Abstract
Objective
This project investigated the effectiveness of contingency management for improving retention in treatment and positive outcomes among patients with dual disorders in intensive outpatient treatment for addiction.
Methods
The effect of contingency management was explored among a group of 160 patients exposed to contingency management (n = 88) and not exposed to contingency management (no contingency management, n = 72) in a partial hospitalization program. Patients referred to the partial hospitalization program for treatment of substance use and comorbid psychiatric disorders were diagnosed by psychiatrists and specialist clinicians according to the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-IV-TR). A unique application of the contingency management “fishbowl” method was used in the to improve consistency of attendance at treatment sessions, which patients attended five days a week. Days attending treatment and drug-free days were the main outcome variables. Other outcomes of interest were depression, anxiety and psychological stress, coping ability, and intensity of drug cravings.
Results
Patients in the contingency management group attended more treatment days compared to patients in the no contingency management group; M = 16.2 days (SD = 10.0) vs. M = 9.9 days (SD = 8.5), respectively; t = 4.2, df = 158, p<.001. No difference was found between the treatment groups on number of drug-free days. Psychological stress and drug craving were inversely associated with drug-free days in bivariate testing (r =−.18, p<.02; r = −.31, p<.001 respectively). Treatment days attended and drug craving were associated with drug-free days in multivariate testing (B = .05, SE =.01, β = .39, t =4.9, p <.001; B = −.47 SE = .12, β = −.30, t =−3.9, p <.001; respectively; Adj. R2 = .21). Days attending treatment partially mediated the relationship between exposure to contingency management and self-reported drug-free days.
Conclusions
Contingency management is a valuable adjunct for increasing retention in treatment among patients with dual disorders in partial hospitalization treatment. Exposure to contingency management increases retention in treatment, which in turn contributes to increased drug-free days. Interventions for coping with psychological stress and drug cravings should be emphasized in intensive dual diagnosis group therapy.
Keywords: contingency management, intensive outpatient treatment, drug-free days
Contingency management has robust support as an adjunctive treatment for reducing substance use and substance-positive urines among individuals with alcohol, cannabis, cocaine and opioid use disorders (Alessi et al., 2011; Drake et al., 2008; Dutra et al., 2008; Petry et al, 2005; Rash et al., 2008). Furthermore, contingency management has been found to increase retention in treatment, primarily among patients with opioid and stimulant abuse. Recent studies have found that contingency management is also associated with improved depressive and psychotic symptoms among patients with stimulant and opioid use disorders (Rhodes et al., 2003; Petry et al., 2012; Mayet et al., 2005; Kirby et al., 2008; Petry et al., 2013; McDonell et al., 2013; Petry et al., 2013).
Patients with substance dependence and severe psychiatric disorders (dual diagnosis, dual disorders or comorbidity) require intensive treatments (Kelly et al., 2012) and retention is critical to maximize positive outcomes (Humphreys & McLellan, 2011). Although contingency management has been found to increase treatment attendance (Walker et al., 2010), the relationship of comorbidity and contingency management has not been well-studied. Some studies of treatment retention in community-based clinics using contingency management have not included comorbidity while others have not used standardized methods for characterizing comorbidity in the sample (Ledgerwood et al., 2008; Petry et al., 2011; Carey & Carey, 1990; Helmus et al., 2003).
The primary objectives of the current project were to investigate: 1) the effectiveness of contingency management for improving treatment retention in a heterogeneous sample of patients with dual disorders in a community-based partial hospitalization program; 2) the effect contingency management has on clinical variables, including drug-free days, depression, anxiety, drug craving, psychological stress and coping ability; and 3) the relationships between the clinical variables and drug-free days. A secondary objective was to describe the comorbidity of the sample based on the DSM-IV (American Psychiatric Association, 2000), and to investigate the effect of contingency management on clinical symptoms.
A quality improvement program evaluation was conducted during a period in which a contingency management program was systematically provided or withdrawn while prospectively collecting self-report clinical data on patients. The patients’ medical records were then reviewed during the same time period for data on patient diagnoses, consistency of attendance and frequency of drug-free days.
We hypothesized that patients exposed to contingency management would: 1) remain in treatment longer and; 2) report more drug-free days during treatment. We expected that patients exposed to contingency management would report decreased depression, anxiety, drug craving and psychological stress and increased coping ability, compared to those not exposed to contingency management.
METHODS
This quality improvement program evaluation was conducted in the partial hospitalization program of the Center for Psychiatric and Chemical Dependency Services at the University of Pittsburgh Medical Center (UPMC), Pittsburgh, PA. In accord with the University of Pittsburgh Institutional Review Board, the program evaluation was approved by the Quality Improvement Review Committee of the UPMC. The operation of the contingency management project in conjunction with the partial hospitalization program was discussed with all patients during treatment. Written informed consent to participate was waived because the contingency management program was a quality improvement initiative and was operated as a standard part of treatment.
The partial hospitalization program provides integrated treatment for addiction and comorbid psychiatric conditions, including manualized group therapy five days a week for six weeks (Daley, 2011). Patients then receive less intensive outpatient treatment. Partial hospitalization program patients typically experience the most severe substance use disorders and are routinely referred to partial hospitalization program following medical detoxification or inpatient psychiatric treatment. Partial hospitalization program sessions typically include a broad range of recovery topics, including understanding the concept and interactions of dual disorders, the impact of substance use on families and children, the importance of 12-Step support programs and managing emotions and lifestyle changes.
Participants
One hundred sixty-seven patients were admitted to the partial hospitalization program during the quality improvement project period. Seven patients (.04%) provided no data for the project and were therefore excluded from the analysis. Of the 160 patients who were included, 83 (52%) were males, the mean age was 40.2 years (SD = 10.4), and most were Caucasian (n = 108, 68%) or African-American (n = 49, 31%). Eighty-eight patients (55%) were exposed to the contingency management intervention, while 72 (45%) were not exposed to contingency management at all. The sample in the contingency management group is larger because some patients initially participated in the no contingency management group but returned to the partial hospitalization program at a time when the contingency management intervention was operational. These patients were, therefore, reassigned to the contingency management group. In this way, patients in the no contingency management group were never exposed to the contingency management program. No differences were found between the rates of recruitment for the contingency management vs. the no contingency management groups across treatment phases (χ2 = 0.53, df = 2, p = .78).
Project Design
We began the quality improvement program evaluation with collection of baseline data (no contingency management) for six weeks prior to the first round of the intervention. We then began three periods of a 6-week intervention phase (contingency management) followed by a 6-week no intervention phase (no contingency management), for a total of three testing periods comprised of three separate samples. The expectation was that changes in attendance at group therapy would be higher during periods of intervention and lower during non-intervention periods. Baseline data collection began in October 2007, and the first intervention period began in mid-November 2007. The project was conducted through June 2008.
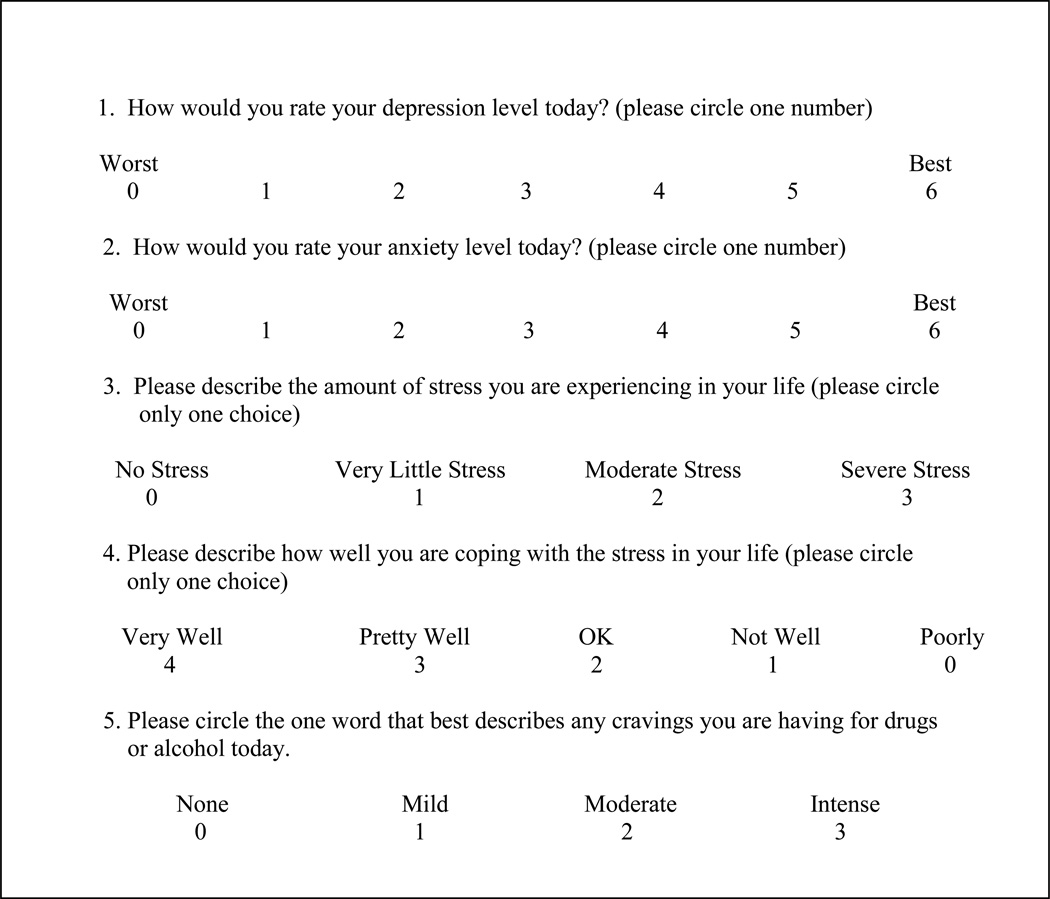
Symptom Rating Report
The project was conducted as a standard part of treatment. Due to time constraints data collection was limited to completing a one-page self-report form each day in the five minutes before the start of the first treatment session. The collection form included Likert Scale items about depression, anxiety, drug cravings, psychological stress and coping ability. Figure 1 contains these five items. Partial hospitalization program group therapists collected the symptom rating report form prior to treatment each day. Patients did not submit all self-report forms, resulting in 21% missing data on the clinical items.
Figure 1.
Symptom Rating Form for Partial Hospitalization Program
Attendance at Group Therapy and Drug-Free Days
Medical records were reviewed to determine: 1) the number of days patients attended the program, and 2) patients’ self-report of the date of their last drug use. Attendance was calculated by counts of days that patients attended at least two of three partial hospitalization program sessions. Drug-free days were calculated by counting the total number of days between the patient’s reported date of last use and his/her date of next use (missing data = 1.8%).
Diagnosis and Comorbidity
Partial hospitalization program treatment includes an evaluation by a psychiatrist and diagnoses defined by the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition TR (American Psychiatric Association, 2000) were entered into the medical record. Patients in the project had a median of 3 diagnoses, ranging from 1 to 7 diagnoses.
Frequencies and percentages of substance-related diagnoses in the sample include: 84 (53%) with alcohol use disorder; 53 (33%) with cocaine use disorder; 32 (20%) with opioid use disorder; 25 (16%) with cannabis use disorder; and 25 (16%) with other substance use disorders. psychiatric disorders include: 69 (43%) with depressive disorder – not otherwise specified; 47 (29%) with major depression; 26 (16%) with bipolar disorder; 21 (13%) with anxiety disorder – not otherwise specified; 17 (11%) with other anxiety disorders; 5 (3%) with attention deficit-hyperactivity disorder; 5 (3%) with psychotic disorders; and 1 (.006%) with eating disorder. Table 1 shows comorbid pairings of the primary substance use and psychiatric disorders.
Table 1.
Frequencies and Percentages of Paired Comorbid Substance Use and Psychiatric Disorders (N = 160)
| Substance Use Disordersa | ||||||
|---|---|---|---|---|---|---|
| Psychiatric Disorders | Alcohol n (%) |
Stimulant n (%) |
Opioid n (%) |
Cannabis n (%) |
Sedative/Hypnotic n (%) |
Poly-Substance n (%) |
| Major Depressive Disorder | 19 (6.5) | 15 (5.1) | 4 (1.3) | 6 (2.0) | 3 (1.0) | 1 (0.4) |
| Bipolar Disorder | 16 (5.4) | 7 (2.4) | 4 (1.3) | 5 (1.6) | 2 (0.7) | 3 (1.0) |
| Depressive Disorder NOSb | 47 (16.0) | 28 (9.5) | 17 (5.7) | 14 (4.7) | 4 (1.3) | 10 (3.4) |
| Anxietyc | 23 (7.8) | 10 (3.4) | 7 (2.4) | 7 (2.4) | 2 (0.7) | 8 (2.7) |
| Psychoticd | 2 (0.7) | 2 (0.7) | 0 (0.0) | 3 (1.0) | 1 (0.4) | 0 (0.0) |
| Othere | 7 (2.4) | 6 (2.0) | 8 (2.7) | 1 (0.4) | 0 (0.0) | 3 (1.0) |
Note. NOS = not otherwise specified.
1 case of hallucinogen abuse was recorded (not included above); 0 cases of inhalant use disorder
Includes mood disorder NOS
Generalized anxiety disorder, posttraumatic stress disorder, anxiety disorder NOS, obsessive-compulsive disorder, panic disorder
Psychotic disorder NOS, schizoaffective disorder
Attention deficit-hyperactivity disorder, eating disorder NOS
Contingency Management Procedures for Increasing Attendance at Treatment
The fishbowl method was used in the contingency management intervention because it was considered the easiest to implement and manage in the partial hospitalization program. Group members were surveyed and chose gift cards from local grocery and department stores as incentives. Incentives included gift cards ($5 to $25), snacks and dollar store items, and $3 gift cards for coffee shops (value range = $1.00 to $25.00).
The fishbowl contained 500 slips; 250 had no cash value but had positive messages to encourage sobriety; 250 had merchandise value. Non-winning slips and prizes won were replaced weekly so patients were consistently reinforced by drawing winning slips, and by witnessing winning draws among their peers. The total cost of incentives for the 9-month project was approximately $3,300.
Staff involved in operating the contingency management included two project assistants. The same two assistants, trained by the first author, administered the procedures during the entire 9-month project period. In order to verify that the procedures were being implemented properly, the first author attended all groups where drawing from the fishbowl took place during the first contingency management period. The project assistants administered all draws from the fishbowl and awarded prizes once a week, immediately following the last group session each Friday.
Reinforcement Schedule
Daily group attendance was kept by the group therapists and provided to the first author who reviewed the attendance records and determined the number of draws each group member would receive each week. A group therapy treatment session in the partial hospitalization program consisted of three separate parts, each lasting an hour. Credit for a draw from the fishbowl was given only if a patient attended at least two of the three parts of each treatment session. There were no deviations from this rule.
Each week represented a single program period and rights to draw from the fishbowl were not carried over from week to week. Patients received 1 draw from the fishbowl for attending their group therapy treatment session each Monday. Patients who attended on Tuesday received 2 more draws; 3 more for attending the Wednesday and so on, with a potential to earn up to 15 draws each week. If a patient missed a treatment session his/her starting point for draws from the fishbowl was reset to 0. The patient received 1 draw at the next session and the reinforcement schedule proceeded. The critical component of the method is that the number of draws increased commensurate with the number of consecutively attended treatment sessions. The schedule outlined below indicates the draws for a patient who attended every session in the week (left) and for a patient who missed one session (right).
| Attended All Sessions | Missed One Session | ||
| Mon = 1 draw | 1+ | Mon = 1 draw | 1+ |
| Tues.= 2 draws | 2+ | Tues.= 2 draws | 2+ |
| Wed.= 3 draws | 3+ | Wed. = Missed Session | 0+ |
| Thurs.= 4 draws | 4+ | Thurs.= 1 draw | 1+ |
| Fri. = 5 draws | 5 = 15 draws | Fri. = 2 draws | 2 = 6 draws |
Data Analysis
Data were analyzed using PASW Statistics 21.0. The data were examined for assumption of normalcy and one variable (drug-free days) was found be significantly skewed. The data contained no zeros. Therefore, the drug-free days variable was transformed by computing its natural log and the transformed variable was used in the analysis. The Likert scales used to rate clinical symptoms represent ordinal level data. However, parametric testing is recommended for analyses of ordinal level data because such data is quite robust for yielding valid outcomes using parametric tests (Norman, 2010). All tests used an alpha level of .05 as indicative of statistical significance. The score on the first day (which was taken prior to conducting any treatment) was used to measure clinical severity prior to treatment. Patient scores of clinical ratings on their first day of treatment were also used to test for pre-treatment differences on demographic and the clinical variables (depression, anxiety, emotional stress, coping ability and drug craving).
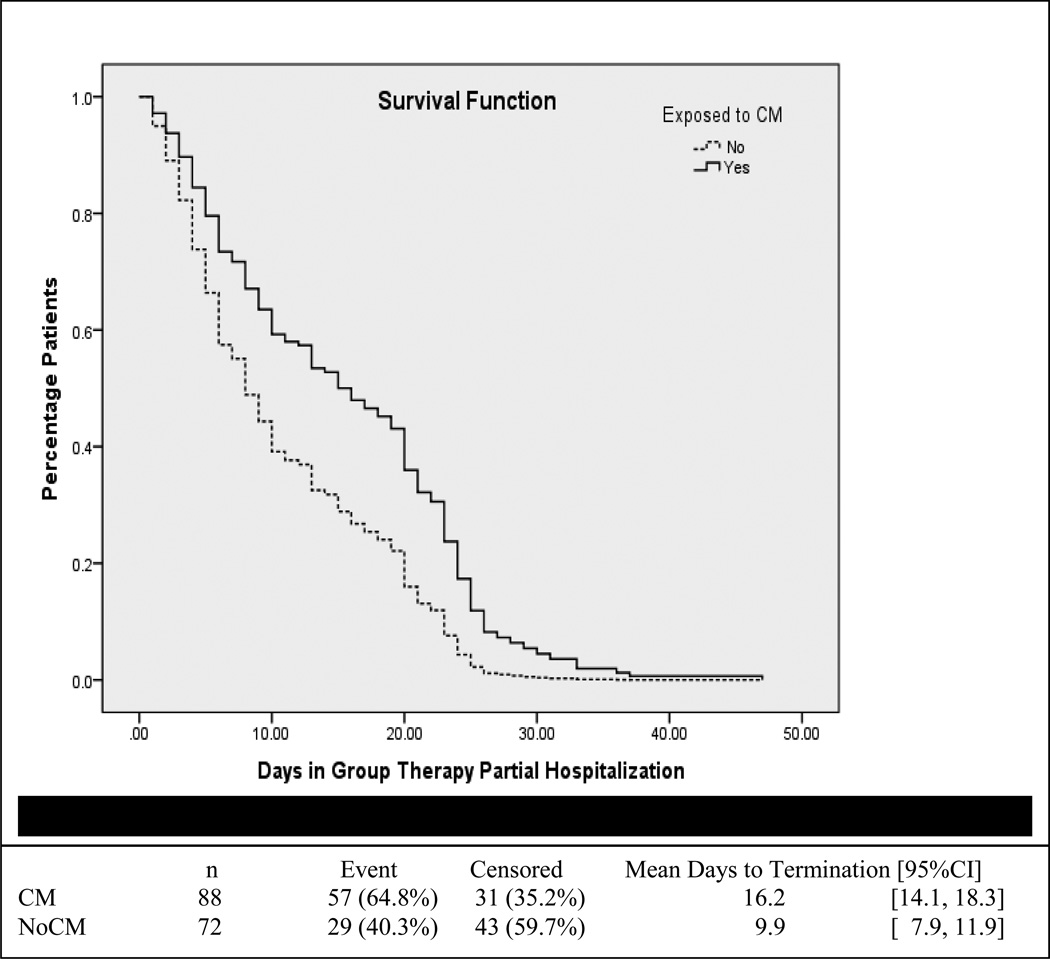
Retention in treatment was tested using Student’s t-tests to determine differences on days in treatment between patients in the contingency management program compared to patients who were not exposed to contingency management. Cox regression analysis was used to show graphically the differences for “survival” in the partial hospitalization program program based on membership in the contingency management and no contingency management groups. The mean number of days patients spent in the partial hospitalization program based on membership in the contingency management and no contingency management groups was used as the time variable. The event variable was the last day the patient was in the partial hospitalization program (right-censored data).
Our clinical ratings were taken on a daily basis and clinical symptoms such as depression are affected by transient variability that cannot be controlled. This phenomenon is why improvement in psychotherapy is a cumulative, and not a linear process (Bell et al., 1996). Therefore, the mean score is the most valid score for measuring improvement because the mean accounts for such changes over time.
The mean score was computed from all scores other than the score reported on the first day of treatment. Student’s t-tests were used for testing differences between the contingency management and no contingency management groups on self-reported drug-free days, and the clinical variables of depression, anxiety, stress, coping ability and craving for drugs. The contingency management and no contingency management groups were tested for differences on days attending the partial hospitalization program and drug-free days. Correlation analyses were used to test the relationships of clinical variables to drug-free days. Statistically significant variables (p ≤ .05) in relation to drug-free days were included in a multivariate linear regression analysis.
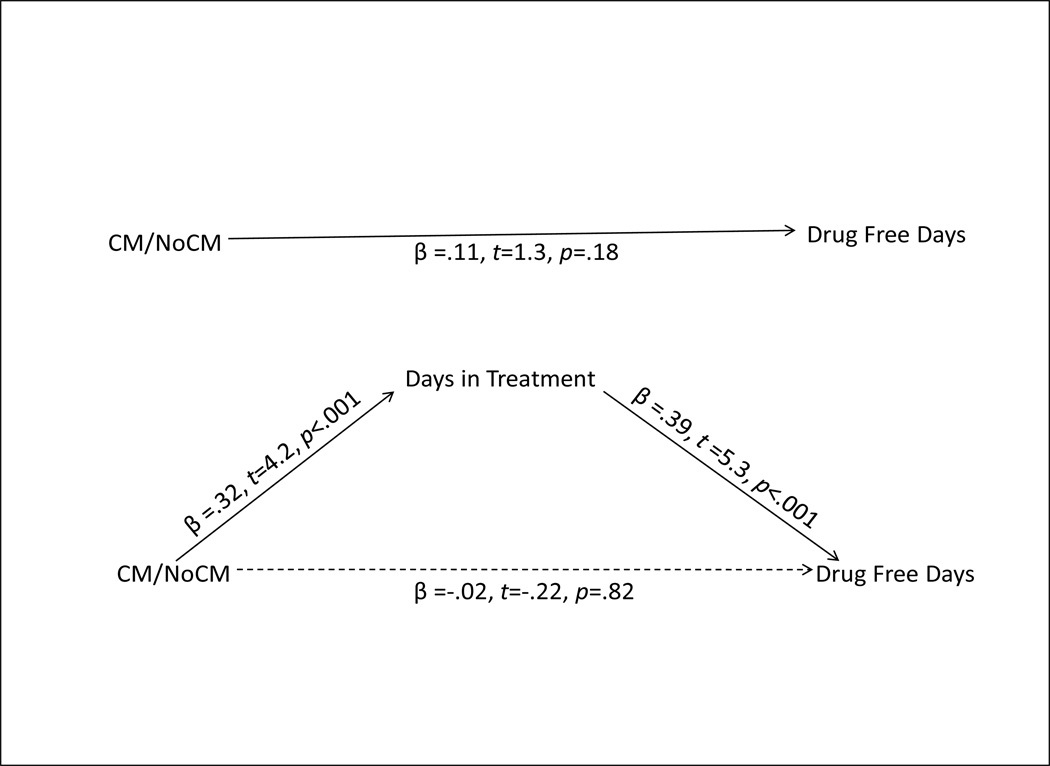
Following the Baron and Kenny (1986) model, a test of mediation was conducted using linear regression with the group treatment variable (contingency management vs. no contingency management) as the independent variable, days in partial hospitalization program treatment as the mediating variable and drug-free days as the dependent variable. The project design satisfies the criteria for mediation because the variables follow a temporal order consistent with the contingency management vs. no contingency management intervention preceding treatment attendance, which precedes the total count of drug-free days (Baron & Kenny, 1986).
RESULTS
Pre-Treatment Group Differences
No significant differences were found at baseline between groups on gender or race. However, there was a significant difference with regard to anxiety. Patients who were not Caucasian (primarily African-Americans) had significantly less anxiety (M = 4.0, SD = 1.4) compared to those who were Caucasian (M = 3.1, SD = 1.6); t = 3.3, df = 156, p = .001. No pre-treatment differences were found between the contingency management and no contingency management groups on clinical variables, suggesting that clinical changes related to treatment group assignment were not related to pre-treatment differences.
Demographic Characteristics
Patients who were not Caucasian reported significant improvement, compared to Caucasians, on anxiety; M = 4.0 (SD = 1.3) vs. M = 3.5 (SD = 1.2), respectively; t = 2.5, df = 158, p <.02; and stress; M = 1.7 (SD = 0.6) vs. M = 1.9 (SD = 0.6), respectively; t = −2.4, df = 158, p <.02. No differences related to race or gender were found on days attending treatment or frequency of drug-free days.
Clinical Symptoms and Days in Treatment
The mean number of days in treatment for the total sample was 13.4 (SD = 10.0, range = 1 – 47). Overall, patients in the contingency management group attended a mean of 16.2 (SD = 10.0) days in the partial hospitalization program, as opposed to patients in the no contingency management group, who attended a mean of 9.9 days (SD = 8.5); t = 4.2, df = 158, p<.001). This pattern basically held true for each testing period during the 9-month project. The first 12-week testing period included 60 patients (33 in the intervention group and 27 in the no intervention group). The contingency management group attended significantly more days in treatment than the no contingency management group; M = 17.0 days (SD = 10.6) vs. M = 11.2 days (SD = 9.3), respectively; t = 2.2, df = 58, p <.04). The second 12-week testing period included 44 patients (26 in the intervention group and 18 in the no intervention group). The contingency management group attended somewhat more days in treatment than the no contingency management group, but this did not reach significance; M = 17.0 days (SD = 11.4) vs. M = 11.4 (SD = 10.0), respectively; t = 1.6, df = 42, p <.10). The third testing period included 56 patients (29 in the intervention group and 27 in the no intervention group). The contingency management group attended significantly more days in treatment than the no contingency management group; M = 14.7 days (SD = 8.0) vs. M = 7.7 days (SD = 6.1), respectively; t = 3.7, df = 54, p < .002).
We found that three clinical variables were significantly associated with days of treatment attendance in bivariate analyses. Increased treatment attendance was associated with improved depression (r =.18, p<.03) and increased coping ability (r =.24, p<.003), while decreased treatment attendance was associated with increased psychological stress (r =−.35, p<.001).
We entered the clinical variables, along with the group treatment variable, into a Cox regression. The model was significant (−2 Log L = 1298.5; overall χ2 = 27.29, df = 4, p <.001; change from previous step χ2 = 27.34, df = 4, p <.001). The treatment group variable entered the model first; B = .61, SE = .17, Wald = 13.0, Hazard Ratio = 1.8, 95% CI [1.3, 2.5], p<.001. The stress variable remained in the model; B = .54, SE = .23, Wald = 5.7, Hazard Ratio = 1.7, 95% CI [1.1,2.7], p >02). Figure 2 displays a survival plot of patient retention in the partial hospitalization program based on exposure to the contingency management intervention.
Figure 2.
Survival Plot of Patient Retention in Partial Hospitalization Program by Group
Improvement on Clinical Variables Related to Contingency Management Exposure
We found no statistically significant differences between the contingency management and no contingency management groups on depression, anxiety, stress level, coping ability and drug cravings. A within-group analysis of the full sample found significant improvement on all clinical variables, regardless of group membership (data not shown).
Treatment Group, Clinical Improvement and Drug-Free Days
The mean number of drug-free days in the non-transformed data for the total sample was 37.3 (SD = 39.6, range = 1 – 346). Using the log transformed data, no differences were found between the contingency management and no contingency management groups on drug-free days, M = 3.2 (SD = 1.2) vs. M = 2.9 (SD = 1.1) days; t = 1.4, df = 158, p =.18. Two clinical variables, psychological stress and drug craving, were negatively associated with drug-free days (r = −.18, p<.02 and r = −.31, p<.001, respectively).
Multivariate Analysis of Drug-Free Days
Statistically significant variables identified in bivariate testing, treatment days attended, psychological stress and drug craving, were entered into a linear regression analysis with log drug-free days as the dependent variable. Treatment days attended entered the regression first (B = .05, SE =.01, β = .39, t =4.9, p <.001), and drug craving was also significant in the model (B = −.47 SE = .12, β = −.30, t =−3.9, p <.001; Adj. R2 = .21).
Test of Mediation
We found that the number of days in treatment partially mediated the relationship between the contingency management/no contingency management group variable and the number of log transformed drug-free days. Figure 3 displays these relationships.
Figure 3.
Mediation of Treatment Group and Drug-free Days by Days in Treatment
Comorbidity
Our small sample (N = 160) did not permit investigating comorbidity beyond diagnostic pairings. Furthermore, few diagnostic categories (see Table 1) contain enough of a subsample to permit testing of the relationship between comorbidity and our outcomes of clinical improvement, days in treatment and drug-free days.
DISCUSSION
To our knowledge this is the first open treatment evaluation of contingency management that includes DSM-IV defined comorbidity as a covariate for determining the impact of psychiatric severity on retention in treatment and abstinence from drugs. Unfortunately, our small sample did not allow statistical testing to determine whether particular comorbidities differentially impact the effect of contingency management. Notwithstanding this limitation, the results of our project confirm the value of contingency management as an adjunct to intensive group treatment for patients in a community-based, dual diagnosis clinic. Patients attended more treatment days in the partial hospitalization program when the contingency management intervention was operating and fewer treatment days when the intervention was not operating.
We believe our application of the fishbowl method demonstrates that contingency management can be used to enhance consistent attendance at intensive treatment. Such consistency in attendance is effective for reinforcing gains in treatment based on the clinical reality that improvement is positively associated with time spent in treatment (Zhang et al., 2003). Improving treatment attendance also has major implications for the viability of treatment programs which receive reimbursement only when patients attend treatment. A review of payment for partial hospitalization program services in our clinic found that approximately $49,000 in revenue was collected during the no contingency management phases of the project. This figure rose to $95,000 during the contingency management phases of the project.
In contrast with our hypothesis, we did not find a significant difference in drug-free days between the contingency management group and the no contingency management group. Furthermore, no interaction was found between the treatment groups on psychological stress or drug cravings in relation to drug-free days. However, psychological stress was inversely associated with days spent in treatment. Our findings are consistent with other research (Dobkin et al., 2002) and with a recent review (Penberthy et al., 2010) indicating that psychosocial stress is one of the major reasons for low treatment retention among patients with cocaine addiction.
Drug craving was retained in multivariate testing as a robust inverse indicator of drug-free days in our project. This finding is consistent with Sinha’s (2011) review that drug craving is among the most commonly reported reasons for relapse. We did not measure time to relapse, but relapse (fewer drug-free days) is a major reason for treatment dropout and our findings suggest that drug craving may place patients at risk for relapse.
Unlike other recent findings (McDonell et al., 2013; Petry et al., 2013), we found no difference on symptom ratings related to treatment group (contingency management vs. no contingency management). However, our sample was heterogeneous regarding substance use while Petry and colleagues’ and McDonnell and colleagues’ studied stimulant users. Furthermore, treatment as usual in Petry and colleagues’ study appears to have been somewhat less intense compared to ours, and the content of the group therapy in both other studies focused on topics specific to substance abuse, while our manualized treatment emphasized content related to dual disorders. McDonnell and colleagues (2013) sample had a large proportion of psychotic patients and used a wide variety of types and intensities of interventions for treatment as usual. Conversely, our sample was low on rates of psychosis and our intensive outpatient treatment used a very structured format. Finally, time constraints for data collection on clinical variables restricted us to using measures that may be conceptually different compared to those of psychiatric symptoms used in the other referenced studies. Any or all of these differences could account for our differing findings.
We found that contingency management increases days in treatment and days in treatment partially mediates the relationship between exposure to the intervention and drug-free days. Baron and Kenny (1986) note that “perfect” mediation occurs only if the independent variable has no effect on the dependent variable when the mediator is controlled, which does not occur in our model. Therefore, in fact, our findings are consistent with partial mediation. For example, it is clear that drug craving also had a significant effect on the frequency of drug-free days in our sample. The findings on the relationship between the group treatment variable (contingency management vs. no contingency management) and drug-free days fall outside the range of statistical significance (Figure 3). However, recent research suggests that statistical significance between the independent and dependent variables is not essential for mediation when dilution between the variables occurs, thus contributing to a distal effect of the independent variable on the dependent variable (Krause et al., 2010). It is quite possible that such dilution occurs in the relationship between treatment group assignment and drug-free days in our model.
We could not test the comorbid pairings in Table 1 for differences on outcomes. However, the rates of diagnoses in the sample are informative and we discuss the composition of the sample in relation to other research findings. Torrens and colleagues (2012) note that comorbid depression and substance use disorders may be as high as 43% among treatment-seeking patients. One hundred sixteen (73%) of our participants were diagnosed with a mood disorder other than bipolar disorder and 47(29%) of these diagnoses were for Major Depression. We found no cases of substance-induced disorders, likely due to clinician judgment that psychiatric disorders in our patients have an onset prior substance related conditions. Although we cannot know this with certainty, mood-related symptoms among our patients who did not meet full criteria for major depression or bipolar disorder (mood or depressive disorders not otherwise specified) may be part of withdrawal syndromes associated with substance dependence. Finally, contingency management has been found effective among patients with psychosis and substance use disorders (Horsfall et al., 2009; Hjorthøj et al., 2009). However, patients with psychosis are routinely treated in other specialty clinics in our treatment system, and we found few patients with psychosis and substance use disorder in our sample. Therefore, we could not assess the effectiveness of contingency management for this group of patients.
Our method involved patient diagnoses generated from open clinical interviews by clinic-based psychiatrists and we do not have information on the accuracy of the diagnoses. Moderate to high levels of diagnostic inaccuracy would affect the validity of our outcomes related to comorbidity. Furthermore, we were unable to include Axis II pathology as a covariate. Any of these limitations may have affected our outcomes. Limitations notwithstanding, continuation of this line of research is important to the field.
We found one difference with regard to race, which is consistent with other research. Patients who were not Caucasian (primarily African-Americans) started treatment with less anxiety than Caucasians and reported less anxiety and stress than Caucasians in response to treatment. One explanation offered for this finding is that drug abuse among Caucasians is related primarily to psychopathology, whereas African-American drug abuse occurs most often in response to social and environmental factors (Roberts, 2000).
This project was conducted in a “real world” treatment setting and subjected to the same limitations associated with research conducted in active treatment settings. First, we were unable to retrieve information on reasons for treatment termination (e.g., dropping out or being referred to a higher level of care), and our findings could be confounded if patients disproportionately left treatment in our clinic only to immediately participate in treatment elsewhere. It is possible that patients attended treatment at different rates related to season changes. Such a phenomenon could limit the validity of the findings. The amount of time patients may have spent in treatment prior to enrolling in our partial hospitalization program could not be determined by our method of reviewing medical records. Therefore, this variable was not controlled for in our analyses. We were unable to collect clinical data using well-validated, but time-consuming instruments (Furukawa, 2010). This aspect of our method limited the dimensions of the syndromes we rated (e.g., depression). Finally, we were limited to use of self-report data, the validity of which may be open to question. However, research suggests that the validity of self-report data increases with the frequency of collection (Kimberlin & Winterstein, 2008) and we collected data on all treatment days, which may ameliorate this limitation.
Similarly, the main strengths of our project are due to its “real world” conditions. Contingency management is particularly adaptable to all modes and levels of care (Stitzer & Petry, 2006) and this feature allowed us to easily integrate the contingency management program into our intensive outpatient program. Unlike randomized trials, patients in our clinic freely accepted treatment but did not “volunteer” for research and they were not paid for participation. There were no exclusion criteria so patients were not interviewed by research staff, which can confound results of clinical trials (Clifford et al., 2000). Finally, by including all patients, our findings are likely to be quite generalizable to the population of patients with moderate-severe dual disorders in public clinics.
Conclusions
Contingency management is easily integrated into intensive outpatient programs for patients with dual disorders, and is associated with increased retention in treatment. Our findings further indicate the need for a targeted focus on reducing drug craving and psychological stress.
ACKNOWLEDGMENTS
The authors wish to thank the therapists and project staff of the Center for Psychiatric and Chemical Dependency Services at the University of Pittsburgh Medical Center for their help and professionalism in implementing this project. We also thank the patients of the partial hospitalization program for their cooperation during the operation of the project. Janis McDonald and Cindy Hurney provided indispensible expertise preparing the manuscript for publication.
Dr. Daley receives grant support from NIDA and book royalties from Oxford University Press, Hazelden Independence Press.
FUNDING
This project was supported by funding from the National Institute on Drug Abuse (NIDA; U10 DA020036).
Footnotes
DISCLOSURES
The authors report no financial relationships with commercial interests with regard to this manuscript.
Contributor Information
Thomas M. Kelly, Email: kellytm@upmc.edu.
Dennis C. Daley, Email: DaleyDC@upmc.edu.
Antoine B. Douaihy, Email: douaihya@upmc.edu.
REFERENCES
- Alessi SM, Rash C, Petry NM. Contingency management is efficacious and improves outcomes in cocaine patients with pretreatment marijuana use. Drug and Alcohol Dependence. 2011;118(1):62–67. doi: 10.1016/j.drugalcdep.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV-TR) 4th Edition. Washington DC: Author; 2000. text revision edition. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bell DC, Atkinson JS, Williams ML, Nelson R, Spence RT. The trajectory of client progress: A longitudinal pilot study. Journal of Substance Abuse Treatment. 1996;13(3):211–218. doi: 10.1016/s0740-5472(96)00046-3. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP. Enhancing the treatment attendance of mentally ill chemical abusers. Journal of Behavior Therapy and Experimental Psychiatry. 1990;21(3):205–209. doi: 10.1016/0005-7916(90)90008-9. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, Franzke LH, Longabaugh R, Beattie MC. Alcohol treatment research follow-up interviews and drinking behaviors. Journal of Studies on Alcohol. 2000;61(5):736–743. doi: 10.15288/jsa.2000.61.736. [DOI] [PubMed] [Google Scholar]
- Daley DC. Co-Occurring disorders recovery workbook: Strategies to manage substance use and mental health disorders. Independence, MO: Herald Publishing; 2011. [Google Scholar]
- Dobkin PL, DeCivita M, Paraherakis A, Gill K. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction. 2002;97:347–356. doi: 10.1046/j.1360-0443.2002.00083.x. [DOI] [PubMed] [Google Scholar]
- Drake RE, O’Neal EL, Wallach MA. A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. Journal of Substance Abuse Treatment. 2008;34(1):123–138. doi: 10.1016/j.jsat.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Furukawa TA. Assessment of mood: Guides for clinicians. Journal of Psychosomatic Research. 2010;68:581–589. doi: 10.1016/j.jpsychores.2009.05.003. [DOI] [PubMed] [Google Scholar]
- Helmus TC, Saules KK, Schoener EP, Roll JM. Reinforcement of counseling attendance and alcohol abstinence in a community-based dual-diagnosis treatment program: A feasibility study. Psychology of Addictive Behaviors. 2003;17(3):249–251. doi: 10.1037/0893-164X.17.3.249. [DOI] [PubMed] [Google Scholar]
- Hjorthoj C, Fohlmann A, Nordentoft M. Reprint of “Treatment of cannabis use disorders in people with schizophrenia spectrum disorders – A systematic review”. Addictive Behaviors. 2009;34:846–851. doi: 10.1016/j.addbeh.2009.02.003. [DOI] [PubMed] [Google Scholar]
- Horsfall J, Cleary M, Hunt GE, Walter G. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): A review of empirical evidence. Harvard Review of Psychiatry. 2009;17(1):24–34. doi: 10.1080/10673220902724599. [DOI] [PubMed] [Google Scholar]
- Humphreys K, McLellan AT. A policy-oriented review of strategies for improving the outcomes of services for substance use disorder patients. Addiction. 2011;106(12):2058–2066. doi: 10.1111/j.1360-0443.2011.03464.x. [DOI] [PubMed] [Google Scholar]
- Kelly TM, Daley DC, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addictive Behaviors. 2012;37(1):11–24. doi: 10.1016/j.addbeh.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimberlin CL, Winterstein AG. Validity and reliability of measurement instruments used in research. American Journal of Health System Pharmacy. 2008;65:2276–2284. doi: 10.2146/ajhp070364. [DOI] [PubMed] [Google Scholar]
- Kirby KC, Kerwin ME, Carpenedo CM, Rosenwasser BJ, Gardner RS. Interdependent group contingency management for cocaine-dependent methadone maintenance patients. Journal of Applied Behavior Analysis. 2008;41(4):579–595. doi: 10.1901/jaba.2008.41-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause MR, Serlin RC, Ward SE, Rony YZ, Ezenwa MO, Naab F. Testing mediation in nursing research: Beyond Baron and Kenny. Nursing Research. 2010;59(4):288–294. doi: 10.1097/NNR.0b013e3181dd26b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledgerwood DM, Alessi SM, Hanson T, Godley MD, Petry NM. Contingency management for attendance to group substance abuse treatment administered by clinicians in community clinics. Journal of Applied Behavior Analysis. 2008;41:517–526. doi: 10.1901/jaba.2008.41-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayet S, Farrell M, Ferri M, Amato L, Davoli M. Psychosocial treatment for opiate abuse and dependence. Cochrane database of systematic reviews. 2005 Jan 25;(1):CD004330. doi: 10.1002/14651858.CD004330.pub2. [DOI] [PubMed] [Google Scholar]
- McDonell MG, Srebnik D, Angelo F, McPherson S, Lowe JM, Sugar A, Ries RK. Randomized controlled trial of contingency management for stimulant use in community mental health patients with serious mental illness. The American Journal of Psychiatry. 2013;170(1):94–101. doi: 10.1176/appi.ajp.2012.11121831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman G. Likert scales, levels of measurement and the “laws” of statistics. Advances in Health Sciences Education: Theory and Practice. 2010;15(5):625–632. doi: 10.1007/s10459-010-9222-y. [DOI] [PubMed] [Google Scholar]
- Penberthy JK, Ait-Daoud N, Vaughan M, Fanning T. Review of treatment for cocaine dependence. Current Drug Abuse Reviews. 2010;3:49–62. doi: 10.2174/1874473711003010049. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Ledgerwood DM. A randomized trial of contingency management delivered by community therapists. Journal of Consulting and Clinical Psychology. 2012;80(2):286–298. doi: 10.1037/a0026826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Marx J, Austin M, Tardif M. Vouchers versus prizes. Contingency management treatment of substance abusers in community settings. Journal of Consulting and Clinical Psychology. 2005;73(6):1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Rash CJ. Contingency management treatments decrease psychiatric symptoms. Journal of Consulting and Clinical Psychology. 2013;81(5):926–931. doi: 10.1037/a0032499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Carroll KM. Contingency management is efficacious in opioid-dependent outpatients not maintained on agonist pharmacotherapy. Psychology of Addictive Behaviors. 2013;27(4):1036–1043. doi: 10.1037/a0032175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, Li R. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs. Archives of General Psychiatry. 2003;62:1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Petry NM, Weinstock J, Alessi SM. A randomized trial of contingency management delivered in the context of group counseling. Journal of Consulting and Clinical Psychology. 2011;79(5):686–696. doi: 10.1037/a0024813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CJ, Alessi SM, Petry NM. Contingency management is efficacious for cocaine abusers with prior treatment attempts. Experimental & Clinical Psychopharmacology. 2008;16(6):547–554. doi: 10.1037/a0014042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes GL, Saules KK, Helmus TC, Roll J, Beshears RS, Ledgerwood DM, Schuster CR. Improving on-time counseling attendance in a methadone treatment program: A contingency management approach. The American Journal of Drug and Alcohol Abuse. 2003;29(4):759–773. doi: 10.1081/ada-120026259. [DOI] [PubMed] [Google Scholar]
- Roberts A. Psychiatric comorbidity in white and African-American illicit substance abusers: Evidence for differential etiology. Clinical Psychology Review. 2000;20(5):667–677. doi: 10.1016/s0272-7358(99)00020-3. [DOI] [PubMed] [Google Scholar]
- Sinha R. New findings on biological factors predicting addiction relapse vulnerability. Current Psychiatry Reports. 2011;13:398–405. doi: 10.1007/s11920-011-0224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer M, Petry N. Contingency management for treatment of substance abuse. Annual Review of Clinical Psychology. 2006;2:411–434. doi: 10.1146/annurev.clinpsy.2.022305.095219. [DOI] [PubMed] [Google Scholar]
- Torrens M, Rossi PC, Martinez-Riera R, Martiez-Sanvisens D, Bulbena A. Psychiatric co-morbidity and substance use disorders: Treatment in parallel systems or in one integrated system? Substance Use & Misuse. 2012;47:1005–1014. doi: 10.3109/10826084.2012.663296. [DOI] [PubMed] [Google Scholar]
- Witbrodt J, Mertens J, Kaskutas LA, Bond J, Chi F, Weisner C. Do 12-step meeting attendance trajectories over 9 years predict abstinence? Journal of Substance Abuse Treatment. 2012;43(1):30–43. doi: 10.1016/j.jsat.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Friedmann PD, Gerstein DR. Does retention matter? Treatment duration and improvement in drug use. Addiction. 2003;98:673–684. doi: 10.1046/j.1360-0443.2003.00354.x. [DOI] [PubMed] [Google Scholar]