Abstract
Purpose
The purpose was to evaluate the effectiveness of the academic asthma education and counseling SHARP program on fostering psychosocial acceptance of asthma.
Design and Methods
This was a phase III, two-group, cluster randomized, single-blinded, longitudinal study. Students from grades 4 and 5 (N = 205) with asthma and their caregivers completed surveys at pre-intervention and at 1, 12, and 24 months post-intervention. Analysis involved multilevel modeling.
Results
All students demonstrated significant improvement in aspects of acceptance; students in SHARP demonstrated significant improvement in openness to sharing and connectedness with teachers over students in the control condition.
Practice Implications
The SHARP program offers a well-tested, effective program for psychosocial acceptance of asthma, which is welcomed by schools.
Children and adolescents with asthma, ages 9–14 years, experience increased morbidity and mortality over all other age groups across the lifespan (Akinbami, 2006; Akinbami, Moorman, & Liu, 2011; Mannino et al., 2002). They are admitted to hospitals in life-threatening situations, restricted from participating in normal life activities, and absent from school more than their peers. These adverse outcomes are often attributed to poor self-management. Nursing care outcome criteria for children with asthma have long specified that pulmonary function will be promoted with responsibility for self-care assumed (Larter, Kieckhefer, & Paeth, 1993). While some healthcare professionals assume that older school-age children and early adolescents, hereafter referred to as students, are unable or unwilling to accept responsibility for managing their condition, most healthcare providers realize that asthma is multi-factorial with individual, disease, and environmental factors that affect how well the condition is controlled.
Older school-age students and early adolescents with asthma have stated and demonstrated that accepting asthma as a chronic condition is especially difficult as they transition from elementary to middle or junior high school (Kintner, 1997, 2004, 2007; Kintner et al., 2012; Kintner & Sikorskii, 2009). Many of the issues they encounter are associated with school situations and activities. Students report experiencing a barrage of negative emotions, facing numerous psychosocial challenges, worrying about the stigmatization of the condition, feeling embarrassed by symptoms and taking medications in public, needing help with decision-making, and struggling in situations where the symptoms and treatments conflict with the normative behavior of healthy peers (Edgecombe, Latter, Peters, & Roberts, 2010; Kintner, 2004, 2007; Rhee, Belyea, & Brasch, 2010; Stewart, Masuda, Letourneau, Anderson, & McGhan, 2011; Tibosch et al., 2010). Strong anecdotal evidence points to life-threatening situations in schools resulting from students not complying with treatment protocols for reasons such as embarrassment or taunting from peers, non-cooperation or policy-based restrictions of school personnel, or age-appropriate risk-taking behavior of students.
Interdisciplinary, comprehensive, developmentally-appropriate, school-based asthma health education and counseling programs for older school-age students are needed that address the multiple factors affecting cognitive, psychosocial, and behavioral outcomes that impact condition severity, quality of life, and use of healthcare services (National Institutes of Health [NIH], 2007). A school-based, theory-driven, and evidence-guided academic health education and counseling program was developed by nurse specialists in pediatric asthma, school/family health care, and psychiatric/mental health counseling working in collaboration with other healthcare professionals and school personnel. The program, Staying Healthy–Asthma Responsible & Prepared™ (SHARP), was designed to foster acceptance of asthma by addressing cognitive, psychosocial, and behavioral aspects of condition management that impact condition severity, use of healthcare systems, and quality of life outcomes (Kintner et al., 2012; Kintner & Sikorskii, 2009). In addition, SHARP was designed to integrate into schools in such a way that it would be more likely to be embraced by schools pressured to demonstrate academic outcomes.
SHARP targets older school-age students on the cusp of growth trajectories for shifting away from parental to more personal responsibility for managing their condition as they transition from elementary to middle or junior high school. Feasibility, benefits, and efficacy of SHARP are established. Students in grades 6 to 7 with asthma, their caregivers, school personnel, and community partners were interviewed and completed satisfaction surveys to establish SHARP’s feasibility (Kintner et al., 2012). A single-group, pre-post and 12-month follow-up study confirmed SHARP’s benefits using students in grades 6–7 with asthma on cognitive, psychosocial, behavior, and quality of life outcomes (Kintner et al., 2012). Efficacy of SHARP was established using a two-group, pretest–posttest, randomized clinical trial with treatment and usual care control groups of students in grades 4–6 with asthma (Kintner & Sikorskii, 2009).
This paper presents results of a phase III randomized clinical trial conducted to evaluate the effectiveness and impact of SHARP on cognitive, psychosocial, and behavioral factors that impact asthma severity/control, use of healthcare services, and quality-of-life outcomes including school attendance/absenteeism. The age range for this study was determined by the grade at which students in the target school district transition into middle school. Students transitioned into middle school in the sixth grade; therefore, students with asthma enrolled in the fourth and fifth grades were invited to participate. Cognitive, behavior, quality of life, asthma severity/control, quality of life, and use of healthcare services outcomes are reported elsewhere.
Purpose
The purpose of this paper is to report the effectiveness of SHARP on fostering psychosocial acceptance of asthma in fourth- and fifth-grade students with asthma at 1, 12, and 24 months post-intervention. When evaluating effectiveness, students enrolled in the academic health education and counseling program being evaluated are compared to students enrolled in an attention-control or condition-control program. Because all students enrolled in the study were diagnosed with asthma, we elected to use a well-established, non-academic asthma health education and counseling program for comparison. We hypothesized that compared to students enrolled in elementary schools who received a condition-control program; students in elementary schools that received SHARP would demonstrate equivalent or increased psychosocial acceptance of asthma. Students randomized to the condition-control group received the non-academic asthma health education and counseling program Open Airways for Schools (Clark et al., 2004), a curriculum that is disseminated through the American Lung Association.
Acceptance of Asthma Framework
The acceptance of asthma model (AAM), developed through a series of qualitative and quantitative studies (Kintner, 2004, 2007) from an ecological approach (Bronfenbrenner, 1979) within a lifespan development perspective (Santrock, 2010), guided development and evaluation of the SHARP program (Kintner et al., 2012; Kintner & Sikorskii, 2009). The model specifies that asthma knowledge and reasoning impact psychosocial factors (e.g., acceptance of asthma) that subsequently impact behavioral factors to ameliorate asthma severity and control, use of healthcare services, and quality-of-life outcomes. Individual, disease, and environmental influences impact children and adolescents throughout the acceptance process.
Acceptance of asthma is a latent variable defined as the expressed desire to take possession of one’s chronic condition (Kintner, 1997, 2004, 2007; Kintner et al., 2012; Kintner & Sikorskii, 2009). Indicators of acceptance include: (a) openness to learning about the condition or expressed receptivity to new information, (b) openness to sharing the conditions with others or expressed willingness to share one’s feelings and confidences about the illness, thus making the condition publicly known, (c) vigilance in monitoring and managing the condition by maintaining a quality of being watchful and attentive to warning signs and symptoms, (d) taking control over illness-imposed limitations by assuming responsibility for regulating one’s condition, and (e) connectedness with members of one’s social network by feeling united with others sharing similar life experiences.
Methods
This cluster-randomized, single-blinded clinical trial used a two-group, longitudinal, prospective design. The study was in compliance with the Helsinki Declaration, the Health Insurance Portability and Accountability Act, and the Family Education Rights and Privacy Act. Human subjects’ approvals were obtained through three institutional review boards.
Sample and Sampling
Participants consisted of fourth- and fifth-grade students, ages 9–12 years, diagnosed with asthma and their caregivers. Eligibility criteria for students included a diagnosis of asthma, availability to participate in study-related activities, verbal and written assent, permission of the caregiver, and ability to academically perform in English at or near grade level. Eligibility criteria for caregivers included caring for the student with asthma, availability to participate in study-related activities, verbal and written consent, and the ability to understand English.
A convenience sampling method was used. Students were recruited in fall 2009 and 2010 from 23 elementary schools located in a diverse, primarily minority, moderately sized, medically under-served, low socioeconomic, inner-city community. The schools were matched based on school enrollment numbers, standardized reading and math scores, free/reduced lunch eligibility, and racial/ethnic proportions prior to randomization. The interventions were delivered in spring 2010 and 2011. The unit of analysis was the student.
Of the 2,770 student/caregiver dyads screened for eligibility, 2,554 dyads were excluded primarily due to lack of an asthma diagnosis, 216 dyads were enrolled and completed preprogram assessment, and 205 dyads were randomized to one of the two programs. All students allocated to SHARP (n = 117) and the control condition (n = 88) received their respective program. Data were collected at four time points. Retention was 83% (n = 168) at 24 months post-program. Several students who completed baseline surveys left the district prior to randomization and delivery of the programs. A CONSORT chart providing eligibility, screening, enrollment, randomization, participation, and follow-up numbers is contained in a manuscript currently in review for publication.
Data Collection
Data were collected from participants using audio-linked, password-protected electronic databases loaded on password-protected and encrypted laptop computers. Pairs of data collectors, blinded to the randomization, collected data from dyads in their homes at baseline pretest, 1-month posttest, and 12- and 24-month follow-up. All data collection sessions were digitally audio-recorded for safety and quality assurance. Data collectors completed standardized checklists before leaving the site, and data collectors and designated research team members reviewed audio-recorded sessions according to established protocols using a standardized checklist to confirm that policies and procedures were followed. Students and caregivers were offered a cash award (Kintner et al., 2012) of $15 each or $30 per dyad at each data collection time point to acknowledge their time and effort in completing surveys. Individual de-identified data entry files labeled using coded identification numbers were merged into one relational systems file before raw data were downloaded into SPSS for analysis. All participant-signed documents were kept separate from the data. No unanticipated events were reported.
Interventions
Both asthma education and counseling programs were delivered on a weekly basis, February through April, by trained, certified elementary school teachers in schools during instructional time. Students enrolled in schools randomized to SHARP received 10, 50-minute workbook-guided sessions, and members of their social network were invited to participate in a community component (Kintner et al., 2012; Kintner & Sikorskii, 2009). Students enrolled in schools randomized to Open Airways for Schools (OAS) received six, 50-minute lessons and took home handouts for their caregivers (Clark et al., 2004; Evans et al., 1987). SHARP stipulates that certified elementary school teachers be trained to deliver the program (a) because elementary school teachers are educated to instruct students in meeting grade-level academic benchmarks and performance-based assessment in diverse subject matter using a variety of techniques and methods and (b) so that content is viewed as part of school work to increase acceptability by school personnel, students, and caregivers. Teachers were trained to deliver OAS to standardize delivery of the programs for comparison. Counseling aspects of both programs are summarized below.
Staying Healthy-Asthma Responsible & Prepared™
Designed as an academic program, SHARP integrates into existing school curricula as an elective course for grades 4–7 (Kintner et al., 2012; Kintner & Sikorskii, 2009). The program is offered as a pull-out program scheduled during students’ enrichment periods or recess, music, art, or PE/Gym classes. The program enhances skills in reading, writing, and arithmetic by including spelling words, math problems, reading and writing assignments, demonstrations, and learning activities from biology, psychology, and sociology. Counseling aspects encourage students to share their thoughts and feelings about what it is like for them to live with asthma. The acceptance of asthma model is used to help students process their thoughts and feelings through the use of creative artistic and written expressions, small group discussion, and guided role-playing. Aspects of the acceptance model explicitly link across sessions. Students are offered the personal choice to accept responsibility for their asthma by setting personal goals early in the program and are then provided a structured process to reach their goals. Students invite members of their supportive social network (e.g., caregivers, family members, friends, classmates, and school personnel) to attend the community component.
Open Airways for Schools
Written at the second- to third-grade level, OAS aims to enable students with asthma ages 8–11 years to take care of their condition (Bruzzese, Markman, Appel, & Webber, 2001; Clark et al., 2004; Evans et al., 1987; Velsor-Friedrich, Pigott, & Srof, 2005). By completion of the program, students should have gained knowledge to be able to take steps to prevent symptoms, recognize warning signs and respond appropriately, discuss problems with others, and feel confident taking care of their asthma. Threads are woven throughout the sessions to deliver messages that asthma is treatable, symptoms do not have to be a crisis, prescribed medications are needed, solutions to problems can be found, and children can live normal and active lives. OAS is disseminated to individuals and groups for use in schools with students enrolled in grades 2–5. Personal observation confirms that the program has been used with students enrolled in grades K-12.
Roles of Nurse Specialists
School nurses identified 10 certified elementary school teachers, eight participating per year, who were randomly assigned and trained to deliver one of the two programs. Teachers knew little about asthma and had limited experience counseling students with asthma prior to participating in training sessions. Nurse specialists in pediatric asthma and psychiatric/mental health counseling conducted the initial program-specific training sessions and then maintained communication with the teachers during weekly meetings that were used to reflect on delivered sessions and to prepare for upcoming sessions. Although teachers rarely required additional asthma information following the initial training, nurse specialists were available to provide clarifying information and developmentally appropriate prompts or scripts as needed.
Fidelity
All SHARP sessions and OAS lessons were audio-recorded for fidelity and quality assurance. Teachers completed session-/lesson-specific checklists before leaving the classroom following each session/lesson. Teachers used a second series of session-/lesson-specific checklists to review audio-recordings of their sessions/lessons according to protocol. Finally, nurse specialists used session-/lesson-specific checklists to review the first session/lesson delivered by each teacher, and all sessions/lessons were reviewed by designated research assistants to confirm that they were delivered according to protocol. All students received 100% of their respective programs.
Instruments
Self-report measures were used. Internal consistency reliability and stability, construct validity, readability, and age appropriateness were considered when selecting instruments. Caregivers completed the General Health History Survey and four additional instruments. Students completed the Acceptance of Asthma Questionnaire and four additional instruments.
General Health History Survey (GHHS)
This is a 39-item instrument (Kintner et al., 2012) used to collect demographic (e.g., sex, age, grade in school, race/ethnicity, and family structure) and asthma-related information (e.g., age at onset of symptoms and diagnosis, and prescribed medications). Three items are used to compute the family’s socioeconomic status.
Acceptance of Asthma Questionnaire (AAQ)
Completed by students, this is a two-part, 5-point, Likert-type, self-report survey measuring aspects of an individual’s level of acceptance of asthma (Kintner, 2007). Response options range from 1 (totally disagree) to 3 (unsure) and 5 (totally agree). Negatively worded items are reverse scored. Part 1 contains 4 scales measuring levels of openness to learning about the condition, openness to sharing the condition with others, vigilance in monitoring for symptoms, and taking control over illness-imposed limitations. Part 2 contains 5 scales that consider one’s asthma when measuring levels of connectedness with friends, classmates, and school/classroom and physical education (PE) or gym teachers. When confirming psychometric properties, items capturing connectedness with classmates grouped by positively and negatively worded items revealing two unique factors. Whereas higher scores for positively worded classmate items are interpreted as more supportive relationships; higher scores for negatively worded classmate items are interpreted as less isolating or stigmatizing relationships. Mean scores computed for each scale have the potential to range from 1.00 to 5.00. Scale summaries for this sample including the number of items per scale as well as the number of students who completed the scale, minimum and maximum scores, item to total correlations, Cronbach’s standardized alpha correlation coefficient, exploratory factor loadings, and percent of variance explained at baseline pretest, 1-month posttest, and 12- and 24-month follow-up are presented in Tables 1–2.
Table 1.
AAQ Scale Summaries, Internal Consistency Reliability, and Exploratory Factor Analysis at Four Time Points for Open to Learning and Sharing, Vigilance, and Taking Control
| Scale | Items | N | Min-Max Scores | Item to Total Correlations | Standardized Alpha Coefficient | Factor Loadings | % Variance Explained |
|---|---|---|---|---|---|---|---|
| Open to Learning | 8 | ||||||
| Baseline Pretest | 205 | 1.25 to 5.00 | .31 to .68 | .81 | .36 to .76 | 43.30 | |
| 1-month Posttest | 199 | 2.13 to 5.00 | .38 to .60 | .80 | .50 to .76 | 41.84 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .53 to .69 | .86 | .63 to .81 | 50.77 | |
| 24-month Follow-up | 167 | 1.25 to 5.00 | .52 to .74 | .88 | .61 to .83 | 54.97 | |
| Open to Sharing | 5 | ||||||
| Baseline Pretest | 205 | 1.00 to 5.00 | .35 to .55 | .70 | .56 to .77 | 45.12 | |
| 1-month Posttest | 199 | 1.00 to 5.00 | .46 to .68 | .82 | .62 to .81 | 58.77 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .57 to .73 | .84 | .71 to .85 | 60.75 | |
| 24-month Follow-up | 167 | 1.00 to 5.00 | .50 to .72 | .81 | .65 to .87 | 57.15 | |
| Vigilance | 6 | ||||||
| Baseline Pretest | 205 | 1.00 to 5.00 | .31 to .52 | .65 | .51 to .72 | 36.66 | |
| 1-month Posttest | 199 | 1.50 to 5.00 | .43 to .51 | .74 | .54 to .79 | 42.33 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .48 to .59 | .79 | .65 to .73 | 48.25 | |
| 24-month Follow-up | 167 | 1.00 to 5.00 | .36 to .70 | .78 | .57 to 82 | 48.00 | |
| Taking Control | 5 | ||||||
| Baseline Pretest | 205 | 1.00 to 5.00 | .30 to .61 | .76 | .48 to .82 | 51.37 | |
| 1-month Posttest | 199 | 1.40 to 5.00 | .36 to .64 | .77 | .54 to .80 | 52.19 | |
| 12-month Follow-up | 167 | 1.60 to 5.00 | .51 to .74 | .85 | .64 to .87 | 61.91 | |
| 24-month Follow-up | 167 | 1.00 to 5.00 | .30 to .69 | .75 | .45 to .84 | 51.24 |
NOTE: AAQ – Acceptance of Asthma Questionnaire
Table 2.
AAQ Scale Summaries, Internal Consistency Reliability, and Exploratory Factor Analysis at Four Time Points for Connectedness with Peers and Teachers
| Scale | Items | N | Min-Max Scores | Item to Total Correlations | Standard Alpha Coefficient | Factor Loadings | % Variance Explained |
|---|---|---|---|---|---|---|---|
| Connected with Friends | 6 | ||||||
| Baseline Pretest | 123 | 1.00 to 5.00 | .48 to .55 | .72 | .65 to .82 | 43.58 | |
| 1-month Posttest | 199 | 1.00 to 5.00 | .50 to .67 | .83 | .66 to .80 | 53.50 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .41 to .68 | .82 | .57 to .83 | 53.35 | |
| 24-month Follow-up | 167 | 1.33 to 5.00 | .41 to .65 | .79 | .54 to .80 | 49.17 | |
| Connected with Classmates-Neg | 6 | ||||||
| Baseline Pretest | 121 | 1.33 to 5.00 | .36 to .51 | .72 | .54 to .70 | 41.30 | |
| 1-month Posttest | 199 | 1.17 to 5.00 | .42 to .55 | .74 | .51 to .75 | 43.40 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .44 to .56 | .76 | .60 to .74 | 45.42 | |
| 24-month Follow-up | 167 | 1.00 to 5.00 | .46 to .59 | .78 | .58 to .74 | 46.88 | |
| Connected with Classmates-Pos | 5 | ||||||
| Baseline Pretest | 121 | 1.00 to 5.00 | .45 to .58 | .75 | .65 to .76 | 49.55 | |
| 1-month Posttest | 199 | 1.00 to 5.00 | .51 to .68 | .81 | .67 to .83 | 57.31 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .36 to .72 | .82 | .47 to .87 | 59.07 | |
| 24-month Follow-up | 167 | 1.00 to 5.00 | .51 to .71 | .82 | .68 to .84 | 57.67 | |
| Connected with School Teacher | 6 | ||||||
| Baseline Pretest | 122 | 1.40 to 5.00 | .29 to .50 | .70 | .33 to .81 | 38.11 | |
| 1-month Posttest | 199 | 1.00 to 5.00 | .4 to .52 | .71 | .49 to .81 | 39.88 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .49 to .62 | .80 | .66 to .77 | 49.39 | |
| 24-month Follow-up | 166 | 1.00 to 5.00 | .44 to .62 | .79 | .57 to .77 | 48.00 | |
| Connected with PE Teacher | 6 | ||||||
| Baseline Pretest | 122 | 1.00 to 5.00 | .35 to .53 | .73 | .59 to .71 | 41.83 | |
| 1-month Posttest | 199 | 1.00 to 5.00 | .46 to .66 | .80 | .64 to .78 | 49.62 | |
| 12-month Follow-up | 167 | 1.00 to 5.00 | .58 to .66 | .83 | .68 to 80 | 54.41 | |
| 24-month Follow-up | 165 | 1.00 to 5.00 | .55 to .71 | .86 | .67 to .81 | 59.12 |
NOTE: AAQ – Acceptance of Asthma Questionnaire; NEG – Reverse-scored Negatively Worded Classmate Items; POS – Positively Worded Classmate Items; PE – Physical Education
Data Processing and Analysis
SPSS for Windows 19 (IBM SPSS, 2010) was used to compute descriptive statistics. An overview of the multiple imputation method used to account for missing data and multilevel modeling process used to evaluate the effect of SHARP is provided.
Missing data
The R Amelia package (Honaker & King, 2010) was used to perform multiple imputations to account for missing data following best-practice recommendations (Graham, 2009). Twenty data sets with imputed values for missing data were created. Parameter estimates from the 20 models were combined using Rubin’s formulas (Rubin, 1987) and degrees of freedom and inferential tests were derived. Sensitivity analysis (McKnight, McKnight, Sidani, & Figueredo, 2007) in which models were fit using all available data was used to confirm results for the models fit with imputed data.
Multilevel models
Multilevel models that were fit using the R lme4 package (Bates, Maechler, & Bolker, 2013; Gelman & Hill, 2007) contained two levels: time points and participants. Several viable unconditional growth models (i.e., models with time variables representing longitudinal change and no other independent variables) were fit using longitudinal model building recommendations (Singer & Willett, 2003) and then compared using the Akaike Information Criterion (AIC) and guidelines from Burnham and Anderson (2002) to assess which model was the best representation of longitudinal change for each outcome. After establishing the best unconditional growth model, person-level variables (e.g., intervention condition) and then covariates (e.g., age, grade, and sex/gender) were added. Simple slope contrasts (Bauer & Curran, 2005) at each assessment point were computed using the R Contrast package (Kuhn, Weston, Wing, & Forester, 2011).
Results
The sample consisted of 205 fourth- and fifth-grade students, ages 9–12 years (M = 10.02, SD = .70), diagnosed with asthma and their caregivers. Sixty percent were male. Students were primarily Black (43%) or mixed Black and White (13%), of single parent households (69%), and with lower (59%) to low-middle (34%) socioeconomic backgrounds. Severity of asthma ranged from intermittent and mild persistent (55%) to moderate (37%) and severe (8%) persistent. Caregivers, ages 19–69 years, (M = 39, SD = 8) were primarily female (88%) and biological parents (88%).
Model Development
Data for all covariates were complete with the exception of percentage of overall school writing proficiency (9.76%) and severity of asthma (2.93%). The acceptance outcomes of open to learning and sharing, vigilance, and taking control had 3.90% missing data at baseline pretest, 2.93% at posttest, 19.02% at 12-month follow-up, and 18.54% at 24-month follow-up. The outcomes of the connectedness scales had 43.5% missing data at baseline pretest due to skip patterns introduced per the request of data collectors for students demonstrating what the data collectors deemed limited attention spans or lower reading abilities. When offered the choice by the data collectors, about 50% of the students elected to skip the connectedness items at baseline. Skip patterns were removed when trained educators deemed them unnecessary. Missing data at posttest and 12-month and 24-month follow-up was 2.93%, 19.02%, and 18.54%, respectively. Sensitivity analysis in which all of the models were fit using all available data indicated that the models fit with imputed data (N = 205) held up well despite the substantially reduced sample size (n = 99–178).
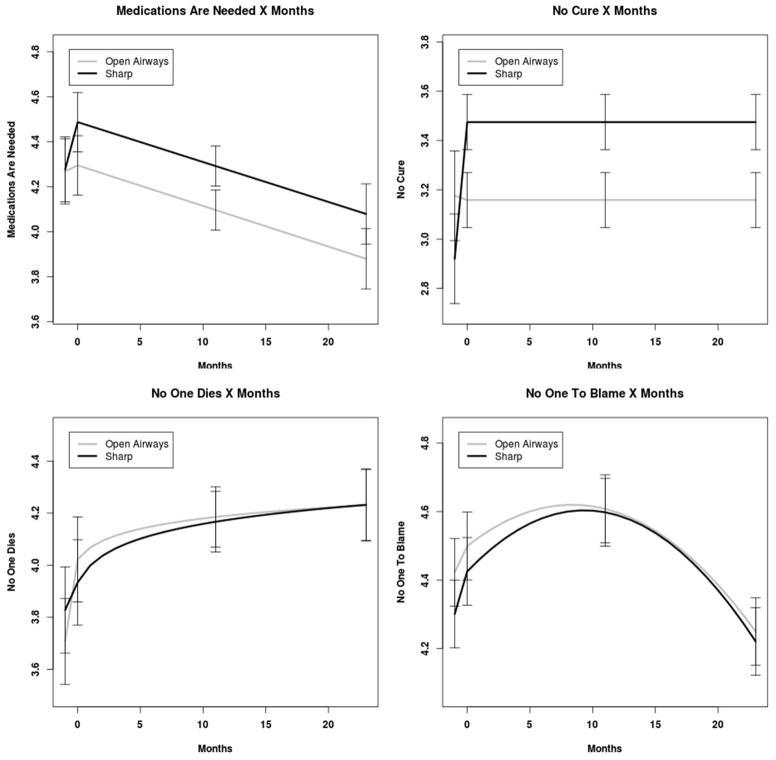
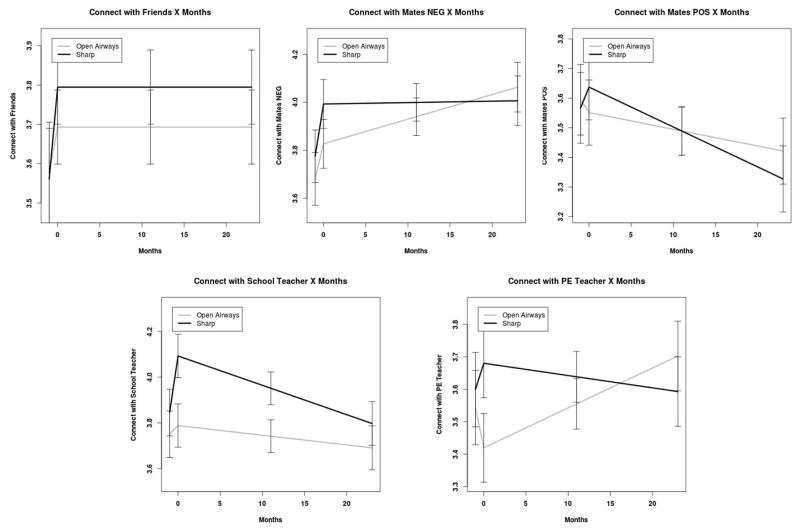
Means and standard deviations for the SHARP and OAS participants are presented in Table 3. Parameter estimates for openness to learning and sharing, vigilance, taking control, and connectedness with others are presented in Tables 4–7. Fitted values for the models with standard errors of the difference for simple slope estimates of SHARP and Open Airways participants at each assessment point are displayed in Figures 1–2. Main effects are summarized below.
Table 3.
Acceptance of Asthma Means (SD) for Open Airways and SHARP Participants at Each Assessment
| Outcome | Baseline Pretest | 1-month posttest | 12-month follow-up | 24-month follow-up |
|---|---|---|---|---|
| Open to Learning | ||||
| Open Airways | 4.02 (0.69) | 4.26 (0.65) | 4.04 (0.84) | 3.98 (0.92) |
| SHARP | 3.81 (0.79) | 4.31 (0.66) | 4.06 (0.76) | 3.90 (0.86) |
| Open to Sharing | ||||
| Open Airways | 2.99 (1.01) | 3.29 (1.21) | 2.97 (1.19) | 3.28 (1.10) |
| SHARP | 2.91 (1.03) | 3.60 (1.05) | 3.28 (1.17) | 3.06 (1.17) |
| Vigilance | ||||
| Open Airways | 3.43 (0.75) | 3.86 (0.80) | 3.69 (0.86) | 3.75 (0.84) |
| SHARP | 3.21 (0.85) | 3.74 (0.84) | 3.68 (0.86) | 3.56 (0.93) |
| Taking Control | ||||
| Open Airways | 3.61 (1.06) | 3.99 (0.98) | 3.95 (0.99) | 4.16 (0.79) |
| SHARP | 3.72 (0.87) | 4.02 (0.76) | 3.95 (0.93) | 4.15 (0.79) |
| Connected with Friends | ||||
| Open Airways | 3.78 (0.80) | 3.75 (1.05) | 3.65 (1.15) | 3.78 (1.00) |
| SHARP | 3.48 (0.99) | 3.81 (0.98) | 3.75 (0.89) | 3.77 (0.85) |
| Connected with Classmates - Negative | ||||
| Open Airways | 3.86 (0.94) | 3.87 (0.92) | 3.86 (0.90) | 4.16 (0.87) |
| SHARP | 3.83 (0.95) | 3.93 (0.98) | 3.95 (1.00) | 4.03 (0.94) |
| Connected with Classmates - Positive | ||||
| Open Airways | 3.72 (0.97) | 3.55 (1.06) | 3.53 (1.01) | 3.51 (1.03) |
| SHARP | 3.46 (0.96) | 3.62 (1.00) | 3.37 (1.00) | 3.33 (0.95) |
| Connected with Classroom Teachers | ||||
| Open Airways | 4.11 (0.73) | 3.95 (0.81) | 3.72 (1.00) | 3.91 (0.89) |
| SHARP | 3.68 (0.85) | 4.01 (0.81) | 3.78 (0.84) | 3.75 (0.90) |
| Connected with PE/Gym Teachers | ||||
| Open Airways | 3.74 (0.91) | 3.59 (1.02) | 3.56 (1.00) | 3.91 (0.95) |
| SHARP | 3.44 (0.88) | 3.63 (0.93) | 3.41 (1.01) | 3.52 (1.00) |
NOTE: SHARP – Staying Healthy–Asthma Responsible & Prepared™; PE –Physical Education
Table 4.
Parameter Estimates for Acceptance of Asthma in Openness to Learning and Sharing
| Open to Learning | Open to Sharing | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Parameter | B | SE | df | t | p | B | SE | df | t | p |
| Intercept | 2.29 | 0.21 | 168 | 10.76 | < .001 | 2.01 | 0.24 | 151 | 8.23 | < .001 |
| Baseline | 0.51 | 0.04 | 168 | 12.70 | < .001 | 0.57 | 0.05 | 153 | 12.52 | < .001 |
| Female | −0.02 | 0.06 | 163 | −0.38 | .706 | −0.11 | 0.09 | 172 | −1.18 | .238 |
| Age of student | −0.10 | 0.06 | 177 | −1.70 | .090 | −0.07 | 0.09 | 172 | −0.75 | .452 |
| Fifth grade | −0.05 | 0.09 | 176 | −0.59 | .556 | −0.07 | 0.13 | 169 | −0.57 | .572 |
| African American | 0.00 | 0.07 | 154 | 0.01 | .989 | 0.07 | 0.10 | 174 | 0.74 | .460 |
| Hispanic | −0.01 | 0.10 | 167 | −0.05 | .960 | −0.06 | 0.15 | 153 | −0.42 | .676 |
| Time since diagnosis | 0.02 | 0.01 | 166 | 1.54 | .125 | 0.02 | 0.02 | 172 | 1.13 | .258 |
| Stimuli of allergies | −0.07 | 0.08 | 174 | −0.80 | .422 | −0.36 | 0.12 | 162 | −2.95 | .004* |
| Stimuli of exercise | 0.04 | 0.07 | 135 | 0.49 | .624 | 0.01 | 0.11 | 145 | 0.07 | .944 |
| Prescribed long-acting bronchodilator | −0.13 | 0.08 | 166 | −1.59 | .114 | −0.19 | 0.12 | 169 | −1.52 | .131 |
| Prescribed inhaled steroid | 0.01 | 0.07 | 154 | 0.08 | .934 | 0.07 | 0.10 | 165 | 0.75 | .454 |
| Family Socioeconomic status | −0.00 | 0.00 | 177 | −1.96 | .051* | −0.00 | 0.00 | 168 | −0.26 | .794 |
| Reading Proficient %Overall | 0.01 | 0.01 | 154 | 1.20 | .234 | −0.00 | 0.01 | 174 | −0.27 | .788 |
| Writing Proficient %Overall | 0.00 | 0.01 | 129 | 0.06 | .953 | 0.01 | 0.01 | 142 | 1.28 | .203 |
| Math Proficient %Overall | −0.01 | 0.01 | 166 | −1.76 | .080 | −0.01 | 0.01 | 149 | −1.00 | .320 |
| Severity of Asthma | 0.02 | 0.02 | 128 | 1.01 | .314 | 0.03 | 0.03 | 133 | 1.18 | .242 |
| SHARP Participation | 0.14 | 0.09 | 175 | 1.50 | .134ns | 0.27 | 0.14 | 183 | 1.98 | .050* |
| Pre-post | 0.26 | 0.09 | 177 | 2.95 | .004* | 0.35 | 0.13 | 181 | 2.70 | .008* |
| SHARP Participation by Pre-post | 0.23 | 0.12 | 171 | 1.90 | .059ns | 0.35 | 0.17 | 180 | 1.99 | .048* |
| Months | −0.01 | 0.00 | 170 | −3.61 | < .001* | −0.06 | 0.02 | 149 | −2.71 | .008* |
| SHARP Participation by Month | −0.00 | 0.01 | 170 | −0.63 | .531ns | 0.01 | 0.03 | 150 | 0.50 | .616ns |
p < .05,
Non-significant
NOTE: SHARP – Staying Healthy–Asthma Responsible & Prepared™
Table 7.
Parameter Estimates for Acceptance of Asthma in Connectedness with School Teachers
| Classroom Teachers | PE/Gym Teachers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Parameter | B | SE | df | t | p | B | SE | df | t | p |
| Intercept | 1.79 | 0.24 | 64 | 7.49 | < .001 | 1.07 | 0.28 | 60 | 3.89 | < .001 |
| Baseline | 0.58 | 0.05 | 36 | 11.20 | < .001 | 0.63 | 0.05 | 39 | 11.68 | < .001 |
| Female | −0.13 | 0.07 | 148 | −1.99 | .048* | −0.25 | 0.08 | 127 | −3.30 | .001* |
| Age of student | 0.00 | 0.07 | 102 | 0.01 | .992 | −0.09 | 0.09 | 62 | −1.00 | .321 |
| Fifth grade | −0.10 | 0.11 | 65 | −0.88 | .384 | 0.19 | 0.12 | 68 | 1.56 | .124 |
| African American | 0.02 | 0.08 | 99 | 0.27 | .784 | 0.06 | 0.09 | 88 | 0.67 | .507 |
| Hispanic | −0.09 | 0.12 | 96 | −0.74 | .459 | −0.09 | 0.13 | 88 | −0.66 | .509 |
| Time since diagnosis | −0.00 | 0.02 | 90 | −0.27 | .786 | 0.03 | 0.02 | 93 | 1.64 | .105 |
| Stimuli of allergies | −0.06 | 0.09 | 124 | −0.68 | .496 | 0.01 | 0.10 | 142 | 0.10 | .920 |
| Stimuli of exercise | −0.02 | 0.08 | 101 | −0.29 | .771 | 0.06 | 0.09 | 112 | 0.72 | .470 |
| Prescribed long-acting bronchodilator | 0.08 | 0.10 | 97 | 0.79 | .431 | 0.02 | 0.11 | 99 | 0.21 | .831 |
| Prescribed inhaled steroid | 0.00 | 0.08 | 90 | 0.04 | .965 | 0.13 | 0.09 | 73 | 1.39 | .169 |
| Family Socioeconomic status | −0.00 | 0.00 | 133 | −1.12 | .266 | −0.00 | 0.00 | 73 | −1.61 | .111 |
| Reading Proficient %Overall | −0.02 | 0.01 | 109 | −1.84 | .069 | −0.01 | 0.01 | 87 | −1.24 | .220 |
| Writing Proficient %Overall | 0.01 | 0.01 | 70 | 1.78 | .080 | 0.02 | 0.01 | 54 | 2.11 | .040* |
| Math Proficient %Overall | −0.01 | 0.01 | 57 | −1.19 | .237 | −0.03 | 0.01 | 75 | −2.45 | .017* |
| Severity of Asthma | 0.02 | 0.02 | 98 | 0.94 | .349 | 0.01 | 0.03 | 67 | 0.54 | .593 |
| SHARP Participation | 0.26 | 0.11 | 107 | 2.43 | .017* | 0.23 | 0.12 | 123 | 2.01 | .046* |
| Pre-post | −0.01 | 0.12 | 66 | −0.09 | .929ns | −0.10 | 0.12 | 97 | −0.79 | .434ns |
| SHARP Participation by Pre-post | 0.26 | 0.15 | 69 | 1.73 | .088ns | 0.20 | 0.16 | 92 | 1.25 | .213ns |
| Months | −0.00 | 0.00 | 128 | −1.01 | .313ns | 0.01 | 0.01 | 117 | 2.07 | .041* |
| SHARP Participation by Month | −0.01 | 0.01 | 121 | −1.01 | .314ns | −0.02 | 0.01 | 136 | −2.23 | .027* |
p < .05,
Non-significant
NOTE: SHARP – Staying Healthy–Asthma Responsible & Prepared™; PE – Physical Education
Figure 1.
Figure 2.
Openness to Learning
We observed a main effect for the pretest-posttest (t[177] = 2.95, p = .004) change in openness to learning, indicating that there was an average increase from pre- to post-intervention for all participants, and a main effect for months (t[170] = −3.61, p < .001), indicating that there was a decrease in openness to learning across posttest assessments for all participants. The SHARP participation by pre-post interaction approached significance (t[171] = 1.90, p = .059), indicating that SHARP participants exhibited a potentially greater increase between pretest and posttest assessments.
Openness to Sharing
We observed a main effect for the pretest-posttest (t[181] = 2.70, p = .008) change in openness to sharing, indicating that there was an average increase from pre- to post-intervention for all participants, and a main effect for months (t[149] = −2.71, p = .008), indicating that there was a decrease in openness to sharing across post-test assessments for all participants. The SHARP main effect was significant (t[183] = 1.98, p = .050), indicating that SHARP participants exhibited higher levels of openness to sharing at posttest. The SHARP participation by pre-post interaction was significant (t[180] = 1.99, p = .048), indicating that the SHARP participants exhibited a greater increase between pretest and posttest assessments.
Vigilance and Taking Control
We observed a main effect for the pretest-posttest change in vigilance (t[182] = 4.10, p < .001) and taking control (t[173] = 4.89, p < .001), indicating that there was an average increase in vigilance and taking control from pre- to post-intervention for all participants. The increases were sustained over time.
Connectedness with Peers and Teachers
The main effects for the pretest-posttest change in connectedness with friends and classmates were not significant indicating that there was limited change in connectedness with peers from pre- to post-intervention for all participants. The SHARP main effects for connectedness with classroom teachers (t[107] = 2.43, p = .017) and PE/Gym teachers (t[123] = 2.01, p = .046) were significant, indicating that SHARP participants exhibited higher levels of connectedness with classroom and PE/Gym teachers at posttest compared to the control condition.
Discussion
The effectiveness of SHARP, compared to the control condition, on fostering psychosocial acceptance of asthma in older school-age students with asthma was demonstrated through (a) increased levels of openness to learning about and sharing the condition from baseline to posttest and as students transitioned into middle school, (b) equivalent increased levels of vigilance and taking control from baseline to posttest that were sustained over time, and (c) increased levels of connectedness with teachers from baseline to posttest.
Using multilevel modeling to examine the psychosocial growth and development of students as they transitioned from elementary into middle school was exceedingly valuable. For example, students were open to learning during delivery of the program; however, openness to learning appeared to diminish after students learned what they thought they needed to know. Openness to sharing also increased during delivery of the program; however, as students became more comfortable with their condition, the need to share with others became increasingly selective. Vigilance in monitoring and taking control of the condition increased and remained stable over time for all students as predicted.
Although there was limited change in connectedness with friends and classmates from pre- to post-intervention for all students, feelings of connectedness with members of their social network evolved as students transitioned into middle school. This is understandable knowing that several elementary schools merged into much larger middle schools. Reverse-scored, negatively-worded feelings of connectedness with classmates sharply increased during delivery of the programs for all students and then remained stable for SHARP participants and trended upward overtime for OAS participants, indicating that students with asthma felt less stigmatized following their respective programs. Positively worded feelings indicative of supportive relationships waned as peers shifted throughout the day from one class to another in middle school. Although students were encouraged to invite all members of their social network to the community programs, only a few close friends of one student with asthma and one school secretary attended.
Connectedness with school teachers functioned as predicted. Students with one teacher per grade level in elementary school felt connected with their teachers. Students with several teachers throughout the day in middle schools naturally felt less connected. Connectedness with PE/Gym teacher over time must be interpreted with caution due to protocol confusion at 24-months follow-up. When students shared that they no longer had PE/Gym class, some of the data collectors instructed students to select “unsure” rather than encouraging students to respond in a more general manner about how they felt about PE/Gym teachers overall.
SHARP seeks to provide anticipatory guidance to students in preparation for transition to middle school by role-playing who to tell, what to say, when to share, and how to present asthma information so that other people (i.e., peers, school teachers, and club/sports youth leaders) will be better able to respond and meet their needs (Kintner et al., 2012, Kintner & Sikorskii, 2009). School board members, administrators, principals, and teachers are requesting an academic version of SHARP for classmates of students with asthma. A classmate program might have greater impact on students’ perceptions of connectedness with peers and school personnel than the SHARP program for students with asthma alone.
Connectedness with peers and teachers must be interpreted with caution due to missing data secondary to skip patterns introduced during data entry at baseline as described above and potentially unequal group sizes following randomization. While we acknowledge the possibility of bias in the presence of large amounts of missing data at baseline for the connectedness scales, the case-wise exclusion or discarding of large amounts of non-missing data would be even more problematic. Although group membership was impacted when the target school district consolidated schools, any apparent or actual differences between the groups was controlled using multilevel modeling.
Findings of this study advance nursing theory and evidence-based practice by (a) offering a reliable and valid instrument to measure acceptance of asthma and (b) confirming the effectiveness of the academic SHARP program on fostering psychosocial acceptance of asthma in older school-age students with the condition. Recommendations for future research include adapting the community program of classmates of students with asthma, continuing assessment of connectedness with members of one’s social network over time, and conducting a series of dissemination and implementation level studies to determine cost-effectiveness and system-wide outcomes of SHARP in school districts and communities across the country.
How might this information affect nursing practice?
Pediatric nurse specialists seeking to advance theory and evidence-based practice now have a feasible, beneficial, efficacious, and effective academic asthma health education and counseling program for older school-age students that (a) is age and developmentally appropriate, (b) welcomed by school districts when delivered by nurse-supervised school teachers (Kintner et al., 2012), and (c) addresses psychosocial factors that impact morbidity, mortality, and quality-of-life outcomes. The academic approach used for SHARP serves as a model for introducing education and counseling programs for other health-related conditions such as epilepsy and diabetes into school settings.
Table 5.
Parameter Estimates for Acceptance of Asthma in Vigilance and Taking Control
| Vigilance | Taking Control | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Parameter | B | SE | df | t | p | B | SE | df | t | p |
| Intercept | 1.87 | 0.19 | 161 | 9.99 | < .001 | 2.38 | 0.19 | 160 | 12.27 | < .001 |
| Baseline | 0.58 | 0.04 | 163 | 14.30 | < .001 | 0.49 | 0.04 | 149 | 13.71 | < .001 |
| Female | −0.11 | 0.07 | 162 | −1.63 | .104 | −0.08 | 0.07 | 154 | −1.11 | .268 |
| Age of student | −0.06 | 0.06 | 164 | −0.97 | .336 | −0.10 | 0.07 | 169 | −1.54 | .125 |
| Fifth grade | −0.08 | 0.09 | 175 | −0.88 | .378 | 0.01 | 0.10 | 167 | 0.09 | .930 |
| African American | 0.05 | 0.07 | 156 | 0.76 | .446 | −0.12 | 0.07 | 168 | −1.64 | .103 |
| Hispanic | −0.06 | 0.11 | 164 | −0.60 | .549 | −0.08 | 0.12 | 150 | −0.67 | .503 |
| Time since diagnosis | 0.02 | 0.01 | 153 | 1.18 | .238 | −0.00 | 0.01 | 153 | −0.22 | .827 |
| Stimuli of allergies | −0.05 | 0.09 | 180 | −0.53 | .599 | −0.07 | 0.09 | 158 | −0.73 | .467 |
| Stimuli of exercise | −0.03 | 0.08 | 148 | −0.34 | .732 | −0.02 | 0.08 | 159 | −0.27 | .789 |
| Prescribed long-acting bronchodilator | 0.02 | 0.09 | 145 | 0.19 | .847 | 0.03 | 0.09 | 177 | 0.31 | .760 |
| Prescribed inhaled steroid | 0.06 | 0.07 | 161 | 0.87 | .384 | 0.04 | 0.08 | 134 | 0.54 | .591 |
| Family Socioeconomic status | −0.00 | 0.00 | 142 | −1.58 | .117 | 0.00 | 0.00 | 129 | 0.06 | .949 |
| Reading Proficient %Overall | 0.01 | 0.01 | 157 | 1.04 | .300 | −0.00 | 0.01 | 150 | −0.17 | .863 |
| Writing Proficient %Overall | 0.00 | 0.01 | 108 | 0.59 | .558 | −0.01 | 0.01 | 120 | −0.84 | .404 |
| Math Proficient %Overall | −0.01 | 0.01 | 144 | −1.53 | .129 | −0.01 | 0.01 | 159 | −0.85 | .399 |
| Severity of Asthma | −0.01 | 0.02 | 164 | −0.61 | .541 | −0.01 | 0.02 | 145 | −0.41 | .679 |
| SHARP Participation | 0.03 | 0.07 | 156 | 0.38 | .703ns | 0.01 | 0.08 | 170 | 0.18 | .858ns |
| Pre-post | 0.34 | 0.08 | 182 | 4.10 | < .001* | 0.43 | 0.09 | 173 | 4.89 | < .001* |
| SHARP Participation by Pre-post | 0.10 | 0.11 | 168 | 0.86 | .389ns | −0.08 | 0.12 | 180 | −0.71 | .478ns |
p < .05,
Non-significant
NOTE: SHARP – Staying Healthy–Asthma Responsible & Prepared™
Table 6.
Parameter Estimates for Acceptance of Asthma in Connectedness with Peers
| Good Friends | Classmates – Negatively Wordeda Reverse Scored | Classmates – Positively Worded | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Parameter | B | SE | df | t | p | B | SE | df | t | p | B | SE | df | t | p |
| Intercept | 2.25 | 0.27 | 68 | 8.38 | < .001 | 1.71 | 0.24 | 68 | 7.22 | < .001 | 1.81 | 0.26 | 58 | 6.94 | < .001 |
| Baseline | 0.47 | 0.05 | 62 | 9.19 | < .001 | 0.57 | 0.05 | 46 | 12.60 | < .001 | 0.54 | 0.05 | 40 | 10.77 | < .001 |
| Female | −0.17 | 0.09 | 125 | −1.88 | .063 | −0.26 | 0.08 | 107 | −3.27 | .001 | −0.23 | 0.09 | 76 | −2.54 | .013* |
| Age of student | −0.03 | 0.09 | 128 | −0.33 | .739 | −0.13 | 0.08 | 74 | −1.55 | .126 | −0.07 | 0.08 | 84 | −0.79 | .432 |
| Fifth grade | −0.09 | 0.12 | 138 | −0.71 | .478 | 0.14 | 0.11 | 92 | 1.21 | .228 | −0.07 | 0.12 | 92 | −0.60 | .553 |
| African American | 0.18 | 0.10 | 119 | 1.83 | .070 | 0.08 | 0.08 | 137 | 1.05 | .297 | 0.10 | 0.09 | 126 | 1.14 | .256 |
| Hispanic | 0.06 | 0.16 | 101 | 0.39 | .699 | 0.02 | 0.14 | 65 | 0.17 | .869 | −0.23 | 0.14 | 100 | −1.69 | .093 |
| Time since diagnosis | 0.00 | 0.02 | 121 | 0.05 | .958 | 0.01 | 0.02 | 102 | 0.34 | .732 | 0.03 | 0.02 | 125 | 1.91 | .058 |
| Stimuli of allergies | −0.26 | 0.12 | 140 | −2.18 | .031* | −0.00 | 0.11 | 112 | −0.04 | .970 | −0.13 | 0.11 | 139 | −1.24 | .219 |
| Stimuli of exercise | 0.01 | 0.10 | 120 | 0.07 | .943 | −0.05 | 0.09 | 105 | −0.53 | .600 | 0.06 | 0.09 | 109 | 0.65 | .518 |
| Prescribed long-acting bronchodilator | 0.17 | 0.12 | 159 | 1.40 | .163 | 0.05 | 0.11 | 109 | 0.50 | .621 | −0.04 | 0.12 | 93 | −0.38 | .705 |
| Prescribed inhaled steroid | −0.08 | 0.10 | 99 | −0.81 | .419 | 0.03 | 0.08 | 110 | 0.37 | .715 | 0.04 | 0.09 | 90 | 0.42 | .675 |
| Family Socioeconomic status | −0.00 | 0.00 | 134 | −0.31 | .761 | −0.00 | 0.00 | 93 | −0.13 | .896 | −0.01 | 0.00 | 79 | −2.11 | .038* |
| Reading Proficient %Overall | −0.00 | 0.01 | 135 | −0.03 | .979 | 0.01 | 0.01 | 112 | 0.80 | .426 | −0.00 | 0.01 | 128 | −0.31 | .757 |
| Writing Proficient %Overall | 0.01 | 0.01 | 96 | 1.09 | .279 | −0.00 | 0.01 | 50 | −0.12 | .908 | 0.01 | 0.01 | 89 | 1.55 | .124 |
| Math Proficient %Overall | −0.02 | 0.01 | 81 | −1.77 | .080 | −0.01 | 0.01 | 58 | −1.01 | .318 | −0.02 | 0.01 | 70 | −1.58 | .118 |
| Severity of Asthma | 0.05 | 0.03 | 133 | 1.94 | .055 | 0.01 | 0.03 | 56 | 0.49 | .628 | 0.01 | 0.03 | 87 | 0.46 | .644 |
| SHARP Participation | 0.12 | 0.09 | 159 | 1.26 | .211ns | 0.06 | 0.12 | 101 | 0.50 | .618ns | 0.08 | 0.11 | 153 | 0.67 | .502ns |
| Pre-post | 0.10 | 0.11 | 90 | 0.97 | .336ns | 0.12 | 0.11 | 114 | 1.14 | .256 ns | −0.04 | 0.12 | 129 | −0.33 | .740 ns |
| SHARP Participation by Pre-post | 0.13 | 0.14 | 107 | 0.94 | .349ns | −0.00 | 0.14 | 106 | −0.01 | .995 ns | 0.11 | 0.16 | 122 | 0.74 | .462 ns |
| Months | 0.01 | 0.00 | 119 | 2.15 | .034* | −0.00 | 0.01 | 125 | −0.84 | .401 ns | |||||
| SHARP Participation by Month | −0.01 | 0.01 | 126 | −0.92 | .357 ns | −0.01 | 0.01 | 133 | −1.01 | .314 ns | |||||
Reverse Scored,
p < .05,
Non-significant
NOTE: SHARP – Staying Healthy–Asthma Responsible & Prepared™
Acknowledgments
This research study was funded by the National Institutes of Health, R01 NR010544 Comparison of Asthma Programs for Schools, and The University of Texas at Austin School of Nursing Ed and Molly Smith Centennial Fellowship in Nursing. For information about SHARP or the program of research, contact Dr. Kintner, School of Nursing, 1710 Red River Street, Austin, TX 78701 (ekintner@mail.nur.utexas.edu).
Footnotes
Disclosure: The authors report no actual or potential conflicts of interest.
Contributor Information
Eileen K. Kintner, Associate Professor, The University of Texas at Austin School of Nursing.
Gwendolyn Cook, Research Associate, Comparison of Asthma Programs for Schools, The University of Texas at Austin School of Nursing.
C. Nathan Marti, Statistician, The University of Texas at Austin, Division of Statistics and Scientific Computation, Austin, TX.
Melissa Gomes, Licensed School Counselor, Lansing School District.
Linda Meeder, State School Nurse Consultant, Michigan Department of Community Health, Lansing, MI.
Laurie A. Van Egeren, Director, Community Evaluation, and Research Collaborative Co-Director, National Collaborative for the Study of University Engagement, Michigan State University, University Outreach and Engagement, East Lansing, MI, USA.
References
- Akinbami L. The state of childhood asthma, United States, 1980–2005. Advance Data. 2006;381:1–24. [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. National Health Statistics Reports. 2011;32:1–14. [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B. lme4: Linear mixed-effects models using S4 classes. 2013 http://CRAN.R-project.org/package=lme4.
- Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40(3):373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Bruzzese JM, Markman LB, Appel D, Webber M. An evaluation of Open Airways for Schools: Using college students as instructors. Journal of Asthma. 2001;38(4):337–342. doi: 10.1081/jas-100000261. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multi-model inference: A practical information-theoretic approach. New York: Springer; 2002. [Google Scholar]
- Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004;125(5):1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- Edgecombe K, Latter S, Peters S, Roberts G. Health experiences of adolescents with uncontrolled severe asthma. Archives of Disease in Childhood. 2010;95(12):985–991. doi: 10.1136/adc.2009.171579. [DOI] [PubMed] [Google Scholar]
- Evans D, Clark NM, Feldman CH, Rips J, Kaplan D, Levison MJ, Mellins RB. A school health education program for children with asthma aged 8–11 years. Health Education Quarterly. 1987;14(3):267–279. doi: 10.1177/109019818701400302. [DOI] [PubMed] [Google Scholar]
- Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. New York, NY: Cambridge University Press; 2007. [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Honaker J, King G. What to do about missing values in time-series cross-section data. American Journal of Political Science. 2010;54:561–581. doi: 10.1111/j.1540-5907.2010.00447.x. [DOI] [Google Scholar]
- IBM SPSS. IBM SPSS 19.0 for Windows. Armonk, NY: IBM Company; 2010. [Google Scholar]
- Kintner EK. Adolescent process of coming to accept asthma: A phenomenological study. Journal of Asthma. 1997;34(6):547–561. doi: 10.3109/02770909709055399. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Lack of relationship between acceptance and knowledge of asthma in school-age children and early adolescents. Journal for Specialists in Pediatric Nursing. 2004;9(1):5–14. doi: 10.1111/j.1088-145x.2004.00005.x. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Testing the acceptance of asthma model with children and adolescents. Western Journal of Nursing Research. 2007;29(4):410–431. doi: 10.1177/0193945907299657. [DOI] [PubMed] [Google Scholar]
- Kintner EK, Sikorskii A. Randomized clinical trial of a school-based academic and counseling program for older school-age students. Nursing Research. 2009;58(5):321–331. doi: 10.1097/NNR.0b013e3181b4b60e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Allen A, Meeder L, Bumpus J, Lewis K. Feasibility and benefits of a school-based academic and counseling program for older school-age students. Research in Nursing & Health. 2012;35(5):507–517. doi: 10.1002/nur.21490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn M, Weston S, Wing J, Forester J. Contrast (Version 0.17) 2011 Retrieved from http://cran.r-project.org/web/packages/contrast/index.html.
- Larter NL, Kieckhefer G, Paeth ST. Content validation of standards of nursing care for the child with asthma. Journal of Pediatric Nursing. 1993;8(1):15–21. [PubMed] [Google Scholar]
- Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma--United States, 1980–1999. Morbidity & Mortality Weekly Report Surveillance Summaries. 2002;51(1):1–13. [PubMed] [Google Scholar]
- McKnight P, McKnight K, Sidani S, Figueredo A. Missing data: A gentle introduction. New York, NY: Guilford; 2007. [Google Scholar]
- National Institutes of Health. National Institutes of Health, National Heart, Lung, and Blood Institute Expert Panel Report 3: Guidelines for diagnosis and management of asthma. U.S. Department of Health and Human Services; 2007. Retrieved from http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. [Google Scholar]
- Rhee H, Belyea MJ, Brasch J. Family support and asthma outcomes in adolescents: Barriers to adherence as a mediator. The Journal of Adolescent Health. 2010;47(5):472–478. doi: 10.1016/j.jadohealth.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons, Inc; 1987. [Google Scholar]
- Santrock JW. A topical approach to lifespan development. 5. Boston, MA: McGraw-Hill; 2010. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Stewart M, Masuda JR, Letourneau N, Anderson S, McGhan S. “I want to meet other kids like me”: Support needs of children with asthma and allergies. Issues In Comprehensive Pediatric Nursing. 2011;34(2):62–78. doi: 10.3109/01460862.2011.572638. [DOI] [PubMed] [Google Scholar]
- Tibosch M, Reidsma C, Landstra A, Hugen C, Gerrits P, Brouwer M, Verhaak C. An asthma-related quality of life instrument is unable to identify asthmatic children with major psychosocial problems. European Journal of Pediatrics. 2010;169(12):1495–1501. doi: 10.1007/s00431-010-1250-3. [DOI] [PubMed] [Google Scholar]
- Velsor-Friedrich B, Pigott T, Srof B. A practitioner-based asthma intervention program with African American inner-city school children. Journal of Pediatric Health Care. 2005;19(3):163–171. doi: 10.1016/j.pedhc.2004.12.002. http://dx.doi.org/10.1016/j.pedhc.2004.12.002. [DOI] [PubMed] [Google Scholar]