Abstract
Background
Spinal anesthesia (SA) is usually associated with hypotension in pregnant women. We sought to assess the influence of various maternal positions on SA-induced hypotension.
Material/Methods
The study population comprised 99 women at full-term gestation scheduled for elective cesarean section. They were randomized into 3 equal groups: the LL group, in which the patient was placed in the full left-lateral position until the start of surgery with the Whitacre needle bevel oriented laterally; the LS group, in which the patient was placed in the full left-lateral position initially and then shifted to the left-tilt supine position with the needle bevel oriented laterally; and the CS group, in which the patient was initially placed in the full left-lateral position and then shifted to the left-tilt supine position with the needle oriented in the cephalad direction.
Results
The incidences of hypotension in the LL, LS, and CS groups were 9.7%, 54.8%, and 56.3%, respectively. Ephedrine requirements were lower in the LL group than in the LS group (P<0.01).
Conclusions
The maternal position during the induction of anesthesia played an important role in the development of hypotension during cesarean delivery.
MeSH Keywords: Anesthesia, Obstetrical; Anesthetics; Cesarean Section
Background
Spinal anesthesia (SA) is generally accompanied by hypotension. Hypotensive episodes can cause maternal and fetal discomfort and even lead to the death of either, if prolonged [1]. In pregnant women, hypotension induced by SA occurs due to the cephalad spread of the local anesthetics in the subarachnoid space and/or the aortocaval compression caused by the gravid uterus [2]. Both these factors can be influenced by the parturients’ postures during and immediately after the subarachnoid injection [3–6]. A study by Mendonca et al. [4] on the effect of the parturients’ positions (left lateral versus tilted supine) during and after the induction of SA by the administration of hyperbaric bupivacaine revealed that hypotension was less frequent, and the requirement of the ephedrine dose lower, among mothers placed in the left lateral position than in those placed in the tilted supine position. However, in that study, the women were first placed in the right lateral position for 2 min after the induction of SA and then moved to the left lateral position and other positions. In other similar studies [3,5] on the role of the maternal positions, the mothers were repeatedly turned to avoid unilateral block when using hyperbaric bupivacaine. Therefore, to determine whether the intermediate step of placing the patient in the right lateral position could be omitted, we analyzed the effect of maternal positions on hemodynamic stability following SA during elective cesarean section (c- section).
Material and Methods
Study protocol
This was a single-center study, and the subjects were consecutive patients. The study protocol was approved by the Hospital Ethics Committee, and written informed consent was obtained from all the patients.
Patient selection
The study population comprised 99 women who were at full-term gestation, opted for elective cesarean delivery under combined spinal-epidural anesthesia (CSEA), and had American Society of Anesthesiologists (ASA) physical status of I or II. Women with neurological or psychiatric diseases, heart disease, pregnancy-induced hypertension, diabetes mellitus, multiple pregnancies, contraindications to regional blocked anesthesia, or baseline systolic blood pressure (BP) lower than 100 mmHg were excluded from the study. Patients were also excluded if they had a history of hypersensitivity to the study drugs. The patients were randomly assigned to the following 3 groups by the sealed-envelope technique: the LL group, in which CSEA was performed with the needle bevel oriented laterally and the patient in the full left-lateral position until the start of surgery; the LS group, in which CSEA was performed with the needle oriented laterally when the patient was initially placed in the full left-lateral position and then turned to the left-tilt supine position; and the CS group, in which CSEA was performed with the needle bevel oriented in the cephalad direction when the patient was initially in the full left-lateral position and then shifted to the left-tilt supine position.
CSEA procedures
All patients were maintained at the nil-per-os condition, as per the ASA standards, and did not receive any preoperative medications, except intravenous fluid adjusted according to the patient’s body weight. Standard monitoring devices were attached to the patient, and data obtained from electrocardiography, pulse oximetry, and non-invasive BP measurements were recorded. The baseline value of systolic BP was calculated as the mean of 3 recordings obtained from the left arm while the patient was in a resting state. The venous channels were opened before the induction of anesthesia; fluid balance was achieved by administration of 4 ml/kg WanWen infusion (hydroxyethyl starch 130/0.4 sodium chloride injection) and maintained with administration of 10 ml/(kg/h) crystalloid fluid.
The induction of CSEA in all the patients was performed by the attending physicians, by using the needle-through-needle CSEA technique. The skin on the operative area was disinfected by the application of 10% povidone-iodine with the patient placed in the lateral decubitus position. Intradermal injection of 1% lidocaine was administered, followed by penetration of the skin and superficial tissue by a 20-gauge introducer needle. The epidural space was identified at the L3–L4 level with an 18-gauge Tuohy needle. A midline approach with the standard technique of loss of resistance to saline was used. A 26-gauge Whitacre spinal needle was then inserted through the Tuohy needle. After free flow of cerebral spinal fluid (CSF) was obtained, hyperbaric ropivacaine (10 mg; Astra Zeneca Pharmaceuticals, Sweden) and sufentanil (5 μg; Yichang Humanwell Pharmaceutical Co., Ltd., China) were injected within 30 s. The 0.5% hyperbaric ropivacaine solution was prepared as a combination of 1 ml of 1% ropivacaine with 0.5 ml of sufentanil (10 μg/ml) and 0.5 ml of 10% dextrose. An epidural catheter was advanced up to a distance of 4 cm into the epidural space and fixed. The time point of administering the spinal injection was considered as the starting time point for all subsequent events. After the administration of the lateral injection, women in the LL group were maintained in the lateral decubitus position until the start of surgery, when they were shifted to the left-tilt supine position. In the LS group, the women were shifted to the left-tilt supine position immediately after the lateral injection. In the CS group, the injection was administered in the cephalad direction, after which the patients were immediately shifted to the left-tilt supine position.
Maternal BP was non-invasively measured at the forearm every 2 min after the administration of the intrathecal injection. Ephedrine (6 mg) was then administered intravenously if the patient developed hypotension. Hypotension was defined as a systolic BP of less than 100 mm Hg or a 20% drop from the baseline level. Decreases in the heart rate to less than 50 beats per min (bpm) were treated with incremental doses of intravenous atropine (0.25 mg). The level of sensory block, defined as the loss of pinprick sensation, was recorded bilaterally at the mid-clavicle line every 2 min. Surgery commenced after adequate sensory block was reached at the upper level of T6. If the block did not reach this level 20 min after the administration of the spinal injection, 5-ml increments of 2% lidocaine were administered through the epidural catheter every 5 min until adequate block height was achieved. The status of the newborn was assessed using Apgar scores obtained at 1 and 5 min after birth and values of umbilical cord blood gas.
Statistical analyses
The primary outcome in this study was a reduction in ephedrine requirement. On the basis of data obtained in previous studies, we calculated that the sample size necessary to detect an intergroup difference in the requirement of 10 mg ephedrine with a power of 90% and at a significance level of 5% was 30 patients per group. Accordingly, 99 parturients were recruited in all to account for potential dropouts.
The secondary outcomes analyzed were changes in the maternal BP, highest level of sensory block, fetal Apgar scores, umbilical arterial pH, and base excess (BE) values. Parametric data are presented as mean values ± standard deviation (SD) and non-parametric data as medians (range) and numbers (percentage), as appropriate. Analysis of variance tests followed by least standard deviation tests were used to compare the means for parametric data, and the Kruskal-Wallis test to compare group variability for non-parametric data and data with non-normal distributions. A P value of <0.05 was considered significant. All statistical analyses were performed using SAS 9.0® software (version 9.0; SAS Institute, USA).
Results
Complete data were obtained for 94 (LL group, 31; LS and CS groups, 32 each) of the 99 women. In the remaining cases (2 each in the LL and LS group and 1 in the CS group), technical difficulties were encountered during the induction of CSEA: failure to achieve free flow of CSF during the spinal injection in 4 patients and failure to identify the epidural space in 1.
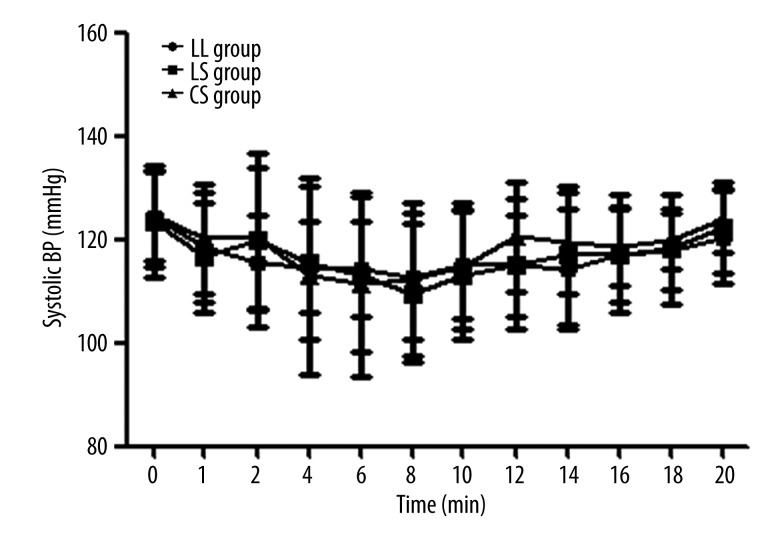
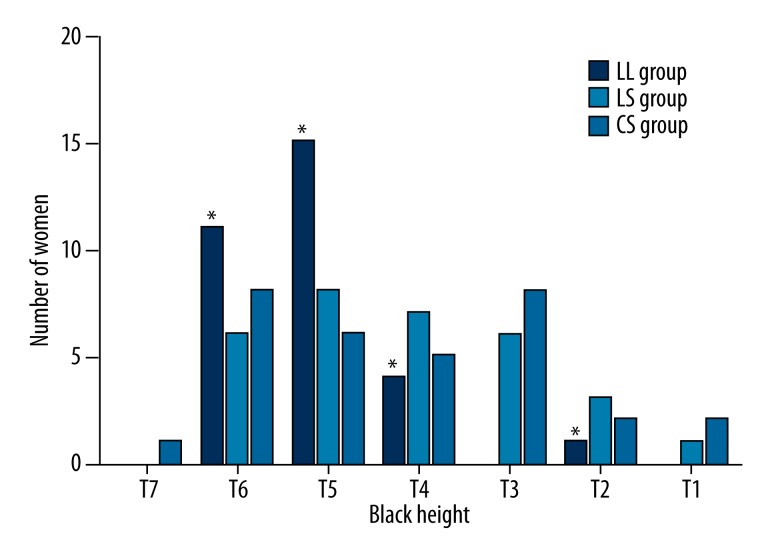
Maternal characteristics were similar in each group (Table 1). No intergroup difference was noted in the time to complete the intrathecal injection, with removal of the needle and fixation of the epidural catheter. However, the time required to reposition women was longer in the LL group compared with the LS group (P<0.05) (Table 2). Similarly, the 3 groups did not show any statistical difference in the time required to achieve T6 sensory block and the maximum height of the sensory block between the lower left and upper right sides of patients in the LL group (Table 3). Three women required epidural supplementation to achieve T6 sensory block. Although there were no significant intergroup differences in the levels of maternal systolic BP, the ephedrine requirements in the 3 groups varied (Figure 1). A significantly lower number of patients required ephedrine in the LL group (3 patients) than in the LS group and CS groups (17 and 18 patients, respectively; P<0.01). Sixteen women experienced nausea and 10 vomited during the study (Table 4). No significant difference was noted in the variability in the upper limit of the block height between the 2 supine groups (Figure 2). However, none of the patients in the LL group had a block height above T2, as assessed by the absence of sharp prick sensation, unlike the case with the LS group (P<0.05). Time to surgical incision and duration of surgery were similar in the 3 groups (Table 5). One patient in the LL group, 3 in the LS group, and 2 in the CS group required intra-operative epidural supplements for discomfort, which was primarily due to prolonged surgery with regression of block height. No significant intergroup differences were noted in the Apgar scores recorded for the newborns (Table 6). Umbilical artery blood gas analysis showed that the pH values were higher, and the base excess values lower, in the LL group than in the LS group (P<0.05).
Table 1.
Patient data (mean and standard deviation).
| LL group n=31 |
LS group n=31 |
CS group n=32 |
|
|---|---|---|---|
| Age (years) | 29.5 (3.3) | 29.1 (3.6) | 29.3 (3.8) |
| Height (cm) | 160.1 (3.1) | 160.7 (3.4) | 159.8 (3.1) |
| Weight (kg) | 68.6 (7.0) | 66.8 (6.0) | 66.7 (5.5) |
| Baseline systolic BP (mmHg) | 124.0 (9.4) | 123.0 (10.9) | 125.0 (8.6) |
No significant difference between groups.
Table 2.
Induction of combined spinal-epidural anesthesia (time in seconds from beginning of spinal injection, mean and standard deviation).
| LL group n=31 |
LS group n=31 |
CS group n=32 |
|
|---|---|---|---|
| Time to completion of intrathecal injection | 26.3 (2.5) | 26.7 (2.4) | 26.3 (2.9) |
| Time to needle removal | 69.7 (13.1) | 65.2 (9.1) | 70.8 (11.4) |
| Time to fixation of epidural catheter | 140.0 (12.0) | 136.1 (15.7) | 135.3 (15.7) |
| Time to reposition patient | 958.0 (13.5)* | 178.0 (14.7) | 174.0 (17.7) |
Compared with group LS, P<0.05.
Table 3.
Spinal block development in women placed in the left lateral position (median (range)).
| Left side (lower) | Right side (upper) | |
|---|---|---|
| Time to T6 block (min) | 8 (6–10) | 9 (6–10) |
| Maximum height of block | T5 (T2–T6) | T6 (T3–T6) |
No significant difference between groups.
Figure 1.
Changes in systolic blood pressure following intrathecal injection. No significant difference was noted between the 3 groups.
Table 4.
Complications associated with induction of combined spinal-epidural anesthesia.
| LL group n=31 |
LS group n=31 |
CS group n=32 |
|
|---|---|---|---|
| Incidence of hypotension | 3 (9.7%) | 17 (54.8%) | 18 (56.3%) |
| Ephedrine (mg) | |||
| Pre-delivery median (range) | 0 (0–6)* | 6 (0–24) | 6 (0–18) |
| Post-delivery median (range) | 0 (0–0)** | 0 (0–12) | 6 (0–12) |
| Nausea (n) | 2 | 8 | 6 |
| Vomiting (n) | 2 | 4 | 4 |
Compared with group LS, P<0.01.
Figure 2.
Maximum block height (assessed by loss of pinprick sensation). * compared with group LS, P<0.05.
Table 5.
Surgical timings (mean and standard deviation).
| LL group n=31 |
LS group n=31 |
CS group n=32 |
|
|---|---|---|---|
| Knife-to-skin to delivery (min) | 7.6 (1.1) | 7.9 (1.0) | 7.9 (1.2) |
| Uterine incision-delivery (min) | 3.0 (0.8) | 3.1 (1.1) | 3.1 (0.9) |
| Duration of surgery (min) | 38.4 (7.7) | 38.4 (8.7) | 38.3 (8.3) |
| Intra-operation supplementation (n) | 1 | 3 | 5 |
No significant difference between groups.
Table 6.
Neonatal data (mean and standard deviation).
| LL group n=31 |
LS group n=31 |
CS group n=32 |
|
|---|---|---|---|
| Apgar score | |||
| 1 min (median (range)) | 9.0 (8–10) | 9.0 (8–10) | 9.0 (8–10) |
| 5 min (median (range)) | 10.0 (10) | 10.0 (10) | 10.0 (10) |
| Umbilical artery pH | 7.33 (0.04)* | 7.29 (0.04) | 7.29 (0.04) |
| Umbilical artery base excess | −1.72 (1.35)** | −2.67 (1.74) | −2.91 (1.36) |
Compared with group LS, P<0.05.
Discussion
Hypotension is a common complication of SA. The maternal supine position can cause several pressure-related symptoms, such as hypotension due to the compression of the inferior vena cava by the uterus, particularly in the second and/or the third trimester of the pregnancy [7]. A study on parturient women showed that the intra-abdominal pressure was significantly lower when mothers were in the left-lateral tilt position than in the supine position (10.9±4.67 mm Hg vs. 8.9±4.87 mm Hg, P=0.0004) [8]. In the lateral position, the uterus may shift away from the aorta and inferior vena cava, thereby releasing the aortocaval compression. Theoretically, the intrathecal spread of the hyperbaric local anesthetic drug injected in the cephalad direction may follow the principles of gravity [9]. Therefore, it might be anticipated that induction of SA by the injection of the hyperbaric local anesthetic agent may generate a significant unilateral block when the mother is in the full left lateral position; this is presumably why Mendoca et al. changed the position of the patients from side to side [4]. However, Cui et al. found that the injection of the hyperbaric local anesthetic with the needle bevel oriented laterally resulted in a more symmetric block between the left (lower) and right (upper) sides when the patient was placed in the full left lateral position [10]; consistent with their findings, ours showed that unilateral block did not occur in the LL group. Although the reason for this finding is not immediately apparent, it may be related to the fluid dynamics of the hyperbaric local anesthetic agent as it enters in the CSF circulation; further investigation is necessary to clarify this.
Under normal conditions, hypotension caused by a reduction in systemic vascular resistance is compensated by an increase in cardiac output. However, under SA, this compensation is attenuated by an increase in the venous capacitance because of the venous dilatation in the lower parts of the body. This further complicates the aortocaval compression in mothers under SA for c-section delivery. Finally, instead of the compensatory increase, the cardiac output of the mother is usually decreased [11]. Thus, the combination of reduced cardiac output and decreased systemic vascular resistance results in maternal hypotension after the induction of the SA.
The incidence of the hypotension after SA is as high as 80% [5], and the severity of the hypotension usually depends on the height of the block, the position of the parturient, and the prophylactic measures taken against hypotension. Mendonca et al. have shown that hypotension was less frequent among mothers placed in the left lateral position (64%) than among those placed in the tilted supine position (90%) and that mothers in the left lateral position had lower ephedrine requirement before repositioning for surgery [4]. Similarly, Lewis et al. reported that the incidence of hypotension was 64% in the lateral group and 78.6% in the tilted supine group [12]. In their study, although the frequency of hypotension and overall ephedrine requirement did not differ significantly between the 2 groups, it is noteworthy that the tilted supine group tended to show a higher incidence of hypotension and nausea with or without vomiting. Our experiment did not specially study the incidence of nausea and vomiting, but Matthias et al. reported that a prophylactic medication with tropisetron 2 mg and metoclopramide 20 mg is a highly efficient method for preventing nausea and vomiting during c-section [13]. The lower incidence in hypotension in their study might also be explained by the use of a smaller dose of bupivacaine. Consistent with these studies, ours showed that the incidence of hypotension was lower in the LL group with the lateral position (3 (9.7%) than in the 2 groups with the tilted supine position, i.e., the LS and CS groups (17 [54.8%] and 18 [56.3%], respectively). Although there were no significant differences in mean systolic BP between the groups (Figure 1), ephedrine requirements varied, with those in LL group requiring significantly less ephedrine than those in the LS group (P<0.01). In their study, Rees et al. considered a decrease in BP as the primary outcome measure and could not show a major intergroup difference; however, when they changed their primary outcome to use of ephedrine, they were able to demonstrate improved hemodynamic stability in the lateral group [14]. Considering these results, we believe that the maternal hemodynamic stability in the LL group may have been improved.
Our findings seem to indicate that our positioning sequences might further reduce ephedrine requirements and thereby preclude the need for the change to the right lateral position, which requires manpower and also entails possible risks to the staff and the mother [4]. Furthermore, the preferred maternal posture for CSEA varies among anesthetists, and lack of familiarity with certain maternal positions might influence their performance.
Uterine blood flow is pressure-dependent because there is no auto-regulation mechanism on the placental bed. Additionally, prolonged maternal hypotension is harmful to the fetus, and it is also frequently associated with nausea and vomiting for the mother. Brief episodes of maternal hypotension may also result in lower Apgar scores and fetal acidosis [15]. This is possibly due to the reduction in the uteroplacental blood flow occurring during the block while the patient is maintained in the supine position after the induction of the SA [14]. In addition, Apgar scores are considered poor predictors of outcome, which might be the reason for their exclusion in other reports [4,5]. Standard BE values have more recently been identified as better surrogate markers than pH for predicting the significance of the neonatal morbidity [16]. We found no significant intergroup differences in the fetal Apgar scores at 1 and 5 min; however, umbilical artery blood gas analysis showed that the pH values were slightly higher, and the BE values were lower, in the LL group than in the LS groups (P<0.05).
At present, the management of hypotension during SA in obstetrics remains controversial. Although fluid preload, pushing the uterus to the left side, and use of vasopressor, may often be employed in an attempt to prevent this complication, the incidence of SA-induced hypotension may not effectively decrease with these measures alone. Our approach of directing the bevel of the Whitacre needle laterally and maintaining the patient in the full left lateral position until the start of surgery provided satisfactory blockade for surgery and good hemodynamic stability. However, further research is necessary to elucidate the mechanism by which hyperbaric local anesthetics interact with the CSF in order to develop optimal therapeutic strategies for hypotension in high-risk parturient women. Hypotension is also a common complication of patients with hypertension disorders undergoing SA during c-section. Krzysztof et al. reported that IFN-γ and leptin might be risk markers of c-section in patients with hypertension disorders. Further studies are needed to provide evidence to define the complicated mechanisms of such high-risk disorders in parturient women [17].
Our study has a few limitations. The time taken to reposition the women in the LL group was longer than that required in the other 2 groups because the left lateral position was maintained until the start of the surgery in the LL group. However, this negative effects of this delay may be more than offset by the better hemodynamic stability achieved in the left lateral position and the possible benefits of the position for the fetus.
Conclusions
Our study shows that maternal position during the induction of anesthesia influences the development of hypotension during cesarean delivery. On the basis of our findings, for satisfactory nerve block and good hemodynamic stability, we recommend directing the bevel of the Whitacre needle laterally and maintaining the patient in the full left-lateral position until the start of the surgery.
Footnotes
Conflict of interests
All authors declare that they have no conflict of interests.
Source of support: Departmental sources
References
- 1.De-Giorgio F, Grassi VM, Vetrugno G, et al. Supine hypotensive syndrome as the probable cause of both maternal and fetal death. J Forensic Sci. 2012;57:1646–49. doi: 10.1111/j.1556-4029.2012.02165.x. [DOI] [PubMed] [Google Scholar]
- 2.Eckstein KL, Marx GF. Aortocaval compression and uterine displacement. Anesthesiology. 1974;40:92–96. doi: 10.1097/00000542-197401000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Russell R, Popat M, Richards E, Burry J. Combined spinal epidural anaesthesia for caesarean section: a randomised comparison of Oxford, lateral and sitting positions. Int J Obstet Anesth. 2002;11:190–95. doi: 10.1054/ijoa.2002.0964. [DOI] [PubMed] [Google Scholar]
- 4.Mendonca C, Griffiths J, Ateleanu B, Collis RE. Hypotension following combined spinal-epidural anaesthesia for Caesarean section. Left lateral position vs. tilted supine position. Anaesthesia. 2003;58:428–31. doi: 10.1046/j.1365-2044.2003.03090.x. [DOI] [PubMed] [Google Scholar]
- 5.Hallworth SP, Fernando R, Columb MO, Stocks GM. The effect of posture and baricity on the spread of intrathecal bupivacaine for elective cesarean delivery. Anesth Analg. 2005;100:1159–65. doi: 10.1213/01.ANE.0000149548.88029.A2. [DOI] [PubMed] [Google Scholar]
- 6.Paech MJ. Should we take a different angle in managing pregnant women at delivery? Attempting to avoid the ‘supine hypotensive syndrome’. Anaesth Intensive Care. 2008;36:775–77. doi: 10.1177/0310057X0803600603. [DOI] [PubMed] [Google Scholar]
- 7.Lanni SM, Tillinghast J, Silver HM. Hemodynamic changes and baroreflex gain in the supine hypotensive syndrome. Am J Obstet Gynecol. 2002;187:1636–41. doi: 10.1067/mob.2002.127304. [DOI] [PubMed] [Google Scholar]
- 8.Chun R, Baghirzada L, Tiruta C, Kirkpatrick AW. Measurement of intra-abdominal pressure in term pregnancy: a pilot study. Int J Obstet Anesth. 2012;21:135–39. doi: 10.1016/j.ijoa.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Birnbach DJ, Datta S, Gatt SP. Textbook of obstetric anesthesia. Churchill Livingstone; 2000. [Google Scholar]
- 10.Cui Y, Xu J, Jiang X, et al. Lateral injection using a Whitacre needle with patients in the lateral decubitus position maintained for a prolonged time period produces symmetric sensory block. Anesth Analg. 2012;115:973–76. doi: 10.1213/ANE.0b013e3182536f3a. [DOI] [PubMed] [Google Scholar]
- 11.Thomas DG, Robson SC, Redfern N, et al. Randomized trial of bolus phenylephrine or ephedrine for maintenance of arterial pressure during spinal anaesthesia for Caesarean section. Br J Anaesth. 1996;76:61–65. doi: 10.1093/bja/76.1.61. [DOI] [PubMed] [Google Scholar]
- 12.Lewis NL, Ritchie EL, Downer JP, Nel MR. Left lateral vs. supine, wedged position for development of block after combined spinal-epidural anaesthesia for Caesarean section. Anaesthesia. 2004;59:894–98. doi: 10.1111/j.1365-2044.2004.03752.x. [DOI] [PubMed] [Google Scholar]
- 13.Voigt M, Frohlich CW, Huttel C, et al. Prophylaxis of intra- and postoperative nausea and vomiting in patients during cesarean section in spinal anesthesia. Med Sci Monit. 2013;19:993–1000. doi: 10.12659/MSM.889597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rees SG, Thurlow JA, Gardner IC, et al. Maternal cardiovascular consequences of positioning after spinal anaesthesia for Caesarean section: left 15 degree table tilt vs. left lateral. Anaesthesia. 2002;57:15–20. doi: 10.1046/j.1365-2044.2002.02325.x. [DOI] [PubMed] [Google Scholar]
- 15.Reynolds F, Seed PT. Anaesthesia for Caesarean section and neonatal acid-base status: a meta-analysis. Anaesthesia. 2005;60:636–53. doi: 10.1111/j.1365-2044.2005.04223.x. [DOI] [PubMed] [Google Scholar]
- 16.Backe SK, Lyons G. Oxygen and elective caesarean section. Br J Anaesth. 2002;88:4–5. doi: 10.1093/bja/88.1.4. [DOI] [PubMed] [Google Scholar]
- 17.Rytlewski K, Huras H, Kusmierska-Urban K, et al. Leptin and interferon-gamma as possible predictors of cesarean section among women with hypertensive disorders of pregnancy. Med Sci Monit. 2012;18(8):CR506–11. doi: 10.12659/MSM.883271. [DOI] [PMC free article] [PubMed] [Google Scholar]