Abstract
Purpose
The purpose was to evaluate the effectiveness of SHARP, an academic asthma health education and counseling program, on fostering use of effective asthma self-care behaviors.
Design and Methods
This was a phase III, two-group, cluster randomized, single-blinded, longitudinal design guided the study. Caregivers of 205 fourth- and fifth-grade students completed the asthma health behaviors survey at pre-intervention and 1, 12, and 24 months post-intervention. Analysis involved multilevel modeling.
Results
All students demonstrated improvement in episode management, risk-reduction/prevention, and health promotion behaviors; SHARP students demonstrated increased improvement in episode management and risk-reduction/prevention behaviors.
Practice Implications
Working with schoolteachers, nurses can improve use of effective asthma self-care behaviors.
Healthcare professionals attribute a proportion of the high morbidity, mortality, burden, costs, and challenges in children ages 14–19 years with asthma to inadequate or ineffective self-care. Inadequate and ineffective asthma self-care behaviors include lack in compliance, poor adherence with treatment regimes, pronounced inaccuracy of symptom perception, and underestimation of symptom severity. To address these issues, the National Asthma Education and Prevention Guidelines (National Institutes of Health [NIH], 2007) were published. The guidelines specify that a successful asthma management plan includes educating students and caregivers about the condition. Nursing care outcome criteria for children and adolescents with asthma, hereafter referred to as students, have long specified that pulmonary function will be promoted with minimal exacerbation occurring, preventative care understood, follow-up care received, age-appropriate knowledge verbalized, and responsibility for self-care behaviors assumed (Larter, Kieckhefer, & Paeth, 1993). Nurses seek to ensure that students are able to (a) obtain adequate sleep, rest, and dietary intake to maintain wellness and growth and (b) perform daily activities and exercise to maintain or improve physical strength and endurance. Students and their caregivers must learn and use effective asthma self-care behaviors.
Effective self-care behaviors can be classified as episode management, risk-reduction/prevention, and health promotion activities (Kintner, 2007; Kintner et al., 2012; Kintner & Sikorskii, 2009). Episode management behaviors include using quick-reliever medication as prescribed to reduce bronchoconstriction, a peak flow meter to monitor levels of constriction, diaphragmatic and pursed-lip breathing with prolonged forced exhalation to expel trapped air through constricted bronchial tubes, mind and/or body relaxation to slow breathing and relieve tense muscles, cough and deep breathing exercises to rid the lungs of excess mucus, engaging in quiet-time activities to remain calm, and sipping warm fluids to moisten and relax mucus membranes. Asthma risk-reduction/prevention behaviors include using controller medications (e.g., corticosteroids and long-acting bronchodilators) as prescribed, avoiding stimuli or triggers, using hypoallergenic pillows and pillow and mattress protectors, and monitoring for exacerbation of symptoms. Asthma health promotion behaviors include exercising to maintain or improve physical fitness, ensuring adequate sleep and rest, using proper hygiene (e.g., frequent hand-washing and rinsing of the mouth after using inhalers), and eating well-balanced nutritious meals.
When the NIH (2007) recommended expanding asthma self-care education beyond physicians’ offices to schools and community settings, school-based programs were developed and launched (e.g., Pike et al., 2011). However, when pressured to demonstrate academic outcomes, school administrators were reluctant to adopt non-academic programs (Bruzzese, Evans, & Kattan, 2009). Consequently, a school- and community-based, theory-driven, and evidence-guided academic asthma health education and counseling program was developed by nurse specialists in pediatric asthma, school/family healthcare, and psychiatric/mental health counseling working collaboratively with a respiratory therapist and two certified elementary schoolteachers who served on curriculum boards (Kintner et al., 2012; Kintner & Sikorskii, 2009). The program, Staying Healthy–Asthma Responsible & Prepared™ (SHARP), was designed to address cognitive, psychosocial, behavioral, and quality-of-life aspects of living with asthma. The program was also designed to integrate into existing school curricula in such a way that it would be more acceptable to administrators seeking to demonstrate academic outcomes. This report focuses on SHARP’s behavioral outcomes, specifically the use of effective episode management, risk reduction, and health promotion self-care behaviors. SHARP has both a school component and a community component.
The SHARP School Component targets older school-age students on the cusp of growth trajectories for shifting away from parental to more personal responsibility for managing their condition as they transition from elementary to middle or junior high school. The SHARP Community Components targets virtually all members of the community through students with mild to severe asthma by using personal invitations to include members of the students’ supportive network, specifically caregivers, family members, neighbors, friends, classmates, schoolteachers, and youth club/group leaders. Feasibility, benefits, and efficacy of the program are established (Kintner et al., 2012; Kintner & Sikorskii, 2009). This paper presents results of a phase III randomized clinical trial conducted to evaluate the effectiveness and impact of SHARP on cognitive, psychosocial, behavioral, and quality-of-life aspects of asthma self-care.
Purpose
The purpose of this paper is to report effectiveness of SHARP, an academic asthma health education and counseling program, on fostering use of effective asthma episode management, risk-reduction/prevention, and health promotion self-care behaviors in fourth- and fifth-grade students with asthma at 1, 12, and 24 months post-intervention. We hypothesized that compared to students enrolled in elementary schools that received a control program; students in elementary schools that received SHARP would demonstrate equivalent or increased use of effective self-care behaviors. Students randomized to the control group received the non-academic asthma education and counseling program Open Airways for Schools (Clark et al., 2004), a curriculum that is disseminated through the American Lung Association.
Acceptance of Asthma Framework
An ecological approach (Bronfenbrenner, 1979), lifespan development perspective (Santrock, 2010), and the acceptance of asthma model (Kintner, 1997, 2004, 2007) guided development and evaluation of SHARP (Kintner et al., 2012; Kintner & Sikorskii, 2009). The acceptance of asthma model (AAM) is a latent variable model. The model specifies that cognitive and psychosocial factors impact the use of effective asthma self-care behaviors that ameliorate asthma severity and control, use of healthcare services, and quality-of-life outcomes. Individual, disease, and environmental influences impact students as they grow and develop. Self-care behaviors are defined as episode management, risk-reduction/prevention, and health promotion activities influential in effectively controlling one’s chronic condition.
Methods
A two-group, single-blinded, cluster-randomized trial was used. Two institutional review boards and the school district approved the study that was in full compliance with the Helsinki Declaration. Family Education Rights and Privacy Act (FERPA) and Health Insurance Portability and Accountability Act (HIPAA) rights of students with asthma were protected. All members of the research team were certified in the protection of human subjects, FERPA, and HIPAA. No adverse events were reported.
Sample and Sampling
Participants consisted of caregivers of students diagnosed with asthma enrolled in grades 4 and 5. Caregiver eligibility included (a) direct responsibility and knowledge of the child’s asthma, (b) expressed willingness, ability, and availability to participate in all study-related activities, (c) written informed consent, and (d) the ability to understand the English language. Student eligibility criteria included (a) a diagnosis of asthma, (b) expressed willingness, ability, and availability to participate in all study-related activities, (c) caregiver informed written permission, (d) written informed assent, and (e) demonstrated ability to academically perform in English at or near grade level.
Using a convenience sampling method, caregiver/student dyads were recruited in fall 2009 and 2010 from 23 elementary schools. The moderately-sized school district consisted of a diverse and medically under-served population of primarily minority, lower socioeconomic, and inner-city families. Prior to randomization, the schools were matched on free and reduced lunch eligibility, school enrollment numbers, standardized reading and math scores, and race and ethnic proportions. Both SHARP and Open Airways for Schools (OAS) were delivered in spring 2010 and 2011. Caregiver/student dyads served as the unit of analysis.
A CONSORT chart providing eligibility, enrollment, randomization, and participation numbers is contained in a manuscript currently in review. Of the 2,770 student/caregiver dyads screened for eligibility, 270 dyads were eligible and 216 enrolled and completed baseline surveys. Six families withdrew from the study for personal reasons (e.g., moving from the district) prior to randomization. The remaining 205 dyads were allocated to SHARP (n = 117) or OAS (n = 88). Data were collected at four time points over 2.6 years. Attrition at 24 months follow-up was limited to 12%, thus allowing for sufficient power based on a minimum post-attrition sample size of 150 dyads.
Data Collection
Audio-linked, password-protected electronic databases were used for data collection. Data collectors were blinded to the randomization. They collected data at baseline or pretest, 1-month posttest, and at 12- and 24-month follow-up. To acknowledge their time and effort in completing the surveys, monetary cash awards of $15 each were offered to caregivers and their children at each data collection time point.
Interventions
Both programs were delivered in schools during instructional time by nurse-trained and nurse-supervised certified elementary schoolteachers. Both SHARP and OAS were delivered on a weekly basis, February through April. The schoolteachers were identified by the school nurse and well known to the district. To confirm intervention fidelity, all program sessions were digitally audio-recorded and reviewed be designated team members using program- and session-specific checklists. All caregivers received program-specific materials and all students received 100% of their respective programs.
Staying Healthy-Asthma Responsible & Prepared™
Students enrolled in schools randomized to SHARP participated in a school component, and members of their social network, including their caregivers, were invited to attend the community component (Kintner et al., 2012; Kintner & Sikorskii, 2009). The school component consisted of 10 sessions, each 50 minutes in length. Students learned the anatomy of the respiratory system and the pathophysiology of asthma, determined the level of symptom and condition severity, and discussed medications used to prevent and treat symptoms during the first three sessions. Use of effective asthma health behaviors content was covered during sessions 4–6. Students were taught the underlying principles of 11 episode management, eight risk reduction/prevention, and four health promotion behaviors before being offered the opportunity to practice and rehearse the behaviors. The final four sessions explored (a) thoughts and feelings about asthma, (b) beliefs about asthma as a chronic condition, (c) reasoning about asthma management, and (d) quality-of-life aspects of living with a life-long condition.
The community component was organized as a 90-minute asthma health fair with an interactive information sharing presentation (Kintner et al., 2012; Kintner & Sikorskii, 2009). Caregivers and students invited members of their social networks to attend. A nurse specialist in pediatric asthma who was experienced and skilled in public speaking facilitated the information sharing presentation. During the community component, attendees learned about (a) the respiratory system, the pathophysiology of asthma, and medications and treatments used to prevent and control symptoms, (b) effective self-care behaviors, and (c) psychosocial, reasoning, and quality-of-life aspects of living with asthma. Caregiver/student dyads were given (a) a peak flow meter and stethoscope used to manage acute exacerbation of symptoms and (b) pillow and mattress protectors for risk-reduction/prevention of symptoms and health promotion in enhancing undisturbed sleep. Caregivers who were unable to attend the information-sharing program were given the SHARP Community Component materials, including the 35-page informational booklet.
Open Airways for Schools
Students enrolled in schools randomized to OAS attended six lessons, each 50 minutes in length. In addition, they took home bullet-point handouts to teach their caregivers about asthma (Clark et al., 2004; Evans et al., 1987). OAS seeks to empower students with asthma to manage their condition (Bruzzese, Markman, Appel, & Webber, 2001; Clark et al., 2004; Evans et al., 1987; Velsor-Friedrich, Pigott, & Srof, 2005). By completion of the program, caregivers and students should have gained knowledge to be able to take steps to prevent symptoms and recognize warning signs and respond appropriately.
Instruments
The AAM uses several indicators or scales to measure its latent variables. This study used 10 instruments with multiple subscales to measure more than 50 indicators of the model’s eight latent variables. Caregivers and students each completed five instruments. All of the latent variables and instruments used to measure them are identified and described in previous publications (Kintner et al., 2012; Kintner & Sikorski, 2009). All data presented in this report came from two of the instruments completed by the caregivers of the students with asthma. Internal consistency reliability, and stability and construct validity were considered when selecting the self-report instruments described below.
General Health History Survey (GHHS)
We used our 39-item survey to collect demographic and asthma-related information (Kintner et al., 2012). Demographic information included age, grade in school, and family structure. Asthma related information included age when symptoms first appeared and when the condition was diagnosed as well as medications and treatments prescribed to manage the condition. Caregiver’s education and occupation and family income scores were used to compute the family’s socioeconomic status.
Asthma Health Behaviors (AHB) Survey
Completed by caregivers as an objective measure of self-care behaviors, this was a 34-item, 5-point Likert-type survey measuring episode management (2 scales), risk-reduction/prevention (2 scales and 2 single-item indicators), and health promotion behaviors (2 scales and 2 single-item indicators). Episode management behaviors included (a) using medication as prescribed (i.e., using controller bronchodilator and corticosteroid medications as prescribed and using reliever bronchodilator before exercise and for symptoms while moving away from stimuli) and (b) using appropriate symptom management techniques (i.e., diaphragmatic and pursed-lip breathing, mind-body relaxation, body listening, quiet-time activities, and percussion and postural drainage) activities. Risk-reduction/prevention behaviors included (a) talking with others before problems arise and asking for help when needed, (b) watching for stimuli or triggers and symptoms while maintaining ongoing communication with healthcare providers, (c) using a pillow protector, and (d) using a mattress protector. Health promotion behaviors included (a) exercising without symptoms to maintain or improve physical fitness, (b) sleeping undisturbed for 7–9 hours per night to obtain adequate sleep and rest, (c) maintaining overall hygiene and cleanliness (e.g., washing hands, taking showers, cleaning bedding, and keeping one’s room dust- and clutter-free), and (d) rinsing one’s mouth after using an inhaler. The scale assessing eating habits was not used due to poor reliability and validity.
Response options ranged from 0 (not applicable or never) to 1 (rarely), 2 (sometimes), 3 (usually), and 4 (always). Negatively worded items are reversed scored. Mean scores computed for each scale have the potential to range from 0.00 to 4.00. Scale summaries for this sample, including the number of items per scale as well as the number of caregivers that completed the scale, minimum and maximum scores, item to total correlations, Cronbach’s standardized alpha correlation coefficient, exploratory factor loadings, and percent of variance explained at baseline pretest, 1-month posttest, and 12- and 24-month follow-up, are presented in Table 1.
Table 1.
Episode Management (EM), Risk Reduction/Prevention (RR), and Health Promotion (HP) Scale Summaries, Internal Consistency Reliability, and Exploratory Factor Analysis at Four Time Points
| Scale | Items | N | Min-Max Scores | Item to Total Correlations | Standard Alpha Coefficient | Factor Loadings | % Variance Explained |
|---|---|---|---|---|---|---|---|
| EM-Uses Medications as Prescribed | 5 | ||||||
| Baseline Pretest | 205 | 0.00 to 4.00 | .40 to .62 | .75 | .55 to .78 | 49.80 | |
| 1-month Posttest | 177 | 0.00 to 4.00 | .26 to .66 | .74 | .35 to .87 | 50.20 | |
| 12-month Follow-up | 168 | 0.00 to 4.00 | .42 to .63 | .77 | .51 to .85 | 50.65 | |
| 24-month Follow-up | 168 | 0.00 to 4.00 | .42 to .69 | .80 | .52 to .87 | 55.07 | |
| EM-Uses Appropriate Symptom Management Techniques | 6 | ||||||
| Baseline Pretest | 205 | 0.00 to 3.67 | .45 to .51 | .77 | .54 to .76 | 46.06 | |
| 1-month Posttest | 177 | 0.00 to 4.00 | .49 to .67 | .83 | .66 to .79 | 54.13 | |
| 12-month Follow-up | 168 | 0.00 to 4.00 | .54 to .61 | .82 | .66 to .80 | 52.65 | |
| 24-month Follow-up | 168 | 0.00 to 3.83 | .56 to .65 | .84 | .67 to .78 | 54.74 | |
| RR-Maintains Being Watchful in Monitoring | 5 | ||||||
| Baseline Pretest | 205 | 0.00 to 4.00 | .39 to .69 | .78 | .58 to .85 | 53.94 | |
| 1-month Posttest | 177 | 0.00 to 4.00 | .40 to .74 | .79 | .58 to .87 | 55.87 | |
| 12-month Follow-up | 153 | 0.00 to 4.00 | .37 to .70 | .76 | .59 to .85 | 51.56 | |
| 24-month Follow-up | 136 | 0.00 to 4.00 | .30 to .67 | .74 | .49 to .83 | 50.00 | |
| RR-Talks with Others as Needed | 5 | ||||||
| Baseline Pretest | 205 | 0.00 to 4.00 | .51 to .63 | .79 | .66 to .84 | 53.74 | |
| 1-month Posttest | 177 | 0.00 to 4.00 | .53 to .68 | .81 | .62 to .88 | 56.37 | |
| 12-month Follow-up | 153 | 0.00 to 4.00 | .48 to .64 | .80 | .60 to .82 | 54.75 | |
| 24-month Follow-up | 136 | 0.00 to 4.00 | .55 to .72 | .84 | .67 to .88 | 60.33 | |
| HP-Exercises without Symptoms to Maintain/Improve Fitness | 4 | ||||||
| Baseline Pretest | 205 | 0.00 to 4.00 | .35 to .77 | .75 | .48 to .92 | 58.67 | |
| 1-month Posttest | 177 | 0.00 to 4.00 | .42 to .73 | .75 | .60 to .89 | 57.86 | |
| 12-month Follow-up | 153 | 0.00 to 4.00 | .30 to .76 | .75 | .41 to .91 | 59.06 | |
| 24-month Follow-up | 136 | 0.00 to 4.00 | .35 to .76 | .77 | .48 to .90 | 60.00 | |
| HP-Maintains Overall Hygiene/Cleanliness | 5 | ||||||
| Baseline Pretest | 162 | 0.40 to 4.00 | .37 to .54 | .70 | .54 to .75 | 44.58 | |
| 1-month Posttest | 103 | 0.80 to 4.00 | .45 to .70 | .79 | .61 to .84 | 54.31 | |
| 12-month Follow-up | 153 | 1.00 to 4.00 | .45 to .67 | .76 | .64 to .78 | 51.23 | |
| 24-month Follow-up | 136 | 0.60 to 4.00 | .40 to .51 | .70 | .52 to .77 | 45.19 |
Data Processing and Analysis
SPSS for Windows 19 (IBM SPSS, 2010) was used to compute descriptive statistics. Based on best-practice recommendations of Graham (2009), multiple imputations were performed to account for missing data using the R Amelia package (Honaker & King, 2010). Twenty data sets were created for missing data with imputed values. Rubin’s formulas (1987) were used to combine parameter estimates from the 20 models before degrees of freedom and inferential tests were derived. The R lme4 package (Bates, Maechler, & Bolker, 2013; Gelman & Hill, 2007) was used for multilevel modeling. The models were fit using time point and participant levels. Viable unconditional growth models such as models with variables representing change over time were fit using longitudinal model building recommendations (Singer & Willett, 2003). The models were then compared using the Akaike Information Criterion (AIC) and guidelines from Burnham and Anderson (2002) to assess which model best represented longitudinal change for each outcome. Person-level variables including the intervention condition (i.e., SHARP) were added before covariates including grade in school, age in years, gender, race or ethnicity, socioeconomic status, time since diagnosis, stimuli of allergies and/or exercise, severity of asthma, prescribed long-acting bronchodilator and/or inhaled steroid, and school-level variables, specifically proficiency in reading, writing, and math, were added. Finally, the R Contrast package (Kuhn, Weston, Wing, & Forester, 2011) was used to compute simple slope contrasts (Bauer & Curran, 2005) at each assessment point. Sensitivity analysis (McKnight, McKnight, Sidani, & Figueredo, 2007) was used to confirm results for the models fit with imputed data.
Results
The sample consisted of caregivers of 205 students diagnosed with asthma enrolled in grades 4 and 5, ages 9–12 years (M = 10.02, SD = .70). Caregivers ages 19–69 years (M = 39, SD = 8) were primarily female (88%) and consisted of biological parents (88%), grandparents (6%), legal guardians (4%), step parents (2%), and extended family members (2%). Students were primarily male (60%), and Black (43%) or mixed Black and White (13%), and non-Hispanic White (23%), of single parent households (69%) with lower (59%) to low-middle (34%) socioeconomic backgrounds. Time since diagnosis ranged from 4 months to 11 years (M = 6.37, SD = 2.58) and reported stimuli included allergies (82%) and exercise (74%). Severity of asthma ranged from mild (55%) to moderate (37%) and severe (8%) persistent. Prescribed medications included bronchodilators (74%), long-acting bronchodilator (18%), and inhaled steroids (42%). School level proficiency in reading ranged from 68% to 95% (M = 85.16, SD = 5.25), writing 10% to 50% (M = 39.91, SD = 8.27), and math 67% to 95% (M = 86.51, SD = 5.80). Although the community programs were well attended, only 35% of the 117 students randomized to SHARP were represented by at least one member of their social network at the event.
Model Development
With the exception of percentage of overall school writing proficiency (9.76%), family socioeconomic status (0.49%), and severity of asthma (2.93%), all data for all covariates were complete. The episode management and use of pillow/mattress protector behaviors had 3.41% missing data at baseline pretest, 14.15% at posttest, 18.54% at 12-month follow-up, and 18.05% at 24-month follow-up. The risk reduction/prevention and health promotion behaviors for exercises without symptoms to maintain and improve fitness and sleeps undisturbed 7–9 hours per night had 3.41% missing data at baseline pretest, 14.15% at posttest, 25.37% at 12-month follow-up, and 33.66% at 24-month follow-up. Because the health promotion scale was augmented during the study, data for maintains overall hygiene and cleanliness, and maintains oral hygiene with inhaler use both had 22.44% missing data at baseline pretest; both had 49.76% missing data at posttest; at 12-month follow-up, overall hygiene and cleanliness had 25.37% missing data and maintains oral hygiene had 55.61% missing data; and both had 33.66% missing data at 24-month follow-up. Sensitivity analysis in which the models were fit using available data indicated that the models fit with imputed data were similar despite the reduced sample size.
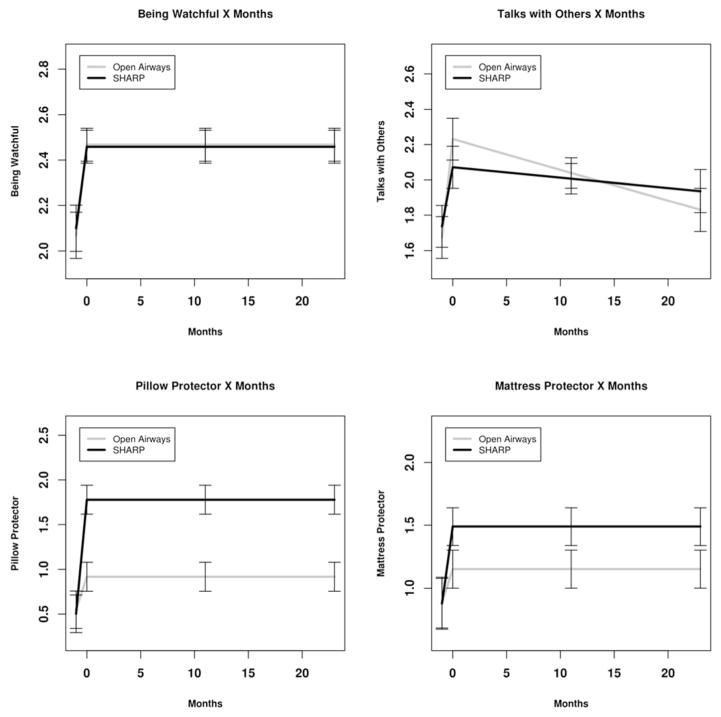
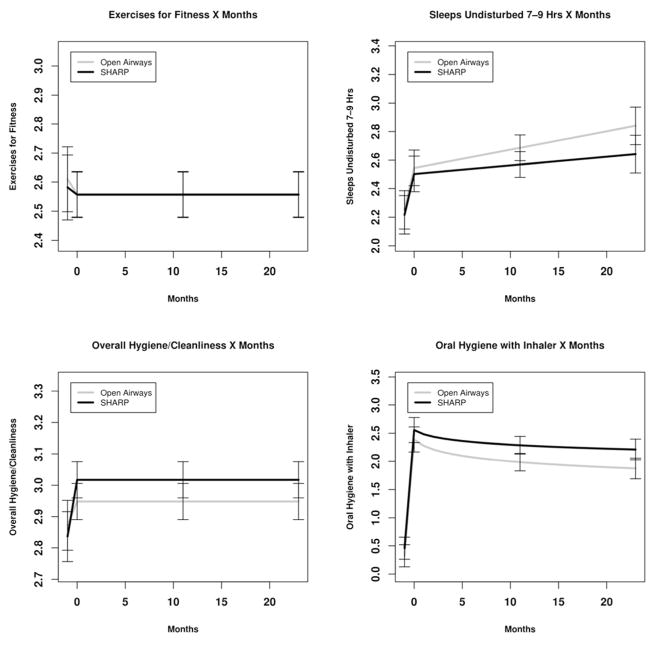
Means and standard deviations for SHARP and OAS participants are presented in Table 2. Parameter estimates for episode management, risk reduction/prevention, and health promotion self-care behaviors are presented in Tables 3–5. Fitted values for the model with standard errors of the difference for simple slope estimates of SHARP versus Open Airways participants at each assessment point are displayed in Figures 1–3. Significant effects are summarized below.
Table 2.
Episode Management (EM), Risk Reduction/Prevention (RR), and Health Promotion (HP) Means (SD) for Open Airways and SHARP Participants at Each Assessment
| Outcome | Baseline Pretest | 1-month posttest | 12-month follow-up | 24-month follow-up |
|---|---|---|---|---|
| EM-Uses Medications as Prescribed | ||||
| Open Airways | 2.68 (0.98) | 2.79 (0.95) | 2.79 (1.10) | 2.74 (1.18) |
| SHARP | 2.58 (1.12) | 2.71 (1.11) | 2.79 (1.00) | 2.66 (1.16) |
| EM-Uses Appropriate Symptom Management Techniques | ||||
| Open Airways | 0.95 (0.81) | 1.40 (0.98) | 1.34 (0.92) | 1.19 (0.88) |
| SHARP | 0.96 (0.88) | 1.59 (0.94) | 1.50 (1.03) | 1.58 (0.94) |
| RR-Maintains Being Watchful in Monitoring | ||||
| Open Airways | 2.08 (0.89) | 2.48 (0.94) | 2.52 (0.89) | 2.46 (0.82) |
| SHARP | 2.11 (1.02) | 2.45 (0.92) | 2.43 (0.89) | 2.49 (0.90) |
| RR-Talks with Others as Needed | ||||
| Open Airways | 1.63 (1.11) | 2.28 (1.14) | 1.99 (1.11) | 1.84 (1.14) |
| SHARP | 1.78 (1.07) | 2.13 (1.10) | 2.00 (1.05) | 2.02 (1.23) |
| RR-Uses a Pillow Protectora | ||||
| Open Airways | 0.60 (1.38) | 0.78 (1.46) | 0.91 (1.59) | 1.08 (1.66) |
| SHARP | 0.52 (1.25) | 1.75 (1.80) | 1.86 (1.78) | 1.88 (1.80) |
| RR-Uses a Mattress Protectora | ||||
| Open Airways | 0.90 (1.60) | 0.96 (1.60) | 1.35 (1.72) | 1.22 (1.75) |
| SHARP | 0.89 (1.52) | 1.42 (1.77) | 1.49 (1.78) | 1.68 (1.79) |
| HP-Exercises without Symptoms to Maintain/Improve Fitness | ||||
| Open Airways | 2.62 (1.00) | 2.54 (1.06) | 2.58 (0.96) | 2.47 (0.96) |
| SHARP | 2.59 (1.02) | 2.63 (0.89) | 2.45 (0.99) | 2.56 (1.05) |
| HP-Sleeps Undisturbed 7–9 Hours per Nighta | ||||
| Open Airways | 2.32 (1.10) | 2.58 (1.09) | 2.88 (1.01) | 2.88 (1.11) |
| SHARP | 2.14 (1.14) | 2.40 (1.06) | 2.48 (1.09) | 2.49 (1.21) |
| HP-Maintains Overall Hygiene/Cleanliness | ||||
| Open Airways | 2.95 (0.71) | 3.01 (0.69) | 2.94 (0.75) | 3.03 (0.71) |
| SHARP | 2.80 (0.77) | 3.01 (0.80) | 3.02 (0.70) | 2.92 (0.77) |
| HP-Maintains Oral Hygiene with Inhaler Usea | ||||
| Open Airways | 0.36 (1.15) | 2.20 (1.66) | 1.88 (1.64) | 1.83 (1.75) |
| SHARP | 0.40 (1.06) | 2.15 (1.74) | 2.16 (1.66) | 2.11 (1.76) |
Single item indicator
NOTE: SHARP – Staying Healthy-Asthma Responsible & Prepared™
Table 3.
Parameter Estimates for Episode Management (EM) in Uses Medications and Symptom Management Techniques
| Scale | |||||
|---|---|---|---|---|---|
|
| |||||
| Parameter | B | SE | df | t | p |
| EM-Uses Medications as Prescribed | |||||
| Intercept | 1.02 | 0.19 | 108 | 5.39 | < .001* |
| Baseline | 0.57 | 0.04 | 126 | 14.10 | < .001* |
| SHARP Participation | 0.12 | 0.09 | 122 | 1.25 | .212ns |
| Pre-post | 0.06 | 0.10 | 172 | 0.60 | .546ns |
| SHARP Participation by Pre-post | 0.09 | 0.13 | 161 | 0.69 | .490ns |
| EM-Uses Appropriate Symptom Management Techniques | |||||
| Intercept | 0.67 | 0.14 | 175 | 4.79 | < .001* |
| Baseline | 0.65 | 0.04 | 167 | 15.66 | < .001* |
| SHARP Participation | 0.22 | 0.08 | 151 | 2.77 | .006* |
| Pre-post | 0.34 | 0.09 | 171 | 3.96 | < .001* |
| SHARP Participation by Pre-post | 0.24 | 0.11 | 168 | 2.08 | .039* |
p < .05,
Non-significant
NOTE: SHARP – Staying Healthy-Asthma Responsible & Prepared™
Table 5.
Parameter Estimates for Health Promotion (HP) in Exercising, Sleeping, and Maintaining Overall Hygiene and Cleanliness and Oral Hygiene with Inhaler Use
| Scale | |||||
|---|---|---|---|---|---|
|
| |||||
| Parameter | B | SE | df | t | p |
| HP-Exercises without Symptoms to Maintain/Improve Fitness | |||||
| Intercept | 1.17 | 0.16 | 165 | 7.46 | < .001* |
| Baseline | 0.60 | 0.03 | 119 | 18.09 | < .001* |
| SHARP Participation | −0.00 | 0.08 | 112 | −0.03 | .979ns |
| Pre-post | −0.05 | 0.10 | 144 | −0.53 | .594ns |
| SHARP Participation by Pre-post | 0.03 | 0.13 | 155 | 0.21 | .834ns |
| HP-Sleeps Undisturbed 7–9 Hours per Night | |||||
| Intercept | 1.53 | 0.20 | 130 | 7.69 | < .001* |
| Baseline | 0.54 | 0.04 | 132 | 15.20 | < .001* |
| SHARP Participation | −0.04 | 0.13 | 153 | −0.34 | .735ns |
| Pre-post | 0.29 | 0.13 | 157 | 2.25 | .026* |
| SHARP Participation by Pre-post | −0.01 | 0.17 | 166 | −0.05 | .962ns |
| Months | 0.01 | 0.01 | 148 | 2.12 | .036* |
| SHARP Participation by Month | −0.01 | 0.01 | 149 | −0.85 | .399ns |
| HP-Maintains Overall Hygiene/Cleanliness | |||||
| Intercept | 0.67 | 0.14 | 88 | 4.76 | < .001* |
| Baseline | 0.72 | 0.04 | 73 | 19.94 | < .001* |
| SHARP Participation | 0.07 | 0.06 | 91 | 1.20 | .233ns |
| Pre-post | 0.08 | 0.06 | 121 | 1.21 | .229ns |
| SHARP Participation by Pre-post | 0.11 | 0.08 | 145 | 1.31 | .191ns |
| HP-Maintains Oral Hygiene with Inhaler Use | |||||
| Intercept | 1.64 | 0.32 | 64 | 5.18 | < .001* |
| Baseline | 0.73 | 0.09 | 27 | 8.23 | < .001* |
| SHARP Participation | 0.17 | 0.22 | 78 | 0.75 | .455ns |
| Pre-post | 2.07 | 0.21 | 86 | 9.83 | < .001* |
| SHARP Participation by Pre-post | 0.03 | 0.27 | 108 | 0.12 | .903ns |
| Months (log transformed) | −0.16 | 0.07 | 53 | −2.28 | .026* |
| SHARP Participation by Month (log transformed) | 0.05 | 0.09 | 78 | 0.63 | .532ns |
p < .05,
Non-significant
NOTE: SHARP – Staying Healthy-Asthma Responsible & Prepared™
Figure 1.
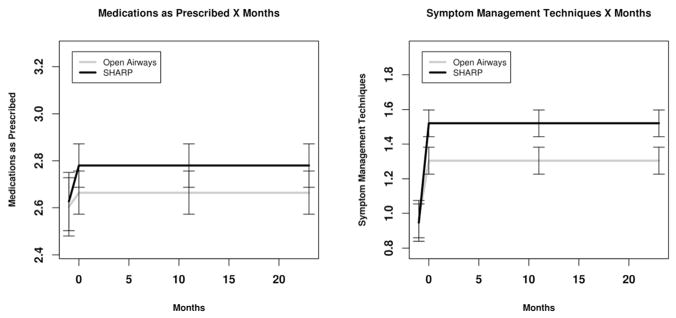
Episode Management (EM) in Using Medications as Prescribed and Symptom Management Techniques as Appropriate for SHARP and Open Airways Participants. Fitted values for SHARP and Open Airways participants with ± one standard error of the difference for simple slope estimates of SHARP versus Open Airways participants at each assessment point
Figure 3.
Risk Reduction/Prevention (RR) Behaviors in Being Watchful, Talking with Others, and Using Pillow and Mattress Protectors for SHARP and Open Airways Participants. Fitted values for SHARP and Open Airways participants with ± one standard error of the difference for simple slope estimates of SHARP versus Open Airways participants at each assessment point
Episode Management
Although Figure 1 might indicate otherwise, no significant effect was observed in uses medication as prescribed from pretest to posttest, during follow-up, or by program. We observed a main effect from pre-post change (t[171] = 3.96, p < .001) in use of appropriate symptom management techniques, indicating an average increase from pre- to post-intervention for all participants. The SHARP participation by pre-post interaction was significant (t[168] = 2.08, p = .039), indicating that SHARP participants had a greater increase. The SHARP main effect was significant (t[151] = 2.77, p = .006), indicating that SHARP participants exhibited increased use of appropriate symptom management techniques at post-test.
Risk Reduction/Prevention
Time since diagnosis was a significant covariate (t[143] = 2.15, p = .034) with maintains being watchful in monitoring for stimuli and symptoms. We observed a main effect from pre-post change (t[171] = 4.84, p < .001) in maintains being watchful in monitoring for stimuli and symptoms, indicating that there was an average increase from pre- to post-intervention for all participants. We observed a main effect from pre-post change (t[162] = 4.95, p < .001) in talking with others when needed, indicating that there was an average increase from pre- to post-intervention for all participants. Talking with others when needed decreased by months (t[128] = −3.24, p = .002) for all participants as students transitioned into middle or junior high school.
We observed a main effect from pre-post change (t[162] = 2.23, p = .027) in uses a pillow protector, indicating that there was an average increase from pre- to post-intervention for all participants. The SHARP participation by pre-post interaction was significant (t[160] = 4.14, p < .001) for uses pillow protector, indicating that the SHARP participants exhibited a great increase between pre- and post-test assessments. The SHARP main effect for use of pillow (t[115] = 5.34, p < .001) and mattress (t[121] = 2.24, p = .027) protectors were significant, indicating that SHARP participants exhibited increased use in the protectors at post-test.
Health Promotion
No significant changes were observed between participants in exercising without symptoms to maintain/improve fitness or maintaining overall hygiene and cleanliness. We observed a main effect from pre-post change (t[157] = 2.25, p < .026) in sleeps undisturbed 7–9 hours per night, indicating that there was an average increase from pre- to post-intervention for all participants that continued to increase over time (t[148] = 2.12, p < .036). Being prescribed an inhaled steroid was a significant covariate (t[86] = 5.70, p < .001) with oral hygiene by rinsing the mouth after inhaler use. We observed a main effect from pre-post change (t[86] = 9.83, p < .001) in maintaining oral hygiene by rinsing the mouth after inhaler use, indicating that there was an average increase from pre- to post-intervention for all participants. However, maintaining oral hygiene decreased by months (t[53] = −2.28, p = .026) for all participants as students transitioned into middle or junior high school.
Discussion
The effectiveness of SHARP, compared to the control condition, on fostering use of effective asthma self-care behaviors in older school-age students was demonstrated through (a) increased use of appropriate symptom management techniques and pillow/mattress protectors for SHARP, (b) equivalent increase in being watchful in monitoring for stimuli and symptoms, talking with others, and rinsing the mouth after inhaler use for all students, and (c) equivalent reporting of students using medications as prescribed. With regard to missing data due to changes in the health promotion subscales during the study, sensitivity analysis indicated that the models fit with imputed data held up well despite missing data. SHARP was effective in fostering use of effective episode management, risk reduction/prevention, and health promotion behaviors.
Individual’s scores for use of effective self-care behaviors ranged from never to always. Overall group mean scores ranged from (a) usually for overall hygiene, uses medication as prescribed, exercises without symptoms, and being watchful in monitoring to (b) sometimes for talks with others and oral hygiene, and (c) rarely to sometimes for using pillow/mattress protectors and appropriate symptom management techniques. More emphasis on recognizing self-care behaviors and understanding the rationale for effective episode management, risk reduction/prevention, and health promotion behaviors is needed to advance overall use. Self-care behaviors need to be taught, demonstrated, rehearsed, and incorporated into everyday life.
Historically, asthma research focused on identifying problem behaviors associated with inadequate and ineffective asthma management (e.g., Creer et al., 1989). Asthma education programs were developed that primarily focused on medications used to control and relieve symptoms and the proper use of peak flow meters, inhalers, and spacers that impacted compliance, adherence, adjustment, and adaptation outcomes (e.g., Rachelefsky, 2007). More recently, the importance of self-efficacy in the management of asthma has been explored (e.g., Kaul, 2011). However, this program of research is innovative and unique by focusing on three classifications of effective asthma self-care behaviors that impact asthma control, quality of life, and use of healthcare services (Kintner et al., 2012; Kintner & Sikorskii, 2009) and by using caregivers as more objective observers of the child’s behaviors.
After teaching anatomy of the respiratory system, the pathophysiology of asthma, and the proper use of medications including peak flow monitoring and inhaler use, SHARP offers a comprehensive approach to understanding the rationale for using effective episode management, risk reduction or prevention, and health promotion behaviors in the context of living with asthma (Kintner et al., 2012; Kintner & Sikorskii, 2009). The SHARP Student Component devotes 50 minutes each to (a) learning techniques for managing asthma symptoms in addition to medications, (b) exploring ways to reduce the chance of having an asthma episode, including role playing how to talk with others about asthma, and (c) discussing ways to stay healthy while living with asthma. Students are provided with opportunities to practice purse-lip and abdominal breathing, percussion and postural draining, body listening, and mind and body relaxation. They learn how to engage in quiet time activities to remain calm during acute episodes. The importance of obtaining proper nutrition, exercising to maintain or improve physical fitness, obtaining adequate rest and sleep, and using good hygiene to prevent infections is stressed. The SHARP Community Component interactive presentation devotes 30–40 minutes to discussing effective self-care behaviors. In addition, caregiver/student dyads are given (a) peak flow meters and stethoscopes to help them better assess exacerbation of symptoms and (b) pillow and mattress protectors to reduce or prevent symptoms and promote health and wellness by enhancing undisturbed sleep.
Our previous research indicates that caregiver knowledge of asthma serves as a mediator to student retention of asthma knowledge and adoption of effective self-care behaviors following the student’s participation in an asthma education program (Kintner, 2004). Students retain what is learned when caregivers reinforce what was taught. Caregivers must have the same or more knowledge of asthma than their children. For this study, caregivers were responsible for monitoring and assessing their children’s behaviors despite often having limited knowledge of the behaviors. Caregiver participation in SHARP required attendance at the community program and/or review of the 35-page booklet. Caregiver participation in OAS required the review of 6 one-page bullet-point handouts sent home in students’ backpacks. Additional analyses are required to explore how the caregiver’s knowledge of asthma and participation in the community component impacted his/her ability to accurately assess the child’s behaviors.
Our previous studies reported 68%–70% caregiver participation in the SHARP Community Component (Kintner et al., 2012; Kintner & Sikorskii, 2009). Timing and scheduling influenced caregiver attendance in this study. Although attendance at four of the six community programs exceeded expectation, two of the programs competed with other real world events. The programs were scheduled 6–12 months in advance to secure the meeting space. As the dates approached, we became aware that one program was scheduled in competition with the season finale of a popular television show and another program was scheduled on the first game day of the new little league season. As we prepare for dissemination and implementation of SHARP in communities across the country and around the world, careful attention will be given to the scheduling of both the student and community components to reach virtually all community members through students diagnosed with mild intermittent to severe persistent asthma.
How Might This Information Affect Nursing Practice?
Pediatric nurse specialists are able to lead interdisciplinary teams using SHARP School and Community Components to foster the use of effective episode management, risk reduction/prevention, and health promotion self-care behaviors that impact asthma control, quality of life, and use of healthcare services outcomes in older school-age students with asthma and members of their social networks.
Figure 2.
Health Promotion (HP) Behaviors in Exercising, Sleeping, and Maintaining Overall Hygiene/Cleanliness and Oral Hygiene with Inhaler Use for SHARP and Open Airways Participants. Fitted values for SHARP and Open Airways participants with ± one standard error of the difference for simple slope estimates of SHARP versus Open Airways participants at each assessment point
Table 4.
Parameter Estimates for Risk Reduction/Prevention (RR) in Being Watchful, Talking with Others, and Using Pillow and Mattress Protectors
| Scale | |||||
|---|---|---|---|---|---|
|
| |||||
| Parameter | B | SE | df | t | p |
| RR-Maintains Being Watchful in Monitoring | |||||
| Intercept | 1.06 | 0.14 | 99 | 7.39 | < .001* |
| Baseline | 0.60 | 0.03 | 155 | 18.49 | < .001* |
| SHARP Participation | −0.01 | 0.07 | 129 | −0.12 | .905ns |
| Pre-post | 0.40 | 0.08 | 171 | 4.84 | < .001* |
| SHARP Participation by Pre-post | −0.04 | 0.11 | 168 | −0.36 | .717ns |
| RR-Talks with Others as Needed | |||||
| Intercept | 1.11 | 0.17 | 121 | 6.52 | < .001* |
| Baseline | 0.70 | 0.03 | 136 | 20.43 | < .001* |
| SHARP Participation | −0.16 | 0.12 | 119 | −1.34 | .182 ns |
| Pre-post | 0.56 | 0.11 | 162 | 4.95 | < .001* |
| SHARP Participation by Pre-post | −0.22 | 0.15 | 147 | −1.46 | .146 ns |
| Months | −0.02 | 0.01 | 128 | −3.24 | .002* |
| SHARP Participation by Month | 0.01 | 0.01 | 108 | 1.57 | .119 ns |
| RR-Uses a Pillow Protectora | |||||
| Intercept | 0.57 | 0.28 | 155 | 2.05 | .042* |
| Baseline | 0.52 | 0.05 | 131 | 9.80 | < .001* |
| SHARP Participation | 0.86 | 0.16 | 115 | 5.34 | < .001* |
| Pre-post | 0.37 | 0.17 | 162 | 2.23 | .027* |
| SHARP Participation by Pre-post | 0.91 | 0.22 | 160 | 4.14 | < .001* |
| RR-Uses a Mattress Protectora | |||||
| Intercept | 0.35 | 0.26 | 163 | 1.34 | .182ns |
| Baseline | 0.61 | 0.04 | 154 | 15.18 | < .001* |
| SHARP Participation | 0.34 | 0.15 | 121 | 2.24 | .027* |
| Pre-post | 0.27 | 0.16 | 164 | 1.64 | .103ns |
| SHARP Participation by Pre-post | 0.35 | 0.22 | 156 | 1.60 | .112ns |
Single item indicator
p < .05,
Non-significant
NOTE: SHARP – Staying Healthy-Asthma Responsible & Prepared™
Acknowledgments
This research study was funded by the National Institutes of Health, R01 NR010544 Comparison of Asthma Programs for Schools, and The University of Texas at Austin School of Nursing Ed and Molly Smith Centennial Fellowship in Nursing. We wish to recognize collaborating sites (i.e., Lansing School District; Sparrow Health System; Southside, Foster, and Gier Park Community Centers), community partners (i.e., Asthma Initiative of Michigan, American Lung Association, Healthy Homes University, Asthma and Allergy Foundation, Jackson Community and Delta College Respiratory Care Programs, Michigan Pharmacists Association, Self-Realization Meditation Healing Center, and KFC), research team members, and participants for their support in delivery of the programs.
Footnotes
Disclosure: The authors report no actual or potential conflicts of interest.
Contributor Information
Eileen K. Kintner, Associate Professor, The University of Texas at Austin School of Nursing.
Gwendolyn Cook, Research Associate, Comparison of Asthma Programs for Schools, The University of Texas at Austin School of Nursing.
C. Nathan Marti, Statistician, The University of Texas at Austin, Division of Statistics and Scientific Computation, Austin, TX.
April Allen, Licensed Respiratory Therapist, Allegiance Asthma Resource Person, and Jackson Asthma Coalition Coordinator, Cardiopulmonary Rehabilitation, Allegiance Health, Jackson, MI.
Debbie Stoddard, Site Coordinator, Michigan State University, University Outreach and Engagement, East Lansing, MI.
Phyllis Harmon, Administrative Research Assistant, Comparison of Asthma Programs for Schools, The University of Texas at Austin School of Nursing, Austin, TX.
Melissa Gomes, Licensed School Counselor, Lansing School District.
Linda Meeder, State School Nurse Consultant, Michigan Department of Community Health, Lansing, MI.
Laurie A. Van Egeren, Director, Community Evaluation, and Research Collaborative Co-Director, National Collaborative for the Study of University Engagement, Michigan State University, University Outreach and Engagement, East Lansing, MI, USA.
References
- Bates D, Maechler M, Bolker B. lme4: Linear mixed-effects models using S4 classes. 2013 Retrieved from http://CRAN.R-project.org/package=lme4.
- Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40:373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Bruzzese JM, Evans D, Kattan M. School-based asthma programs. Journal of Allergy & Clinical Immunology. 2009;124:195–200. doi: 10.1016/j.jaci.2009.05.040. [DOI] [PubMed] [Google Scholar]
- Bruzzese JM, Markman LB, Appel D, Webber M. An evaluation of Open Airways for Schools: Using college students as instructors. Journal of Asthma. 2001;38(4):337–342. doi: 10.1081/jas-100000261. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multi-model inference: A practical information-theoretic approach. New York, NY: Springer; 2002. [Google Scholar]
- Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004;125:1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- Creer TL, Wigal JK, Tobin DL, Kotses H, Snyder SE, Winder JA. The revised asthma problem behavior checklist. Journal of Asthma. 1989;26:17–29. doi: 10.3109/02770908909073226. [DOI] [PubMed] [Google Scholar]
- Evans D, Clark NM, Feldman CH, Rips J, Kaplan D, Levison MJ, Mellins RB. A school health education program for children with asthma aged 8–11 years. Health Education Quarterly. 1987;14:267–279. doi: 10.1177/109019818701400302. [DOI] [PubMed] [Google Scholar]
- Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. New York, NY: Cambridge University Press; 2007. [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Honaker J, King G. What to do about missing values in time-series cross-section data. American Journal of Political Science. 2010;54:561–581. doi: 10.1111/j.1540-5907.2010.00447.x. [DOI] [Google Scholar]
- IBM SPSS. IBM SPSS 19.0 for Windows. Armonk, NY: IBM Company; 2010. [Google Scholar]
- Kaul T. Helping African American children self-manage asthma: The importance of self-efficacy. Journal of School Health. 2011;81:29–33. doi: 10.1111/j.1746-1561.2010.00554.x. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Adolescent process of coming to accept asthma: A phenomenological study. Journal of Asthma. 1997;34:547–561. doi: 10.3109/02770909709055399. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Lack of relationship between acceptance and knowledge of asthma in school-age children and early adolescents. Journal for Specialists in Pediatric Nursing. 2004;9(1):5–14. doi: 10.1111/j.1088-145x.2004.00005.x. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Testing the acceptance of asthma model with children and adolescents. Western Journal of Nursing Research. 2007;29:410–431. doi: 10.1177/0193945907299657. [DOI] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Allen A, Meeder L, Bumpus J, Lewis K. Feasibility and benefits of a school-based academic and counseling program for older school-age students. Research in Nursing & Health. 2012;35:507–517. doi: 10.1002/nur.21490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Sikorskii A. Randomized clinical trial of a school-based academic and counseling program for older school-age students. Nursing Research. 2009;58:321–331. doi: 10.1097/NNR.0b013e3181b4b60e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn M, Weston S, Wing J, Forester J. Contrast (Version 0.17) 2011 Retrieved from http://cran.r-project.org/web/packages/contrast/index.html.
- Larter NL, Kieckhefer G, Paeth ST. Content validation of standards of nursing care for the child with asthma. Journal of Pediatric Nursing. 1993;8:15–21. [PubMed] [Google Scholar]
- Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma--United States, 1980–1999. Morbidity & Mortality Weekly Report Surveillance Summaries. 2002;51:1–13. [PubMed] [Google Scholar]
- McKnight P, McKnight K, Sidani S, Figueredo A. Missing data: A gentle introduction. New York, NY: Guilford; 2007. [Google Scholar]
- National Institutes of Health. National Heart, Lung, and Blood Institute, Expert panel report 3: Guidelines for diagnosis and management of asthma. U.S. Department of Health and Human Services; 2007. Retrieved from http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. [Google Scholar]
- Pike EV, Richmond CM, Hobson A, Kleiss J, Wottowa J, Sterling DA. Development and evaluation of an integrated asthma awareness curriculum for the elementary school classroom. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2011;88(Suppl 1):61–67. doi: 10.1007/s11524-010-9477-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachelefsky GS. Improving patient adherence: The asthma template. Pediatric Asthma, Allergy & Immunology. 2007;20(3):146–156. doi: 10.1089/pai.2007.012. [DOI] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons, Inc; 1987. [Google Scholar]
- Santrock JW. A topical approach to lifespan development. 5. Boston, MA: McGraw-Hill; 2010. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Velsor-Friedrich B, Pigott T, Srof B. A practitioner-based asthma intervention program with African American inner-city school children. Journal of Pediatric Health Care. 2005;19(3):163–171. doi: 10.1016/j.pedhc.2004.12.002. [DOI] [PubMed] [Google Scholar]