Abstract
Although disruption of mitochondrial homeostasis and biogenesis (MB) is a widely accepted pathophysiologic feature of sepsis-induced acute kidney injury (AKI), the molecular mechanisms responsible for this phenomenon are unknown. In this study, we examined the signaling pathways responsible for the suppression of MB in a mouse model of lipopolysaccharide (LPS)-induced AKI. Downregulation of peroxisome proliferator-activated receptor γ coactivator-1α (PGC-1α), a master regulator of MB, was noted at the mRNA level at 3 hours and protein level at 18 hours in the renal cortex, and was associated with loss of renal function after LPS treatment. LPS-mediated suppression of PGC-1α led to reduced expression of downstream regulators of MB and electron transport chain proteins along with a reduction in renal cortical mitochondrial DNA content. Mechanistically, Toll-like receptor 4 (TLR4) knockout mice were protected from renal injury and disruption of MB after LPS exposure. Immunoblot analysis revealed activation of tumor progression locus 2/mitogen-activated protein kinase kinase/extracellular signal-regulated kinase (TPL-2/MEK/ERK) signaling in the renal cortex by LPS. Pharmacologic inhibition of MEK/ERK signaling attenuated renal dysfunction and loss of PGC-1α, and was associated with a reduction in proinflammatory cytokine (e.g., tumor necrosis factor-α [TNF-α], interleukin-1β) expression at 3 hours after LPS exposure. Neutralization of TNF-α also blocked PGC-1α suppression, but not renal dysfunction, after LPS-induced AKI. Finally, systemic administration of recombinant tumor necrosis factor-α alone was sufficient to produce AKI and disrupt mitochondrial homeostasis. These findings indicate an important role for the TLR4/MEK/ERK pathway in both LPS-induced renal dysfunction and suppression of MB. TLR4/MEK/ERK/TNF-α signaling may represent a novel therapeutic target to prevent mitochondrial dysfunction and AKI produced by sepsis.
Introduction
Acute kidney injury (AKI) is characterized by a rapid decrease in renal function over the course of hours to days and is associated with significant morbidity and mortality (∼40%) (Uchino et al., 2005). Despite recent efforts to better understand AKI, mortality associated with this clinical disorder has remained unchanged over the last five decades (Thadhani et al., 1996; Waikar et al., 2008). Sepsis is the most common contributing factor to the development of AKI, mortality resulting from AKI is almost doubled in septic patients (∼70%), and treatment is limited to dialysis and supportive care (Silvester et al., 2001; Schrier and Wang, 2004; Uchino et al., 2005; Bagshaw et al., 2007; Waikar et al., 2008). Taken together, these data reveal a significant need for further study of the pathophysiologic mechanisms underlying renal injury with an emphasis on identifying therapeutic targets to improve clinical outcomes in septic AKI.
Much of the difficulty in developing effective therapies for sepsis-induced AKI stems from the multifactorial nature of the disease. Septic AKI is thought to arise as a result of complex interactions involving alterations in renal hemodynamics, microvascular/endothelial cell dysfunction, and direct effects of inflammatory cells and their products (cytokines/chemokines) on the kidney (Wan et al., 2008). The degree to which changes in global renal blood flow contribute to renal injury remains a topic of intense debate. However, it is generally accepted that microvascular dysfunction leads to sluggish capillary flow and subsequent development of local regions of hypoperfusion and hypoxia in the septic kidney (Wu et al., 2007a,b; Gomez et al., 2014). Reduced microvascular flow also amplifies injury by prolonging exposure of the renal parenchyma to inflammatory cells and various inflammatory molecules, including proinflammatory cytokines such as tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and IL-6, which are primary mediators of cellular injury in sepsis-induced AKI (Cunningham et al., 2002; Chawla et al., 2007; Wang et al., 2011; Xu et al., 2014). Data from postmortem studies and experimental models indicate that tubular cell apoptosis and necrosis are relatively limited in the septic kidney when compared with other forms of AKI (Guo et al., 2004; Langenberg et al., 2008). However, histologic findings, including tubular cell vacuolization, tubular dilatation, and the presence of swollen mitochondria, provide strong evidence that sublethal injury to the proximal tubule may play an important role in the development of sepsis-induced AKI (Langenberg et al., 2008; Tran et al., 2011; Takasu et al., 2013).
The overt structural changes noted in tubular mitochondria after sepsis-induced AKI are of particular note given that the proximal tubule relies heavily on mitochondrial generation of ATP to drive active transport of electrolytes and fluids. Thus, mitochondrial and/or proximal tubule dysfunction may contribute to loss of renal function and disease progression in AKI (Soltoff, 1986; Thadhani et al., 1996). Recent studies have demonstrated suppression of peroxisome proliferator-activated receptor γ coactivator-1α (PGC-1α), and consequently, mitochondrial biogenesis (MB) in experimental models of sepsis-induced AKI, including systemic endotoxin exposure and cecal ligation and puncture (CLP) (Tran et al., 2011). PGC-1α, a “master regulator of MB,” promotes transcriptional activity in both the nucleus and mitochondria to facilitate the generation of new, functional mitochondria in response to a variety of physiologic stimuli (Finck and Kelly, 2006; Sanchis-Gomar et al., 2014). Loss of PGC-1α after sepsis-induced AKI is closely associated with renal and mitochondrial dysfunction and reduced expression of electron transport chain proteins. In addition, proximal tubule-specific PGC-1α knockout delayed recovery of renal function after saline resuscitation in mice treated with lipopolysaccharide (LPS) (Tran et al., 2011). These findings indicate that suppression of PGC-1α and MB may play an important role in disease progression and recovery in the setting of septic AKI.
Our study determined the signaling mechanisms responsible for suppression of MB in the renal cortex after endotoxic AKI. We report that LPS exposure leads to downregulation of PGC-1α and mitochondrial markers in the renal cortex. LPS-induced renal dysfunction and disruption of MB were dependent on Toll-like receptor 4/mitogen-activated protein kinase kinase/extracellular signal-regulated kinase (TLR4/MEK/ERK) and production of the proinflammatory cytokine TNF-α. Inhibition of the TLR4/MEK/ERK/TNF-α signaling may offer a novel therapeutic approach to reverse suppression of MB and loss of renal function in septic AKI.
Materials and Methods
LPS Model of Sepsis-Induced AKI.
Six- to 8-week-old male C57BL/6 mice were acquired from the National Institutes of Health National Cancer Institute/Charles River Laboratories (Frederick, MD). Mice were given an intraperitoneal injection of 0.5, 2, or 10 mg/kg lipopolysaccharide (LPS) derived from Escherichia coli serotype O111:B4 (Sigma-Aldrich, St. Louis, MO). Control mice received an intraperitoneal injection of an equal volume of 0.9% normal saline. Mice were euthanized by isoflurane asphyxiation and cervical dislocation at 1, 3, and 18 hours after LPS exposure, and kidneys and serum were collected for molecular analysis. For experiments using TLR4-deficient animals, TLR4 knockout (TLR4KO) mice were generated by crossing C57BL/10ScN mice with the tlr4LPS-d mutation onto the C57BL/6 background for at least five generations (Ellett et al., 2009). All studies were conducted in accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. Animal use was approved by the Institutional Animal Care and Use Committee at the Medical University of South Carolina.
To determine the role of MEK/ERK signaling in LPS-induced AKI, the MEK inhibitor GSK1120212 (trametinib, chemical structure provided in Gilmartin et al., 2011) was obtained from Selleckchem Chemicals (Houston, TX). GSK1120212 is a potent and specific inhibitor of MEK1/2 that has been previously used in mouse models (Yamaguchi et al., 2011, 2012). Mice received an injection of GSK1120212 (1 mg/kg i.p.) or vehicle control (dimethylsulfoxide i.p.) 1 hour before administration of LPS.
To assess the effects of TNF-α on regulation of MB in this model, rat anti–TNF-α neutralizing antibody (clone MP6-XT22) and the appropriate rat IgG1 κ isotype control antibody (clone RTK2071) were purchased from BioLegend (San Diego, CA). Mice were randomly assigned to one of three groups: 1) control, 2) LPS + isotype control antibody (25 mg/kg), and 3) LPS + anti–TNF-α neutralizing antibody (25 mg/kg). Isotype control antibody and anti–TNF-α neutralizing antibody were administered intravenously 1 hour before LPS via tail vein injection. Control mice received an intravenous injection of vehicle control (phosphate-buffered saline).
Recombinant mouse TNF-α was obtained from BioLegend to evaluate whether TNF-α alone reproduced LPS-mediated changes in renal function and/or MB. Wild-type C57BL/6 male mice (6 to 8 weeks of age) were treated intravenously with either vehicle control (diluent), 20 μg/kg recombinant murine TNF-α, or 50 μg/kg TNF-α via tail vein injection. Animals were euthanized at 18 hours after TNF-α administration, and kidneys and serum were collected for analysis.
Blood Urea Nitrogen Measurement.
Blood urea nitrogen (BUN) was determined using the QuantiChrom Urea Assay kit (BioAssay Systems, Hayward, CA) based on the manufacturer’s directions. All values are expressed as BUN concentration in milligrams per deciliter.
Quantitative Real-Time Polymerase Chain Reaction Analysis of mRNA Expression.
Total RNA was isolated from renal cortical tissue with TRIzol reagent (Life Technologies, Grand Island, NY). The iScript Advanced cDNA Synthesis Kit for quantitative real-time polymerase chain reaction (qRT-PCR) (Bio-Rad Laboratories, Hercules, CA) was used to produce a cDNA library from 1 μg total RNA according to the manufacturer’s protocol. We performed qRT-PCR with the generated cDNA using the SsoAdvanced Universal SYBR Green Supermix reagent (Bio-Rad Laboratories). The relative mRNA expression of all genes was determined by the 2−ΔΔCt method, and 18S ribosomal RNA (18S rRNA) was used as a reference gene for normalization as previously described elsewhere (Wills et al., 2012). Primer pairs used for PCR were as described in Table 1.
TABLE 1.
Primer pairs used for qRT-PCR
| Gene | Primer Sequence | Accession No. | |
|---|---|---|---|
| PGC-1α | Sense | 5′-AGGAAATCCGAGCGGAGCTGA-3′ | NM_008904.2 |
| Antisense | 5′-GCAAGAAGGCGACACATCGAA-3′ | ||
| PGC-1β | Sense | 5′-CTCTGACGCTCTGAAGGACG-3′ | NM_133249.2 |
| Antisense | 5′-GTGCCATCCACCTTGACACA-3′ | ||
| PRC | Sense | 5′-ATTCAGAGCTGCTCGTGTCC-3′ | NM_001081214.1 |
| Antisense | 5′-GGGCCCCAAAGGGTCAAT-3′ | ||
| NRF1 | Sense | 5′-TCGGGCATTTATCCCAGAGATGCT-3′ | NM_001164226.1 |
| Antisense | 5′-TACGAGATGAGCTATACTGTGTGT-3′ | ||
| TFAM | Sense | 5′-GCTGATGGGTATGGAGAAG-3′ | NM_009360.4 |
| Antisense | 5′-GAGCCGAATCATCCTTTGC-3′ | ||
| NDUFS1 | Sense | 5′-AGATGATTTGGGAACAACAG-3′ | NM_001160038.1 |
| Antisense | 5′-TAAGGCTTAGAGGTTAGGGC-3′ | ||
| NDUFB8 | Sense | 5′-CGCCAAGAAGTATAACATGC-3′ | NM_026061.2 |
| Antisense | 5′-TCATCCTGAGTTCTGAGTGG-3′ | ||
| ATPSβ | Sense | 5′-CTATGTGCCTGCTGATGACC-3′ | NM_016774.3 |
| Antisense | 5′-GGATAGATGCCCAACTCAGC-3′ | ||
| COXI | Sense | 5′-ACCATCATTTCTCCTTCTCC-3′ | ENSMUSG00000064351.1 |
| Antisense | 5′-GGTGGGTAGACTGTTCATCC-3′ | ||
| ND1 | Sense | 5′-TAGAACGCAAAATCTTAGGG-3′ | ENSMUSG00000064341.1 |
| Antisense | 5′-TGCTAGTGTGAGTGATAGGG-3′ | ||
| TNF-α | Sense | 5′-TCCCTCTCATCAGTTCTATGGCCCA-3′ | NM_013693.3 |
| Antisense | 5′-GTGTGGGTGAGGAGCACGTA-3′ | ||
| IL-1β | Sense | 5′-TGCCACCTTTTGACAGTGATG-3′ | NM_008361.3 |
| Antisense | 5′-ATGTGCTGCTGCGAGATTTG-3′ | ||
| ICAM-1 | Sense | 5′-CACGTGCTGTATGGTCCTCG-3′ | NM_010493.2 |
| Antisense | 5′-TAGGAGATGGGTTCCCCCAG-3′ | ||
| E-Selectin | Sense | 5′-TTCGGCACAGTGTGTGAGTT-3′ | NM_011345.2 |
| Antisense | 5′-TGACTGGGGCTTCACAGGTA-3′ | ||
| KIM-1 | Sense | 5′-GCATCTCTAAGCGTGGTTGC-3′ | NM_134248.2 |
| Antisense | 5′-TCAGCTCGGGAATGCACAA-3′ | ||
| NGAL | Sense | 5′-ATGCACAGGTATCCTCAGGT-3′ | NM_008491.1 |
| Antisense | 5′-ACCATGGCGAACTGGTTGT-3′ | ||
| 18S rRNA | Sense | 5′-TTGACGGAAGGGCACCACCAG-3′ | NR_003278.3 |
| Antisense | 5′-GCACCACCACCCACGGAATCG-3′ | ||
Analysis of Mitochondrial DNA Content.
Mitochondrial DNA content was determined by qRT-PCR analysis. Total DNA was isolated from the renal cortex using the DNeasy Blood and Tissue Kit (Qiagen, Valencia, CA) as described in the manufacturer’s protocol. Extracted DNA was quantified, and 5 ng was used for PCR. Relative mitochondrial DNA content was assessed by the mitochondrial-encoded NADH dehydrogenase 1 [NADH dehydrogenase subunit 1 (ND1)] and was normalized to nuclear-encoded β-actin. Primer sequences for ND1 and β-actin were ND1 sense: 5′-TAGAACGCAAAATCTTAGGG-3′; ND1 antisense: 5′-TGCTAGTGTGAGTGATAGGG-3′; β-actin sense: 5′-GGGATGTTTGCTCCAACCAA-3′; and β-actin antisense: 5′-GCGCTTTTGACTCAGGATTTAA-3′.
Immunoblot Analysis.
Protein was extracted from renal cortex using radioimmunoprecipitation assay buffer (50 mM Tris-HCl, 150 mM NaCl, 0.1% SDS, 0.5% sodium deoxycholate, 1% Triton X-100, pH 7.4) with protease inhibitor cocktail (1:100), 1 mM sodium fluoride, and 1 mM sodium orthovanadate (Sigma-Aldrich). Total protein amount was determined by BCA protein assay. Equal protein quantities (50–100 μg) were loaded onto 4–15% SDS-PAGE gels (Bio-Rad Laboratories). Proteins were resolved by gel electrophoresis and transferred onto nitrocellulose membranes (Life Technologies). Membranes were blocked in 2.5% bovine serum albumin and incubated overnight with primary antibody at 4°C.
Primary antibodies used in these studies included neutrophil gelatinase-associated lipocalin (NGAL)/lipocalin-2 (1:1000), phospho–tumor progression locus 2 (phospho-TPL2) (1:500), total TPL2 (1:1000; all from Abcam, Cambridge, MA), phospho-ERK1/2 (1:1000), total ERK1/2 (1:1000; both from Cell Signaling Technology, Danvers, MA), kidney injury molecule-1 (KIM-1) (1:1000; R&D systems, Minneapolis, MN), PGC-1 (1:100; Cayman Chemical, Ann Arbor, MI), and β-actin (1:1000; Santa Cruz Biotechnology, Dallas, TX).
Membranes were incubated with the appropriate horseradish peroxidase–conjugated secondary antibody before visualization using enhanced chemiluminescence (Thermo Scientific, Waltham, MA) and the GE ImageQuant LAS4000 (GE Life Sciences, Pittsburgh, PA). Optical density was determined using the National Institutes of Health ImageJ software (version 1.46).
Statistical Analysis.
All data are shown as mean ± S.E.M. When comparing two experimental groups, an unpaired, two-tailed t test was used to determine statistical differences. A one-way analysis of variance (ANOVA) followed by Tukey’s post hoc test was performed for comparisons of multiple groups. P < 0.05 was considered statistically significant. All statistical tests were performed using GraphPad Prism software (GraphPad Software, San Diego, CA).
Results
Endotoxin Exposure Leads to Acute Kidney Injury in Mice.
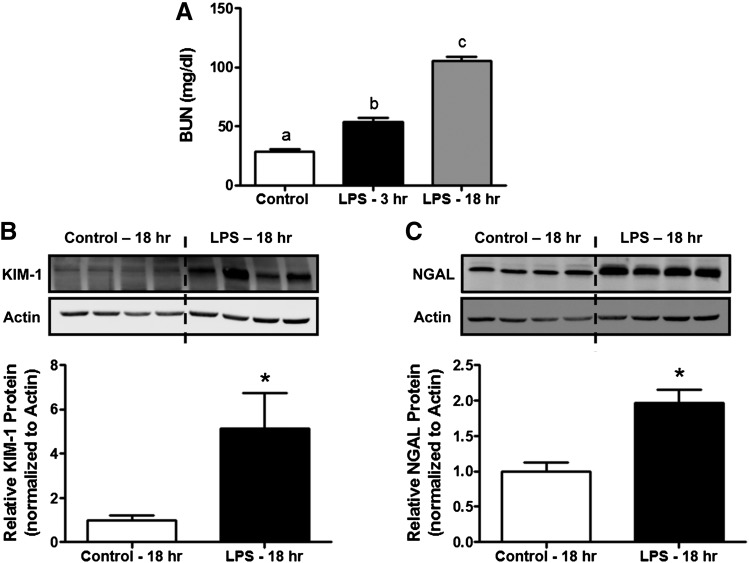
To confirm the effects of systemic LPS exposure on renal function, we measured BUN at 3 and 18 hours after administration in mice. BUN increased 1.9- and 3.8-fold at 3 and 18 hours after LPS exposure, respectively, indicating a time-dependent reduction in renal function (Fig. 1A). These findings are consistent with other studies reporting markedly reduced glomerular filtration rate and elevated BUN with 4 hours of endotoxin exposure in mice (Bhargava et al., 2013).
Fig. 1.
Systemic LPS administration induces renal dysfunction and tubular injury in mice. Six- to 8-week-old male C57BL/6 mice were injected intraperitoneally with LPS (10 mg/kg) or saline vehicle and euthanized at 3 and 18 hours. (A) Renal function at 3 and 18 hours after LPS was determined by BUN (n = 7 animals/group). Immunoblot analysis of renal cortical (B) KIM-1 and (C) NGAL expression was used to assess tubular injury (n = 4 animals/group). Data are shown as mean ± S.E.M. for each group. Different superscripts above the bars indicate statistically significant differences (P < 0.05) when compared with time-point controls. *P < 0.05 versus control.
To confirm proximal tubule injury in this model, we also measured the protein expression of KIM-1 and NGAL in the renal cortex by immunoblot analysis at 18 hours. KIM-1 and NGAL increased ∼5- and ∼2-fold, respectively, in mice receiving LPS when compared with vehicle-treated controls (Fig. 1, B and C). No changes were noted in KIM-1 and NGAL protein levels at 3 hours after LPS exposure, although their mRNA were upregulated at this time point (data not shown). Together, these findings indicate that systemic LPS exposure results in rapid development of AKI and specifically leads to injury in the renal proximal tubule.
LPS-Induced AKI Leads to Persistent Suppression of PGC-1α.
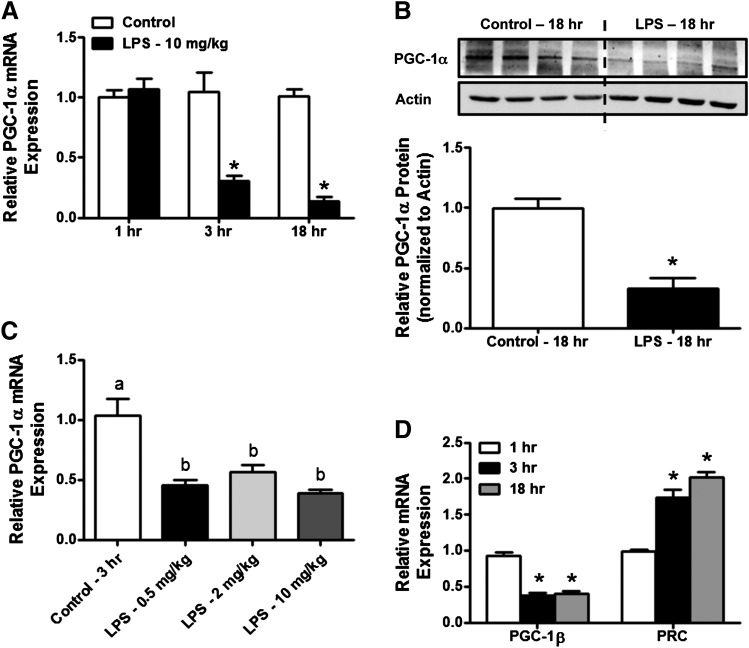
Because disruption of MB and homeostasis has been associated with loss of renal function and delayed recovery in multiple experimental models of AKI, we hypothesized that systemic endotoxin exposure would lead to disruption of PGC-1α (Tran et al., 2011; Funk and Schnellmann, 2012, 2013). PGC-1α mRNA was reduced by 70% as early as 3 hours after LPS exposure and progressively decreased at the 18-hour time point to ∼10% of control (Fig. 2A). In addition, an ∼70% decrease in PGC-1α protein expression was noted at 18 hours after LPS exposure (Fig. 2B). No change was observed in PGC-1α protein at the 3-hour time point (data not shown). To determine whether LPS has a dose-dependent effect on renal cortical PGC-1α expression, mice were treated with 0.5 and 2 mg/kg of LPS, and PGC-1α mRNA was examined 3 hours after administration. Interestingly, lower doses of LPS (0.5 and 2 mg/kg) reduced the PGC-1α transcript ∼55 and ∼45%, respectively, similar to the 10 mg/kg dose (∼60%) (Fig. 2C).
Fig. 2.
LPS-induced AKI is associated with suppression of PGC-1α expression in the renal cortex. Total RNA and protein were extracted from the renal cortex of vehicle- and LPS-treated mice. (A) Time-dependent changes in PGC-1α mRNA expression at 1, 3, and 18 hours after LPS exposure (10 mg/kg) were determined by qRT-PCR analysis (n = 5–6/group). (B) Protein levels of PGC-1α were assessed by Western blot (n = 4/group). (C) To determine the dose-dependent effects of endotoxin on renal cortical PGC-1α expression, a separate group of mice were treated with varying doses of LPS (0.5, 2, and 10 mg/kg), and PGC-1α mRNA was measured (n = 6/group). (D) Time-dependent changes in other members of the PGC-1 family (PGC-1β, PRC) were also determined by qRT-PCR (n = 6/group). Values are expressed as relative expression compared with time point controls and are presented as mean ± S.E.M. Statistically significant differences (P < 0.05) are denoted by superscripts above bars. *P < 0.05 versus time-point control.
To further characterize the effects of endotoxin on MB, we measured the mRNA expression in the renal cortex of other members of the PGC-1 family: peroxisome proliferator-activated receptor γ coactivator-1β (PGC-1β) and peroxisome proliferator-activated receptor γ coactivator-related protein 1 (PRC). Transcript levels of PGC-1β were decreased ∼60% in LPS-treated mice at 3 and 18 hours compared with vehicle-treated controls. In contrast, PRC mRNA increased 1.7-fold as early as 3 hours after administration and remained elevated at 18 hours (2-fold) (Fig. 2D). These data demonstrate that systemic LPS exposure results in suppression of PGC-1α and PGC-1β at the mRNA and/or protein levels in the renal cortex.
PGC-1α Suppression by LPS Results in Disruption of Mitochondrial Homeostasis.
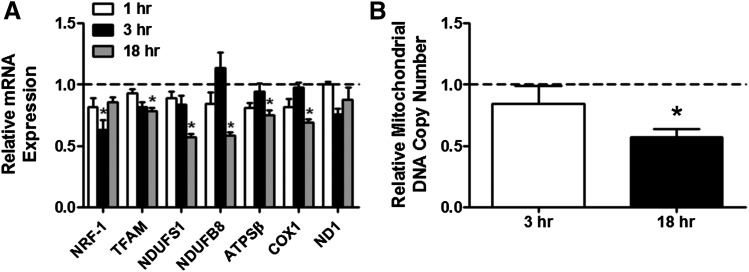
To determine whether mitochondrial homeostasis was altered in the renal cortex as a result of reduced PGC-1α expression after endotoxin administration, we assessed the mRNA expression of downstream mediators of MB [nuclear respiratory factor-1 (NRF-1) and mitochondrial transcription factor a (TFAM)] as well as nuclear-encoded [NADH dehydrogenase (ubiquinone) Fe-S protein 1 (NDUFS1), NADH dehydrogenase (ubiquinone) β-subcomplex 8 (NDUFB8), and ATP synthase β (ATPSβ)] and mitochondrial-encoded [cytochrome c oxidase subunit 1 (COX1) and ND1] components of the electron transport chain. An ∼38% decrease in NRF-1 mRNA was observed 3 hours after LPS exposure, which recovered to control levels by 18 hours. Transcript levels of TFAM, NDUFS1, NDUFB8, ATPSβ, and COX1 were also decreased (∼25, 43, 42, 25, and 31%, respectively) at the 18-hour time point, and these decreases correspond with the reduction in PGC-1α protein (Fig. 3A). We also assessed mitochondrial DNA copy number as a marker of mitochondrial quantity. Relative mitochondrial DNA content in the renal cortex was reduced 43% 18 hours after LPS exposure (Fig. 3B). These findings indicate that suppression of PGC-1α after systemic endotoxin exposure is associated with widespread disruption of transcriptional regulation of mitochondrial proteins and depletion of mitochondrial DNA content.
Fig. 3.
Disruption of mitochondrial homeostasis in endotoxic AKI. Total RNA and DNA were harvested from renal cortical tissue of mice treated with saline vehicle or LPS (10 mg/kg i.p.) at 1, 3, 18, and 42 hours. (A) Expression of key regulators of mitochondrial biogenesis (NRF-1, TFAM), nuclear-encoded components of the electron transport chain (NDUFS1, NDUFB8, ATPSβ), and mitochondrial-encoded respiratory proteins (COX1, ND1) were measured at the mRNA level (n = 6/group). (B) Relative mitochondrial DNA content in the renal cortex was determined by qRT-PCR analysis (n = 5–6 animals/group). Data are shown as expression relative to vehicle-treated animals (mean ± S.E.M.). *P < 0.05 versus time point controls.
TLR4 Is Required for Endotoxin-Induced AKI and Disruption of Mitochondrial Homeostasis.
Although LPS primarily signals through activation of TLR4, recent studies have identified TLR4-independent signaling pathways that contribute to endotoxic shock in mice (Hagar et al., 2013; Kayagaki et al., 2013). To determine whether TLR4 signaling is responsible for both endotoxin-induced AKI and suppression of MB, we used TLR4KO mice and wild-type controls and assessed renal function and mitochondrial homeostasis 18 hours after LPS exposure.
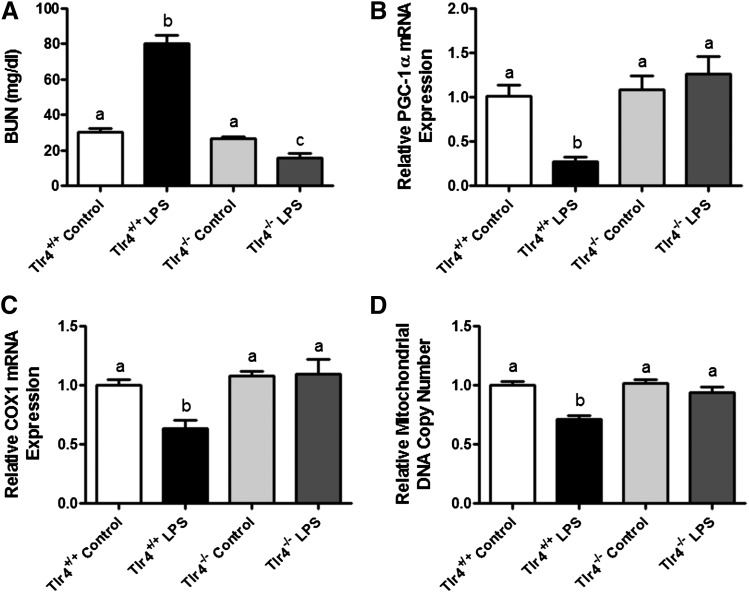
As expected, systemic LPS exposure in wild-type mice resulted in an increase in BUN (Fig. 4A). However, TLR4KO mice were completely protected from endotoxic AKI. These findings are in agreement with previous studies demonstrating an essential role for TLR4 in LPS-induced renal dysfunction in mice (Cunningham et al., 2004).
Fig. 4.
TLR4 is necessary for development of LPS-induced AKI and suppression of mitochondrial biogenesis. Wild-type and TLR4 knockout mice were treated with LPS (10 mg/kg i.p.) or saline vehicle and euthanized at 18 hours for biochemical analysis. (A) BUN was used to assess renal function after LPS exposure. Transcript levels of (B) PGC-1α and (C) COX1 as well as (D) mitochondrial DNA copy number served as markers of mitochondrial homeostasis (n = 3–4/group for all analyses). Statistically significant differences are indicated by superscripts above bars (P < 0.05).
We next determined the role of TLR4 in endotoxin-mediated suppression of PGC-1α and MB. A 73% decrease in PGC-1α mRNA was noted in wild-type mice subjected to LPS while PGC-1α mRNA in TLR4KO mice was similar to controls (Fig. 4B). COX1 mRNA and mitochondrial DNA content were also decreased (∼40 and ∼30%, respectively) in wild-type mice 18 hours after LPS exposure and remained unchanged in TLR4KO mice (Fig. 4, C and D). Taken together, these data reveal an essential role for TLR4 in both LPS-mediated renal damage and suppression of MB.
LPS-Induced AKI Leads to Activation of TPL-2/ERK Signaling in the Renal Cortex.
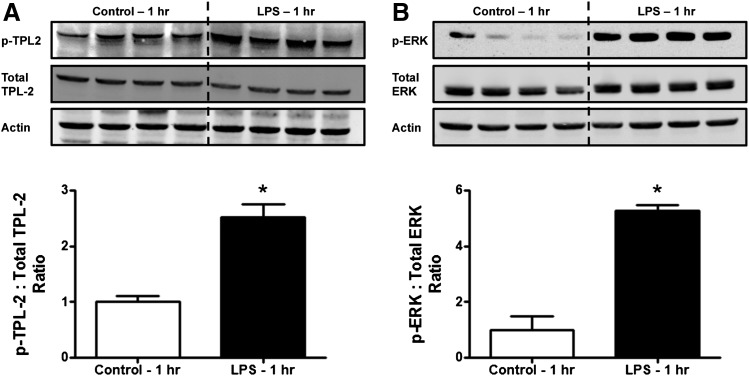
TLR4 is known to initiate signaling by a number of different mediators, most notably nuclear factor κB (NF-κB) and members of the mitogen-activated protein kinase (MAPK) family, including extracellular signal-related kinases 1/2 (ERK1/2), p38 MAPKs, and c-Jun N-terminal kinases (Ostuni et al., 2010; Lin and Tang, 2014). Previous studies showed that ERK1/2 activation may negatively regulate expression of PGC-1α in multiple organs including the brain and skeletal muscle (Coll et al., 2006; Ashabi et al., 2012). In addition, TPL-2 is thought to be critical for activation of ERK1/2 in response to LPS (Dumitru et al., 2000; Banerjee et al., 2006). We hypothesized that TPL-2/ERK signaling would be activated in the renal cortex and that this pathway contributes to disruption of MB in endotoxin-induced AKI. Phosphorylated TPL-2 (Thr209) increased 1.5-fold 1 hour after LPS treatment and returned to control levels at 3 hours (Fig. 5). A 5-fold elevation of ERK1/2 phosphorylation was observed 1 hour after LPS treatment and remained elevated at 3 hours (Figs. 5B and 6D). These findings indicate that TPL-2/ERK signaling is activated quickly in the renal cortex in response to systemic endotoxin exposure.
Fig. 5.
Systemic LPS exposure enhances TPL-2/ERK signaling in the renal cortex. Mice were treated with LPS (10 mg/kg i.p.) or vehicle. Immunoblot analysis revealed increased phosphorylated/activated (A) TPL-2 (Thr209) and (B) ERK1/2 (Thr202/Tyr204) in the renal cortex of LPS-treated mice at 1 hour. Levels of phospho-TPL-2 and phospho-ERK1/2 were normalized to their respective total protein content, and actin was used as a secondary loading control. Data are presented as phosphorylated/total ratio relative to vehicle controls (mean ± S.E.M.; n = 4/group for all analyses). *P < 0.05 versus control.
Fig. 6.
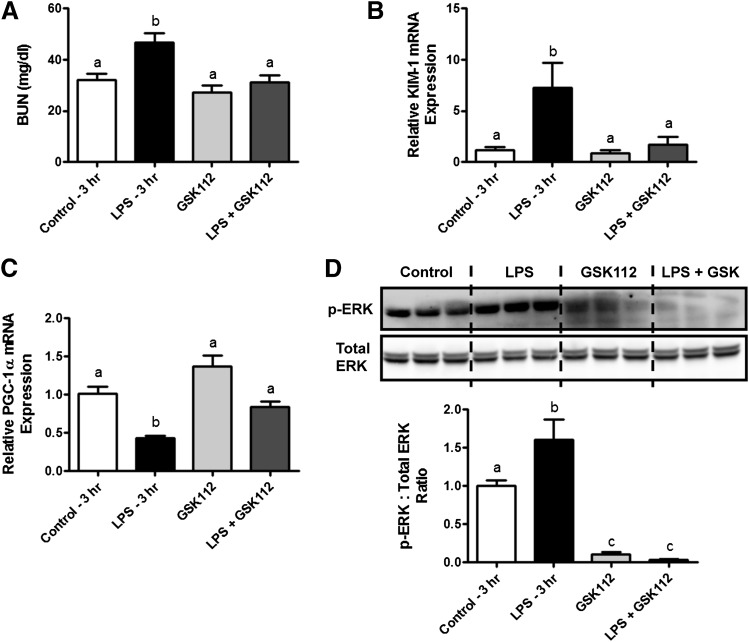
Inhibition of MEK/ERK signaling prevents early changes in renal function and mitochondrial biogenesis in endotoxic AKI. Mice were pretreated with the MEK1/2 inhibitor GSK1120212 (GSK112; 1 mg/kg) 1 hour before systemic LPS exposure. Serum and kidneys were collected at 3 hours after LPS exposure to determine the role of MEK/ERK signaling in early pathophysiology. (A) Renal function was assessed by changes in BUN. (B) The effects of MEK/ERK inhibition on tubular injury were determined by measuring KIM-1 mRNA expression in the renal cortex. (C) PGC-1α transcript levels were determined by qRT-PCR. (D) Inhibition of ERK1/2 activation was confirmed by immunoblot analysis of phosphorylated and total ERK1/2 levels in the renal cortex. Data are shown as mean ± S.E.M. (n = 5–6/group for all analyses). Different superscripts indicate statistically significant differences (P < 0.05).
Early ERK Activation Mediates LPS-Induced Renal Injury and Suppression of MB.
To further elucidate the role of ERK1/2 signaling in LPS-induced AKI and disruption of mitochondrial homeostasis, mice were treated with the potent and selective MEK1/2 inhibitor GSK1120212 (GSK112; 1 mg/kg) 1 hour before LPS administration. MEK1/2 are directly responsible for phosphorylation of ERKs, so inhibition of MEK1/2 by GSK112 will prevent downstream activation of ERK1/2.
In the first experiment, mice were euthanized 3 hours after LPS administration to determine the early effects of ERK activation on renal dysfunction and MB. Pretreatment with GSK112 attenuated endotoxin-mediated elevation of BUN at 3 hours (Fig. 6A) and markedly reduced the increase in renal cortical KIM-1 transcript levels in LPS-treated mice (Fig. 6B). GSK112 alone did not have an effect on either BUN or renal cortical KIM-1 (Fig. 6, A and B). Interestingly, GSK112 administration in mice receiving LPS also blocked suppression of PGC-1α mRNA expression (Fig. 6C). Immunoblot analysis demonstrated effective blockade of ERK1/2 activation in mice treated with MEK1/2 inhibitor (Fig. 6D). These data identify a novel role for early TLR4-mediated ERK1/2 activation in both renal dysfunction and suppression of MB in the renal cortex in LPS-induced AKI.
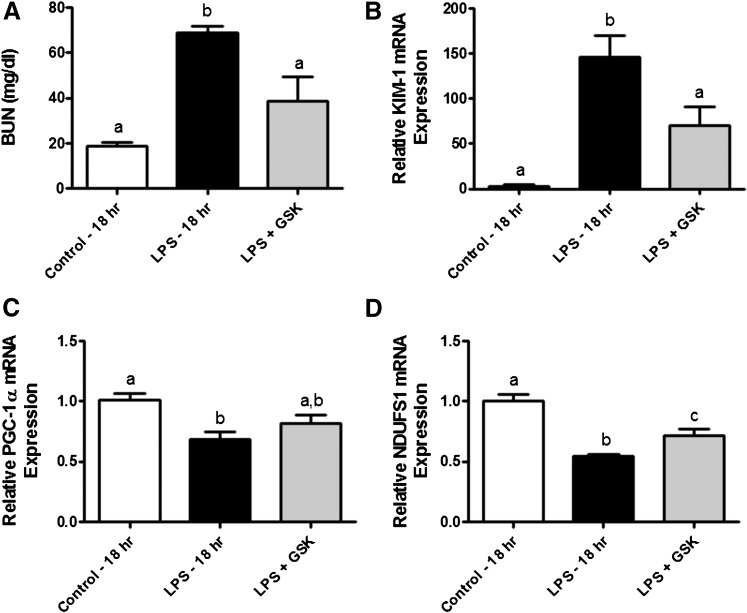
A separate group of mice was pretreated with GSK112 (1 mg/kg) or vehicle control, and serum and kidneys were collected at 18 hours after LPS exposure for biochemical analysis. The BUN increased 3.6-fold in LPS-treated animals and was partially attenuated by GSK112 (∼2.1-fold versus control) (Fig. 7A). In addition, GSK112 pretreatment partially blocked the LPS-induced increase in renal cortical KIM-1 mRNA expression, indicating a reduction in tubular injury (Fig. 7B). A modest effect of GSK112 administration on the transcript levels of PGC-1α and its transcriptional target NDUFS1 was also noted in LPS mice (Fig. 7, C and D).
Fig. 7.
Effects of GSK1120212 on LPS-induced AKI and suppression of mitochondrial biogenesis at 18 hours. Mice receiving GSK1120212 (GSK112; 1 mg/kg) 1 hour before endotoxin administration were euthanized at 18 hours after LPS exposure for biochemical analysis. Renal dysfunction and tubular injury were determined by (A) BUN and (B) KIM-1 mRNA expression, respectively. Transcript levels of (C) PGC-1α and (D) NDUFS1 were determined by qRT-PCR analysis. Values are presented as mean ± S.E.M. for n ≥ 6/group. Superscripts above bars are used to denote statistically significant differences compared with control (P < 0.05).
Taken together, these findings indicate that rapid activation of ERK1/2 in the renal cortex after systemic endotoxin exposure contributes to the early development of renal injury and disruption of mitochondrial homeostasis.
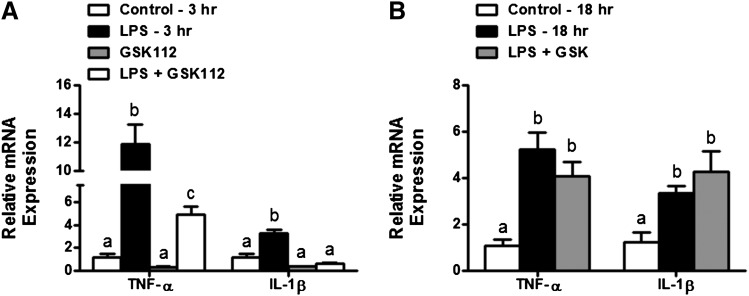
Early ERK Activation Promotes Expression of Proinflammatory Cytokines in the Renal Cortex after LPS Administration.
TLR4-mediated activation of ERK1/2 is known to induce expression of proinflammatory cytokines, including TNF-α and IL-1β (DeFranco et al., 1998; Schaefer et al., 2005; Luan et al., 2014). Recent reports also indicate that these cytokines may negatively regulate PGC-1α expression and MB in a variety of cell types, including renal proximal tubule cells and skeletal muscle cells (Tran et al., 2011; Remels et al., 2013). We therefore examined ERK1/2 signaling in the expression of TNF-α and IL-1β in the renal cortex after systemic endotoxin administration in mice. LPS administration resulted in a robust increase in TNF-α (∼12-fold) and IL-1β (∼3.3-fold) mRNA at 3 hours and GSK112 inhibition of MEK/ERK partially attenuated the early increase in mRNA expression of both proinflammatory cytokines (Fig. 8A). However, pretreatment with GSK112 had no effect on expression of either TNF-α or IL-β at 18 hours after LPS exposure (Fig. 8B). These findings reveal an important role for TLR4-induced ERK signaling in early induction of proinflammatory cytokines in the renal cortex after systemic endotoxin administration.
Fig. 8.
MEK/ERK signaling controls early renal expression of proinflammatory cytokines in response to endotoxin. Inflammatory changes were evaluated in the renal cortex of mice treated with LPS and GSK1120212 (GSK112; 1 mg/kg) as described above. We used qRT-PCR to determine mRNA levels of TNF-α and IL-1β at both (A) 3 hours and (B) 18 hours after LPS exposure. Values are expressed as relative expression versus control (mean ± S.E.M.) for n ≥ 6/group; different superscripts indicate statistically significant differences (P < 0.05).
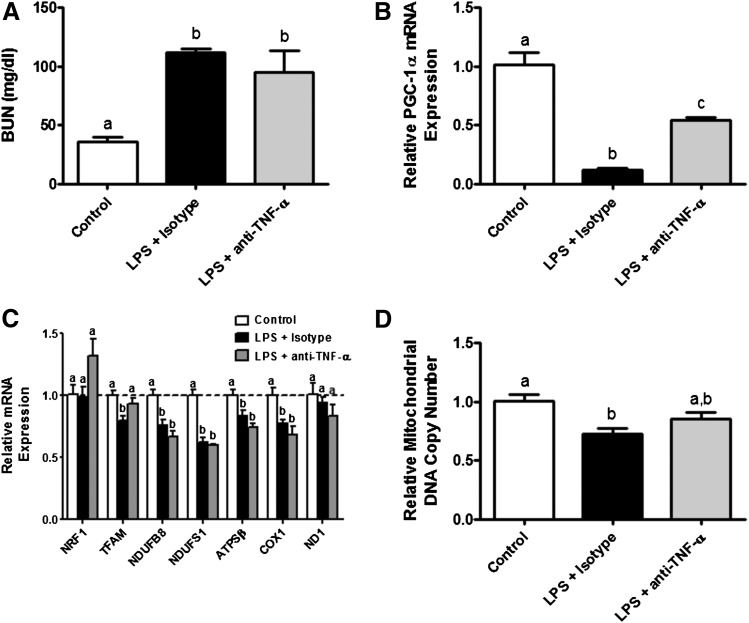
Involvement of TNF-α in LPS-Mediated Suppression of PGC-1α.
Because proinflammatory cytokines have been implicated as a potential mechanism for suppression of PGC-1α in renal proximal tubules, and ERK signaling promoted TNF-α expression in the kidney cortex, we used a neutralizing antibody directed against murine TNF-α to further elucidate its role in this process. Mice were treated intravenously with either TNF-α neutralizing antibody (25 mg/kg) or the appropriate isotype control antibody (25 mg/kg) 1 hour before LPS administration. TNF-α neutralization had no effect on the LPS-induced increase in BUN at 18 hours (Fig. 9A). However, suppression of PGC-1α mRNA levels was partially attenuated in mice receiving the anti–TNF-α antibody (Fig. 9B).
Fig. 9.
TNF-α mediates suppression of PGC-1α in the renal cortex of LPS-treated mice. Mice were treated with anti-TNF-α neutralizing antibody or the appropriate isotype control antibody 1 hour before systemic LPS exposure, and renal function and mitochondrial homeostasis were evaluated at 18 hours. (A) Renal dysfunction was determined by measuring BUN. Transcript levels of (B) PGC-1α and (C) mitochondrial biogenesis markers were assessed. (D) We used qRT-PCR analysis to determine relative mitochondrial DNA content. Data are mean ± S.E.M. (n = 4/group), and different superscripts indicate statistically significant differences (P < 0.05).
Surprisingly, TNF-α neutralization had no effect on the observed decreases in NDUFB8, NDUFS1, ATPSβ, and COX1 transcripts, or mitochondrial DNA content (Fig. 9, C and D). Taken together, these data indicate that the TLR4/ERK/TNF-α signaling axis may act as a critical mechanism for suppression of MB in the setting of endotoxic AKI.
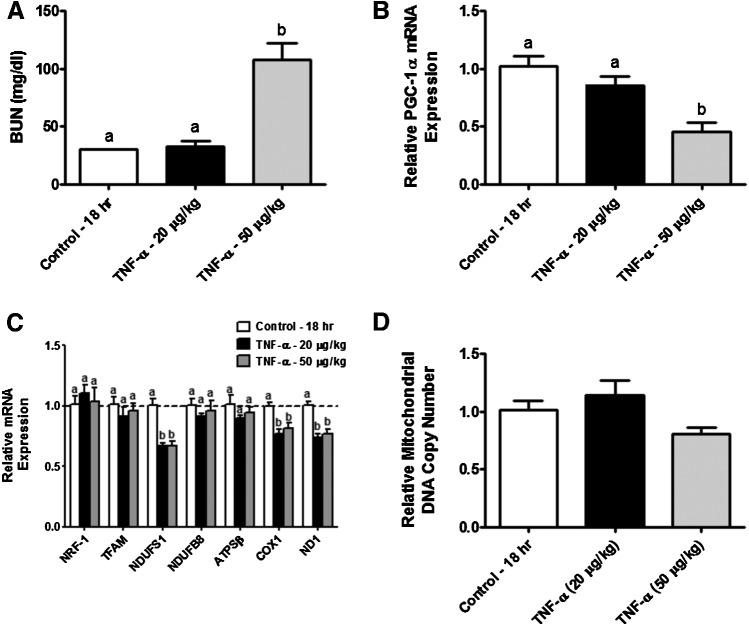
Recombinant TNF-α Is Sufficient to Produce Kidney Injury and Disrupt MB in the Renal Cortex.
To further characterize the effects of TNF-α on renal dysfunction and mitochondrial homeostasis, mice received intravenous injections of low-dose recombinant murine TNF-α (20 μg/kg), high-dose TNF-α (50 μg/kg), or the appropriate vehicle. The TNF-α dosing was based on preliminary experiments and previous reports to determine the appropriate doses that have no effect on renal function (low dose) or produce renal injury (high dose) (Xu et al., 2014).
As expected, an increase in BUN was noted only in mice receiving high-dose TNF-α (Fig. 10A). Renal dysfunction in these animals was associated with a 55% decrease in renal cortical PGC-1α mRNA (Fig. 10B). Both low- and high-dose TNF-α suppressed transcript levels of both nuclear-encoded (NDUFS1) and mitochondrial-encoded (ND1, COX1) respiratory proteins (Fig. 10C). A modest but not statistically significant decrease in mitochondrial DNA content was observed in animals treated with high-dose TNF-α (Fig. 10D). These findings indicate that recombinant TNF-α is sufficient to cause both renal injury and suppression of MB in the renal cortex.
Fig. 10.
Recombinant TNF-α induces AKI and renal mitochondrial dysfunction in mice. Mice were treated with recombinant TNF-α at variable doses (20 or 50 μg/kg) or the appropriate diluent. (A) Serum was collected at 18 hours and BUN was determined. Total RNA and DNA were extracted from the renal cortex to assess expression of (B) PGC-1α, (C) downstream targets, and (D) relative mitochondrial DNA content by qRT-PCR. Values are mean ± S.E.M. from n = 6 animals/group (P < 0.05 where denoted by different superscripts).
Discussion
Disruption of mitochondrial homeostasis is an important contributor to the initiation and progression of both tubular injury and renal dysfunction in AKI (Tran et al., 2011; Funk and Schnellmann, 2012; Che et al., 2014). Mitochondrial turnover is regulated by a complex interplay between fission/fusion, autophagy/mitophagy, and MB (Gottlieb and Gustafsson, 2011; Stallons et al., 2013). Our laboratory and others have recently demonstrated alterations in MB in experimental models of AKI (Weinberg, 2011; Funk and Schnellmann, 2012; Jesinkey et al., 2014; Stallons et al., 2014). MB is tightly controlled by the PGC-1 family of transcriptional coactivators including PGC-1α, PGC-1β, and PRC which coordinate both nuclear and mitochondrial responses to increase cellular mitochondrial content. PGC-1α is considered a master regulator of MB in organs with high energy demands including the kidney (Puigserver et al., 1998; Scarpulla, 2011) PGC-1α expression is localized to renal proximal tubule cells, which rely on mitochondrial ATP production to facilitate active transport of solutes, indicating that MB may be essential for tubular function (Portilla et al., 2002).
Recent studies have characterized mitochondrial dysfunction in sepsis-induced AKI (Tran et al., 2011; Patil et al., 2014). Tran et al. (2011) demonstrated that mitochondrial dysfunction was associated with acute downregulation of PGC-1α in the kidney after endotoxin exposure or CLP in mice. PGC-1α suppression in these models was correlated with both reduced expression of transcriptional targets of PGC-1α and renal dysfunction. Restoration of normal renal function in LPS-treated mice given saline resuscitation at the 18-hour time point coincided with the return of PGC-1α mRNA and protein to baseline levels, further indicating a potential role for MB in both the pathogenesis of and recovery from septic AKI. Proximal tubule–specific PGC-1α knockout in mice resulted in prolonged renal dysfunction in response to systemic LPS exposure. Together, these findings provide strong evidence that PGC-1α and MB may be viable therapeutic targets in sepsis-induced AKI.
Systemic endotoxin exposure in mice led to rapid deterioration of renal function as measured by BUN at 3 hours, and further increases in BUN and renal cortical KIM-1 and NGAL at 18 hours. Despite relatively minimal renal histologic findings, these data provide strong molecular evidence for the involvement of tubular insult in the pathophysiology of sepsis-induced AKI.
Progressive renal dysfunction and tubular cell injury were closely associated with a reduction in PGC-1α mRNA and protein in the renal cortex after endotoxin administration. These findings are similar to previous studies reporting negative correlations between BUN and PGC-1α transcript levels in mice receiving LPS or CLP (Tran et al., 2011). Interestingly, lower doses of LPS that did not induce renal dysfunction acutely had a similar effect on PGC-1α mRNA, and PGC-1α protein levels did not change at the 3-hour time point when renal and tubular injury were first observed, as indicated by increased BUN and KIM-1 mRNA expression. These findings indicate that suppression of PGC-1α and subsequent MB is unlikely to be the initial causative factor and alone is not sufficient for the development of sepsis-induced AKI.
Early increases in circulating proinflammatory cytokines and renal microvascular dysfunction are also important mediators of renal injury in mice after systemic LPS exposure (Cunningham et al., 2002; Wu et al., 2007b). However, suppression of renal cortical PGC-1α and MB likely contribute to disease progression through disruption of energy-dependent tubular transport and repair processes (Soltoff, 1986; Thadhani et al., 1996; Nowak et al., 1998). This idea is supported by earlier studies demonstrating that both global and proximal tubule–specific PGC-1α knockout leads to persistent renal injury in LPS-induced AKI in mice (Tran et al., 2011).
We also measured transcript levels of PGC-1β and PRC. PGC-1β expression was decreased, but not as markedly as PGC-1α. In contrast, PRC mRNA levels rose after LPS treatment similar to findings reported in ischemia/reperfusion- and glycerol-induced AKI (Funk and Schnellmann, 2012). Given the relative lack of knowledge regarding the role of PGC-1β and PRC in renal mitochondrial homeostasis, it is difficult to interpret these findings, so further work is warranted.
Previous studies showed that TLR4 is required for LPS-induced renal dysfunction (Cunningham et al., 2004). However, a number of TLR4-independent actions of LPS have been described (Hagar et al., 2013; Kayagaki et al., 2013). As predicted, TLR4-deficient mice did not develop renal injury, and markers of MB and mitochondrial DNA content did not decrease after endotoxin exposure. These findings demonstrate that TLR4 is required for suppression of renal PGC-1α and MB in LPS-induced AKI. It is important to note that the MB response to sepsis is tissue specific. Upregulation of hepatic PGC-1α and PGC-1β is markedly enhanced in TLR4-deficient mice after sepsis, suggesting that TLR4 may be an important negative regulator of MB (Sweeney et al., 2010). Further studies are needed to evaluate the possibility that TLR4 activation is a common mechanism underlying suppression of MB in multiple forms of AKI.
Binding of LPS to TLR4 activates a number of downstream signaling mediators, most notably NF-κB and MAPK, including ERK1/2, p38 MAPK, and c-Jun N-terminal kinase (Ostuni et al., 2010; Lin and Tang, 2014). We observed rapid (1 hour) activation of TPL-2/MEK/ERK signaling in the renal cortex. These findings are similar to those of previous studies demonstrating TLR4-dependent increases in ERK1/2 phosphorylation after LPS exposure in the medullary thick ascending limb of the kidney (Watts et al., 2013). Although TPL-2 is known to be required for LPS-induced ERK1/2 activation in macrophages, this is the first study to demonstrate increased TPL-2 phosphorylation in the renal cortex in response to systemic endotoxin exposure (Dumitru et al., 2000; Banerjee et al., 2006). A recent study did reveal that TPL-2 knockout mice are protected from kidney ischemia/reperfusion, although this effect was not attributed to the MAPK function of TPL-2 (Yaomura et al., 2008).
MEK/ERK signaling has been implicated as a negative regulator of both PGC-1α and MB. Pharmacologic inhibition of MEK reversed reductions in protein levels of PGC-1α and downstream regulators of MB (NRF-1, TFAM) in the hippocampi of rats receiving intracerebroventricular injections of amyloid-β (Ashabi et al., 2012). In addition, blockade of ERK activation prevented palmitate-induced downregulation of PGC-1α in skeletal muscle myotubes in vitro (Coll et al., 2006). The MEK1/2 inhibitor GSK1120212 (GSK112) blocked ERK1/2 activation and reduced early renal dysfunction and tubular injury (3 hours) in mice subjected to systemic LPS. The protective effects of GSK112 were associated with restoration of renal cortical PGC-1α expression. These findings indicate an important role for MEK/ERK signaling in LPS-induced renal injury and suppression of MB. In mice observed to 18 hours after LPS exposure, GSK112 partially attenuated the loss of renal function and injury to the proximal tubule. However, only modest effects were noted on PGC-1α expression and mitochondrial DNA content. This may indicate that the TPL-2/MEK/ERK pathway is essential for early suppression of PGC-1α in the renal cortex after endotoxic AKI, but other signaling mechanisms contribute to late-phase disruption of MB and renal dysfunction. Among these, NF-κB has been identified as a potential regulator of PGC-1α transcriptional activity (Alvarez-Guardia et al., 2010; Remels et al., 2013). Further work is necessary to address the role of NF-κB in LPS-induced mitochondrial dysfunction.
MEK/ERK activation downstream of TLR4 results in activation of a transcriptional program to increase cytokine expression in response to LPS (Guha et al., 2001; Banerjee et al., 2006). In addition, proinflammatory cytokines have been implicated in regulation of PGC-1α and MB (Tran et al., 2011; Remels et al., 2013). Administration of exogenous TNF-α reduced expression of PGC-1α and its transcriptional targets in primary human renal epithelial cells in vitro (Tran et al., 2011). In addition, TNF-α and IL-1β induced disruption of MB in skeletal muscle cells (Remels et al., 2013). As expected, inhibition of MEK/ERK signaling attenuated early upregulation of both TNF-α and IL-1β in the renal cortex of LPS-treated mice. Mice pretreated with an anti–TNF-α neutralizing antibody and exposed to LPS exhibited less PGC-1α mRNA loss. The partial restoration of PGC-1α after TNF-α neutralization may indicate that multiple proinflammatory cytokines (TNF-α, IL-1β, IL-6) signal through similar mechanisms to suppress PGC-1α in the setting of sepsis-induced AKI.
To our knowledge, this is the first study to report the effects of TNF-α neutralization on PGC-1α and subsequent MB in vivo. We did not detect an effect of anti–TNF-α on BUN 18 hours after LPS exposure. However, an earlier study using the same TNF-α neutralizing antibody before endotoxin administration noted a significant reduction in BUN at the 4-hour time point (Bhargava et al., 2013). We were able to reproduce the effects of LPS on renal dysfunction and suppression of PGC-1α expression by administration of recombinant TNF-α in naïve mice. Together, these findings strongly implicate TNF-α as a downstream mediator of TLR4/MEK/ERK signaling in LPS-induced AKI and PGC-1α and MB suppression.
A significant decrease in cortical peritubular capillary flow has been noted as early as 2 hours after LPS exposure in mice, indicating that LPS has rapid effects on renal hemodynamics (Wu et al., 2007b). A limitation of our current study is that it does not address whether modulation of TLR4/MEK/ERK and TNF-α signaling might improve microvascular function and thereby restore glomerular filtration in response to LPS. TNF-α neutralization using the soluble decoy receptor TNFsRp55 has been shown to restore both glomerular filtration and renal plasma flow after systemic exposure to a lower dose of LPS (5 mg/kg) (Knotek et al., 2001). Future studies using conditional, tissue-specific knockout of TLR4 and downstream signaling targets in the tubular epithelium, vascular endothelium, and vascular smooth muscle may address whether the renal protective effects observed in this study are due to direct actions of pharmacologic agents on the tubular epithelium or indirect actions on the renal vasculature.
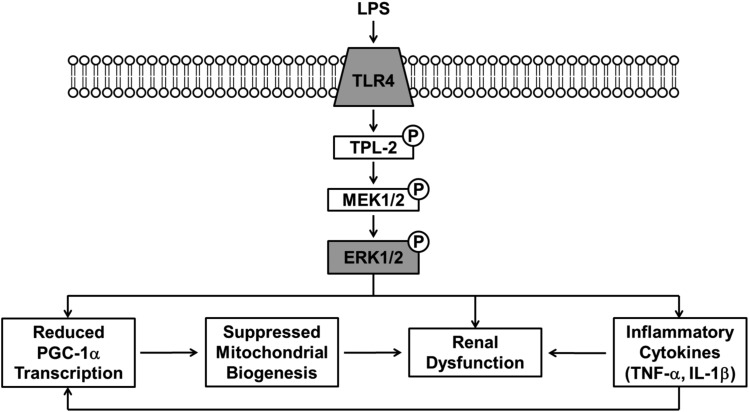
The current study identifies a novel mechanism mediating injury and suppression of MB in a mouse model of septic AKI. In particular, the TLR4/TPL-2/MEK/ERK/TNF-α signaling axis was required for early renal dysfunction and disruption of mitochondrial homeostasis in LPS-induced AKI (Fig. 11). This pathway may represent a viable therapeutic target in the treatment of sepsis-associated AKI. Further studies are warranted to determine whether this mechanism is common to other forms of AKI and to identify the downstream targets of ERK and inflammatory cytokines in this process.
Fig. 11.
Proposed mechanisms of LPS-induced suppression of mitochondrial biogenesis in the renal cortex. Systemic LPS exposure leads to activation of TLR4, which, in turn, initiates signaling through the TPL-2/MEK/ERK pathway via phosphorylation (P). ERK1/2 activation contributes to multiple downstream effects of LPS, including renal dysfunction, suppression of PGC-1α, and subsequent mitochondrial biogenesis and production of proinflammatory cytokines, such as TNF-α and IL-1β. Disruption of PGC-1α and MB leads to progressive renal dysfunction and prevents recovery after sepsis-induced AKI (Tran et al., 2011). TNF-α production also contributes to renal dysfunction and decreases PGC-1α transcription to further amplify LPS-mediated effects (Cunningham et al., 2002; Bhargava et al., 2013).
Abbreviations
- AKI
acute kidney injury
- ATPSβ
ATP synthase β
- BUN
blood urea nitrogen
- CLP
cecal ligation and puncture
- COX1
cytochrome c oxidase subunit 1
- ERK
extracellular signal-regulated kinase
- IL
interleukin
- KIM-1
kidney injury molecule-1
- KO
knockout
- LPS
lipopolysaccharide
- MB
mitochondrial biogenesis
- MAPK
mitogen-activated protein kinase
- MEK
mitogen-activated protein kinase kinase
- ND1
NADH dehydrogenase subunit 1
- NDUFB8
NADH dehydrogenase (ubiquinone) β-subcomplex 8
- NDUFS1
NADH dehydrogenase (ubiquinone) Fe-S protein 1
- NF-κB
nuclear factor κB
- NGAL
neutrophil gelatinase-associated lipocalin
- NRF-1
nuclear respiratory factor-1
- PGC-1α
peroxisome proliferator-activated receptor γ coactivator-1α
- PGC-1β
peroxisome proliferator-activated receptor γ coactivator-1β
- PRC
peroxisome proliferator-activated receptor γ coactivator-related protein 1
- qRT-PCR
quantitative real-time polymerase chain reaction
- TNF-α
tumor necrosis factor-α
- TFAM
mitochondrial transcription factor a
- TLR4
Toll-like receptor 4
- TPL-2
tumor progression locus 2
Authorship Contributions
Participated in research design: Smith, Stallons, Collier, Schnellmann.
Conducted experiments: Smith, Stallons, Collier.
Contributed new reagents or analytic tools: Chavin.
Performed data analysis: Smith, Stallons, Collier, Schnellmann.
Wrote or contributed to the writing of the manuscript: Smith, Schnellmann.
Footnotes
This work was supported in part by the National Institutes of Health National Institute of General Medical Sciences [Grants GM084147 (to R.G.S.) and P20-GM103542-02 (to South Carolina COBRE in Oxidants, Redox Balance, and Stress Signaling]; the National Institutes of Health National Center for Research Resources [Grant UL1-RR029882]; the Biomedical Laboratory Research and Development Program of the Department of Veterans Affairs [Grant 5I01 BX-000851 (to R.G.S.)]; and the South Carolina Clinical and Translational Research Institute at the Medical University of South Carolina. Animal facilities were funded by the National Institutes of Health National Center for Research Resources [Grant C06-RR015455].
References
- Alvarez-Guardia D, Palomer X, Coll T, Davidson MM, Chan TO, Feldman AM, Laguna JC, Vázquez-Carrera M. (2010) The p65 subunit of NF-κB binds to PGC-1α, linking inflammation and metabolic disturbances in cardiac cells. Cardiovasc Res 87:449–458. [DOI] [PubMed] [Google Scholar]
- Ashabi G, Ramin M, Azizi P, Taslimi Z, Alamdary SZ, Haghparast A, Ansari N, Motamedi F, Khodagholi F. (2012) ERK and p38 inhibitors attenuate memory deficits and increase CREB phosphorylation and PGC-1α levels in Aβ-injected rats. Behav Brain Res 232:165–173. [DOI] [PubMed] [Google Scholar]
- Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, et al. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators (2007) Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes. Clin J Am Soc Nephrol 2:431–439. [DOI] [PubMed] [Google Scholar]
- Banerjee A, Gugasyan R, McMahon M, Gerondakis S. (2006) Diverse Toll-like receptors utilize Tpl2 to activate extracellular signal-regulated kinase (ERK) in hemopoietic cells. Proc Natl Acad Sci USA 103:3274–3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhargava R, Altmann CJ, Andres-Hernando A, Webb RG, Okamura K, Yang Y, Falk S, Schmidt EP, Faubel S. (2013) Acute lung injury and acute kidney injury are established by four hours in experimental sepsis and are improved with pre, but not post, sepsis administration of TNF-α antibodies. PLoS ONE 8:e79037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawla LS, Seneff MG, Nelson DR, Williams M, Levy H, Kimmel PL, Macias WL. (2007) Elevated plasma concentrations of IL-6 and elevated APACHE II score predict acute kidney injury in patients with severe sepsis. Clin J Am Soc Nephrol 2:22–30. [DOI] [PubMed] [Google Scholar]
- Che R, Yuan Y, Huang S, Zhang A. (2014) Mitochondrial dysfunction in the pathophysiology of renal diseases. Am J Physiol Renal Physiol 306:F367–F378. [DOI] [PubMed] [Google Scholar]
- Coll T, Jové M, Rodríguez-Calvo R, Eyre E, Palomer X, Sánchez RM, Merlos M, Laguna JC, Vázquez-Carrera M. (2006) Palmitate-mediated downregulation of peroxisome proliferator-activated receptor-gamma coactivator 1α in skeletal muscle cells involves MEK1/2 and nuclear factor-κB activation. Diabetes 55:2779–2787. [DOI] [PubMed] [Google Scholar]
- Cunningham PN, Dyanov HM, Park P, Wang J, Newell KA, Quigg RJ. (2002) Acute renal failure in endotoxemia is caused by TNF acting directly on TNF receptor-1 in kidney. J Immunol 168:5817–5823. [DOI] [PubMed] [Google Scholar]
- Cunningham PN, Wang Y, Guo R, He G, Quigg RJ. (2004) Role of Toll-like receptor 4 in endotoxin-induced acute renal failure. J Immunol 172:2629–2635. [DOI] [PubMed] [Google Scholar]
- DeFranco AL, Crowley MT, Finn A, Hambleton J, Weinstein SL. (1998) The role of tyrosine kinases and map kinases in LPS-induced signaling. Prog Clin Biol Res 397:119–136. [PubMed] [Google Scholar]
- Dumitru CD, Ceci JD, Tsatsanis C, Kontoyiannis D, Stamatakis K, Lin JH, Patriotis C, Jenkins NA, Copeland NG, Kollias G, et al. (2000) TNF-alpha induction by LPS is regulated posttranscriptionally via a Tpl2/ERK-dependent pathway. Cell 103:1071–1083. [DOI] [PubMed] [Google Scholar]
- Ellett JD, Evans ZP, Atkinson C, Schmidt MG, Schnellmann RG, Chavin KD. (2009) Toll-like receptor 4 is a key mediator of murine steatotic liver warm ischemia/reperfusion injury. Liver Transplant 15:1101–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finck BN, Kelly DP. (2006) PGC-1 coactivators: inducible regulators of energy metabolism in health and disease. J Clin Invest 116:615–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk JA, Schnellmann RG. (2012) Persistent disruption of mitochondrial homeostasis after acute kidney injury. Am J Physiol Renal Physiol 302:F853–F864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk JA, Schnellmann RG. (2013) Accelerated recovery of renal mitochondrial and tubule homeostasis with SIRT1/PGC-1α activation following ischemia-reperfusion injury. Toxicol Appl Pharmacol 273:345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmartin AG, Bleam MR, Groy A, Moss KG, Minthorn EA, Kulkarni SG, Rominger CM, Erskine S, Fisher KE, Yang J, et al. (2011) GSK1120212 (JTP-74057) is an inhibitor of MEK activity and activation with favorable pharmacokinetic properties for sustained in vivo pathway inhibition [erratum: 2012;15:2413]. Clin Cancer Res 17:989–1000. [DOI] [PubMed] [Google Scholar]
- Gomez H, Ince C, De Backer D, Pickkers P, Payen D, Hotchkiss J, Kellum JA. (2014) A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock 41:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb RA, Gustafsson AB. (2011) Mitochondrial turnover in the heart. Biochim Biophys Acta 1813:1295–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guha M, O’Connell MA, Pawlinski R, Hollis A, McGovern P, Yan SF, Stern D, Mackman N. (2001) Lipopolysaccharide activation of the MEK-ERK1/2 pathway in human monocytic cells mediates tissue factor and tumor necrosis factor alpha expression by inducing Elk-1 phosphorylation and Egr-1 expression. Blood 98:1429–1439. [DOI] [PubMed] [Google Scholar]
- Guo R, Wang Y, Minto AW, Quigg RJ, Cunningham PN. (2004) Acute renal failure in endotoxemia is dependent on caspase activation. J Am Soc Nephrol 15:3093–3102. [DOI] [PubMed] [Google Scholar]
- Hagar JA, Powell DA, Aachoui Y, Ernst RK, Miao EA. (2013) Cytoplasmic LPS activates caspase-11: implications in TLR4-independent endotoxic shock. Science 341:1250–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesinkey SR, Funk JA, Stallons LJ, Wills LP, Megyesi JK, Beeson CC, Schnellmann RG. (2014) Formoterol restores mitochondrial and renal function after ischemia-reperfusion injury. J Am Soc Nephrol 25:1157–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayagaki N, Wong MT, Stowe IB, Ramani SR, Gonzalez LC, Akashi-Takamura S, Miyake K, Zhang J, Lee WP, Muszyński A, et al. (2013) Noncanonical inflammasome activation by intracellular LPS independent of TLR4. Science 341:1246–1249. [DOI] [PubMed] [Google Scholar]
- Knotek M, Rogachev B, Wang W, Ecder T, Melnikov V, Gengaro PE, Esson M, Edelstein CL, Dinarello CA, Schrier RW. (2001) Endotoxemic renal failure in mice: role of tumor necrosis factor independent of inducible nitric oxide synthase. Kidney Int 59:2243–2249. [DOI] [PubMed] [Google Scholar]
- Langenberg C, Bagshaw SM, May CN, Bellomo R. (2008) The histopathology of septic acute kidney injury: a systematic review. Crit Care 12:R38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M, Tang SC. (2014) Toll-like receptors: sensing and reacting to diabetic injury in the kidney. Nephrol Dial Transplant 29:746–754. [DOI] [PubMed] [Google Scholar]
- Luan H, Zhang Q, Wang L, Wang C, Zhang M, Xu X, Zhou H, Li X, Xu Q, He F, Yuan J, Lv Y. (2014) OM85-BV induced the productions of IL-1β, IL-6, and TNF-α via TLR4- and TLR2-mediated ERK1/2/NF-κB pathway in RAW264.7 cells. J Interferon Cytokine Res 34:526–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowak G, Aleo MD, Morgan JA, Schnellmann RG. (1998) Recovery of cellular functions following oxidant injury. Am J Physiol 274:F509–F515. [DOI] [PubMed] [Google Scholar]
- Ostuni R, Zanoni I, Granucci F. (2010) Deciphering the complexity of Toll-like receptor signaling. Cell Mol Life Sci 67:4109–4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil NK, Parajuli N, MacMillan-Crow LA, Mayeux PR. (2014) Inactivation of renal mitochondrial respiratory complexes and manganese superoxide dismutase during sepsis: mitochondria-targeted antioxidant mitigates injury. Am J Physiol Renal Physiol 306:F734–F743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portilla D, Dai G, McClure T, Bates L, Kurten R, Megyesi J, Price P, Li S. (2002) Alterations of PPARα and its coactivator PGC-1 in cisplatin-induced acute renal failure. Kidney Int 62:1208–1218. [DOI] [PubMed] [Google Scholar]
- Puigserver P, Wu Z, Park CW, Graves R, Wright M, Spiegelman BM. (1998) A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell 92:829–839. [DOI] [PubMed] [Google Scholar]
- Remels AH, Gosker HR, Bakker J, Guttridge DC, Schols AM, Langen RC. (2013) Regulation of skeletal muscle oxidative phenotype by classical NF-κB signalling. Biochim Biophys Acta 1832:1313–1325. [DOI] [PubMed] [Google Scholar]
- Sanchis-Gomar F, García-Giménez JL, Gómez-Cabrera MC, Pallardó FV. (2014) Mitochondrial biogenesis in health and disease. Molecular and therapeutic approaches. Curr Pharm Des 20:5619–5633. [DOI] [PubMed] [Google Scholar]
- Scarpulla RC. (2011) Metabolic control of mitochondrial biogenesis through the PGC-1 family regulatory network. Biochim Biophys Acta 1813:1269–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer L, Babelova A, Kiss E, Hausser HJ, Baliova M, Krzyzankova M, Marsche G, Young MF, Mihalik D, Götte M, et al. (2005) The matrix component biglycan is proinflammatory and signals through Toll-like receptors 4 and 2 in macrophages. J Clin Invest 115:2223–2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrier RW, Wang W. (2004) Acute renal failure and sepsis. N Engl J Med 351:159–169. [DOI] [PubMed] [Google Scholar]
- Silvester W, Bellomo R, Cole L. (2001) Epidemiology, management, and outcome of severe acute renal failure of critical illness in Australia. Crit Care Med 29:1910–1915. [DOI] [PubMed] [Google Scholar]
- Soltoff SP. (1986) ATP and the regulation of renal cell function. Annu Rev Physiol 48:9–31. [DOI] [PubMed] [Google Scholar]
- Stallons LJ, Funk JA, Schnellmann RG. (2013) Mitochondrial homeostasis in acute organ failure. Curr Pathobiol Rep 1:169–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallons LJ, Whitaker RM, Schnellmann RG. (2014) Suppressed mitochondrial biogenesis in folic acid-induced acute kidney injury and early fibrosis. Toxicol Lett 224:326–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney TE, Suliman HB, Hollingsworth JW, Piantadosi CA. (2010) Differential regulation of the PGC family of genes in a mouse model of Staphylococcus aureus sepsis. PLoS ONE 5:e11606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takasu O, Gaut JP, Watanabe E, To K, Fagley RE, Sato B, Jarman S, Efimov IR, Janks DL, Srivastava A, et al. (2013) Mechanisms of cardiac and renal dysfunction in patients dying of sepsis. Am J Respir Crit Care Med 187:509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thadhani R, Pascual M, Bonventre JV. (1996) Acute renal failure. N Engl J Med 334:1448–1460. [DOI] [PubMed] [Google Scholar]
- Tran M, Tam D, Bardia A, Bhasin M, Rowe GC, Kher A, Zsengeller ZK, Akhavan-Sharif MR, Khankin EV, Saintgeniez M, et al. (2011) PGC-1α promotes recovery after acute kidney injury during systemic inflammation in mice. J Clin Invest 121:4003–4014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, et al. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818. [DOI] [PubMed] [Google Scholar]
- Waikar SS, Liu KD, Chertow GM. (2008) Diagnosis, epidemiology and outcomes of acute kidney injury. Clin J Am Soc Nephrol 3:844–861. [DOI] [PubMed] [Google Scholar]
- Wan L, Bagshaw SM, Langenberg C, Saotome T, May C, Bellomo R. (2008) Pathophysiology of septic acute kidney injury: what do we really know? Crit Care Med 36(4, Suppl)S198–S203. [DOI] [PubMed] [Google Scholar]
- Wang Z, Herzog C, Kaushal GP, Gokden N, Mayeux PR. (2011) Actinonin, a meprin A inhibitor, protects the renal microcirculation during sepsis. Shock 35:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts BA, 3rd, George T, Good DW. (2013) Lumen LPS inhibits HCO3− absorption in the medullary thick ascending limb through TLR4-PI3K-Akt-mTOR-dependent inhibition of basolateral Na+/H+ exchange. Am J Physiol Renal Physiol 305:F451–F462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg JM. (2011) Mitochondrial biogenesis in kidney disease. J Am Soc Nephrol 22:431–436. [DOI] [PubMed] [Google Scholar]
- Wills LP, Trager RE, Beeson GC, Lindsey CC, Peterson YK, Beeson CC, Schnellmann RG. (2012) The β2-adrenoceptor agonist formoterol stimulates mitochondrial biogenesis. J Pharmacol Exp Ther 342:106–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L, Gokden N, Mayeux PR. (2007a) Evidence for the role of reactive nitrogen species in polymicrobial sepsis-induced renal peritubular capillary dysfunction and tubular injury. J Am Soc Nephrol 18:1807–1815. [DOI] [PubMed] [Google Scholar]
- Wu L, Tiwari MM, Messer KJ, Holthoff JH, Gokden N, Brock RW, Mayeux PR. (2007b) Peritubular capillary dysfunction and renal tubular epithelial cell stress following lipopolysaccharide administration in mice. Am J Physiol Renal Physiol 292:F261–F268. [DOI] [PubMed] [Google Scholar]
- Xu C, Chang A, Hack BK, Eadon MT, Alper SL, Cunningham PN. (2014) TNF-mediated damage to glomerular endothelium is an important determinant of acute kidney injury in sepsis. Kidney Int 85:72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaguchi T, Kakefuda R, Tajima N, Sowa Y, Sakai T. (2011) Antitumor activities of JTP-74057 (GSK1120212), a novel MEK1/2 inhibitor, on colorectal cancer cell lines in vitro and in vivo. Int J Oncol 39:23–31. [DOI] [PubMed] [Google Scholar]
- Yamaguchi T, Kakefuda R, Tanimoto A, Watanabe Y, Tajima N. (2012) Suppressive effect of an orally active MEK1/2 inhibitor in two different animal models for rheumatoid arthritis: a comparison with leflunomide. Inflamm Res 61:445–454. [DOI] [PubMed] [Google Scholar]
- Yaomura T, Tsuboi N, Urahama Y, Hobo A, Sugimoto K, Miyoshi J, Matsuguchi T, Reiji K, Matsuo S, Yuzawa Y. (2008) Serine/threonine kinase, Cot/Tpl2, regulates renal cell apoptosis in ischaemia/reperfusion injury. Nephrology (Carlton) 13:397–404. [DOI] [PubMed] [Google Scholar]