization. No radiographic documentation was carried out at that time. The pain subsided and splint was taken out after 6 weeks. His parents noticed a deformity of the forearm at this time, but did not pursue any further treatment. As the deformity gradually worsened, the child was taken to medical center 4 months after the injury where he was evaluated with radiographs and treated with distal ulnar shortening to correct the forearm deformity [Figure 1]. After 6 weeks of immobilization the child resumed regular activities. He noticed further progression of deformity with pain and difficulty while writing. At this point, he came to our center 1 year after the initial injury. The history was suggestive of punctured wound over the volar aspect on the ulnar side just proximal to the wrist crease, which healed uneventfully with regular dressings. There was no history of persistent infection or wound discharge.
Figure 1.

X-ray of forearm with wrist joint anteroposterior and lateral views showing (a) Nonunion distal radius with positive ulnar variance. (b) Post ulnar shortening
Examination of the right forearm and hand revealed a manus valgus deformity of 45°. A small puckered scar adherent to underlying structures was noted over the ulnar side just proximal to the wrist crease and no sign suggestive of high grade soft-tissue disruption. A surgical scar was seen over the dorsal aspect of the distal ulna. The ulnar styloid was prominent and extrinsic flexor tightness of 20° (degree) was noted in the fourth and fifth fingers. Wrist dorsiflexion was 5° and palmar flexion was 15° both active and passive. There was a jog of forearm supination and pronation. Shortening of right forearm by 7.5 cm was noted and there was stiffness of the metacarpophalangeal joints and interphalangeal joints. The metacarpophalangeal joints had a jog of passive movement. Active and passive flexion ranging from 20-50° (degree) was noted in the proximal, middle and distal interphalangeal joints.
Erythrocyte sedimentation rate and C-reactive protein were within normal limits. Review of his forearm radiograph carried out before ulnar shortening did not show comminution of radius fracture and there was no ulnar nonunion. The following radiographs revealed a distal radius metaphyseal nonunion with tapered proximal fragment pointing toward the ulna with narrowing of the interosseous space. There was a positive ulnar variance. Due to previous surgery the distal ulna had a nonunion with its epiphysis as well [Figure 2]. Magnetic resonance imaging (MRI) confirmed the diagnosis [Figure 3] and there were no signs of infection in MRI as well. Preoperative computed tomogram revealed the relative position of the fragments [Figure 4].
Figure 2.
Radiograph of the right forearm anteroposterior and lateral views (a) showing distal radius portraying the nonunion with manus valgus deformity (b) close up view of same x-ray
Figure 3.

Magnetic resonance imaging (a) Coronal T2 fat suppression images showing the nonunion site at the right distal radius. (b) T1- weighted coronal image showing the distal radius nonunion
Figure 4.

Computed tomogram showing distal radius (arrow) and ulna nonunion
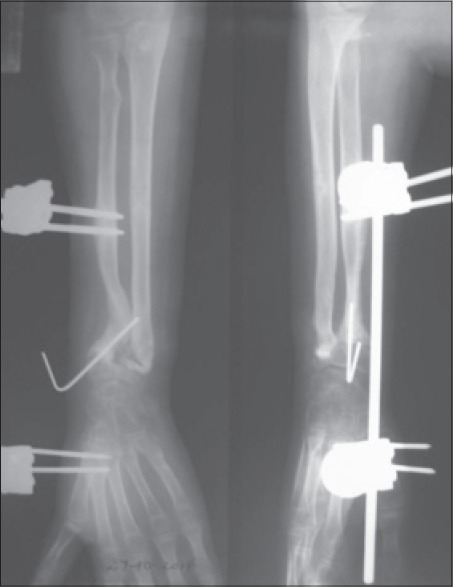
After discussion with the parents and the boy, a preoperative decision was made to do fixator assisted distraction of the forearm bones as a staged procedure to gain length, to be followed later by bone grafting at the site of nonunion. Under general anesthesia monolateral minirail fixator was applied on both radius and ulna percutaneously under image guidance. The nonunion site was not exposed as per the preoperative planning. The parents were taught to do differential distraction and at a rate of 2 mm/day on the radial side and 1 mm/day on the ulnar side from the next day [Figure 5]. Child was followed up with serial radiographs as an outpatient. At the 4th week of distraction the radius had achieved the required length and the ulnar variance got corrected and he was called back for bone grafting. The patient however did not show up at 4 weeks as instructed for bone grafting, but he visited us back at 8 weeks. The repeat radiographs showed new bone formation along the periosteal sleeve of both radius and ulna.
Figure 5.

Postoperative radiographs of forearm and wrist anteroposterior and lateral views showing the minirail fixator on the distal radius and ulna and differential distraction in progress
At 8 weeks through a volar approach, the bony projection at the proximal end of union site interposing the interossous space was removed as it was hindering the forearm rotation. An intact periosteal sleeve with the new bone at the nonunion site was found and left disturbed. The union site was reinforced with a Kirschner wire [Figure 6]. Biopsy to rule out infection was not done to avoid violating the periosteum and callus at the nonunion site. The fixator was removed along with the Kirschner wire after 3 weeks and a volar splint was used for another 3 weeks and active range of motion therapy was started [Figure 7]. At 1 year followup the boy is pain free and able to do all activities of daily living including writing without pain and the parents were happy with the cosmesis achieved. The child is not willing for any kind of intervention for extrinsic flexor tightness. The preoperative Disabilities of the Arm Shoulder and Hand (DASH) score was 20 and the postoperative DASH score was 28.7 at 1 year followup. Passive palmar flexion had improved to 45° and dorsiflexion to 30° at the end of treatment. Forearm had a passive pronation of 50° and 80° supination [Figure 8].
Figure 6.
Followup radiographs of forearm and wrist showing spontaneous union at the end of deformity correction in distal radius which was stabilized with Kirshner wire
Figure 7.

Radiograph at fixator removal depicting union at the fracture site
Figure 8.
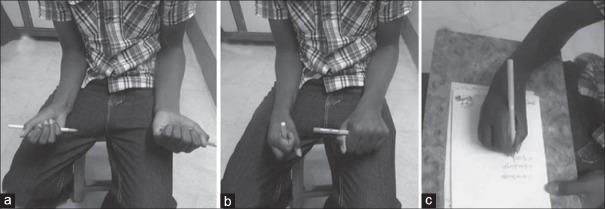
Clinical photograph showing the range of motion and function at one year followup. Active supination and pronation in the right forearm (a and b). The child could grip a pen firmly and write legibly (c)
DISCUSSION
This case report attempts to highlight a rare complication of nonunion in a distal radius metaphyseal fracture in a child and the ability of intact periosteum to reform the bone when length and tension are maintained [Figure 9]. The child had persistent painful nonunion due to various factors such as open injury, inadequate immobilization, and a suspected subacute infection in the initial period.
Figure 9.
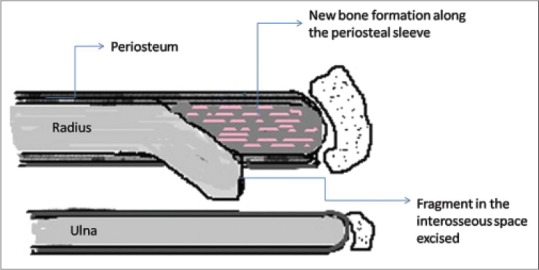
Schematic diagram showing the intraoperative findings
Kwa et al. in the first ever case reported had described a distal radius nonunion following a closed fracture in an otherwise healthy child.4 This was managed by bone grafting and casting. The factors attributed to nonunion in this report were inadequate immobilization and severe initial displacement. In two other case reports, nonunion in children had been attributed to open surgery5, soft-tissue or vascular problems.7
Open injury, high energy fractures, soft-tissue or vascular problems, open surgery, older age group, presence of infection and inadequate immobilization are contributory to pediatric fracture nonunion.2,5,8,7,9 Examination of the serial radiographs and MRI of our patient did not reveal evidence of any local pathology including neurofibromatosis or chronic infection.
Sabharwal6 described bone transport of radius with Ilizarov apparatus in a 12-year-old boy with acquired posttraumatic radial club hand. around 5.1 cm of lengthing was achieved and the docking site was grafted in his case. In our patient after distraction, the stability provided by the fixator and the restoration of length and tension in the periosteum initiated spontaneous regeneration of bone. This was confirmed when we explored for removing the impinging corner of proximal radius and an artist's view of the intraoperative finding is given [Figure 9].
Distraction and compression with Ilizarov circular frames have been used for management of hypertrophic nonunion.10 Though compression is the current standard of care for atrophic nonunion,11 this report has demonstrated that distraction of atrophic nonunion can lead to bone formation in pediatric age group provided the periosteal sleeve remains undisturbed. As our initial plan was to gain radial length and correct ulnar variance followed by open bone grafting, we did not use circular frame as osteotomy and compression were not planned, instead a monolateral frame was used.
Wilde et al. explained that circumferential periosteal release leads to correction of limb length discrepancy and they found that the periosteum is under tension in a child and it retracts on sectioning12 and this was reiterated by Warrel and Taylor.13
Meticulous closure of periosteum at the donor site of fibula graft and tibial cortical graft has been shown to promote rapid healing of donor site defect.14,15 Humoral and genetic factors have been described to cause spontaneous regeneration of bone defects in segmental femoral fracture of various lengths in adults when length and stability of the periosteum was maintained.16
It becomes clear that the periosteum has great osteogenic potential in children. This can be exploited to bridge bone defects and promote union in conditions where the periosteal sleeve is intact. Our case highlights this phenomenon and also demonstrates that nonunion can occur in the pediatric age group if the basic principles of management are disregarded. We recommend external fixation with distraction as one of the treatment options to treat pediatric atrophic nonunion in selected patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Shrader MW, Stans AA, Shaughnessy WJ, Haidukewych GJ. Nonunion of fractures in pediatric patients: 15-year experience at a level I trauma center. Orthopedics. 2009;32:410. doi: 10.3928/01477447-20090511-11. [DOI] [PubMed] [Google Scholar]
- 2.Rang M, Wenger DR. Children are not just small adults. In: Wenger DR, Pring ME, Rang1 M, editors. Rang's Children's Fractures. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 8. [Google Scholar]
- 3.McKee MD, Waddell JP, Yoo D, Richards RR. Nonunion of distal radial fractures associated with distal ulnar shaft fractures: A report of four cases. J Orthop Trauma. 1997;11:49–53. doi: 10.1097/00005131-199701000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Kwa S, Tonkin MA. Nonunion of a distal radial fracture in a healthy child. J Hand Surg Br. 1997;22:175–7. doi: 10.1016/s0266-7681(97)80056-3. [DOI] [PubMed] [Google Scholar]
- 5.Song KS, Kim HK. Nonunion as a complication of an open reduction of a distal radial fracture in a healthy child: A case report. J Orthop Trauma. 2003;17:231–3. doi: 10.1097/00005131-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Sabharwal S. Treatment of traumatic radial clubhand deformity with bone loss using the Ilizarov apparatus. Clin Orthop Relat Res. 2004;424:143–8. doi: 10.1097/01.blo.0000128284.13331.c5. [DOI] [PubMed] [Google Scholar]
- 7.Waters P, Bae DS. Fractures of distal radius and ulna. In: Beaty JH, Kasser JR, editors. Rockwood and Wilkins Fractures in Children. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 335. [Google Scholar]
- 8.Fernandez FF, Eberhardt O, Langendörfer M, Wirth T. Nonunion of forearm shaft fractures in children after intramedullary nailing. J Pediatr Orthop B. 2009;18:289–95. doi: 10.1097/BPB.0b013e32832f5b20. [DOI] [PubMed] [Google Scholar]
- 9.Théorêt C, Stanciu C. Post - traumatic nonunion of the ulna in a child. Can J Surg. 2001;44:301–3. [PMC free article] [PubMed] [Google Scholar]
- 10.Kocaoğlu M, Eralp L, Sen C, Cakmak M, Dincyürek H, Göksan SB. Management of stiff hypertrophic nonunions by distraction osteogenesis: A report of 16 cases. J Orthop Trauma. 2003;17:543–8. doi: 10.1097/00005131-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Tomiì S, Bumbasireviì M, Lesiì A, Mitkoviì M, Atkinson HD. Ilizarov frame fixation without bone graft for atrophic humeral shaft nonunion: 28 patients with a minimum 2-year follow-up. J Orthop Trauma. 2007;21:549–56. doi: 10.1097/BOT.0b013e31814612c8. [DOI] [PubMed] [Google Scholar]
- 12.Wilde GP, Baker GC. Circumferential periosteal release in the treatment of children with leg-length inequality. J Bone Joint Surg Br. 1987;69:817–21. doi: 10.1302/0301-620X.69B5.3680350. [DOI] [PubMed] [Google Scholar]
- 13.Warrell E, Taylor JF. The role of periosteal tension in the growth of long bones. J Anat. 1979;128:179–84. [PMC free article] [PubMed] [Google Scholar]
- 14.Xin ZF, Kim KH, Jung ST. Regeneration of the fibula using a periosteum-preserving technique in children. Orthopedics. 2009;32:820. doi: 10.3928/01477447-20090922-14. [DOI] [PubMed] [Google Scholar]
- 15.Dodabassappa SN, Shah HH, Joseph B. Donor site morbidity following the harvesting of cortical bone graft from the tibia in children. J Child Orthop. 2010;4:417–21. doi: 10.1007/s11832-010-0277-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinsche AF, Giannoudis PV, Matthews SE, Smith RM. Spontaneous healing of large femoral cortical bone defects: Does genetic predisposition play a role? Acta Orthop Belg. 2003;69:441–6. [PubMed] [Google Scholar]


