Abstract
Aim
To compare the original normative data of the Alberta Infant Motor Scale (AIMS) (n=2202) collected 20 years ago with a contemporary sample of Canadian infants.
Method
This was a cross-sectional cohort study of 650 Canadian infants (338 males, 312 females; mean age 30.9wks [SD 15.5], range 2wks–18mo) assessed once on the AIMS. Assessments were stratified by age, and infants proportionally represented the ethnic diversity of Canada. Logistic regression was used to place AIMS items on an age scale representing the age at which 50% of the infants passed an item on the contemporary data set and the original data set. Forty-three items met the criterion for stable regression results in both data sets.
Results
The correlation coefficient between the age locations of items on the original and contemporary data sets was 0.99. The mean age difference between item locations was 0.7 weeks. Age values from the original data set when converted to the contemporary scale differed by less than 1 week.
Interpretation
The sequence and age at emergence of AIMS items has remained similar over 20 years and current normative values remain valid. Concern that the ‘back to sleep’ campaign has influenced the age at emergence of gross motor abilities is not supported.
What this paper adds
The current Alberta Infant Motor Scale (AIMS) normative values remain appropriate to interpret an infant's total AIMS score.
Present infant gross motor abilities are similar to those documented 20 years ago.
‘Back to sleep’ campaigns encouraging supine sleep positions have not affected the age at emergence of gross motor abilities as measured by AIMS items.
The Alberta Infant Motor Scale1 (AIMS) is a Canadian, norm-referenced measure to assess the gross motor abilities of infants from birth to independent walking. Since its publication in 1994, the AIMS has been used internationally as a clinical2,3 and research outcome measure,4–8 and as an educational resource.9 The AIMS normative data comprise 2202 infants born in Alberta, Canada, between March 1990 and June 1992. The present re-evaluation of the normative data was undertaken for three reasons. First, the ‘back to sleep’ campaign initiated internationally in the early 1990s10,11 coincided with the AIMS normative data collection, but many infants were not yet being placed in the supine position for sleep. Subsequent concern that the age at appearance of some infant gross motor abilities may be later because of the introduction of supine sleep position,5,6,12,13 some reports in the literature have suggested that the AIMS normative data were outdated and may identify infants with typical development as delayed in their motor development.6,14,15 The second impetus for a re-evaluation of the normative data was the changing ethnic diversity of Canadian infants; 16.2% of the Canadian population are visible minorities, 3.8% of Canadians have an Aboriginal background but only 10% of the original AIMS normative sample had one of these backgrounds. Finally, some authors have voiced concern that the AIMS norms are not applicable to infants in their country,16 and it would be beneficial to provide them with a feasible statistical method to compare their infants' AIMS data with the normative data. The objective of the study was to compare the original normative data of the AIMS with a contemporary, representative sample of Canadian infants.
Method
Design
A cross-sectional cohort study design was used. As far as possible, the study design mirrored the design of the original normative project.
Participants
In the original normative study, the 58 AIMS items were placed in one of three age groups representing their ages of emergence: 22 weeks or less (19 items), 23 to 36 weeks (19 items), and 37 weeks and older (20 items). For this study, a sample of 450 infants (150 infants in each age category) would produce a standard error equal to the largest standard error in the original AIMS norms (1.3 points). To ensure both the inclusion of infants representing visible minorities (16.2%) and Aboriginal categories (3.8%) as reported in the 2006 Canadian Census and the representation of gross motor variability,17 an additional 75 infants were added to each age category for a targeted sample size of 675. Assuming a 25% attrition rate, the recruitment target was 845 infants from six Canadian cities. Fifty-four preterm infants (8%) were included in the recruitment strategy to represent the prevalence rate of preterm births in Canada.18
For the original project, the Department of Vital Statistics identified a random sample of potential participants, but current confidentiality rules prevented similar identification for the present study. Instead families were identified from the nurseries of hospitals in six Canadian cities (Vancouver, Edmonton, Winnipeg, Toronto, Montreal, Halifax) when their infants were born. In most centers, study information letters were provided to all families and the recruiting person, usually a nurse, met with the families who wanted to know more about the study. Information about families who wanted to participate was sent to one of two project coordinators who then contacted the family and discussed study specifics. Each infant was randomly assigned an assessment age in one of the three age categories, using an age grid in weeks to ensure that ages in weeks were uniformly represented in each of the three age categories. Infants representing preterm, visible minority, and Aboriginal subcategories were distributed among the three age categories. The selection criteria for participation were similar for both studies; all families interested in participating were included in the study.
Data collection
Each infant had one AIMS assessment at an assigned assessment age between 2 weeks and 18 months (adjusted age was used for preterm infants). Two pediatric therapists in each of the six cities attended a 1-day training session led by JD and DB, who were assessors in the original normative project and who have both used the AIMS extensively. At conclusion of the training, each therapist observed and scored a video-recorded AIMS assessment. Therapists had to achieve an 80% item agreement with the criterion standard scoring criteria. During the 2 years of data collection, therapists completed two more video-scoring sessions. In addition, the therapists participated in three teleconferences to discuss scoring and other administration issues as the assessment ages changed, and a site visit was made to each participating centre by either DB or JD to observe each therapist completing assessments and to address any specific site issues.
All assessments were completed at a clinical or academic site. A therapist scored each item and provided general information to the parent. The two project coordinators calculated the total score and the centile rank for each assessment using the centile graph on the AIMS score-sheet (Fig.1). The graph plots infants' ages in months (horizontal axis) and the total raw score (vertical axis) and provides the 5th, 10th, 25th, 50th, 75th, and 90th centile ranks. A centile rank score is derived by plotting an infant's age (to the closest week) against his or her total score, interpolating the centile rank if necessary. The project coordinators designed a grid of centile ranks and ages to ensure that interpolation of centile rankings from the centile graph were the same for infants of the same age with the same total score.
Figure 1.
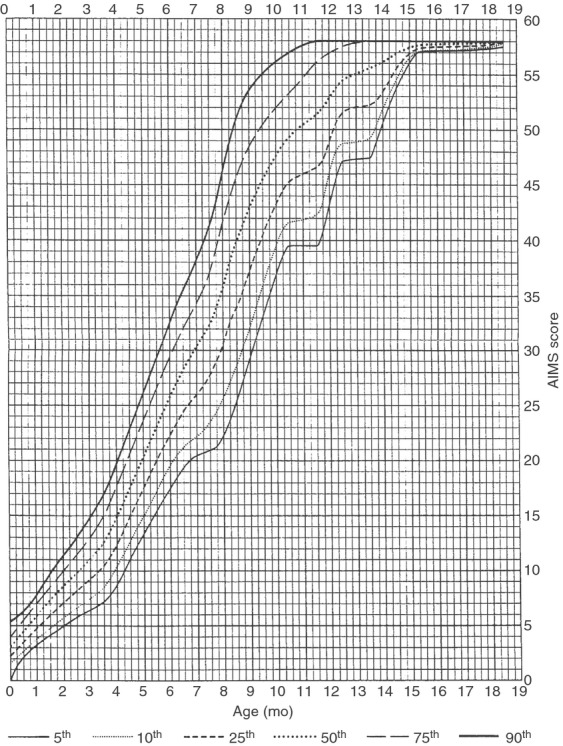
Alberta Infant Motor Scale (AIMS) centile ranks graph.
Data analyses
An important psychometric characteristic of the AIMS is that items describing differing motor abilities can be placed on the age scale representing the age when 50% of the infants would pass each item. This is known as the item location. Item locations can be calculated for each of the two data sets. Comparison of the two sets of locations makes it possible to see if the age scale shown in the original norms1 appears to have shifted. If the age scale has changed, then the norms can be brought up to date by adjusting the age scale.
There are four possible outcomes. (1) The item locations are the same in both data sets. This suggests that the original norms are appropriate for interpreting the scores of contemporary infants. (2) When plotted, the item locations for the two data sets fall on a straight line. The linear relation between the two sets of locations tells us how the current ages map onto the norming sample ages and vice versa. New tables can be generated by applying a linear transformation to the age values on the original tables. (3) The order of the items is the same but the age difference between items varies. A curvilinear transformation of the original age scale is then necessary to generate new tables. (4) The order of the items has changed, requiring a new norming process with a larger sample.
This analytic strategy provides an efficient way to compare data sets without recruiting a sample as large as the original normative sample. We chose this method because it can be replicated feasibly by other researchers who are interested in comparing their data to the published AIMS norms.
To explore the four possibilities, a logistic regression method was used to place AIMS items on the age scale for each of the two occasions. The regression parameters were rescaled to reflect the age at which 50% of the infants passed the item. Details of the analyses are in Appendix SI (online supporting information).
Ethical and administrative approval for the study was obtained from the university ethics boards and health centers.
Results
Eight-hundred and sixty-eight families were recruited and 650 infants (338 males, 312 females) completed an assessment. The sample included 15 (3.2%) infants with Aboriginal heritage and 126 (19.4%) infants of visible minority. Fifty-seven infants (8.7%) were preterm; 44 were 34 to 36 weeks' gestation, and 13 were less than 34 weeks' gestation.
Most mothers (588 [90%]) had post-secondary education, 57 (9%) had completed high school, and five (1%) had less than high school education. Five-hundred and forty-seven families (84%) reported an annual family income greater than $45 000. This income roughly represents Statistics Canada's 2011 cut-off point for families of four persons living above or below the low-income line. The mean age of infants in the original sample was 37.4 weeks (SD 17.6, corrected for preterm birth if necessary), older than the infants in the contemporary sample (mean 30.9, SD 15.5wks). The age difference is primarily because the contemporary sample was designed to have proportionately more infants in the younger age regions where most items are located. In addition, there was some attrition in the contemporary sample that occurred with infants in the oldest age category; many mothers had returned to work and could not attend their appointments. However, because the AIMS centile ranks ‘merge’ after 14 months of age because of a scoring ceiling effect, the impact of fewer infants at this older age is minimal.
Appendix SII (online supporting information) provides the results of the regression and age location for all 58 items except for the four items whose regressions could not be calculated. Ten more items were removed from the next stage of analysis because they did not meet the stability criterion that the proportion of infants passing the item be between 0.10 and 0.90 in both data sets (the regressions of age on performance are unstable for items that have more than 90% of the infants passing or failing). One additional item (Prone 21, mature creeping pattern) was removed because of concern that it had been scored incorrectly. The 8-week age difference for this item between the two data sets was the largest difference identified, and closer examination of scores revealed that some therapists had not scored this item for infants who were walking independently.
The 43 remaining items were used for the next steps in the analyses. Most of the items differed by 2 weeks or less at the age when 50% of the infants passed the item and the average age difference between item locations was 0.7 weeks (TableI). The correlation coefficient between the two sets of age locations was 0.99, revealing a strong linear trend. The original scale was mapped onto the contemporary scale using equation 3 (Appendix SI). Expressed in months, the conversion equation is:
Table I.
Agreement between item locations for 43 items used in equation 3
| Difference in location | Number of items | Item location is earlier in original data | Item location is earlier incontemporary data |
|---|---|---|---|
| <1wk | 21 | 15 | 6 |
| 1–2wks | 11 | 8 | 3 |
| 2–3wks | 9 | 8 | 1 |
| 3–4wks | 1 | 0 | 1 |
| 4–5wks | 1 | 1 | 0 |
| Total | 43 | 32 | 11 |
Across the age scale from birth to 18 months, the maximum shift is less than one-sixth of a month (i.e. <1wk). In other words, age values from the original data set when converted to the contemporary scale differed by less than 1 week.
Discussion
The results suggest that the current normative data of the AIMS remain appropriate to interpret the results of an AIMS assessment. The observed differences in the ages at emergence of individual items between the original and contemporary data are minimal and would affect neither the research nor clinical decisions made using AIMS data. Interpretation of an AIMS score is never made at the level of individual items, but rather from the centile ranking derived by plotting an infant's age to the closest week and his or her total score on the centile graph. The centile rankings provided on the centile graph would be unaffected for all infants because all age differences are less than 1 week. Even if the centile ranks were moved over by 1 week of age, the clinical decisions would not change. Previous work17 suggests that infants do not maintain the same centile score over time and that ‘windows of typical development’ should be used rather than thinking that the 90th centile is ‘better’ than the 60th. Even centile ranks near the recommended cut-off points to identify infants with atypical development (10th centile at 4mo and 5th centile at ≥8mo)19 should not be used in isolation to make clinical decisions regarding follow-up or intervention. AIMS centile rank information should be incorporated with other sources of information such as medical history, other developmental aspects of an infant's development, and the family's concerns to determine a clinical decision.
The age at emergence of gross motor milestones has remained remarkably similar over 20 years. An analysis of the age when 50% of infants passed the four rolling items on the AIMS in the two data sets has been completed and revealed that the items were very similar both in ages at appearance and order of appearance.20 Given the finding that some items appear slightly earlier in the contemporary data, the concern that the ‘back to sleep’ campaign has resulted in delayed motor abilities appears to be unfounded. It was not possible to collect information on infant sleep position for all families, but 452 families reported their infants' sleeping position. Of these families, 304 (67.2%) placed their infants in supine, 46 (10.2%) used a prone sleep position, 18 (4%) used a side position, and 84 (18.6%) used a combination of positions. The influence that ‘tummy time’ while awake may have contributed to the similarity of motor development over time cannot be determined. No information was collected about the amount of time infants played in prone during awake periods, but anecdotally many parents reported that until their infant could roll in both directions independently it was challenging to keep their infant in prone for extended periods of time while awake.
Some concern has been raised in the literature that Canadian norms on the AIMS are inappropriate for infants in other countries.16,21 Our analyses approach may be appealing to researchers interested in evaluating this issue because it requires a smaller sample size than a normative project. The very small sample sizes reported by De Kegel et al. 21 are worrisome and propose the need for new normative data. Our analysis strategy is a feasible, cost-effective strategy that can be replicated by other researchers. We are willing to share the original normative data necessary for the comparisons. However, given the stability of our results over a 20-year period and the increased ethnic diversity of the contemporary sample, it may not be necessary to investigate international differences.
The AIMS profiles of infants of specific visible minorities or gestational ages cannot be compared using these data because of small subsample sizes.
Conclusion
The original centile ranks collected over 20 years ago continue to reflect the contemporary order and age at emergence of infant motor abilities represented on the AIMS. Clinicians can use the present AIMS centiles to interpret both the research and clinical findings of an AIMS assessment.
Acknowledgments
Canadian Institutes of Health Research Funding provided funding for the project. The two project coordinators, Jamie Rishaug and Jane Terhaerdt, were instrumental to the success of the study. We thank the recruiters and assessors involved at each site. Finally, we thank the infants and their families who allowed us the privilege of observing the wonder of development once more. Dr Johanna Darrah is the co-author of ‘Motor Assessment of the Developing Infant’. (which contains the manual for the Alberta Infant Motor Scale) and receives royalties for this text.
Glossary
- AIMS
Alberta Infant Motor Scale
Supporting Information
The following additional material may be found online:
Appendix S1:Details of regression analysis.
Appendix S2: Item locations for 58 items, original and contemporary data sets.
References
- Piper M, Darrrah J. Motor Assessment of the Developing Infant. Philadelphia, PA: Saunders; 1994. [Google Scholar]
- Majnemer A, Snider L. A comparison of developmental assessments of the newborn and young infant. Ment Retard Dev Disabil Res Rev. 2005;11:68–73. doi: 10.1002/mrdd.20052. [DOI] [PubMed] [Google Scholar]
- Spittle AJ, Doyle LW, Boyd RN. A systematic review of the clinimetric properties of neuromotor assessments for preterm infants during the first year of life. Dev Med Child Neurol. 2008;50:254–66. doi: 10.1111/j.1469-8749.2008.02025.x. [DOI] [PubMed] [Google Scholar]
- Manacero S, Nunes ML. Evaluation of motor performance of preterm newborns during the first months of life using the Alberta Infant Motor Scale (AIMS) J Pediatr (Rio J) 2008;84:53–9. doi: 10.2223/JPED.1741. [DOI] [PubMed] [Google Scholar]
- Monson RM, Deitz J, Kartin D. The Relationship between Awake Positioning and Motor Performance among Infants Who Slept Supine. Pediatr Phys Ther. 2003;15:196–203. doi: 10.1097/01.PEP.0000096380.15342.51. [DOI] [PubMed] [Google Scholar]
- Majnemer A, Barr RG. Association between sleep position and early motor development. J Pediatr. 2006;149:623–9. doi: 10.1016/j.jpeds.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Sarajuuri A, Lonnqvist T, Mildh L, et al. Prospective follow-up study of children with univentricular heart: neurodevelopmental outcome at age 12 months. J Thorac Cardiov Sur. 2009;137:139–45. doi: 10.1016/j.jtcvs.2008.06.025. [DOI] [PubMed] [Google Scholar]
- Wang LY, Wang YL, Wang ST, Huang CC. Using the Alberta Infant Motor Scale to early identify very low-birth-weight infants with cystic periventricular leukomalacia. Brain Dev. 2013;35:32–7. doi: 10.1016/j.braindev.2011.08.012. [DOI] [PubMed] [Google Scholar]
- Uesugi M, Takada S, Tokuhisa K, Simada T. Reliability of video-media neurological assessment using the Alberta Infant Motor Scale. Rigakuryoho Kagaku. 2006;21:137–41. [Google Scholar]
- Kattwinkel J, Brooks J, Myerberg D. Positioning and SIDS. Pediatrics. 1992;89:1120–6. [Google Scholar]
- Society CP. Statement:reducing the risk of sudden infant death. Paediatr Child Health. 1996;1:63–7. [Google Scholar]
- Jantz JW, Blosser CD, Fruechting LA. A motor milestone change noted with a change in sleep position. Arch Pediatr Adolesc Med. 1997;151:565–8. doi: 10.1001/archpedi.1997.02170430031006. [DOI] [PubMed] [Google Scholar]
- Davis BE, Moon RY, Sachs HC, Ottolini MC. Effects of sleep position on infant motor development. Pediatrics. 1998;102:1135–40. doi: 10.1542/peds.102.5.1135. [DOI] [PubMed] [Google Scholar]
- Dudek-Shriber L, Zelazny S. The effects of prone positioning on the quality and acquisition of developmental milestones in four-month-old infants. Pediatr Phys Ther. 2007;19:48–55. doi: 10.1097/01.pep.0000234963.72945.b1. [DOI] [PubMed] [Google Scholar]
- Carmeli E, Marmur R, Cohen A, Tirosh E. Preferred sleep position and gross motor achievement in early infancy. Eur J Pediatr. 2008;168:711–5. doi: 10.1007/s00431-008-0829-4. [DOI] [PubMed] [Google Scholar]
- Fleuren KMW, Smit LS, Stijnen T, Hartman A. New reference values for the Alberta Infant Motor Scale need to be established. Acta Paediatr. 2007;96:424–7. doi: 10.1111/j.1651-2227.2007.00111.x. [DOI] [PubMed] [Google Scholar]
- Darrah J, Redfern L, Maguire T, Beaulne A, Watt J. Intra-individual stability of rate of gross motor development in full-term infants. Early Hum Dev. 1998;52:169–79. doi: 10.1016/s0378-3782(98)00028-0. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information. Too Early, Too Small: A Profile of Small Babies Across Canada. Ottawa, ON: CIHI; 2009. [Google Scholar]
- Darrah J, Piper M, Watt M-J. Assessment of gross motor skills of at-risk infants: predictive validity of the Alberta Infant Motor Scale. Dev Med Child Neurol. 1998;40:485–91. doi: 10.1111/j.1469-8749.1998.tb15399.x. [DOI] [PubMed] [Google Scholar]
- Darrah J, Bartlett DJ. Infant rolling abilities - the same of different 20 years after the back to sleep campaign? Early Hum Dev. 2013;89:311–4. doi: 10.1016/j.earlhumdev.2012.10.009. [DOI] [PubMed] [Google Scholar]
- De Kegel A, Peersman W, Onderbeke K, Baetens T, Dhooge I, Van Waelvelde H. New reference values must be established for the Alberta Infant Motor Scales for accurate identification of infants at risk for motor developmental delay in Flanders. Child Care Health Dev. 2012;39:260–7. doi: 10.1111/j.1365-2214.2012.01384.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1:Details of regression analysis.
Appendix S2: Item locations for 58 items, original and contemporary data sets.


