Abstract
Objective
to identify, in 2011, rates of hypertension, cardiovascular and gestational problems in subjects presenting high blood pressure in 1982, when correct cuff size was used, according to the American Heart Association Arm Circumference/Cuff Width ratio of 0.40.
Methods
high blood pressure was defined in 2011 as systolic = 115 mmHg and diastolic = 80mmHg, resulting in 20 subjects between 39 and 43 years old. (Risk Group). They were compared to 20 subjects from the original sample with lower blood pressure values (Control group).
Results
the rates of hypertension, cardiovascular and gestational problems were significantly higher (Fisher: p=0.02) in the Risk Group, with one case of cardiovascular death. Our findings arouse speculations about whether, if a proper cuff had been used in clinical practice, the complications and death could have been avoided.
Conclusions
data suggest compliance with the use of cuff width corresponding to 40% of arm circumference, despite polemics concerning cuff availability and difficulties of using many sizes.
Keywords: Arterial Pressure, Adolescent, Hypertension, Risk Factors
Background
In 1901, Von Recklinghausen observed that the Riva Rocci cuff, 4.5 cm wide, led to blood pressure (BP) overestimation. Such effects were also studied in classical works performed between the 1930's and 1980's, which also revealed problems of BP underestimation caused by larger cuffs. These studies were reviewed in 1996, when a century of the Riva-Rocci sphygmomanometer was celebrated(1). Controversial aspects of the data regarding cuff sizes remain unclear until date.
From 1951 to 1993, the American Heart Association (AHA) recommended an arm circumference/cuff width (AC/CW) ratio of 0.40 and cuff length reaching at least 80% of AC, to avoid over or underestimated BP readings(2-3). The ratio 0.40 was also recommended for use in children and adolescents. Despite the ratio recommendation, a standard cuff 9 cm large was introduced to be used in adolescents, and the standard cuff for adults (12 cm) was also indicated for grown children(4). A contradiction between the theoretical framework and the recommended practice remained in the most recent AHA revision for cuff size (2005), which unsuccessfully attempted to change the ratio value(5).
In 1982, we applied the traditional AHA recommendation for cuff width (ratio 0.4) to measure BP in 999 subjects from the University of São Paulo (USP), 10-59 years old, 299 students, 300 faculty members and 400 officials. Among them, 99 were adolescents from 10 to 14 years old(6), and a fifth revealed hypertensive BP values in 1982, when measured with the recommended 0.40 ratio.
Objective
To evaluate, after 29 years, the rates for hypertension, cardiovascular and gestational problems (target events) in adolescents presenting high BP values in 1982, when cuff width corresponding to 40% of arm circumference was used in compliance with the American Heart Association recommended ratio 0.40.
Methods
A longitudinal study (1982-2011) was performed in 1982 on the University of São Paulo Campus and in 2011 at places the subjects followed had chosen.
Administrative and ethical requirements
The 1982 study was performed at the University of São Paulo School of Pedagogy, following approved faculty proceedings valid at that time. The present study (2011) received approval from the Ethics Committee at the University Guarulhos under number 16/2007 (SISNEP/228). All participants were informed about the study goals and variables, as well as the conditions of their participation. They gave formal written consent, indicating their understanding and agreement to participate in the study.
Recruitment
Subjects were initially contacted by phone or internet. Each of them could choose the place to be interviewed. Although the main aim of the present study was not to measure BP, we realized that this was an attractive reason to increase cooperation.
Design
In 1982, 99 subjects between 10 and 14 years old were studied at the USP Campus as part of a larger protocol. From this original sample, we selected subjects with a systolic BP = 115mmHg and diastolic = 80mmHg in 1982, completing 20 subjects considered as the Risk Group (RG) in 2011. For each of them, a colleague from the original 1982 sample was selected, who had similar socio-demographic characteristics (sex, ethnic and age) and who presented normal BP values in 1982. These 20 subjects were evaluated as Control Group (CG). In other words, the total sample included 40 subjects in 2011, 39-43 years old, 22 of them women, 50% in each group.
Observers and equipment
The use of a double stethoscope facilitated the training between two observers, both nurses. They used two Tycos aneroid manometers because they were easier and quicker to remove from one cuff to another, so as to attend to different AC, at one-minute intervals. Tested weekly against a mercury manometer, the aneroid matched this gold standard equipment at the middle third of the mercury scale (0 mmHg) across the data collection period (only two mmHg differences were observed at the superior and inferior thirds of the scale manometer).
Blood pressure measurement procedure in 1982
It is important to note that BP was measured under a strict protocol to avoid observer, equipment and environment errors, as well as any alarming subject reaction. AC was measured at the middle point of the brachial biceps to apply the AHA ratio 0.4 in order to identify the appropriate cuff size, which the authors named "correct cuff". This cuff was selected from a kit with several widths, varying per centimeter from 7 to 14 cm. The width/length proportion of all cuffs was 1:2. Therefore, cuff width corresponded to 40% of AC and cuff length to 80%, as recommended(6). The arm was placed at the level of the fourth intercostal space, the back resting against the chair backrest. After placing the cuff on the left arm, the subject was asked to stay comfortably for five minutes, relaxing as much as possible physically and mentally. Good compliance was observed after explaining the importance of subject collaboration to reach BP levels near to their resting ones. After one initial measurement, allowing the subjects to familiarize with the measurement procedure, three measurements were performed to calculate the mean value. The criterion to determine diastolic pressure was the fifth Korotkoff sound, as currently recommended. Weight and height measurements were taken to calculate the Body Mass Index. Identification of adolescents with high BP values led researchers to advise their parents to take them for cardiovascular check-up, keeping in mind that only the standard cuff was available in the health units where they were classified as healthy subjects in 1982.
Blood pressure measurement procedure in 2011
The measurement was similar to that adopted in 1982. Weight and height were referred to calculate BMI. To reach the main goal, the subjects were asked about hypertension and cardiovascular and gestational problems diagnosed in health services or medical offices between 1982 and 2011. Data regarding one man's death (25 years old) was obtained from his mother.
Analyses
Data were analyzed using the Statistical Program for the Social Sciences (SPSS 20). Categorical data related to groups were compared using Fisher's Exact Test.
Results
Descriptive results for Arm Circumference and Body Mass Index
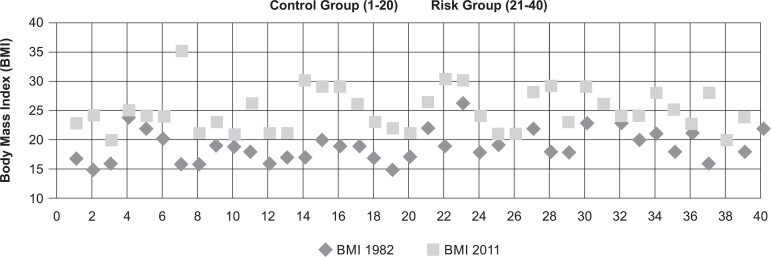
After 29 years, most subjects had an increase in BMI in 2011 relative to 1982, due physical changes from adolescence to adulthood. We found a greater number of overweight subjects in the RG in 2011 when compared to the BMI distribution in 1982, although the only obese found in 2011 was identified in the CG (see Figure 1). The presence of underweight subjects in 1982 as well as in 2011 is noteworthy.
Figure 1.
Body Mass Index distribution as a function of year and groups. São Paulo, SP, Brazil, 2011
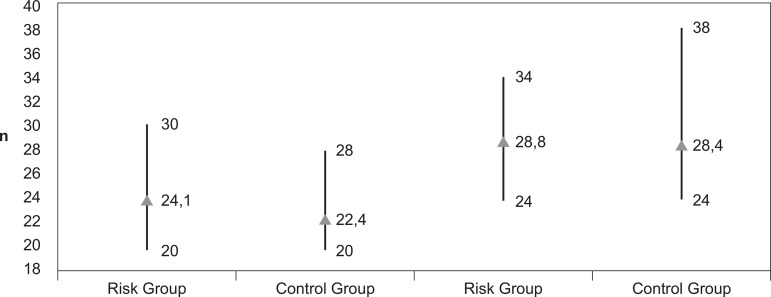
Figure 2 presents data regarding AC in both groups.
Figure 2.
Arm Circumference distribution in 1982 (left) and 2011(right): mean; maximum value and minimum value. São Paulo, SP, Brazil, 2012
The graph reveals a wide range in AC distribution, particularly in 2011 (CG), varying from 24 to 38cm. It is important to note that, even in 2011, the mean AC does not reach 29 cm. The individual values for AC can be observed in Figure 3.
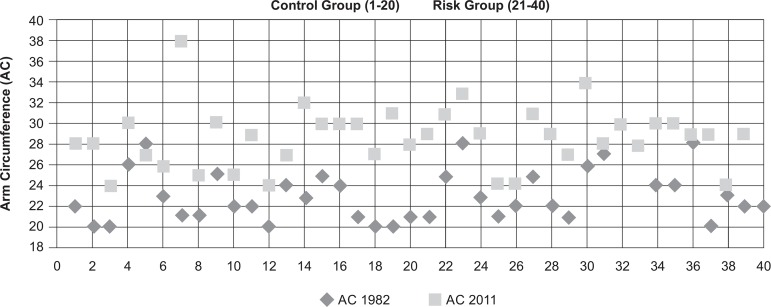
Figure 3.
Individual Arm Circumference distribution as a function of year and groups. São Paulo, SP, Brazil, 2011
None of the subjects had AC reaching 30 cm in 1982 and only seven cases of AC > 30 cm were found in 2011, when they were 39-42 years of age. This is a relevant finding in relation to the inappropriateness of the standard cuff (12cm) in the sample subjects.
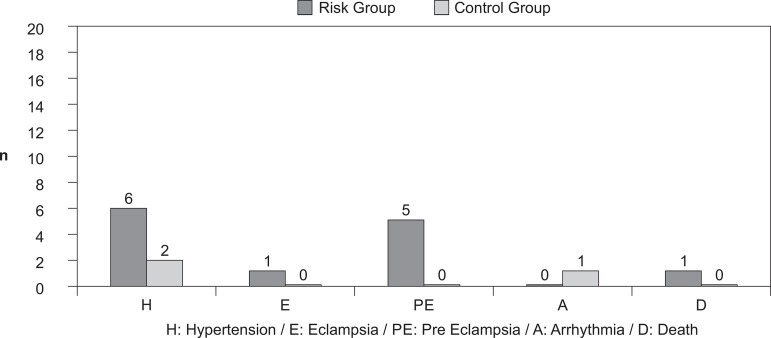
Results for hypertension, cardiac or gestational disorder rates
We found a statistically significant (Fisher: p=0.02) higher rate for the target events (hypertension and cardiac or gestational disorders) in the RG (55.0%) relative to the CG (10.0%). The distinct health problems found in both groups are displayed in Figure 4.
Figure 4.
Absolute frequency (n) related to diagnosed events: rates for hypertension, cardiac or gestational complications and death as a function of groups. São Paulo, SP, Brazil, 2011
In the RG, we found nine subjects with 12 target events. Among them, six were diagnosed as hypertensive in 2011, but only three were under drug treatment. Four females from RG informed five pregnancy events. One had two episodes of pre-eclampsia and is currently under hypertensive treatment. Another had eclampsia in the first pregnancy and pre-eclampsia in the second one, resulting in two miscarriages. Her third and fourth pregnancies were successful after hypertension treatment since the beginning of the gestational period. One male (25 years old) died after a cardiac fibrillation, at the University of São Paulo campus, subsequent to a soccer game. His BP values in 1982 (10 years old) were 126/89 mmHg and heart rate 96. In the control group, one subject had presented arrhythmia not associated with hypertension and another one had only one episode of hypertension.
Discussion
Our data shows important differences between the risk and control groups in the target events: hypertension, cardiovascular and gestational disorders and cardiovascular death rates. These results arouse serious concerns regarding BP evaluation during childhood and adolescence. The European Society of Hypertension emphasized "the growing evidence that children and adolescents with mild BP elevations are much more common than it was thought in the past"(7). A recent review emphasized the higher prevalence of hypertension in adolescents with the increase in obesity worldwide(8). Despite the marked increase in Body Mass Index in children and teenagers in the last two decades, our findings suggest the use of the appropriate cuff in all of them. The lack of AC size knowledge and cuff errors in the field of hypertension diagnosis is a subject of our concern, as recently discussed(9). Although cuff size is frequently mentioned in scientific literature, researchers' attention has been focused only on overweight and obese subjects with large arms. Knowledge regarding AC is poor because researchers adapt their scientific observations according to the cuff size available. Cuff unavailability is a common fact at health institutions(10), resulting in studies of hypertensive, diabetics and obese patients in which only one or two size cuff are employed. Furthermore, there is a shortage of studies showing the correspondence between BMI and AC, as well as the use of proper AC cuff in the general population.
Studies from distinct countries indicate that millions of adolescent females and young women have arm circumferences lower than 28 cm(11-12). We expected a low AC mean in 1982 due to the subjects' age range. However, even in 2011, many of them did not reach 30cm in AC. It should be emphasized that, when the ratio 0.40 is applied to an arm circumference of 30 cm, the traditional 12 cm standard cuff suits the arm perfectly, avoiding over or underestimated BP readings. Our data suggest that the subjects were vulnerable to have their BP readings underestimated in 1982 and that many of them continued under risk up to 2011.
In a study performed in 430 hypertensive patients, the majority overweight or obese (BMI 29.6±0.60), 61% of the subjects had AC = 30 cm (12). According to the author, the use of larger cuffs avoided BP overestimation in these patients. Nevertheless, no mention was made to those with AC lower than 30 cm (29%), leading to the possible masking of a hypertension diagnosis, particularly in women(13). On the opposite, in another North American study performed in 2424 adults (1484 female), it was concluded that "the AC/CW ratio is an important independent contributor to inter-individual variation in BPM"(12). Furthermore, due to the common multi cardiovascular risk found in obese as well as diabetics and hypercholesterolemics, only obese subjects have been a source of concern in the hypertension and cardiology areas, resulting in important questions: How could the actual BP values be in children, adolescents, anorexics, top models and lean women? Which is the correct BP value in normal weighted subjects with thin arms?
In 1980, the use of the adult standard cuff to measure BP in adolescents was recommended, as emphasized(4). Our findings led us to state that this is an equivocal statement that can result in AC/CW ratio changes that can reach 0.50 or more in the leanest arm. This probably happened with the adolescents evaluated in the health units in 1982, when check up results led them to be diagnosed as "normal blood pressure status". Unfortunately, up to date, most hospital units do not follow the recommendations of pediatric societies and even a nine-cm cuff (adolescent cuff) is available only in some university hospitals or special areas.
Our findings suggest that the recommended AHA ratio is appropriate to avoid BP measurement errors. After 1951, when the ratio was proposed, attempts to solve cuff size problems led AHA to recommend cuffs 9, 12 and 15 cm in width (AHA 1980 guidelines)(4), supported by the demonstration of ratio 0.39 being the best one to avoid errors(14). It was the first national step in the USA to improve decisions towards the cuff phenomenon, but this recommendation was not understood. A table for corrections of errors was introduced in the following revision, in 1988(15). However, the interindividual variation found in BPM studies resulted in discrepant values and controversies(16-17), making the author of the first table declare the need for further studies(18). In Brazil, we observed an important variation among subjects, resulting in largely scattered data, strongly discouraging the use of tables to correct cuff size errors(19). The table introduced in 1988 was not kept; another AHA revision was published in 1993, recommending a ten-cm cuff for lean subjects(3). The next statement in 2005(5) not only suspended the use of such cuff, but also changed the ratio recommendation, raising it to 0.46. In view of the scientific community's reaction, the committee published a statement on the need for further studies(20), in response to a Letter to the Editor. Fortunately, a cuff for small persons was proposed in the most recent guidelines of the European Society of Hypertension(21).
The higher hypertension rates found in the RG in our study are in line with findings from adult subjects detected in the original USP sample(6). The evidence of cardiovascular and gestational complications after six-seven years following high-risk subjects led the authors to offer an explanation(22) for the higher mortality rates found in lean people living in the Middle East, in a study including more than 11000 subjects(23). The authors found an inverted correlation between Body Mass Index (BMI) and mortality in hypertensive subjects. We suggested that the long time without diagnosis (hypertension silent phase) due to cuff BP errors allows the disease to advance. Furthermore, after a hypertension diagnosis is established, lean persons may be mistreated due to BP underestimation, resulting in an uncontrolled situation. This also explains the favorable treatment in obese due to the overestimation of anti hypertensive drugs.
The gestational problems rates we found raise questions about blood pressure measurement during pregnancy. In the RG, one woman presented an episode of pre-eclampsia and one of eclampsia, losing two babies. After anti hypertensive treatment, she had two healthy babies. As demonstrated, the use of the standard cuff to evaluate pregnant women, many of them adolescents or young adult with lean arms, can result in BP underestimation(11), masking a pre-eclampsia diagnosis in its early stage, as observed in this study.
We did not expect to find cardiovascular death among the subjects in our young original sample. As described in the results, the application of the ratio 0.40 in 1982 permitted the detection of hypertensive values in a 10-year-old boy. But the use of the standard cuff in his cardiovascular evaluation underestimated BP readings and, in view of "normal BP readings", no other attempts to verify risk were made.
Limitations
Our sample is small and we have difficulties to discuss our data in view of the international literature because this is the first and only study employing AHA AC/CW ratio in children and adolescents. This methodological approach has been used during many years only by Brazilian nurses(24), focusing on several aspects of educational approaches to blood pressure measurement(25). The lack of data from other countries imposes a limitation to analyze the cuff size effect phenomena, an important factor that delays knowledge advancement on a phenomenon that has turned into one of the most controversial issues in hypertension diagnosis(9).
Perspectives
Our findings led to speculate as to whether, if a proper cuff had been used in clinical practice, the relevant complications found in the studied subjects could have been better addressed. The authors suggest two points to improve knowledge on the matter. The first is to identify AC in different countries around the world in addition to height, weight and waist circumference. The second is to conduct prospective studies in larger samples to observe the cuff width effect. We believe that, when using a cuff length encircling 100% AC, we can control for this variable and observe the real cuff width effect. The use of a large range of cuff widths may diminish the polemic surrounding controversial findings from experiments performed in different groups: lean, normal and obese subjects. The main reason for polemics and discrepancies in hypertension and cardiovascular studies, as well as of any associated variable, such as resistance to hypertension treatment, results from the lack of cuff size control and failure in applying the 0.40 ratio in BPM studies.
Conclusions
The application of the AHA CW/AC 0.40 ratio in our research protocol in 1982 enabled us to detect alarming BP levels in adolescents (Risk Group). Their families were advised regarding the need for a cardiovascular checkup, but the use of the standard cuff in health units resulted in "normal health status" on that occasion. Compared to those exhibiting normal BP values in 1982, we found significant differences (p=0.02) when analyzing the Risk and Control groups, for hypertension, gestational complications and cardiovascular death. The analysis of the AHA guidelines from 1951 to 2005 indicates discrepancies between the theoretical framework and the recommendation for cuff size to be used in the clinical practice. We speculate that, if a correct cuff had been used also in clinical practice in the Risk Group, the related problems could have been better addressed. We thus suggest compliance with the AHA CW/AC 0.40 ratio in clinical and research protocols, despite the polemic discussion regarding the cuff width or cuff length effects in the BP readings or other CW/AC.
References
- 1.O´Brien E. Review: a century of confusion: which bladder for accurate blood pressure measurement. J Human Hypertens. 1996;10:565–572. [PubMed] [Google Scholar]
- 2.Bordley J, III, Connor CAR, Hamilton WF, Kerr WJ, Wiggers CJ. Recommendations for human blood pressure determinations by sphygmomanometers. Circulation. 1951;4:503–509. doi: 10.1161/01.cir.4.4.503. [DOI] [PubMed] [Google Scholar]
- 3.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–2470. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 4.Kirkendall WM, Feinleib M, Freis ED, Mark AL. Recommendation for human blood pressure determination by sphygmomanometer. Circulation. 1980;62(5):1146A–1155A. [PubMed] [Google Scholar]
- 5.Pickering TG, Hall JE, Apple LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for Blood Pressure Measurement in Humans and Experimental Animals. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 6.Arcuri EAM. Estudo comparativo da medida de pressão arterial com manguito de largura correta e com manguito de largura padrão [tese de Doutorado] São Paulo (SP): Universidade de São Paulo; 1985. [Google Scholar]
- 7.European Society of Hypertension. Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al. Management of high blood pressure in children and adolescents. J Hypertens. 2009;27:1719–1742. doi: 10.1097/HJH.0b013e32832f4f6b. [DOI] [PubMed] [Google Scholar]
- 8.Feber J, Ahmed M. Hypertension in children: new trends and challenges. Clin Sci. 2010;119:151–161. doi: 10.1042/CS20090544. [DOI] [PubMed] [Google Scholar]
- 9.Arcuri EAM. Fatores de erro na medida da pressão arterial: a influência do manguito. Hipertensão. 2011;14(2):21–32. [Google Scholar]
- 10.Veiga EV, Arcuri EAM, Cloutier L, Santos JLF. Blood pressure measurement: arm circumference and cuff size availability. Rev. Latino-Am. Enfermagem. 2009;17(4):455–461. doi: 10.1590/s0104-11692009000400004. [DOI] [PubMed] [Google Scholar]
- 11.Oliveira SMJV, Arcuri EA, Santos JLF. Cuff width influence on blood pressure measurement during pregnant-puerperal cycle. J Adv Nurs. 2002;38(2):180–189. doi: 10.1046/j.1365-2648.2002.02162.x. [DOI] [PubMed] [Google Scholar]
- 12.Rastam L, Prineas RJ, Gomez-Marin 0. Ratio of cuff width/arm circumference as a determinant of arterial blood pressure measurements in adults. J Intern Med. 1990;227:225–232. doi: 10.1111/j.1365-2796.1990.tb00149.x. [DOI] [PubMed] [Google Scholar]
- 13.Graves JW. Prevalence of blood pressure cuff size in a referral practice of 430 adult hypertensives. Blood Pres Monit. 2001;6:17–20. doi: 10.1097/00126097-200102000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Geddes LA, Tivey R. The importance of cuff width in measurement of blood pressure indirectly. Cardiov Res Bull. 1976;14:69–78. [PubMed] [Google Scholar]
- 15.National High Blood Pressure Education Program (NHBPEP) National Heart, Lung, and Blood Institute (NHLBI) American Heart Association (AHA) Working Meeting on Blood Pressure Measurement: Recommendations for human blood pressure determination by sphygmomanometers. Circulation. 1980;62:1146A–1155A. [PubMed] [Google Scholar]
- 16.Ragan C, Bordley J., III The accuracy of clinical measurements of arterial blood pressure. Bull Johns Hopkins Hosp. 1941;69:504–528. [Google Scholar]
- 17.Holland WW, Humerfelt S. Measurements of blood pressure comparison of intra-arterial and cuff values. Br Med J. 1964;2:1241–1243. doi: 10.1136/bmj.2.5419.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pickering G. High blood pressure. 2nd ed. London: Churchill Livingtone; 1968. 717 p [Google Scholar]
- 19.Arcuri EAM, Santos JLF, Silva MR. Correct width cuff versus standard cuff: wide scattering imposes a limitations to the use of tables for correction of errors in indirect blood pressure determination. Braz J Med Biol Res. 1986;24(2):265–280. [Google Scholar]
- 20.Pickering TG, Hall JE, Apple LJ, Falkner BE, Graves J, Hill MN, et al. Response to Recommendations for blood pressure measurement in Humans and Experimental Animals. Hypertension. 2006;48:5–6. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 21. Guidelines for the Management of Arterial Hypertension The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J. Hypertens. 2007;25(6):1105–1187. doi: 10.1097/HJH.0b013e3281fc975a. [DOI] [PubMed] [Google Scholar]
- 22.Arcuri EAM, Santos JLF, Rocha e Silva M. Is early diagnosis of hypertension a function of cuff width? J Hypertens. 1989;7:S60–S61.1. doi: 10.1097/00004872-198900076-00026. [DOI] [PubMed] [Google Scholar]
- 23.Goulbourt U, Holtzman E, Cohen-Mandelzwieg L, Neufeld HN. Enhanced risk of coronary heart disease mortality in lean. Hypertension. 1987;10:22–28. doi: 10.1161/01.hyp.10.1.22. [DOI] [PubMed] [Google Scholar]
- 24.Arcuri EAM, Araújo TL, Veiga EV, Oliveira SMJV, Lamas JLT, Santos JLF. Pesquisa da medida da pressão no Brasil e a produção científica dos enfermeiros da área. Rev Esc Enferm USP. 2007;41(2):292–298. doi: 10.1590/s0080-62342007000200017. [DOI] [PubMed] [Google Scholar]
- 25.Alavarce DC, Pierin AMG. Elaboração de uma hipermídia educacional para o ensino do procedimento de medida da pressão arterial. Rev Esc Enferm USP. 2011;45:939–944. doi: 10.1590/s0080-62342011000400021. [DOI] [PubMed] [Google Scholar]