Abstract
Young, Black men who have sex with men and transgender women who have sex with men (YBMSM/TW) are at disproportionate risk for HIV and other sexually transmitted infections (HIV/STI). HealthMpowerment.org (HMP) is a mobile phone optimised online intervention that utilises behaviour change and gaming theories to reduce risky sexual behaviours and build community among HIV-positive and negative YBMSM/TW. The intervention is user-driven, provides social support, and utilises a point reward system. A four-week pilot trial was conducted with a diverse group of 15 YBMSM/TW. During exit interviews, participants described how HMP components led to behaviour changes such as asking partners' sexual history, increased condom use, and HIV/STI testing. The user-driven structure, interactivity, and rewards appeared to facilitate sustained user engagement and the mobile platform provided relevant information in real-time. Participants described the reward elements of exceeding their previous scores and earning points toward prizes as highly motivating. HMP showed promise for being able to deliver a sufficient intervention dose and we found a trend toward higher dose received and more advanced stages of behaviour change. In this pilot trial, HMP was well accepted and demonstrates promise for translating virtual intervention engagement into actual behaviour change to reduce HIV risk behaviours.
Keywords: Men who have sex with men, MSM, transgender, HIV, eHealth, mHealth, mobile, intervention, sexual behavior
Introduction
Within the United States (US), young, Black men who have sex with men (YBMSM) and transgender women (TW) who have sex with men face a disproportionate burden of HIV infection (Baral et al., 2013; Herbst et al., 2008; Johnson et al., 2013; Oster et al., 2013; Wejnert et al., 2013). Compared to older and non-Black MSM, YBMSM are less likely to know their HIV status and receive optimal HIV care (Millett et al., 2012; Oster et al., 2011; US Centers for Disease Control, 2010). Structural-level interventions are needed alongside supported individual behaviour-change to reduce transmission and improve care for HIV and STI among YBMSM/TW. A few individual-level interventions for Black MSM have demonstrated reductions in unprotected anal intercourse (UAI) and increased HIV/STI testing (Maulsby et al., 2013). However, in-person delivery and sustained behaviour change demand significant resources, limiting intervention scalability and impact.
High ownership of computers and mobile devices among YBMSM provides a cost-effective, familiar platform to deliver tailored internet- and mobile web-based (electronic health, or eHealth) interventions to improve HIV prevention and care (Community Marketing Inc., 2012). YBMSM's widespread use of online social and sexual networking tools (Duggan & Smith, 2014) suggests that eHealth interventions that utilise social networking and other engaging strategies such as gamification have a greater chance of adoption and sustainability (Gay, Pollak, Adams, & Leonard, 2011; Gustafson et al., 1999). Virtual communities can act platforms through which to implement eHealth interventions by connecting like-peers who can share their experiences, exchange information, and provide mutual counselling, support, and encouragement (Meier, Lyons, Frydman, Forlenza, & Rimer, 2007; J. J. Prochaska, Pechmann, Kim, & Leonhardt, 2012).
Past internet-based interventions for MSM have shown preliminary success in increasing condom use (Carpenter, Stoner, Mikko, Dhanak, & Parsons, 2010; Chiasson, Shaw, Humberston, Hirshfield, & Hartel, 2009; Ko et al., 2013; Miranda, 2013; Rosser et al., 2010) and HIV testing (Ko et al., 2013; Rhodes et al., 2011; Blass et al., 2010; Chiasson et al., 2009). Numerous eHealth intervention components can support sustained engagement and behavior change including: tailoring and user-focus (Lustria, Cortese, Noar, & Glueckauf, 2009; Lustria et al, 2013), user engagement features such as gamification (Baranowski, Buday, Thompson, & Baranowski, 2008; Brox, Fernandez-Luque, & Tollefsen, 2011; Enah, Moneyham, Vance, & Childs, 2013; Primack, 2012), social networking and support (Gay et al., 2011; Gustafson et al., 1999), and access via mobile devices (Gay et al., 2011; Gabarron, Serrano, Wynn, & Armayones, 2012). Our goal was to incorporate all of these promising features in an HIV/STI eHealth intervention explicitly tailored for YBMSM/TW.
HealthMpowerment.org intervention
HealthMpowerment.org (HMP) (Figure 1) is a multi-feature eHealth intervention to reduce risky sexual behaviours, promote health and wellness, and support community-building among YBMSM/TW (Hightow-Weidman et al., 2012; LeGrand, Muessig, Pike, Baltierra, & Hightow-Weidman, 2014; Muessig et al., 2013). We developed HMP through consecutive rounds of evaluation among 130 YBMSM/TW. The website is user-driven and employs responsive web design to optimise computer and smartphone access.
Figure 1. Screen shot of the HMP.org intervention home screen.
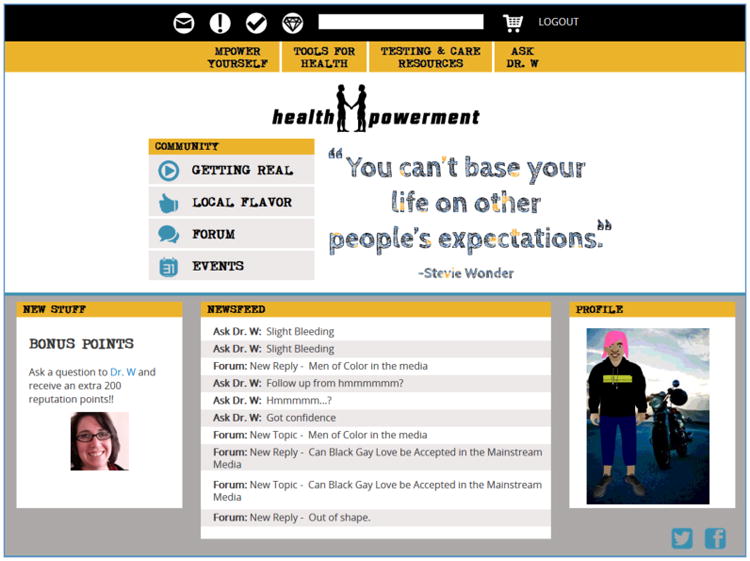
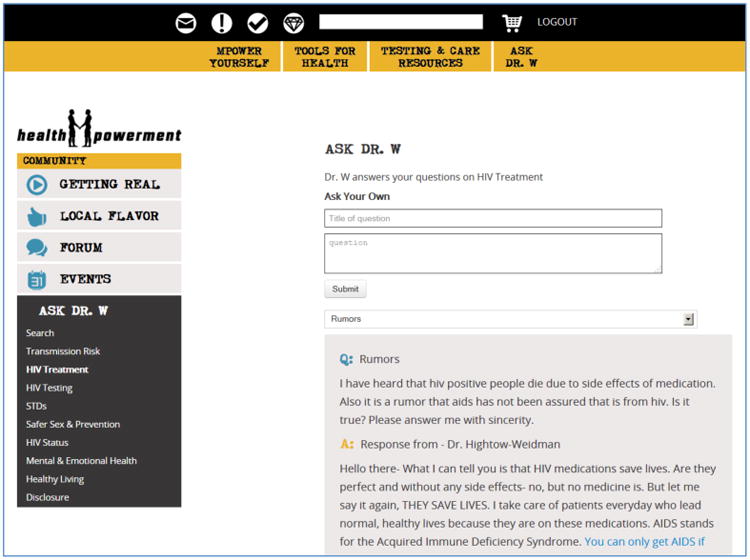
Through HMP's user-driven design, participants choose when and how to engage with the intervention. Each user creates a profile and an avatar to allow personalisation with anonymity. Information on HMP covers a range of health and lifestyle topics (Table 1) to support users' diverse backgrounds and varying need over time. For example, HMP includes resources and support forums for those: never tested for HIV (Figure 2), recently diagnosed HIV-positive, starting antiretroviral medications (ART), and already on ART for a number of years. Health and HIV/STI information is provided through multiple site features including: Quizzes, Know Your Risk (behavioural risk assessments), Ask Dr. W (Figure 3), The Scene (choose-your-own adventure decisional balance game) and the House of Mpowerment (library of brief educational articles and videos) (Table 1). Participants can explore areas of interest and then use the forums, Ask Dr. W, and external resource links to gather additional information and feedback from other users.
Table 1. Components of the healthMpowerment intervention website.
| Site section | Intervention user activities | Intended outcomes |
|---|---|---|
| House of Mpowerment | Read articles (HIV/STI, health) |
|
| Ask Dr. W (Figure 3) | Post anonymous health questions for HMP doctor who responds |
|
| Judge Your Skills | Complete health knowledge quizzes |
|
| Know Your Risk | Complete HIV/STI risk assessment profiles |
|
| My Life, My Goals | Set steps to achieve health goals and receive links to support resources (e.g. tobacco quit lines) |
|
| The Scene | Make behaviour decisions to navigate a choose-your-own adventure game for real-life scenarios. |
|
| Journal | Complete entries in private journal sections (medical history, sexual partners, free text) |
|
| Get Tested | Use GPS locator for HIV/STI testing and care resources |
|
| HMP Store (Figure 2) | Earn points by using HMP to “purchase” prizes (e.g. condom wallet, HMP tshirt), order free HIV/STD test kits |
|
| Local Flavour | Read and post reviews of local businesses and health services |
|
| Events | Read and post events to the community calendar application |
|
| Getting Real | View, create and share multi-media submissions (e.g. poetry, videos, photos)on relevant health and life issues |
|
| Forum | Post and comment to message boards for health and life topics and advice |
|
Figure 2. Screen shot of the HMP.org “Store” and available prizes.
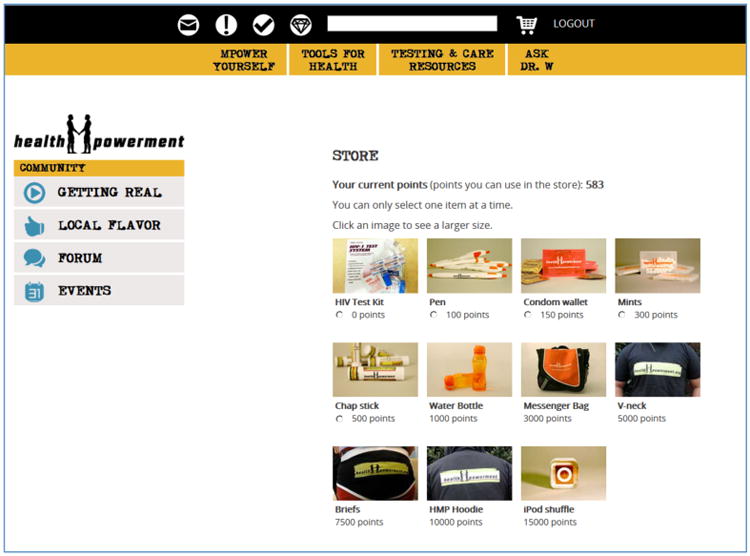
Figure 3. Screen shot of the HMP.org intervention “Ask Dr. W” health care provider forum.
To encourage continued use, participants earn points for completing actions on HMP (e.g. submitting an event to the activities calendar, 5 points; achieving perfect scores on all the health quizzes, 100 points). Points “level-up” users' status within the site (“new face”, “statement”, “star” and “legend”) and earn prizes from the HMP store (e.g. water bottle, messenger bag, hoodie sweatshirt, condom wallet, Figure 2).
Prior to HMP's full randomised controlled trial, we conducted a four-week pilot trial. In this manuscript we demonstrate how HMP components led to changes during the pilot trial in participants' health behaviour intentions and actions across the spectrum of the Stages of Change (J. O. Prochaska & DiClemente, 1992; J. O. Prochaska, Redding, Harlow, Rossi, & Velicer, 1994). We describe features of HMP that provided actionable health information for participants and facilitated sustained intervention engagement.
Methods
Participants
Study methods and quantitative survey outcomes are reported elsewhere (Hightow-Weidman et al., under review). In brief, study announcements were posted in diverse settings in the North Carolina Research Triangle area and online. Inclusion criteria were: born biologically male, age 18 to 30, self-identify as Black or African American, report ever having sex with another man, and reside in North Carolina.
Procedures
At the baseline office visit, participants completed a computer-assisted, multi-domain survey (sexual behaviours, condom attitudes, HIV/STI test history, depression/anxiety, stigma experiences) and a hands-on, guided HMP.org tutorial during which they created a user log-on name and password. Participants were instructed to use the HMP site for at least one hour per week for four weeks. As there are currently no best practice guidelines for type or length of dose for internet-based interventions (Donkin et al., 2013; Lustria et al., 2009; Lustria et al., 2013) one hour per week was selected as a minimum desired dose to be comparable in length to a weekly in-person one-on-one or group counselling session. The user-driven design of HMP.org allows participants to selectively use site features most relevant and timely to them without regard for the length of time it takes to complete a particular activity. For example the length of time required to locate an HIV test clinic, complete a risk assessment, and contribute to a discussion forum might vary, but these activities could all be of equal importance in the behaviour change process of different (or the same) users. Text message reminders were sent to participants who did not log-on to the site at least once per week.
At the end of the four week trial, a second in-person follow-up visit included a repeat of the baseline survey with added website usability questions and a semi-structured qualitative interview exploring users' evaluation of HMP. During the exit interview study staff loaded HMP.org on a computer. Participants navigated through the site while commenting on each section including their use (or non-use) during the field trial, impressions, and assessments. All participants were asked to discuss how their use of the site changed over the four weeks and whether anything in their life changed as a result of using the site. Qualitative interviews lasted between 30 and 70 minutes and were recorded with participants' consent. The analysis in this manuscript focuses on this qualitative interview data.
Theoretical framework
This analysis applies the Stages of Change behavioural theory as a conceptual framework and organisational tool to accommodate the diversity in HMP's intervention components and to identify pathways and mechanisms through which HMP may affect participants' behaviour change processes. In the Stages of Change theory, also referred to as the transtheoretical model, an individual moves through five stages of behavioural change (precontemplation, contemplation, preparation, action, and maintenance, Table 2) from being unaware and having no intention to change, to ultimately maintaining long-term change in a desired behaviour (J. O. Prochaska & DiClemente, 1992). At each stage there are hypothesised mechanisms, processes, and cues to action that encourage movement toward the subsequent stage (J. O. Prochaska et al., 1994). This theory has been applied extensively to study condom use behaviours (Ferrer et al., 2009; Grossman et al., 2008; Gullette & Turner, 2004; Noar, Crosby, Benac, Snow, & Troutman, 2011; Prat, Planes, Gras, & Sullman, 2012; Tung, Lu, & Cook, 2010) and, less so, HIV medication adherence behaviours (Genberg, Lee, Rogers, Willey, & Wilson, 2013; Willey et al., 2000). While the Stages of Change theory is often portrayed linearly, individuals may cycle through stages multiple times during the behaviour change process (Chang et al., 2006).
Table 2. Stages of Change addressed by healthMpowerment components.
| Stage | Definition | HMP components | Example user statements |
|---|---|---|---|
| Precontemplation | Does not perform behaviour. No intention to change | House of Mpowerment; Know Your Risk; Forum | I didn't really know what I was looking for until I happened to stumble upon it1 |
| Contemplation | Thinking about adopting the behaviour | House of Mpowerment; Know Your Risk; Forums; Judge Your Skills; Ask Dr. W | That's what I would go on a website for, see what people are talking about…if I could benefit from anything. Made me want to post… questions2 |
| Preparation | Plans to perform the behaviour, may try out the behaviour but does not do it consistently | House of Mpowerment; Ask Dr. W; Forum; My Life, My Goals; The Scene; Journal | [The site] has gotten me to…go outside of my comfort zone. This gave me a stepping stone…I'm able to socialise a little bit more!3 |
| Action | Consistently performing the behaviour (<6 months) | Ask Dr. W; Journal; My Life, My Goals; Get Tested; Forums; Point system | My whole attitude about condom use changed… [condoms are] one of the big things I'm working on now4 |
| Maintenance | Persisted in performing the behaviour consistently (> 6 months) | Journal; Get Tested; Point system; Forum; Local Flavor; Events | [The Forum] related to me…to see people reaching out for help…I've been through it too, and that's where I will give advice.5 |
HMP13, HIV-positive, age 29;
HMP06, HIV-positive, age 23, TW;
HMP08, HIV-positive, age 27;
HMP04, HIV-negative, age 29;
HMP07, HIV-negative, age 23.
Analysis
Interview recordings were professionally transcribed (© 2014 Verbal Ink) and entered into ATLAS. ti for analysis (qualitative data analysis software, Version 7, Berlin 2011). Three study team members reviewed all transcripts and developed a coding scheme. The code book was designed to capture all examples of health behaviours/actions and behavioural intentions that a participant related to their use of HMP during the four-week pilot trial, components of HMP mentioned, and the participant's reflections on the outcomes of their actions. Codes were inclusive of all health areas discussed (e.g. diet, exercise, smoking, sexual health). Each coded behaviour/intention was assigned one or more stage(s) of change as summarised in Table 2 and informed by the context of the participant's interview. For example, for the health behaviour change outcome of “establishing regular HIV testing”, an instance of talking about wanting to get a HIV test based on an article read on HMP was categorised as “Contemplation”, while an instance of describing an actual plan for getting an HIV test (e.g. clinic identified, appointment scheduled) was categorised as “Preparation”. Coders referenced participants' quantitative survey data for additional information about behaviours reported during the interview.
Two team members independently coded all interview transcripts within ATLAS.ti. Discrepancies were reviewed by a third team member and resolved by group consensus. Coded text and participants' demographic information (e.g. age, education, HIV status) were used to generate matrices in Microsoft Excel to facilitate grouping and comparing behaviours, participants, HMP intervention usage, and stages of behavioural change.
Detailed analysis of the intervention site usage measurement and patterns is reported elsewhere (Baltierra et al., 2014). In brief, participant activity on the website was tracked through a secure administrative portal. Built-in site tracking included time stamps for each user's activity on the site and automated log-out which occurred after 10 minutes of inactivity. Usage data was validated against aggregate statistics from Google Analytics reports and each participant was assigned a usage category based on total time spent on the site during the trial (low=less than one hour; medium=one to five hours; high=more than five hours). Participants' usage categories were also checked against their total points earned on HMP. As expected, these measures were correlated: those who were high users had the highest total points, while low users had the lowest total points. The usage categories were applied in this qualitative analysis to explore patterns between intervention usage and stages of behavioural change.
Results
Sociodemographic characteristics
Table 3 presents the sample's sociodemographic characteristics. Participants ranged in age from 20 to 30 years old. Six participants were HIV-negative and nine were HIV-positive. Participants were asked their: biological sex at birth (required “male” for study inclusion), current gender identity, and current sexual identity (Table 3). While these categories include some overlap (e.g. a transgender person may also identify as gay or bisexual), participants were asked to select the category that “best” describes them and allowed unlimited space for write-in options if they preferred to state their gender or sexual identity in their own words. Six men described their sexual identity as gay, four as bisexual, one as transgender, and four wrote-in a description (queer, same sex loving, MSM, agnostic). Six out of 15 men earned under $11,000 annually and 12 had greater than high school education.
Table 3. Sociodemographic characteristics of 15 HMP.org field trial participants.
| Continuous Variables | Mean | [SD] |
|---|---|---|
| Age in years | 26.1 | [3.3] |
|
| ||
| Categorical Variables | N | (%) |
|
| ||
| Education | ||
| High school or GED | 3 | (20.0) |
| Professional, technical or trade school | 1 | (6.7) |
| Some college | 8 | (53.3) |
| College degree | 2 | (13.3) |
| More than a college degree | 1 | (6.7) |
|
| ||
| Currently employed | 9 | (60.0) |
|
| ||
| Income last year | ||
| Less than $10,999 | 6 | (40.0) |
| 11,000-20,999 | 7 | (46.7) |
| 21,000-30,999 | 2 | (13.3) |
|
| ||
| What gender currently best describes you?1 | ||
| Man | 10 | (66.7) |
| Woman | 0 | (0.00) |
| Transitioning | 1 | (6.7) |
| Undecided | 1 | (6.7) |
| Not reported | 3 | (20.0) |
|
| ||
| How do you best describe your sexual identity?1 | ||
| Gay | 6 | (40.0) |
| Bisexual | 4 | (26.7) |
| Transgender | 1 | (6.7) |
| Write-ins: queer, same gender loving, MSM, agnostic | 4 | (26.7) |
|
| ||
| HIV Status | ||
| Positive | 9 | (60.0) |
| Negative | 6 | (40.0) |
Gender identity and sexual identity questions were asked separately with the categorical choices listed above and a write-in option. No participant wrote-in an option for the gender identity question, while four participants wrote-in an option for the sexual identity question.
HMP usage
Our field trial had 100% four-week retention: all 15 participants completed baseline and follow-up surveys and qualitative interviews. Two of the 15 participants did not log on to the site during the four-week trial. Among the remaining 13 active HMP users, average total time spent on the site was five hours and three minutes (range: 0.5 – 13.3 hours). Among the two participants who did not use the site during the trial, the first reported difficulty logging in and the second explained that they were too busy. However, both participants completed the guided tours of the site at baseline and four-week exit interview (described above). Thus, all 15 participants were exposed to HMP enough to comment on its design, desirability, and usefulness.
Analysis of participants' usage of HMP and stages of change revealed specific patterns (Table 4). First, participants who were categorised as “high” users were more likely to describe behaviours across all the stages of behavioural change. Second, across all stages, low users were most proportionally represented in the Contemplation stage, while medium users were most proportionally represented in the Preparation stage and high users were most proportionally represented in the Action stage. Third, the Action and Maintenance stages were the least commonly represented overall, while the Contemplation stage was the most commonly represented.
Table 4. healthMpowerment intervention usage and Stages of Change.
| User ID | Usage category | Stage of change | ||||
|---|---|---|---|---|---|---|
| Precontemplation | Contemplation | Preparation | Action | Maintenance | ||
|
| ||||||
| 1 | Low | √ | √ | √ | ||
| 5 | Low | √ | √ | √ | ||
| 9 | Low | √ | √ | √ | ||
| 10 | Low | √ | ||||
|
| ||||||
| 2 | Medium | √ | √ | √ | √ | |
| 3 | Medium | √ | √ | √ | √ | √ |
| 6 | Medium | √ | √ | √ | √ | |
| 13 | Medium | √ | √ | √ | √ | |
| 14 | Medium | √ | √ | |||
| 15 | Medium | √ | √ | |||
|
| ||||||
| 4 | High | √ | √ | √ | √ | √ |
| 7 | High | √ | √ | √ | √ | √ |
| 8 | High | √ | √ | √ | √ | √ |
| 11 | High | √ | √ | √ | √ | |
| 12 | High | √ | √ | √ | √ | √ |
|
| ||||||
| Overall %(n) | 80%(12/15) | 93%(14/15) | 73%(11/15) | 53%(8/15) | 67%(10/15) | |
|
| ||||||
| Low | 17% (2/12) | 29% (4/14) | 9% (1/11) | 13% (1/8) | 20% (2/10) | |
| Medium | 42% (5/12) | 36% (5/14) | 45% (5/11) | 25% (2/8) | 40% (4/10) | |
| High | 42% (5/12) | 36% (5/14) | 45% (5/11) | 63% (5/8) | 40% (4/10) | |
Behaviour change
Based on participants' feedback, the user-driven structure, interactive components, and point reward system of HMP allowed participants to explore information of greatest interest to them, compete against themselves, and engage with other users and study staff around a number of HIV-related topics such as coping with diagnosis, dealing with discrimination and stigma, managing medications, and navigating sexual relationships. This engagement with the intervention components took various forms including receiving and providing advice, debating user-generated topics (e.g. disclosing HIV status to a new partner), providing affirmation, and sharing experiences.
As described in the exit interviews, participants connected their online engagement with HMP features to real-world actions and behaviour changes completed during the four-week trial. Some of the actions we describe in this manuscript are primary intervention target outcomes (e.g. reducing unprotected anal intercourse) while other actions are secondary outcomes (e.g. increasing HIV/STI testing) or intermediate changes in behaviour (e.g. increasing awareness about triggers of risk behaviours) along the pathway to the primary behaviour change outcome.
The intentions/actions/behaviours described by participants ranged across all phases of the Stages of Change (precontemplation, contemplation, preparation, action, maintenance) including, for example: changing attitudes about HIV testing, increasing awareness about triggers of risk behaviours (e.g. drugs, alcohol, depression, lack of social outlets), asking partner(s) about their sexual history/HIV status, reducing number of sexual encounters, getting HIV tested, and telling others to get HIV/STI tested. In addition to HIV-related health behaviours, other health-positive behaviour changes that participants attributed to their use of HMP included: going to the gym, losing/gaining weight, quitting/reducing smoking and alcohol use, saving money, and attending community-based social events.
Precontemplation
In our analysis, sections of interview discussions that were characterised in the precontemplation phase of behaviour change commonly included participants' references to the social support features of HMP. Among men whose HMP-affected behaviours could be classified in the precontemplation stage, the most commonly reported barriers to behaviour change included lack of awareness, fear, and lack of social support. As described by participants, HMP provided information, examples, and activities in an engaging manner, raising awareness and facilitating further consideration of specific health topics and risk behaviours. As one participant explained about health and sexuality information he read on HMP, “I didn't really know what I was looking for until I happened to stumble upon it” (HMP13, HIV-positive, age 29).
Men reported feeling a sense of connection to others through HMP and the responses they received from Ask Dr. W and other participants. As one man explained, “It's all about information, learning together, helping each other” (HMP07, HIV-negative, age 23). Some participants reported not feeling comfortable enough to participate in certain sections of HMP (e.g. photo and video posts of the Getting Real section) due to their shyness or fear of being recognised. The user-driven design of these sections facilitated engagement for these individuals at the precontemplation stage. As one YBMSM noted, when he watched others' videos, “It was something I could relate to because it was a similar situation for me” (HMP14, HIV-positive, age 30). Although this participant did not contribute actively to the Getting Real section, he read and watched other peoples' contributions.
Participants also described examples of how HMP provided experience-based information that helped to dispel fears and instil hope. In reading about other YBMSM/TW's experiences, one man explained, “I connected a lot, and when I did feel connected, I would share my information with them” (HMP07, HIV-negative, age 23). This participant went on to describe how HMP could help users extend empathy toward each other. YBMSM/TW could also learn coping strategies from each other. In describing healthcare management, one participant described how HMP connected HIV-infected men at different stages post-diagnosis:
I can truly help you because I understand where you're at in life…because I've been dealing with it [HIV] for 10-plus years and I have the same bills you have, I have the same concept of being a grown-up that you do, so I can help you get through it easier than somebody who is not dealing with it [or] nowhere near your age group. (HMP15, HIV-positive, age 25)
These social interactions on HMP provided motivation: “What really caused me to get on [HMP] was hearing how other people were dealing with things” (HMP01, HIV-positive, age 29). Participants especially liked the videos and postings in the Getting Real section of HMP. Similarly, another participant explained, “I would come on to the site if I needed to talk with someone, maybe I'm going through the same depression that someone else is” (HMP09, HIV-positive, age 30, TW). Another participant echoed this sentiment stating, “It was good to see that I'm not the only one going through certain things in life and that we're all human…that just changed my perspective a little bit about my outlook on life…a little more hope” (HMP06, HIV-positive, age 23, TW).
Contemplation
In our analysis of HMP-affected behaviours that were categorised in the contemplation stage of behaviour change, participants' discussions included how HMP provided additional information, social support, and goal-setting features. As described by a number of participants, these features mutually reinforced learning. For example, participants would take a quiz, then read articles and retake the quiz to increase their score. One user explained, “The whole point to be on [HMP] was to gain information and knowledge” (HMP01, HIV-positive, age 29); another user stated: “The educational part for me was most interesting…[I] started off with the Forum and then really started getting into the information and tests sections – wanted to learn, wanted to win” (HMP03, HIV-negative, age 30). This user highlighted the importance of the games, challenges, and built-in reward features of HMP which positively reinforced continued intervention engagement.
Importantly, users described how the interactive knowledge-based components of HMP provided new information: “I didn't know too much before, especially [about] STD and sexual health” (HMP14, HIV-positive, age 30). Participants strongly endorsed the HMP feature of being able to talk to a doctor anonymously (Ask Dr. W) and described feeling comfortable asking personal questions. A number of users reported being drawn to this section of the website when they noticed that they had similar questions as others: “Somebody may have the same question but they may be scared to ask, while somebody else may be bold to ask” (HMP05, HIV-negative, age 23).
A number of participants described being inspired by other users to ask a question. As one man stated, “We can ask [Dr. W] anything…after reading how she responded to other people” (HMP10, HIV-negative, age 22). All participants reported high ratings for the HMP Forums: “That's what I would go to on a website for, to see what people are talking about and see what they think….see if I could benefit from anything. It made me want to post some questions of my own” (HMP06, HIV-positive, age 23, TW).
Preparation
Participants described examples of how information and virtual interactions on HMP helped them take steps toward healthy behaviours. A number of participants credited HMP with facilitating in-person health-related conversations with their friends and partners. For example, two participants noted that HMP prompted them to begin asking their partners about their sexual history, HIV status, and drug-use (HMP04, HIV-negative, age 29; HMP02, HIV-negative, age 20). For other men, interactions on the site moved them closer to health care services including HIV/STI testing, general health, and mental health: “When I asked the question [on the Forum]…people replied to me in the post, I ended up calling to a couple places…and set up [counselling] appointments in the realisation that I could possibly benefit” (HMP06, HIV-positive, age 23).
Some participants noted that they could share HMP's resources with others. As one man stated, “If I knew someone who did have questions, it'd be an easy place to say ‘oh you should check this out.’” (HMP13, HIV-positive, age 29). Another man explained, “I learned a lot…and then, say if you had a friend that is going through a dilemma…you can say….hey I found this, maybe we can go [get tested] together” (HMP07, HIV-negative, age 23). Importantly, participants recognised HMP as a tool they could apply in their daily lives: “I think the really cool thing about the site that I want it to facilitate is these kind of real-world spaces” (HMP13, HIV-positive, age 29).
YBMSM/TW also described the role of HMP as: “Empowering yourself physically, ethically, psychologically” (HMP09, HIV-positive, age 30, TW). As one user described,
A: [The site] has gotten me to…go outside of my comfort zone…gave me a stepping stone, and I actually found that I'm able to socialise a little bit more, and I was surprised when that happened!
Q: How did that happen?
A: Opening up and seeing other people open up. (HMP08, HIV-positive, age 27)
This passage is typical of how HMP facilitated movement from the preparation to action stage for many participants through modelling behaviour and providing social support.
All participants responded positively to HMP prizes describing how this feature motivated them increase their site use. One man also described how the HMP logo on the prize items (see HMP Store screenshot, Figure 2) provided opportunities to tell others about HMP and initiate sexual health conversations with friends and partners (HMP15, HIV-positive, age 25).
Action
Some participants reported changes in their behaviour during the pilot trial based on their interaction with the HMP intervention. This included reductions in sexual-risk behaviours, but also extended to other health areas including nutrition and fitness, substance use, and mental health.
One participant was motivated to reduce unprotected sex after reading the response to the question he posted on Ask Dr. W about his genital herpes infection:
One thing I didn't know that genital herpes, you carry it after you get it…and you can have outbreaks…and [are] more susceptible to transmitting HIV…I have a boyfriend…he's HIV negative and we're in an open relationship. We have unprotected sex…so now we're not having unprotected sex. (HMP12, HIV-positive, age 26)
Of note, this man previously talked with his partner about condoms but had not made the decision to use condoms until after his involvement with HMP.
The goal setting feature of HMP—My Life, My Goals—was also popular among participants for facilitating behavior change related to exercise and nutrition. For example, one participant credited this feature and suggestions from the Forum with his return to the gym and losing 10 pounds (HMP03, HIV-negative, age 30). Another participant used resources from HMP to start a food journal and was able to begin losing weight toward his fitness goals (HMP13, HIV-positive, age 29).
One man described how the educational articles and the Ask Dr. W forum inspired him to try switching from traditional cigarettes to electronic cigarettes (HMP11, HIV-positive, age 26). Similarly, a number of participants described how information and quizzes on HMP helped them identify the roles that drugs and alcohol played for them in doing unsafe things and two men used resources on HMP to find local assistance programs for substance use (HMP04, HIV-negative, age 29; HMP05, HIV-negative, age 23).
A key feature of the Stages of Change model is “cues to action”. The House of Mpowerment articles, Know Your Risk screeners, and My Life, My Goals applications all provide suggested action steps toward changing a specific behaviour and recommended resources to execute each action. Some participants described how user reviews and suggestions in the Local Scene provided trusted, useful information that helped them make decisions about where to go for testing or finding a gay-friendly venue to socialise. Our analysis showed that HMP participants also became cues to action for each other through sharing experiences in the Forum and Getting Real, and to their peers outside of HMP. As one participant explained: “I ask my friends now, ‘do y'all use condoms?’” (HMP05, HIV-negative, age 23). We found that HMP also provided positive reinforcement which can operate as a cue to future action; one participant described a sense of pride at having his videos online: “I look so good!” (HMP03, HIV-negative, age 30). HMP's text and email message reminders also served as cues to action. These messages encouraged logging on, highlighted site sections and new material, or wished users a fun and safe weekend.
Maintenance
Our analysis found that HMP supported users who were maintaining positive behaviour changes by providing continued social support, advanced information and resources, and strategies for reinforcing healthy behaviours. In the Forum, some participants were motivated to respond to other users' comments: “I was shocked! Somebody actually feels that way? I can answer that question from experience. It wasn't just me taking from the site, but I was also giving to the site as well” (HMP01, HIV-positive, age 29). Forum discussions helped empower users who had more experience dealing with an issue – such as sexuality or HIV – to support those who were less experienced. By sharing in this way, participants also reminded themselves of their own progress and reinforced their positive behaviours: “[The Forum] related to me…to see these people reaching out for help and being able to talk about it…it reminded me, I've been through it too, and that's where I will give advice in the Forums: It all gets better” (HMP07, HIV-negative, age 23). Another participant echoed this sentiment as he explained, “Reading about what others posted about being newly diagnosed brought me back to that place, ok, I already got over that, I already dealt with that” (HMP15, HIV-positive, age 25). Participants who were already practicing positive sexual health behaviours described how information on HMP provided a new perspective and offered new resources to support continued positive behaviours. One man who regularly gets HIV tests explained that using HMP helped him change his attitude about testing from viewing it as a hassle to a regular part of care (HMP03, HIV-negative, age 30).
The majority of users stated that the HMP points and rewards system was highly engaging. As one participant explained, “it made time on the site more personal, made you feel like you were doing something” (HMP06, HIV-positive, age 23, TW). Another participant described the points system as: “A visual representation of your progress on the site” (HMP04, HIV-negative, age 29). The point system motivated participants to use the site via competition: “You're gonna be on there nonstop because that's what you're focused on…I gotta do everything to get these points!” (HMP05, HIV-negative, age 23). Similarly, another man said, “It's an incentive if they tell me I'm gonna get something for it [points], I'm gonna be on there every single day” (HMP14, HIV-positive, age 30).
Discussion
HMP optimises the benefits of eHealth through its user-driven structure, provision of anonymity and confidentiality, and accessibility anytime, anywhere. HMP provides a framework and mechanisms for participants to encourage each other across the stages of health behaviour change and numerous features contribute to the intervention's sustainability which is required to support the transition through—and long-term maintenance of—behaviour change. The HMP administrative team and user-driven web structure facilitate and reinforce participants' movement across stages of behaviour change for their own specific target behaviours at their own pace and comfort level. Participants attributed their behaviour changes to various site features, further emphasising the critical role of user-driven design for facilitating the specific behaviour change that a participant is most ready to embrace.
HMP's experience sharing and community building features (LeGrand et al., 2014) alongside the gamification features (e.g. reputation points, HMP Store rewards, quizzes) all act as motivators and cues to action (Baltierra et al., 2014; Pike et al., 2014). Furthermore, the self-efficacy fostered by HMP helped instill confidence—a key Stages of Change mechanism (J. O. Prochaska & DiClemente, 1992)—as users tried out new behaviours.
There must be perceived community or social network for positive peer pressure and social norms to operate. Many YBMSM report high levels of stigma and social isolation (Ayala, Bingham, Kim, Wheeler, & Millett, 2012; Bogart, Landrine, Galvan, Wagner & Klein, 2013), which limits opportunities to use social support networks to facilitate healthy behaviours. An interactive, engaging eHealth intervention such as HMP has great potential for addressing this need while also maintaining a comfortable level of privacy and anonymity for YBMSM/TW.
The components of the HMP intervention can be aligned with one or more stages of behavioural change. One strength of the intervention is the plasticity allowed within these sections such that the same activity can address different stages of change for different participants. For example, The Forum could be a first exposure for one man about new ways to communicate HIV status to one's partners, while for another man it serves as reinforcement of a behaviour already in place. Similarly, the prize items users earn through their virtual interactions that feature the HMP logo (e.g. water bottles, messenger bag, sweatshirt hoodie) could serve as a visual cue to action for a participant who is initiating a new health behaviour, while for another participant in the maintenance phase, the logo serves as a reminder and an opportunity to initiate in-person sexual health conversations. Our analysis lays theoretical groundwork for future quantitative testing of these behaviour change processes through the HMP RCT and other similar projects under development such as the CDC-funded “Project Power” for Black bisexually active men (Maulsby et al., 2013) and Project HOPE for African American and Latino MSM (Jaganath, Gill, Cohen, & Young, 2012).
Conclusion
eHealth interventions for YBMSM/TW have the potential to reach marginalised, at-risk individuals in a novel, more engaging way. For YBMSM/TW in this pilot trial, HMP was a frequently used, highly acceptable means for HIV/STI as well as whole health intervention. HMP showed promise for being able to deliver a sufficient intervention dose and maintain exposure/engagement over time in order to achieve behaviour change, and in this qualitative assessment of 15 participants we found a pattern between the amount of intervention site use and stages of behaviour change. Our findings emphasise the importance of user generated feedback in the design and evaluation of tailored web and mobile phone based interventions. The Stages of Change theory integrated with theories of social support may offer a useful framework for assessing the mechanisms through which web and mobile phone based interventions can achieve and sustain real-world behaviour change. Furthermore, measuring outcomes along multiple stages of behavioural change may help to demonstrate that these interventions have positive impacts on critical earlier stages of behaviour change as well as main study outcomes.
Acknowledgments
This research was supported by the National Institute for Health (NIH) Grant 5R01MH093275. The views expressed herein do not reflect the official stance of any funding agency.
Biographies
Kathryn Muessig, PhD, is an Assistant Professor in the Department of Health Behavior at the Gillings School of Global Public Health at the University of North Carolina at Chapel Hill (UNC). Her research is primarily focused on intervention development to improve the prevention and treatment of HIV and other sexually transmitted diseases in particular among at-risk and underserved populations. Dr. Muessig's work is divided between North Carolina and China and she is affiliated with UNC's Institute for Global Health and Infectious Diseases and Project UNC in Guangzhou South China.
Contact:kate_muessig@med.unc.edu
Nina Baltierra is a Research Assistant in the Institute for Global Health and Infectious Diseases at the University of North Carolina - Chapel Hill. She is currently pursuing a Master's of Public Health and has been working in sexual and reproductive health for seven years.
Emily Pike is a Project Coordinator in the Institute of Global Health & Infectious Diseases at the University of North Carolina at Chapel Hill. Emily's research focuses on the social, structural, and behavioral factors that drive HIV and other sexually transmitted infections among at-risk population, especially racial and ethnic minority men and transgender women who have sex with men (MSM/TW), and utilising technology to address disparities in care and education. She is trained in qualitative methods for public health research and intervention design and evaluation.
Sara LeGrand, PhD, is an Assistant Research Professor at the Duke Global Health Institute and Center for Health Policy and Inequalities Research with a doctoral degree in Health Services Research. Dr. LeGrand has extensive experience conducting qualitative and quantitative research related to HIV prevention and care with findings published in peer-reviewed journals. She is currently serves as principal investigator, investigator and evaluator for numerous federally and foundation-funded HIV prevention and care grants. Dr. LeGrand is particularly interested in the design and evaluation of technology-based interventions that address disparities in HIV prevention and care.
Dr Hightow-Weidman, MD/MPH, is Clinical Associate Professor in the Division of Infectious Diseases, Department of Medicine, at the University of North Carolina School of Medicine, has been engaged in clinical and behavioral research focusing on HIV among Black MSM in the southeastern U.S. for more than a decade. She has expertise in mobile technologies and the design of primary and secondary HIV prevention interventions for young MSM.
Footnotes
We have no conflicts of interests to declare.
References
- Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. Am J Public Health. 2012;102(S2):S242–S249. doi: 10.2105/AJPH.2011.300641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltierra N, LeGrand S, Pike EC, Muessig KE, Bull S, Hightow-Weidman LB. More than *just* tracking time: measuring engagement within an internet-based HIV/STD intervention; Poster presentation, YTH Live; 2014, April 6-8; San Francisco, California, USA. 2014. http://yth.org/ythlive/about/ [Google Scholar]
- Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22. doi: 10.1016/S1473-3099. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Buday R, Thompson DI, Baranowski J. Playing for real: video games and stories for health-related behavior change. Am J Prev Med. 2008;34(1):74–82. doi: 10.1016/j.amepre.2007.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blas MM, Alva IE, Carcamo CP, Cabello R, Goodreau SM, Kimball AM, Kurth AE. Effect of an online video-based intervention to increase HIV testing in men who have sex with men in Peru. PLoS One. 2010;5(5):e10448. doi: 10.1371/journal.pone.0010448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Landrine H, Galvan FH, Wagner GJ, Klein DJ. Perceived discrimination and physical health among HIV-positive Black and Latino men who have sex with men. AIDS Behav. 2013;17:1431–41. doi: 10.1007/s10461-012-0397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brox E, Fernandez-Luque L, Tollefsen T. Healthy Gaming - Video Game Design to promote Health. Appl Clin Inform. 2011;2(2):128–142. doi: 10.4338/aci-2010-10-r-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter KM, Stoner SA, Mikko AN, Dhanak LP, Parsons JT. Efficacy of a web-based intervention to reduce sexual risk in men who have sex with men. AIDS Behav. 2010;14(3):549–557. doi: 10.1007/s10461-009-9578-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang JC, Dado D, Ashton S, Hawker L, Cluss PA, Buranosky R, Scholle SH. Understanding behavior change for women experiencing intimate partner violence: mapping the ups and downs using the stages of change. Patient Educ Couns. 2006;62(3):330–339. doi: 10.1016/j.pec.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Chiasson MA, Shaw FS, Humberstone M, Hirshfield S, Hartel D. Increased HIV disclosure three months after an online video intervention for men who have sex with men (MSM) AIDS Care. 2009;21(9):1081–1089. doi: 10.1080/09540120902730013. [DOI] [PubMed] [Google Scholar]
- Community Marketing Inc. [accessed January 4,2014];16th Annual Gay & Lesbian Tourism Report: Exploring tourism and hospitality opportunities in the gay and lesbian marketplace 2011–2012. 2012 Retrieved from: http://www.communitymarketinginc.com/documents/temp/CMI_16thLGBTTourismStudy.pdf. archived at: http://www.webcitation.org/6CCB3xyJv.
- Community Marketing Inc. [accessed January 4, 2014];2012 LGBT Community Survey. 2012 Retrieved from: http://www.communitymarketinginc.com/documents/CMI_6th_LGBT_Community_Survey_USv1.pdf. archived at: http://www.webcitation.org/6BJhmVzwt.
- Donkin L, Hickie IB, Christensen H, Naismith SL, Neal B, Cockayne NL, Glozier N. Rethinking the dose-response relationship between usage and outcome in an online intervention for depression: randomized controlled trial. J Med Internet Res. 2013;15(10):e231. doi: 10.2196/jmir.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M, Smith A Pew Research Center. [accessed February 22, 2014];Social Media Update 2013. 2014 Retrieved from: http://www.pewinternet.org/files/2014/01/Social_Networking_2013.pdf. archived at: http://www.webcitation.org/6Na9pDWRN.
- Enah C, Moneyham L, Vance DE, Childs G. Digital gaming for HIV prevention with young adolescents. J Assoc Nurses AIDS Care. 2013;24(1):71–80. doi: 10.1016/j.jana.2012.03.005. [DOI] [PubMed] [Google Scholar]
- Ferrer RA, Amico KR, Bryan A, Fisher WA, Cornman DH, Kiene SM, Fisher JD. Accuracy of the stages of change algorithm: sexual risk reported in the maintenance stage of change. Prev Sci. 2009;10(1):13–21. doi: 10.1007/s11121-008-0108-7. [DOI] [PubMed] [Google Scholar]
- Gabarron E, Serrano JA, Wynn R, Armayones M. Avatars using computer/smartphone mediated communication and social networking in prevention of sexually transmitted diseases among North-Norwegian youngsters. BMC Med Inform Decis Mak. 2012;12:120. doi: 10.1186/1472-6947-12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay G, Pollak J, Adams P, Leonard JP. Pilot study of Aurora, a social, mobile-phone-based emotion sharing and recording system. J Diabetes Sci Technol. 2011;5(2):325–332. doi: 10.1177/193229681100500219. http://www.ncbi.nlm.nih.gov/pubmed/?term=Gay+G+Pollak. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genberg BL, Lee Y, Rogers WH, Willey C, Wilson IB. Stages of change for adherence to antiretroviral medications. AIDS Patient Care STDS. 2013;27(10):567–572. doi: 10.1089/apc.2013.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman C, Hadley W, Brown LK, Houck CD, Peters A, Tolou-Shams M. Adolescent sexual risk: factors predicting condom use across the stages of change. AIDS Behav. 2008;12(6):913–922. doi: 10.1007/s10461-008-9396-y. [DOI] [PubMed] [Google Scholar]
- Gullette DL, Turner JG. Stages of change and condom use among an Internet sample of gay and bisexual men. J Assoc Nurses AIDS Care. 2004;15(2):27–37. doi: 10.1177/1055329003261968. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, Chan CL. Impact of a patient-centered, computer-based health information/support system. Am J Prev Med. 1999;16(1):1–9. doi: 10.1016/s0749-3797(98)00108-1. doi:S0749379798001081. [DOI] [PubMed] [Google Scholar]
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N the HIV/AIDS Prevention Research Synthesis Team. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. http://www.ncbi.nlm.nih.gov/pubmed/?term=17694429. [DOI] [PubMed] [Google Scholar]
- Hightow-Weidman LB, Fowler B, Kibe J, McCoy R, Pike E, Calabria M, Adimora A. HealthMpowerment.org: development of a theory-based HIV/STI website for young black MSM. AIDS Educ Prev. 2011;23(1):1–12. doi: 10.1521/aeap.2011.23.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hightow-Weidman LB, Pike E, Fowler B, Matthews DM, Kibe J, McCoy R, Adimora AA. HealthMpowerment.org: Feasibility and acceptability of delivering an Internet intervention to young Black men who have sex with men. AIDS Care. 2012;24(7):910–920. doi: 10.1080/09540121.2011.647677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaganath D, Gill HK, Cohen AC, Young SD. Harnessing Online Peer Education (HOPE): integrating C-POL and social media to train peer leaders in HIV prevention. AIDS Care. 2012;24(5):593–600. doi: 10.1080/09540121.2011.630355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson AS, Beer L, Sionean C, Hu X, Furlow-Parmley C, Le B, et al. Dean HD. HIV infection - United States, 2008 and 2010. MMWR Surveill Summ. 2013;62(Suppl 3):112–119. http://www.cdc.gov/mmwr/preview/mmwrhtml/su6203a19.htm. [PubMed] [Google Scholar]
- Ko NY, Hsieh CH, Wang MC, Lee C, Chen CL, Chung AC, Hsu ST. Effects of Internet popular opinion leaders (iPOL) among Internet-using men who have sex with men. J Med Internet Res. 2013;15(2):e40. doi: 10.2196/jmir.2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau JT, Lau M, Cheung A, Tsui HY. A randomized controlled study to evaluate the efficacy of an Internet-based intervention in reducing HIV risk behaviors among men who have sex with men in Hong Kong. AIDS Care. 2008;20(7):820–828. doi: 10.1080/09540120701694048. [DOI] [PubMed] [Google Scholar]
- LeGrand S, Muessig KE, Pike EC, Baltierra N, Hightow-Weidman LW. If you build it will they come? Addressing social isolation within a technology-based HIV intervention for young black men who have sex with men. AIDS Care, 12 March, epub ahead of print. 2014 doi: 10.1080/09540121.2014.894608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustria ML, Cortese J, Noar SM, Glueckauf RL. Computer-tailored health interventions delivered over the Web: review and analysis of key components. Patient Educ Couns. 2009;74(2):156–173. doi: 10.1016/j.pec.2008.08.023. [DOI] [PubMed] [Google Scholar]
- Lustria ML, Noar SM, Cortese J, Van Stee SK, Glueckauf RL, Lee J. A meta-analysis of web-delivered tailored health behavior change interventions. J Health Commun. 2013;18(11):1039–1069. doi: 10.1080/10810730.2013.768727. [DOI] [PubMed] [Google Scholar]
- Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, Holtgrave D. A systematic review of HIV interventions for black men who have sex with men (MSM) BMC Public Health. 2013;13:625. doi: 10.1186/1471-2458-13-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier A, Lyons EJ, Frydman G, Forlenza M, Rimer BK. How cancer survivors provide support on cancer-related Internet mailing lists. J Med Internet Res. 2007;9(2):e12. doi: 10.2196/jmir.9.2.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Remis RS. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–348. doi: 10.1016/s0140-6736(12)60899-x. [DOI] [PubMed] [Google Scholar]
- Miranda J, Cote J, Godin G, Blais M, Otis J, Gueheneuc YG, et al. Fowler S. An Internet-Based Intervention (Condom-Him) to Increase Condom Use Among HIV-Positive Men Who Have Sex With Men: Protocol for a Randomized Controlled Trial. JMIR Res Protoc. 2013;2(2):e39. doi: 10.2196/resprot.2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muessig KE, Pike EC, Fowler B, LeGrand S, Parsons JT, Bull SS, et al. Hightow-Weidman LB. Putting prevention in their pockets: developing mobile phone-based HIV interventions for black men who have sex with men. AIDS Patient Care STDS. 2013;27(4):211–222. doi: 10.1089/apc.2012.0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Crosby R, Benac C, Snow G, Troutman A. Application of the attitude-social influence-efficacy model to condom use among African-American STD clinic patients: implications for tailored health communication. AIDS Behav. 2011;15(5):1045–1057. doi: 10.1007/s10461-009-9599-x. [DOI] [PubMed] [Google Scholar]
- Oster AM, Johnson CH, Le BC, Balaji AB, Finlayson TJ, Lansky A, et al. Paz-Bailey G. Trends in HIV Prevalence and HIV Testing Among Young MSM: Five United States Cities, 1994-2011. AIDS Behav. 2013 doi: 10.1007/s10461-013-0566-1. [DOI] [PubMed] [Google Scholar]
- Oster AM, Wiegand RE, Sionean C, Miles IJ, Thomas PE, Melendez-Morales L, et al. Millett GA. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011;25(8):1103–1112. doi: 10.1097/QAD.0b013e3283471efa. [DOI] [PubMed] [Google Scholar]
- Pike EC, Baltierra N, Muessig KE, LeGrand S, Bull S, Hightow-Weidman LB. Level Up! How gamification can be used to spark competition, collaboration, and community in online health behavior interventions; Oral presentation, YTH Live; 2014, April 6-8; San Francisco, California, USA. 2014. http://yth.org/ythlive/about/ [Google Scholar]
- Prat F, Planes M, Gras ME, Sullman MJ. Stages of change and decisional balance for condom use with a romantic partner. J Health Psychol. 2012;17(8):1193–1202. doi: 10.1177/1359105311433911. [DOI] [PubMed] [Google Scholar]
- Primack BA, Carroll MV, McNamara M, Klem ML, King B, Rich M, et al. Nayak S. Role of video games in improving health-related outcomes: a systematic review. Am J Prev Med. 2012;42(6):630–638. doi: 10.1016/j.amepre.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Pechmann C, Kim R, Leonhardt JM. Twitter=quitter? An analysis of Twitter quit smoking social networks. Tobacco Control. 2012;21(4):447–449. doi: 10.1136/tc.2010.042507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Prog Behav Modif. 1992;28:183–218. http://www.ncbi.nlm.nih.gov/pubmed/1620663. [PubMed] [Google Scholar]
- Prochaska JO, Redding CA, Harlow LL, Rossi JS, Velicer WF. The transtheoretical model of change and HIV prevention: a review. Health Educ Q. 1994;21(4):471–486. doi: 10.1177/109019819402100410. http://www.ncbi.nlm.nih.gov/pubmed/7843978. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Vissman AT, Stowers J, Miller C, McCoy TP, Hergenrather KC, et al. Eng E. A CBPR partnership increases HIV testing among men who have sex with men (MSM): outcome findings from a pilot test of the CyBER/testing internet intervention. Health Educ Behav. 2011;38(3):311–320. doi: 10.1177/1090198110379572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosser BR, Oakes JM, Konstan J, Hooper S, Horvath KJ, Danilenko GP, et al. Smolenski DJ. Reducing HIV risk behavior of men who have sex with men through persuasive computing: results of the Men's INTernet Study-II. Aids. 2010;24(13):2099–2107. doi: 10.1097/QAD.0b013e32833c4ac7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung WC, Lu M, Cook DM. Condom use and stages of change among college students in Taiwan. Public Health Nurs. 2010;27(6):474–481. doi: 10.1111/j.1525-1446.2010.00890.x. [DOI] [PubMed] [Google Scholar]
- US Centers for Disease Control. Prevalence and awareness of HIV infection among men who have sex with men --- 21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–1207. http://www.ncbi.nlm.nih.gov/pubmed/?term=20864920. [PubMed] [Google Scholar]
- Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J. HIV infection and awareness among men who have sex with men-20 cities, United States, 2008 and 2011. PLoS One. 2013;8(10):e76878. doi: 10.1371/journal.pone.0076878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willey C, Redding C, Stafford J, Garfield F, Geletko S, Flanigan T, et al. Caro JJ. Stages of change for adherence with medication regimens for chronic disease: development and validation of a measure. Clin Ther. 2000;22(7):858–871. doi: 10.1016/s0149-2918(00)80058-2. http://www.ncbi.nlm.nih.gov/pubmed/10945512. [DOI] [PubMed] [Google Scholar]
- Zickuhr K, Smith A. [accessed 22, 2, 2014];Digital differences Pew Internet & AmericanLife Project. 2012 Apr 13; Retrieved from: http://www.pewinternet.org/files/old-media//Files/Reports/2012/PIP_Digital_differences_041312.pdf. archived at: http://www.webcitation.org/6BL7HMIo4.


